Abstract
Background:
We examined trends in the treatment of femoral neck fractures over the last two decades.
Methods:
We used Medicare Part A administrative data to identify patients hospitalized for closed femoral neck fracture from 1991 to 2008. We used codes from the International Classification of Diseases, Ninth Revision, to categorize treatment as nonoperative, internal fixation, hemiarthroplasty, and total hip arthroplasty. We examined differences in treatment according to hospital hip fracture volume, hospital location (rural or urban), and teaching status.
Results:
Our sample consisted of 1,119,423 patients with intracapsular hip fractures occurring from 1991 to 2008. We found a generally stable trend over time in the percentage of patients managed with nonoperative treatment, internal fixation, hemiarthroplasty, and total hip arthroplasty. We found little difference in surgical treatment across different groups of hospitals (high volume compared with low volume, urban compared with rural, and teaching compared with nonteaching). The percentage of acute care hospitals treating hip fractures remained fairly constant (74.8% in 1991 to 1993 and 69.0% in 2006 to 2008). The median number of hip fractures treated per hospital did not change (thirty-three in 1991 to 1993 and thirty-three in 2006 to 2008). There was no increase in the percentage of fractures treated in high-volume hospitals over time (57.7% in 1991 to 1993 and 57.1% in 2006 to 2008) and little reduction in the percentage of fractures treated in low-volume hospitals (5.8% in 1991 to 1993 and 5.5% in 2006 to 2008).
Conclusions:
There has been little change in the trends of operative and nonoperative treatment for proximal femoral fractures over the last two decades, and there was little evidence of regionalization of hip fracture treatment to higher-volume hospitals.
Femoral neck fractures are a common injury in the elderly population and typically require hospitalization and surgical intervention. The decision regarding the specific treatment of an individual patient is multifactorial and complex. There are surgical and nonsurgical options depending on the fracture characteristics, the overall health of the patient, the patient’s pre-fracture mobility, and the discretion of the treating surgeon.
Surgical options for the treatment of a proximal femoral fracture include internal fixation, hemiarthroplasty, and total hip arthroplasty. Earlier literature demonstrated the superiority of replacement rather than fixation in the treatment of displaced fractures in elderly patients1-8. Although most studies have suggested improved functional outcomes with total hip arthroplasty when compared with hemiarthroplasty9-19, others have found less benefit20,21. Thus, in clinical practice, the treatment of hip fractures continues to depend upon shared decision-making involving discussion among the patient, the patient’s family, and the orthopaedic surgeon. Nonsurgical management remains reserved primarily for those patients who are deemed unfit for surgery because of excessive medical comorbidity.
The treatment of hip fractures has increased importance because of the very high mortality and morbidity associated with this injury. Available data suggest that one-year mortality rates approach 30% and that 25% of patients who survive a hip fracture will require long-term nursing home placement22-24. A higher individual surgeon volume has been associated with a reduction in complications, length of hospital stay, and mortality25,26. A similar association between increasing hospital volume and superior outcomes after hip fractures has not been established, despite the intuitive appeal of such reasoning27-33.
Our primary objective was to evaluate the general trends in surgical and nonsurgical management of femoral neck fractures to examine how treatment might be changing over time. We were interested both in the setting of treatment (high or low-volume centers, rural or urban hospitals, and teaching or nonteaching hospitals) and the proportions of the specific treatment (total hip arthroplasty, hemiarthroplasty, internal fixation, or no surgery) that was chosen. Our secondary objective was to determine if there has been evidence of regionalization in hip fracture treatment to higher-volume centers over time. We anticipated that we would find that patients managed at teaching hospitals, urban hospitals, and high-volume hospitals would be more likely to undergo a total hip arthroplasty, and there would be an increasing tendency for hip fractures to be treated at high-volume centers over time.
Materials and Methods
We used Medicare Provider Analysis and Review (MedPAR) Part A data files to identify fee-for-service beneficiaries who had sustained a closed, transcervical fracture of the femoral neck (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] diagnosis code 820.0x) from January 1, 1991, to December 31, 2008. We did not include fractures at the base of the femoral neck (ICD-9-CM code 820.03) as their treatment is different from that of transcervical femoral neck fractures. We extracted an array of information from the MedPAR files including patient demographic characteristics (age, race, and sex), patient comorbidities, ICD-9-CM codes for diagnoses and procedures, zip code of the patient’s residence, each patient’s unique Medicare beneficiary number, hospital characteristics, and the unique hospital identification number. Comorbid conditions were identified with use of algorithms described by Elixhauser et al.34. We further stratified the number of comorbidities as none, one to two, three to four, and five or more for the purposes of analysis.
We excluded several populations from our analysis including patients with fracture who were younger than sixty-five years, as they are not representative of the general Medicare population, and patients with incomplete demographic data (e.g., missing age, race, or sex).
All patients with hip fracture were stratified into one of four treatment groups based upon ICD-9-CM procedure codes: total hip arthroplasty (81.51), hemiarthroplasty (81.52), internal fixation (79.15, 79.35, 78.55), and none (patients lacking a procedure code associated with their admission were considered nonoperative). Patients managed with a procedure related to the femur other than the three specified above were excluded from the analysis (see Appendix). Our final sample included 1,162,301 patients with a diagnosis of a closed femoral neck fracture from 1991 to 2008.
Hospital Characteristics
We divided our eighteen-year period of investigation into six three-year blocks. In each three-year time interval, we stratified hospitals that treated at least one hip fracture into quartiles by the number of hip fractures treated. Our hospitals of interest were those in the highest and lowest quartiles. The highest quartile represents high-volume hospitals and the lowest quartile represents low-volume hospitals.
We linked the MedPAR data to the American Hospital Association (AHA) annual survey data. The AHA provides hospital-level information such as bed number, teaching status, nurse staffing level, and hospital zip code. We also linked the MedPAR data with the Rural-Urban Commuting Area (RUCA) classification system, which provides a means to classify patient residence and hospital location into rural and urban areas. Specifically, we used the codes recommended by the RUCA web site corresponding to 4.0, 5.0, 6.0, 7.0, 7.2, 7.3, 7.4, 8.0, 8.2, 8.3, 8.4, 9.0, 9.1, 9.2, 10.0, 10.2, 10.3, 10.4, and 10.5 for rural zip codes and 1.0, 1.1, 2.0, 2.1, 2.2, 4.1, 5.1, 7.1, 8.1, and 10.1 for urban zip codes35. The RUCA system has been utilized in previous investigations23,36.
Additionally, we classified the hospitals as major teaching, minor teaching, or nonteaching. A major teaching hospital was considered any hospital that is a member of the Council of Teaching Hospitals and Health Systems37. If a hospital is not a member of the Council of Teaching Hospitals and Health Systems, but does have a residency program affiliated with it, it was considered a minor teaching hospital. Hospitals that do not have any medical training program affiliation were categorized as nonteaching.
Statistical Analyses
We used bivariate methods (t test and chi-square test) to compare the characteristics of patients with hip fracture over the study period. In particular, we compared patient demographic characteristics and comorbidities during each of the three-year study increments to explore how patients with hip fracture have changed over time. We then used similar methods to compare the trends in management between the different three-year intervals. Next, we applied these methods to investigate any changes in hip fracture volume at the hospital level over the same time period. All statistical analyses were performed with use of SAS Version 9.2.3 (SAS Institute, Cary, North Carolina). This study was approved by our institutional review board.
Source of Funding
This work was funded in part by a grant (R01 HL085347) from the National Heart, Lung, and Blood Institute (NHLBI) and a grant (R01 AG033035) from the National Institute on Aging (NIA) at the National Institutes of Health (NIH). One author (P.C.) was supported by the Department of Veterans Affairs and by an award (K24 AR062133) from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) at the NIH. One author (B.J.M.) was supported by a T32 training grant (CA148062-01) from the NIH. Funds from all sources were used for salaries.
Results
Given the large sample size, there were significant differences in many patient demographic characteristics over time (see Appendix). The most striking are the increase in the prevalence of diabetes, heart failure, obesity, and renal failure and the mean number of comorbidities per patient within the time period of our investigation. The annual volume of procedures to treat hip fractures peaked in the mid-1990s before steadily declining in subsequent years (Fig. 1). The mean hospital volume for each of the four treatment modalities remained relatively stable over the study period (Fig. 2), reflecting both the reduction in hip fractures over time and also the gradual reduction in the number of hospitals treating hip fractures.
Fig. 1.
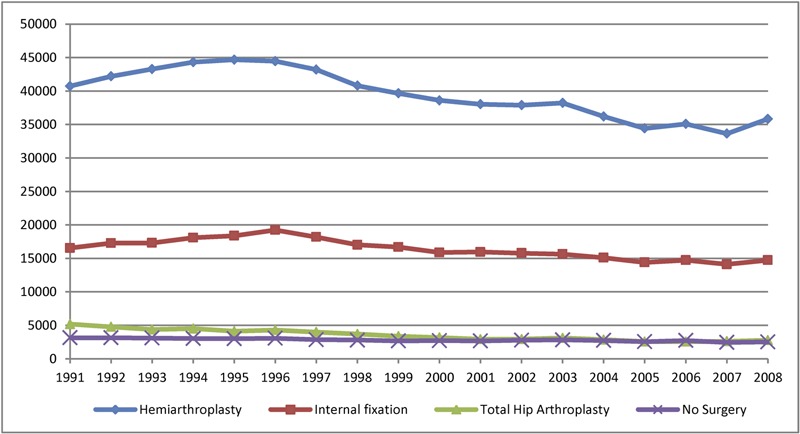
Line graph showing the national volumes of internal fixation, hemiarthroplasty, total hip arthroplasty, and no surgery in the Medicare population from 1991 to 2008.
Fig. 2.
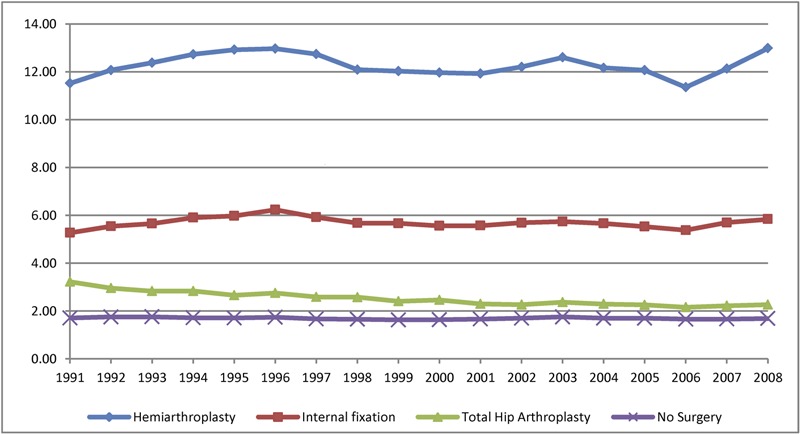
Line graph showing the mean hospital volume for internal fixation, hemiarthroplasty, total hip arthroplasty, and no surgery in the Medicare population from 1991 to 2008.
Viewed from a somewhat different perspective, the percentage of hip fractures treated with each of the four therapeutic options remained relatively constant over time (Fig. 3). The most common surgical procedure was a hemiarthroplasty, accounting for 62.8% of all hip fracture treatment in 1991 to 1993 and 63.9% of all hip fracture treatment in 2006 to 2008 (p < 0.001). After an initial decline in utilization, the proportion of total hip arthroplasty remained steady without indication of a recent increase, with 7.1% of all hip fracture treatment in 1991 to 1993 and 4.8% of all hip fracture treatment in 2006 to 2008 (p < 0.001). A subgroup analysis of major teaching hospitals, rural hospitals, and high and low-volume hospitals further details these trends (see Appendix). Of note is the increase in proportion of total hip arthroplasty at major teaching hospitals in the last time period (2006 to 2008). This is the only hospital-based subgroup we analyzed that showed a recent increase in utilization. We found that the proportion of total hip arthroplasty is also rising in patients with no recorded comorbidities (5.8% in 2003 to 2005 to 6.4% in 2006 to 2008) (see Appendix).
Fig. 3.
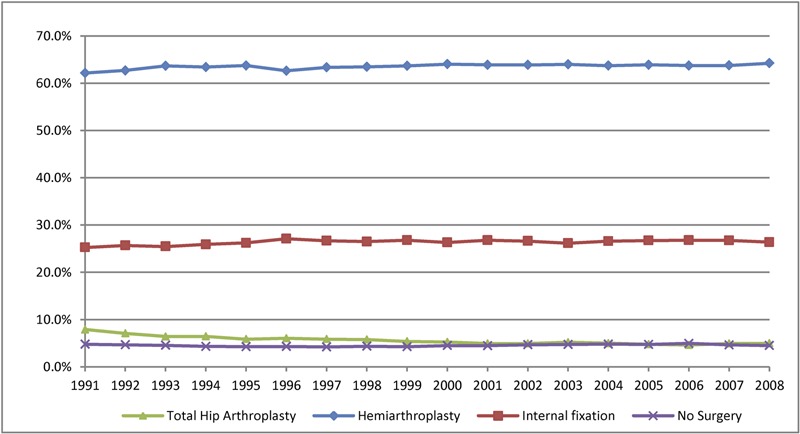
Line graph showing the percentage of hip fractures treated with internal fixation, hemiarthroplasty, total hip arthroplasty, and no surgery in the Medicare population from 1991 to 2008.
The mean and median hospital fracture volumes remained largely unchanged over the study period (see Appendix). The median number of fractures treated ranged from twelve to fourteen per year, with an average of thirteen per year in the period 1991 to 1993 and in the period 2006 to 2008. The lowest quartile contained hospitals treating six fractures or less annually, and the highest quartile contained hospitals treating twenty-three fractures or more annually. The total number of hospitals treating hip fractures steadily decreased over time (4208 from 1991 to 1993 and 3540 from 2006 to 2008); this reduction is largely a reflection of an overall reduction in the number of acute care hospitals in the United States over time (5720 from 1991 to 1993 and 5130 from 2006 to 2008). A number of hospitals (5.4% in 1991 to 1993 and 4.5% in 2006 to 2008) did treat at least one hip fracture, but did not treat any of them operatively.
The proportion of hip fractures treated at high-volume centers remained relatively constant throughout the study period (Fig. 4). In 1991 to 1993, 57.7% of fractures were treated in high-volume centers, and in 2006 to 2008, 57.1% were treated in high-volume centers (p < 0.001). In the same time period, low-volume centers demonstrated a subtle decrease in the relative utilization of total hip arthroplasty, although the overall trend was stable. The most important discrepancy is the percentage of hip fractures treated nonsurgically in low-volume hospitals (8.7% in 1991 to 1993 and 9.2% in 2006 to 2008) compared with high-volume hospitals (3.7% in 1991 to 1993 and 3.7% in 2006 to 2008). This gap is accounted for by a greater percentage of hemiarthroplasty done at high-volume centers (Fig. 5). The proportions of internal fixation and total hip arthroplasty were similar between low and high-volume hospitals.
Fig. 4.
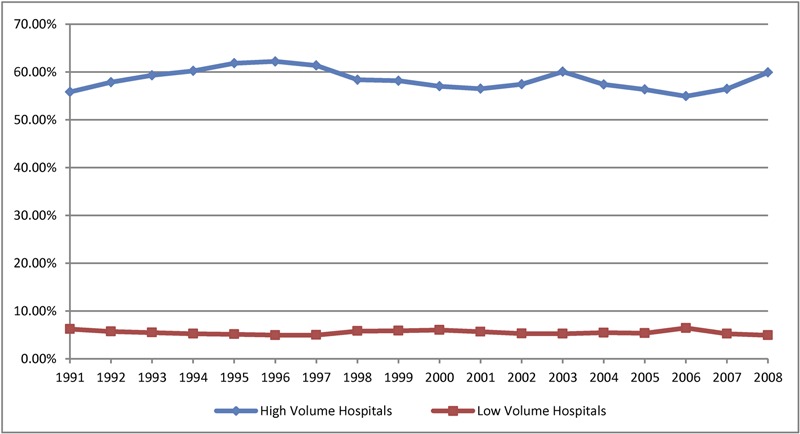
Line graph showing the percentage of all hip fractures treated in high and low-volume hospitals in the Medicare population from 1991 to 2008.
Fig. 5.
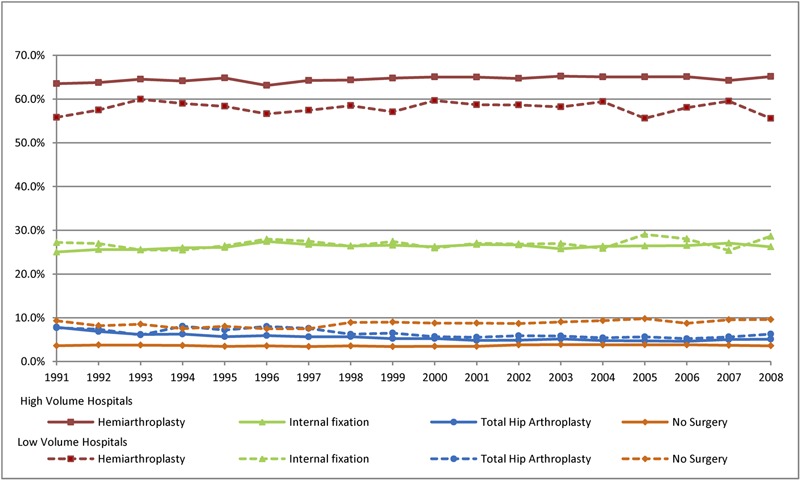
Line graph showing the percentage of hip fracture admissions treated with internal fixation, hemiarthroplasty, total hip arthroplasty, and no surgery in high and low-volume hospitals in the Medicare population from 1991 to 2008.
Discussion
In an investigation of treatment of femoral neck fractures in the Medicare population from 1991 to 2008, we found surprisingly little change in surgical treatment over time. Specifically, we found little change in the proportion of patients with hip fracture managed with four different modalities: internal fixation, hemiarthroplasty, total hip arthroplasty, and no surgery. We also found little difference in hip fracture treatment in high and low-volume hospitals, in rural and urban hospitals, and in teaching and nonteaching hospitals. Finally, we found little evidence for the regionalization of hip fracture surgery to higher-volume centers. In aggregate, our findings were somewhat unexpected given the advances in orthopaedic knowledge during this period of time.
Our finding of little change in the proportion of patients with fracture managed with internal fixation, hemiarthroplasty, total hip arthroplasty, and no surgery over time is important and extends prior research. A previous study by Jain et al. examined trends in the surgical treatment of hip fractures from 1990 to 200138. Surprisingly, the investigators found a decrease in total hip arthroplasty utilization during their study period, but hypothesized that the trend of declining total hip arthroplasty utilization could reverse, and that utilization of total hip arthroplasty would increase in future years as more comparative studies showing the benefits of total hip arthroplasty over hemiarthroplasty were completed. We extended their work to include more contemporary data, but again found no evidence of increased use of total hip arthroplasty for hip fracture treatment. This result is particularly interesting given a number of recent studies that have suggested that total hip arthroplasty may produce better hip fracture outcomes compared with hemiarthroplasty9-16,19. One potential explanation is that surgeons are not choosing total hip arthroplasty for hip fracture because they remain skeptical of the generalizability of the published studies to their patients. For instance, the finding that the proportion of total hip arthroplasty is increasing only in patients without recorded comorbidities may reflect a general acceptance that total hip replacement may be a superior procedure for only the healthiest patients. Alternatively, it is possible that surgeons are choosing to forego total hip arthroplasty because the surgery is typically more complicated and has greater risks of complications than hemiarthroplasty. Yet another potential explanation is that patients and their families are less interested in a more complex surgery with increased risks despite the potential benefits that total hip arthroplasty may afford. Finally, as we were limited to patients over sixty-five years of age, it is possible that an increase in total hip arthroplasty is present in younger patients not represented in this cohort. Each of these possibilities warrants further exploration.
Our finding of little difference in hip fracture treatment in high and low-volume centers is also interesting. We expected that higher-volume centers would be better prepared for the complexities of surgery and postoperative complications and thus would manage a higher proportion of their patients with hip fracture with total hip arthroplasty, but we did not find this. We did find some evidence that a higher proportion of patients were managed nonoperatively in lower-volume centers. We can envision a number of potential explanations for this finding. First, low-volume centers may be less likely to have the multidisciplinary teams of surgeons, anesthesiologists, geriatricians, and other subspecialists necessary to manage patients with high-risk fracture and thus might be reluctant to operate. Second, it is likely that many patients with fracture in low-volume hospitals who are good surgical candidates would be transferred to higher-volume centers for surgery; thus, the subsample of patients with hip fracture who gain admission to low-volume hospitals are likely to represent an extremely high-risk pool as many better operative candidates are likely to be transferred to a higher-volume referral center directly from the emergency department prior to admission. Our analysis focused on patients with hip fracture admitted to an acute care hospital and did not allow us to examine pre-hospital triage decisions.
We also examined whether there might be differences in hip fracture treatments when hospitals were stratified according to teaching status or geographic location. We thought that rural hospitals might have greater difficulty in obtaining orthopaedic surgeon coverage and would likely lack experienced orthopaedic trauma surgeons and that this might, in turn, influence surgical treatment. Concerns with limitations to access and quality of specialty care in rural settings have been raised in other medical conditions39-42. In actuality, the differences in treatment in urban and rural hospitals that we observed were minimal. We also hypothesized that major teaching hospitals, with their intellectual environment, multidisciplinary teams, and training programs, might be more likely to treat hip fractures in accordance with the most recent literature and guidelines. Although we observed slightly greater use of total hip arthroplasty in major teaching hospitals during the last three years of our study, the differences in hip fracture treatment across teaching and nonteaching hospitals were small.
Over the past two decades, substantial evidence has accumulated for improved patient outcomes and standardization of care in hospitals with higher volumes for an array of conditions and procedures including cardiovascular disease43-45, cancer43,46,47, and total joint replacement48-52. There is evidence that elective joint replacement has increasingly regionalized in recent years, potentially in response to a perception of increased quality at high-volume centers53. However, data for hip fractures have not conclusively demonstrated improved outcomes for high-volume hospitals27-29,31,33. Interestingly, high individual surgeon volume of hip fractures appears to benefit independently from hospital volume25-28,54. In fact, Birkmeyer et al. suggested that surgeon volume, rather than hospital volume, is of primary importance in optimizing mortality in a number of surgical procedures55.
The potential reasons for this lack of regionalization of hip fracture treatment are likely complex. It is possible that patients with hip fractures (and their families) prefer to be managed locally, thus hindering any efforts to concentrate care in high-volume centers. Alternatively, surgeons and emergency room physicians may view hip fractures as a general orthopaedic condition in the elderly that does not benefit from treatment at large, tertiary-care, referral hospitals. Finally, it is possible that our finding of a lack of regionalization to high-volume hospitals overlooks concentration of hip fracture treatment among high-volume surgeons; our lack of individual physician-level data precluded us from examining this issue. Regardless, the absence of regionalization of hip fractures can be partially explained and can be justified by the lack of solid evidence demonstrating a clear benefit to treatment in a high-volume center.
We had numerous additional findings that are interesting and warrant brief mention. First, the trend of increasing patient comorbidity over time has been noted in prior longitudinal studies22,56-59. Both Medicare reimbursement policy and increased attention to risk-adjusted outcomes provided strong incentive to exhaustively code all medical comorbidities and likely played a partial role in the increased comorbidity that we observed. However, there is strong evidence that the actual prevalence of diabetes and obesity is increasing and thus not all of the increased prevalence of comorbidities is merely an artifact of coding60-62. Next, we found a decreasing incidence in the total number of hip fractures, which is consistent with previous studies22,63. These reports suggest that this observation is multifactorial and may be due to increasing use of bisphosphonates, lifestyle changes, and public health awareness resulting in fewer fractures22. We also determined that the number of hospitals steadily decreased over our study period. The explanation for this result is likely complex, but is due in part to a high number of hospital mergers and consolidations64.
Our study had several limitations. First, our sample was limited to Medicare beneficiaries, and generalization to the non-Medicare population should be done with care. However, hip fractures are a common orthopaedic injury in the elderly, making the Medicare population an appropriate place for studying this injury. Second, our study relied upon administrative data and we lacked detailed clinical data on patient comorbidity and fracture pathology that may have influenced management decisions. For example, we were not able to distinguish between displaced and nondisplaced femoral neck fractures. Likewise, our reliance upon administrative data precluded us from studying patient and provider decision-making and the factors that led to a particular management decision in a given patient; this is clearly an area for future research. Third, our study did not include enrollees in Medicare managed care plans. Lastly, our study focused on patients hospitalized with hip fractures and we did not evaluate the pre-hospitalization triage or emergency department triage.
In summary, the treatment of femoral neck fractures changed very little during the eighteen-year period of this study and that treatment was largely similar across different groups of hospitals. We also found little evidence of regionalization of hip fracture surgery to higher-volume hospitals. In aggregate, our study highlights the need for continued efforts to compare the medical and functional outcome of hemiarthroplasty and total hip arthroplasty for the treatment of hip fracture.
Appendix
Tables showing the characteristics of Medicare beneficiaries with hip fracture from 1991 to 2008; hip fracture treatment in teaching hospitals, rural hospitals, and high and low-volume hospitals; hip fractures treated with total hip arthroplasty in the Medicare population from 1991 to 2008; and characteristics of U.S. acute care hospitals managing patients with hip fracture from 1991 to 2008; and a figure showing a flowchart of the study cohort generation are available with the online version of this article as a data supplement at jbjs.org.
Supplementary Material
Disclosure of Potential Conflicts of Interest
Tables showing the characteristics of Medicare beneficiaries with hip fracture from 1991 to 2008; hip fracture treatment in teaching hospitals, rural hospitals, and high and low-volume hospitals; hip fractures treated with total hip arthroplasty in the Medicare population from 1991 to 2008; and characteristics of U.S. acute care hospitals managing patients with hip fracture from 1991 to 2008; and a figure showing a flowchart of the study cohort generation
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Bhandari M, Devereaux PJ, Swiontkowski MF, Tornetta P, 3rd, Obremskey W, Koval KJ, Nork S, Sprague S, Schemitsch EH, Guyatt GH. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck. A meta-analysis. J Bone Joint Surg Am. 2003 Sep;85(9):1673-81 [DOI] [PubMed] [Google Scholar]
- 2.Bhandari M, Devereaux PJ, Tornetta P, 3rd, Swiontkowski MF, Berry DJ, Haidukewych G, Schemitsch EH, Hanson BP, Koval K, Dirschl D, Leece P, Keel M, Petrisor B, Heetveld M, Guyatt GH. Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone Joint Surg Am. 2005 Sep;87(9):2122-30 [DOI] [PubMed] [Google Scholar]
- 3.Blomfeldt R, Törnkvist H, Ponzer S, Söderqvist A, Tidermark J. Comparison of internal fixation with total hip replacement for displaced femoral neck fractures. Randomized, controlled trial performed at four years. J Bone Joint Surg Am. 2005 Aug;87(8):1680-8 [DOI] [PubMed] [Google Scholar]
- 4.Healy WL, Iorio R. Total hip arthroplasty: optimal treatment for displaced femoral neck fractures in elderly patients. Clin Orthop Relat Res. 2004 Dec;(429):43-8 [PubMed] [Google Scholar]
- 5.Johansson T, Jacobsson SA, Ivarsson I, Knutsson A, Wahlström O. Internal fixation versus total hip arthroplasty in the treatment of displaced femoral neck fractures: a prospective randomized study of 100 hips. Acta Orthop Scand. 2000 Dec;71(6):597-602 [DOI] [PubMed] [Google Scholar]
- 6.Leonardsson O, Sernbo I, Carlsson A, Akesson K, Rogmark C. Long-term follow-up of replacement compared with internal fixation for displaced femoral neck fractures: results at ten years in a randomised study of 450 patients. J Bone Joint Surg Br. 2010 Mar;92(3):406-12 [DOI] [PubMed] [Google Scholar]
- 7.Rogmark C, Carlsson A, Johnell O, Sernbo I. A prospective randomised trial of internal fixation versus arthroplasty for displaced fractures of the neck of the femur. Functional outcome for 450 patients at two years. J Bone Joint Surg Br. 2002 Mar;84(2):183-8 [DOI] [PubMed] [Google Scholar]
- 8.Tidermark J, Ponzer S, Svensson O, Söderqvist A, Törnkvist H. Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly. A randomised, controlled trial. J Bone Joint Surg Br. 2003 Apr;85(3):380-8 [DOI] [PubMed] [Google Scholar]
- 9.Goh SK, Samuel M, Su DH, Chan ES, Yeo SJ. Meta-analysis comparing total hip arthroplasty with hemiarthroplasty in the treatment of displaced neck of femur fracture. J Arthroplasty. 2009 Apr;24(3):400-6 Epub 2008 Aug 12 [DOI] [PubMed] [Google Scholar]
- 10.Parker MJ, Gurusamy KS, Azegami S. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev. 2010;(6):CD001706 Epub 2010 Jun 16 [DOI] [PubMed] [Google Scholar]
- 11.Avery PP, Baker RP, Walton MJ, Rooker JC, Squires B, Gargan MF, Bannister GC. Total hip replacement and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck: a seven- to ten-year follow-up report of a prospective randomised controlled trial. J Bone Joint Surg Br. 2011 Aug;93(8):1045-8 [DOI] [PubMed] [Google Scholar]
- 12.Baker RP, Squires B, Gargan MF, Bannister GC. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J Bone Joint Surg Am. 2006 Dec;88(12):2583-9 [DOI] [PubMed] [Google Scholar]
- 13.Blomfeldt R, Törnkvist H, Eriksson K, Söderqvist A, Ponzer S, Tidermark J. A randomised controlled trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. J Bone Joint Surg Br. 2007 Feb;89(2):160-5 [DOI] [PubMed] [Google Scholar]
- 14.Hedbeck CJ, Enocson A, Lapidus G, Blomfeldt R, Törnkvist H, Ponzer S, Tidermark J. Comparison of bipolar hemiarthroplasty with total hip arthroplasty for displaced femoral neck fractures: a concise four-year follow-up of a randomized trial. J Bone Joint Surg Am. 2011 Mar 2;93(5):445-50 [DOI] [PubMed] [Google Scholar]
- 15.Keating JF, Grant A, Masson M, Scott NW, Forbes JF. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty. Treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am. 2006 Feb;88(2):249-60 [DOI] [PubMed] [Google Scholar]
- 16.Macaulay W, Nellans KW, Garvin KL, Iorio R, Healy WL, Rosenwasser MP; other members of the DFACTO Consortium Prospective randomized clinical trial comparing hemiarthroplasty to total hip arthroplasty in the treatment of displaced femoral neck fractures: winner of the Dorr Award. J Arthroplasty. 2008 Sep;23(6)(Suppl 1):2-8 [DOI] [PubMed] [Google Scholar]
- 17.Ravikumar KJ, Marsh G. Internal fixation versus hemiarthroplasty versus total hip arthroplasty for displaced subcapital fractures of femur—13 year results of a prospective randomised study. Injury. 2000 Dec;31(10):793-7 [DOI] [PubMed] [Google Scholar]
- 18.Dorr LD, Glousman R, Hoy AL, Vanis R, Chandler R. Treatment of femoral neck fractures with total hip replacement versus cemented and noncemented hemiarthroplasty. J Arthroplasty. 1986;1(1):21-8 [DOI] [PubMed] [Google Scholar]
- 19.Zi-Sheng A, You-Shui G, Zhi-Zhen J, Ting Y, Chang-Qing Z. Hemiarthroplasty vs primary total hip arthroplasty for displaced fractures of the femoral neck in the elderly: a meta-analysis. J Arthroplasty. 2012 Apr;27(4):583-90 Epub 2011 Sep 15 [DOI] [PubMed] [Google Scholar]
- 20.Kannan A, Kancherla R, McMahon S, Hawdon G, Soral A, Malhotra R. Arthroplasty options in femoral-neck fracture: answers from the national registries. Int Orthop. 2012 Jan;36(1):1-8 Epub 2011 Sep 20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van den Bekerom MP, Hilverdink EF, Sierevelt IN, Reuling EM, Schnater JM, Bonke H, Goslings JC, van Dijk CN, Raaymakers EL. A comparison of hemiarthroplasty with total hip replacement for displaced intracapsular fracture of the femoral neck: a randomised controlled multicentre trial in patients aged 70 years and over. J Bone Joint Surg Br. 2010 Oct;92(10):1422-8 [DOI] [PubMed] [Google Scholar]
- 22.Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009 Oct 14;302(14):1573-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miller BJ, Cai X, Cram P. Mortality rates are similar after hip fractures for rural and urban patients. Clin Orthop Relat Res. 2012 Jun;470(6):1763-70 Epub 2011 Oct 21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vochteloo AJ, van Vliet-Koppert ST, Maier AB, Tuinebreijer WE, Röling ML, de Vries MR, Bloem RM, Nelissen RG, Pilot P. Risk factors for failure to return to the pre-fracture place of residence after hip fracture: a prospective longitudinal study of 444 patients. Arch Orthop Trauma Surg. 2012 Jun;132(6):823-30 Epub 2012 Feb 7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ames JB, Lurie JD, Tomek IM, Zhou W, Koval KJ. Does surgeon volume for total hip arthroplasty affect outcomes after hemiarthroplasty for femoral neck fracture? Am J Orthop (Belle Mead NJ). 2010 Aug;39(8):E84-9 [PubMed] [Google Scholar]
- 26.Lavernia CJ. Hemiarthroplasty in hip fracture care: effects of surgical volume on short-term outcome. J Arthroplasty. 1998 Oct;13(7):774-8 [DOI] [PubMed] [Google Scholar]
- 27.Battaglia TC, Mulhall KJ, Brown TE, Saleh KJ. Increased surgical volume is associated with lower THA dislocation rates. Clin Orthop Relat Res. 2006 Jun;447:28-33 [DOI] [PubMed] [Google Scholar]
- 28.Browne JA, Pietrobon R, Olson SA. Hip fracture outcomes: does surgeon or hospital volume really matter? J Trauma. 2009 Mar;66(3):809-14 [DOI] [PubMed] [Google Scholar]
- 29.Forte ML, Virnig BA, Swiontkowski MF, Bhandari M, Feldman R, Eberly LE, Kane RL. Ninety-day mortality after intertrochanteric hip fracture: does provider volume matter? J Bone Joint Surg Am. 2010 Apr;92(4):799-806 [DOI] [PubMed] [Google Scholar]
- 30.Gandjour A, Weyler EJ. Cost-effectiveness of referrals to high-volume hospitals: an analysis based on a probabilistic Markov model for hip fracture surgeries. Health Care Manag Sci. 2006 Nov;9(4):359-69 [DOI] [PubMed] [Google Scholar]
- 31.Hamilton BH, Ho V. Does practice make perfect? Examining the relationship between hospital surgical volume and outcomes for hip fracture patients in Quebec. Med Care. 1998 Jun;36(6):892-903 [DOI] [PubMed] [Google Scholar]
- 32.Shah SN, Wainess RM, Karunakar MA. Hemiarthroplasty for femoral neck fracture in the elderly surgeon and hospital volume-related outcomes. J Arthroplasty. 2005 Jun;20(4):503-8 [DOI] [PubMed] [Google Scholar]
- 33.Sund R. Modeling the volume-effectiveness relationship in the case of hip fracture treatment in Finland. BMC Health Serv Res. 2010;10:238 Epub 2010 Aug 13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998 Jan;36(1):8-27 [DOI] [PubMed] [Google Scholar]
- 35.WWAMI Rural Health Research Center. Rural-urban commuting area codes (RUCAs) http://depts.washington.edu/uwruca. Accessed 2011 Jan 26.
- 36.Abrams TE, Vaughan-Sarrazin M, Kaboli PJ. Mortality and revascularization following admission for acute myocardial infarction: implication for rural veterans. J Rural Health. 2010 Fall;26(4):310-7 Epub 2010 Aug 17 [DOI] [PubMed] [Google Scholar]
- 37.Allison JJ, Kiefe CI, Weissman NW, Person SD, Rousculp M, Canto JG, Bae S, Williams OD, Farmer R, Centor RM. Relationship of hospital teaching status with quality of care and mortality for Medicare patients with acute MI. JAMA. 2000 Sep 13;284(10):1256-62 [DOI] [PubMed] [Google Scholar]
- 38.Jain NB, Losina E, Ward DM, Harris MB, Katz JN. Trends in surgical management of femoral neck fractures in the United States. Clin Orthop Relat Res. 2008 Dec;466(12):3116-22 Epub 2008 Jul 22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sheikh K, Bullock C. Urban-rural differences in the quality of care for Medicare patients with acute myocardial infarction. Arch Intern Med. 2001 Mar 12;161(5):737-43 [DOI] [PubMed] [Google Scholar]
- 40.MacDowell M, Glasser M, Fitts M, Nielsen K, Hunsaker M. A national view of rural health workforce issues in the USA. Rural Remote Health. 2010 Jul-Sep;10(3):1531 Epub 2010 Jul 26 [PMC free article] [PubMed] [Google Scholar]
- 41.Baldwin LM, Cai Y, Larson EH, Dobie SA, Wright GE, Goodman DC, Matthews B, Hart LG. Access to cancer services for rural colorectal cancer patients. J Rural Health. 2008 Fall;24(4):390-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baldwin LM, MacLehose RF, Hart LG, Beaver SK, Every N, Chan L. Quality of care for acute myocardial infarction in rural and urban US hospitals. J Rural Health. 2004 Spring;20(2):99-108 [DOI] [PubMed] [Google Scholar]
- 43.Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, Welch HG, Wennberg DE. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002 Apr 11;346(15):1128-37 [DOI] [PubMed] [Google Scholar]
- 44.Chen J, Krumholz HM, Wang Y, Curtis JP, Rathore SS, Ross JS, Normand SL, Schreiner GC, Mulvey G, Nallamothu BK. Differences in patient survival after acute myocardial infarction by hospital capability of performing percutaneous coronary intervention: implications for regionalization. Arch Intern Med. 2010 Mar 8;170(5):433-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jollis JG, Peterson ED, DeLong ER, Mark DB, Collins SR, Muhlbaier LH, Pryor DB. The relation between the volume of coronary angioplasty procedures at hospitals treating Medicare beneficiaries and short-term mortality. N Engl J Med. 1994 Dec 15;331(24):1625-9 [DOI] [PubMed] [Google Scholar]
- 46.Birkmeyer JD, Sun Y, Wong SL, Stukel TA. Hospital volume and late survival after cancer surgery. Ann Surg. 2007 May;245(5):777-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011 Jun 2;364(22):2128-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jain N, Pietrobon R, Hocker S, Guller U, Shankar A, Higgins LD. The relationship between surgeon and hospital volume and outcomes for shoulder arthroplasty. J Bone Joint Surg Am. 2004 Mar;86(3):496-505 [DOI] [PubMed] [Google Scholar]
- 49.Katz JN, Losina E, Barrett J, Phillips CB, Mahomed NN, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States Medicare population. J Bone Joint Surg Am. 2001 Nov;83(11):1622-9 [DOI] [PubMed] [Google Scholar]
- 50.Katz JN, Phillips CB, Baron JA, Fossel AH, Mahomed NN, Barrett J, Lingard EA, Harris WH, Poss R, Lew RA, Guadagnoli E, Wright EA, Losina E. Association of hospital and surgeon volume of total hip replacement with functional status and satisfaction three years following surgery. Arthritis Rheum. 2003 Feb;48(2):560-8 [DOI] [PubMed] [Google Scholar]
- 51.Shervin N, Rubash HE, Katz JN. Orthopaedic procedure volume and patient outcomes: a systematic literature review. Clin Orthop Relat Res. 2007 Apr;457:35-41 [DOI] [PubMed] [Google Scholar]
- 52.Soohoo NF, Farng E, Lieberman JR, Chambers L, Zingmond DS. Factors that predict short-term complication rates after total hip arthroplasty. Clin Orthop Relat Res. 2010 Sep;468(9):2363-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cram P, Lu X, Callaghan JJ, Vaughan-Sarrazin MS, Cai X, Li Y. Long-term trends in hip arthroplasty use and volume. J Arthroplasty. 2012 Feb;27(2):278: e2. Epub 2011 Jul 12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kreder HJ, Deyo RA, Koepsell T, Swiontkowski MF, Kreuter W. Relationship between the volume of total hip replacements performed by providers and the rates of postoperative complications in the state of Washington. J Bone Joint Surg Am. 1997 Apr;79(4):485-94 [DOI] [PubMed] [Google Scholar]
- 55.Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003 Nov 27;349(22):2117-27 [DOI] [PubMed] [Google Scholar]
- 56.Preyra C. Coding response to a case-mix measurement system based on multiple diagnoses. Health Serv Res. 2004 Aug;39(4 Pt 1):1027-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lindenauer PK, Lagu T, Shieh MS, Pekow PS, Rothberg MB. Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003-2009. JAMA. 2012 Apr 4;307(13):1405-13 [DOI] [PubMed] [Google Scholar]
- 58.Goldfarb MG, Coffey RM. Change in the Medicare case-mix index in the 1980s and the effect of the prospective payment system. Health Serv Res. 1992 Aug;27(3):385-415 [PMC free article] [PubMed] [Google Scholar]
- 59.Doremus HD, Michenzi EM. Data quality. An illustration of its potential impact upon a diagnosis-related group’s case mix index and reimbursement. Med Care. 1983 Oct;21(10):1001-11 [PubMed] [Google Scholar]
- 60.Urbano FL, Pascual RM. Contemporary issues in the care of patients with chronic obstructive pulmonary disease. J Manag Care Pharm. 2005 Jun;11(5)(Suppl A):S2-13, quiz:S14-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Maynard G, O’Malley CW, Kirsh SR. Perioperative care of the geriatric patient with diabetes or hyperglycemia. Clin Geriatr Med. 2008 Nov;24(4):649-65: viii [DOI] [PubMed] [Google Scholar]
- 62.Linjakumpu T, Hartikainen S, Klaukka T, Veijola J, Kivelä SL, Isoaho R. Use of medications and polypharmacy are increasing among the elderly. J Clin Epidemiol. 2002 Aug;55(8):809-17 [DOI] [PubMed] [Google Scholar]
- 63.Gehlbach SH, Avrunin JS, Puleo E. Trends in hospital care for hip fractures. Osteoporos Int. 2007 May;18(5):585-91 Epub 2006 Dec 5 [DOI] [PubMed] [Google Scholar]
- 64.Cuellar AE, Gertler PJ. Trends in hospital consolidation: the formation of local systems. Health Aff (Millwood). 2003 Nov-Dec;22(6):77-87 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest
Tables showing the characteristics of Medicare beneficiaries with hip fracture from 1991 to 2008; hip fracture treatment in teaching hospitals, rural hospitals, and high and low-volume hospitals; hip fractures treated with total hip arthroplasty in the Medicare population from 1991 to 2008; and characteristics of U.S. acute care hospitals managing patients with hip fracture from 1991 to 2008; and a figure showing a flowchart of the study cohort generation


