Abstract
Background:
Venous ulcers are wounds that are thought to occur due to improper functioning of venous valves, usually of the legs. They are the major cause of chronic wounds, occurring in 70% to 90% of chronic wound cases. The treatment of venous ulcers also entails substantial costs. Autologous platelet rich plasma (PRP) is a simple office based procedure which helps in enhancing the wound healing by releasing many growth factors like platelet derived growth factors, fibroblast derived growth factors and epidermal growth factors.
Aim:
To study the efficacy of autologous platelet rich plasma in the management of chronic venous ulcer.
Methodology:
12 patients with 17 venous ulcers were treated with PRP and treatment outcome was measured by percentage of improvement in area and volume of the ulcer.
Results:
12 patients with 17 ulcers were treated with PRP. The mean age of the patients was 33.5 years (SD 9.82). 10 were males and 2 were females. The mean duration of the healing of the ulcers was in 5.1 weeks (SD 3.1). The mean percentage improvement in the area and volume of the ulcer was 94.7% (SD 11.12) and 95.6% (SD 10.19) respectively.
Conclusions:
PRP is safe, simple and effective procedure in treating chronic venous ulcers
Keywords: Non healing, platelet rich plasma, venous ulcers
INTRODUCTION
Venous ulcers are the most common form of leg ulcers which has a significant impact on quality of life and work productivity. In addition, the costs associated with the long-term care of these chronic wounds are substantial.[1] Conventional therapies such as dressings, surgical debridement, compression bandage and even skin grafting cannot provide satisfactory healing since these treatments are not able to provide necessary growth factors that can modulate healing processes. Autologous platelet rich plasma (PRP) is a safe, simple, affordable and less expensive procedure in the treatment of chronic ulcers with reportedly good results. Since, it is an autologous method, it is biocompatible and safe.[2]
The aim of the study was to evaluate the efficacy of platelet rich plasma in the management of chronic venous ulcers. It was a non-randomized uncontrolled study.
MATERIALS AND METHODS
In the study, 12 patients with 17 ulcers were included with the following inclusion and exclusion criteria from January 2011 to June 2012. Ethical clearance was taken from ethics committee before the start of the study.
Inclusion criteria
Ulcers more than 6 weeks duration and patients who had received conventional therapies for at least 6 weeks.
Patients with a bleeding disorder, uncontrolled sugar levels and ulcers with active infection and saphenofemoral incompetency were excluded.
Procedure: Patients were thoroughly examined and ulcer size (length, breadth and depth) was measured. Venous doppler was carried out for all patients. 10 patients had perforator incompetency and 2 patients had superficial vein incompetency.
Under aseptic precautions 20 ml of venous blood was drawn and added to a test tube containing acid citrate dextrose in a ratio of 9:1 (blood: Acid citrate dextrose), centrifuged at 5000 rpm for 15 min to separate the red blood cells from the platelets and plasma. Then the supernatant and the buffy coat composed of platelets and plasma was collected and centrifuged again at 2000 rpm for 5-10 min. The bottom layer about 1.5 ml was taken and 10% calcium chloride was added (0.3 ml for 1 ml of PRP). The mean platelet count was 3.8 Lakhs/cumm (SD 0.95) and the mean final concentration of platelets in PRP was 6.05 Lakhs/cumm (SD 1.25). Thus the activated PRP was applied onto the wound after proper surgical debridement and was dressed with a non-absorbent dressing (paraffin gauze). This process was repeated once weekly for 6 weeks. At every week the ulcer area and volume was calculated and photographs were taken. Wound area was calculated using the formula for an ellipse: Length × width × 0.7854 (an ellipse is closer to a wound shape than a square or rectangle that would be described by simple length × width). The use of an ellipse for calculating wound measurement has been used in RCTs in wound healing literature.[3,4] Volume was calculated using the formula (length × width × 0.7854) × depth.[4]
The treatment outcome was defined as a percentage change of the area and volume, which was calculated as initial measurement minus assessment day measurement divided by initial measurement.
RESULTS
A total of 12 patients with 17 ulcers were treated with PRP. The mean age of the patients was 33.5 years (SD 9.82). 6 (50%) patients were in the age group 30–40 years, 4 (34%) between 20 years and 30 years, 1 (8%) between 50 years and 60 years and 1 (8%) < 20 years 10 (83.33%) were males and 2 (16.66%) were females. The duration of ulcer ranged from 2 months to 1 year with a mean of 5.35 months. The mean duration of the healing of the ulcers was in 5.1 weeks (SD 3.1). 100% improvement in the area of the ulcers was seen in 13 (76%) [Table 1]. 100% improvement in volume of the ulcer was seen in 14 (82%) [Table 2]. The baseline mean area of the ulcer was 10.08 cm2 (SD 6.91) and baseline volume was 6.45 cm3 (SD 5.35). The final area of the ulcer at the end of 6 weeks was 1.13 cm2 (SD 2.56) and final volume of the ulcer was 0.76 cm3 (SD 1.91). The mean percentage improvement in the area and volume of the ulcer was 94.7% (SD 11.12) and 95.6% (SD 10.19) respectively [Figures 1 and 2]. There were no side effects and there was a decrease in pain associated with the ulcers. The primary condition was treated by elevation of the foot at the night. Five patients had undergone sclerotherapy and three patients had undergone surgery for varicose veins with little improvement in the healing of ulcers. Patients were advised for compression therapy after healing of ulcers.
Table 1.
Improvement of the area of the ulcer in percentage at the end of 6th sitting
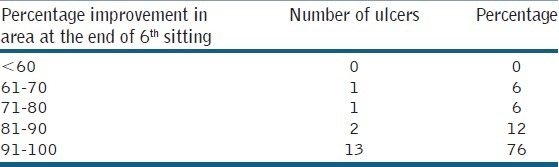
Table 2.
Improvement of volume in percentage at the end of 6th sitting
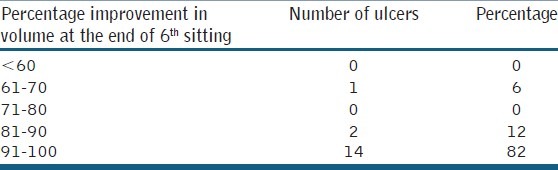
Figure 1.

(a) a patient of venous ulcer of duration 3 months, (b) after one sitting of platelet rich plasma, (c) ulcer at 4th week and (d) ulcer being healed at 6th week
Figure 2.
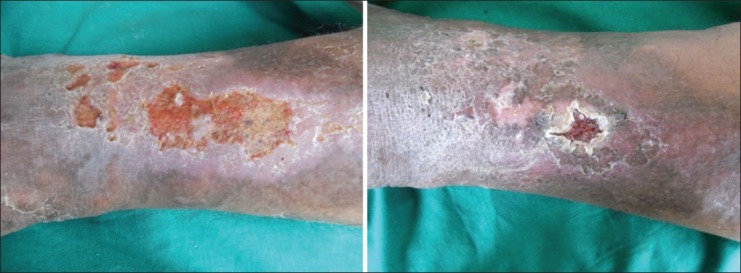
A patient with venous ulcer of 2 months duration healed at 5th week requiring four sittings of platelet rich plasma
DISCUSSION
Venous leg ulcers are responsible for more than half of lower extremity ulcerations, with overall prevalence ranging from 0.06% to 2%.[1] Multiple therapies have been proposed for their treatment. The most popular form of therapy for venous leg ulcers is virtually identical to the compression bandage introduced by Unna in 1885.[5] However, even though limb compression is considered to be standard care for venous leg ulcers, the use of lower-limb compression is not always feasible and successful.[6] The treatment of venous ulcers also entails substantial costs.
PRP is a volume of autologous plasma that has a platelet concentration above baseline i.e., five times more than normal platelet counts.[7]
PRP enhances wound healing by promoting the healing process by seven growth factors present in it. They are platelet derived growth factor (αα, αβ, αβ), fibroblast growth factor, vascular endothelial growth factor, epidermal growth factor, transforming growth factor. These growth factors are important in modulating mesenchymal cell recruitment, proliferation and extra-cellular matrix synthesis during the healing process.[8]
A study conducted by Frykberg et al. on 49 patients with 65 non healing ulcers showed that 63 of 65 ulcers responded with reduction in area, volume and undermining of the ulcers in a mean of 2.8 weeks with 3.2 treatments.[9] The mean percentage of volume and area reduction of venous ulcers were 56.1% (SD 35.2) and 43.1% (SD 32.4) with a mean of 2.3 weeks treatment time. In our study, the mean percentage of volume and area reduction was 95% (SD 10.2) and 94.14% (SD 11.18) with a mean of 5.1 weeks treatment.
CONCLUSION
Chronic venous leg ulcers come with cost and morbidity for patients and society also. PRP is a safe, simple, inexpensive and biocompatible procedure. In our study, PRP is found to be useful in enhancing the wound healing in chronic venous leg ulcers without any adverse events. Since, there is no standardization of the procedure, more randomized control studies are needed to make a standard protocol for the preparation of PRP.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Valencia IC, Falabella A, Kirsner RS, Eaglstein WH. Chronic venous insufficiency and venous leg ulceration. J Am Acad Dermatol. 2001;44:401–21. doi: 10.1067/mjd.2001.111633. [DOI] [PubMed] [Google Scholar]
- 2.Braund R, Hook S, Medlicott NJ. The role of topical growth factors in chronic wounds. Curr Drug Deliv. 2007;4:195–204. doi: 10.2174/156720107781023857. [DOI] [PubMed] [Google Scholar]
- 3.Margolis DJ, Kantor J, Berlin JA. Healing of diabetic neuropathic foot ulcers receiving standard treatment. A meta-analysis. Diabetes Care. 1999;22:692–5. doi: 10.2337/diacare.22.5.692. [DOI] [PubMed] [Google Scholar]
- 4.Blume PA, Walters J, Payne W, Ayala J, Lantis J. Comparison of negative pressure wound therapy using vacuum-assisted closure with advanced moist wound therapy in the treatment of diabetic foot ulcers: A multicenter randomized controlled trial. Diabetes Care. 2008;31:631–6. doi: 10.2337/dc07-2196. [DOI] [PubMed] [Google Scholar]
- 5.Milic DJ, Zivic SS, Bogdanovic DC, Karanovic ND, Golubovic ZV. Risk factors related to the failure of venous leg ulcers to heal with compression treatment. J Vasc Surg. 2009;49:1242–7. doi: 10.1016/j.jvs.2008.11.069. [DOI] [PubMed] [Google Scholar]
- 6.Margolis DJ, Cohen JH. Management of chronic venous leg ulcers: A literature-guided approach. Clin Dermatol. 1994;12:19–26. doi: 10.1016/0738-081x(94)90253-4. [DOI] [PubMed] [Google Scholar]
- 7.Marx RE. Platelet-rich plasma (PRP): What is PRP and what is not PRP? Implant Dent. 2001;10:225–8. doi: 10.1097/00008505-200110000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Singh RP, Marwaha N, Malhotra P, Dash S. Quality assessment of platelet concentrates prepared by platelet rich plasma-platelet concentrate, buffy coat poor-platelet concentrate (BC-PC) and apheresis-PC methods. Asian J Transfus Sci. 2009;3:86–94. doi: 10.4103/0973-6247.53882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frykberg RG, Driver VR, Carman D, Lucero B, Borris-Hale C, Fylling CP, et al. Chronic wounds treated with a physiologically relevant concentration of platelet-rich plasma gel: A prospective case series. Ostomy Wound Manage. 2010;56:36–44. [PubMed] [Google Scholar]


