Abstract
Considering high prevalence and the need to look for alternative medicine, essential hypertension was screened in light of Vata–Pitta Pradhana Rakta Pradoshaja Vikara as mentioned by Acharya Charaka. Comparing the etiological factors, symptomatology, and complications with Rakta Pradoshaja Vikara with that of essential hypertension, a striking similarity was revealed. To prove the practical approach of management of Vata–Pitta Pradhana Rakta Pradoshaja Vikara, a randomized open clinical trial on 33 uncomplicated subjects of essential hypertension was conducted. The subjects were allotted in two groups, viz. (Group A) Virechana group having 16 cases who underwent Virechana Karma by Trivrita, Aragvadha, Eranda Taila, and Draksha Kwatha as Sahapana; and (Group B) Basti group consisting of 17 cases who were administered Dashmoola Kala Basti in which Niruha with Dashmoola Kwatha and Anuvasana with Dashmoola Taila was done. Patients of both the groups were followed by Shamana Chikitsa (Arjunadi Ghanavati). The overall effect of the therapies on systolic and diastolic blood pressure showed that Virechana proved better relief (43.75%) as compared to Basti (29.41%). The response was encouraging and has created scope for further studies.
Keywords: Basti Karma, essential hypertension, Raktapradoshaja Vikara, Virechana Karma
Introduction
Hypertension is called a silent killer because it rarely causes symptoms before it damages the heart, kidneys or brain.[1] It is estimated that 600 million people are affected worldwide with hypertension. By the year 2025, approximately 1 in 3 adults aged over 20 years, totally 1.56 billion people worldwide, will have hypertension.[2] Hypertension is an important public health challenge in both economically developing and developed countries. Significant numbers of individuals with hypertension are unaware of their condition and, among those with diagnosed hypertension, treatment is frequently inadequate. Measures are required at a population level to prevent the development of hypertension and to improve awareness, treatment, and control of hypertension in the community.[2] Moreover, persistent hypertension is one of the risk factors for strokes, heart attacks, heart failure, and arterial aneurysm, and is a leading cause for chronic renal failure. Even moderate elevation of arterial Blood Pressure (BP) leads to shortened life expectancy and causes 5 million premature deaths each year worldwide.[3]
The disease Essential Hypertension (EHT) is neither denoted in Samhita nor in any Samgraha Granthas, but it is stated that every disease cannot be given nomenclature.[4] The term “hypertension” was coined after the invention of sphygmomanometer, however before that about its existence, one can trace the pathway on the tract of symptomatology.
Essential hypertension in the perspective of Rakta Pradoshaja Vikara
Regarding EHT, though it is not mentioned in classics, the Rakta Pradoshaja Vikara concept helps to visualize and successfully categorize it as a Vata Pitta Pradhana Rakta Pradoshaja Vikara in Ayurvedic parlance.[5]
On the basis of strong similarity between etiological factor,[6,7-8] symptom,[5,9] and Doshika involvement in the etiopathology and complication,[10] EHT[11] can be correlated with Vata Pitta Pradhana Rakta Pradoshaja Vikara.
Rationale behind application of Virechana and Basti in the EHT
Acharya Charaka says when Vata is obstructed by Pitta, Kapha, Meda, and Rakta, Virechana should be given with Eranda Taila.[12,13] In EHT, the chief culprit is Vyana Vayu, and is a disease of Bahya,[14] Madhyama Rogamarga, and Marmagata Vyadhi. In these conditions, Basti is the main line of treatment. In both the procedures, mild purgation will occur. As to the mechanism of action of laxative that has been stated in pharmacology, “the laxatives are also likely to act through multiple mechanisms affecting the epithelial transfer directly or indirectly, leading to decreased sodium absorption and increase in chloride excretion by epithelial cell.” This provides a hint that mild laxative action may help in reducing the sodium retention and thus controlling the BP. Both the groups were followed by administration of Arjunadi Ghanavati as the Shamana Yoga which has Arjuna (Terminalia arjuna), Guduchi (Tinospora cordifolia), Gokshura (Tribulus terrestris), Shankhpuhspi (Convolvulus pluricaulis), Jatamamsi (Nordostachys jatamansi), and Guggulu (Commiphora mukul).[15]
With this background, it is planned to evaluate and compare the efficacy of Virechana and Basti Karma in the management of EHT.
Materials and Methods
The patients were selected randomly from Outdoor Patient Department (OPD) and Indoor Patient Department (IPD) of Panchakarma Department of IPGT and RA, Jamnagar Hospital, irrespective of gender, caste, religion, occupation, etc.
Inclusion criteria
Criteria for the selection of the patients were based on the criteria suggested by WHO and JNC-VII (2003). Patients between the age 20 to 60 years were included.
Exclusion criteria
Ischaemic Heart Disease (IHD), Congestive Heart Disease (CHD), Coronary Artery Disease (CAD), coarctation of aorta, renal failure, endocrine diseases, hypertension with cerebral complications, e.g. hypertensive encephalopathy, cerebral haemorrhage, convulsive seizure, and patients having systolic BP more than 180 mm Hg and diastolic pressure more than 110 mm Hg.
Investigations
Routine hematological investigations – haemoglobin %, Total Leucocyte Count (TLC), Differential Leucocyte Count (DLC), Erythrocyte Sedimentation Rate (ESR),
Biochemical parameters – blood urea, serum creatinine, serum cholesterol, triglyceride, High-Density Lipoprotein (HDL), fasting and postprandial blood sugar,
Routine and Microscopic urine examination
Routine and Microscopic examination of stool
Electrocardiography (ECG) and X-ray chest, wherever required. These investigations were conducted to exclude any other underlying pathology.
Groups of treatment
The patients were randomly categorized into the following two groups.
Virechana group (Group A)
In this group, a total of 20 patients were registered, out of whom 16 completed and 4 discontinued the course of therapy.
Basti group (Group B)
In this group, a total of 20 patients were registered, out of whom 17 completed and 3 discontinued the course of treatment.
Schedule for Virechana Karma
Deepana Pachana
As per the condition of Agni, Deepana and Pachana was done for 2-3 days by Trikatu Churna in a dose of 3 g twice in a day.
Snehana
According to Koshtha and Agni, Shuddha Goghrita was given for Snehapana in an increasing dose of 30–50 ml/day for a period of 3-7 days.
Bahya Snehana and Swedana
Bala Taila Bahya Snehana and Sarvanga Mridu Vashpa Sweda were done twice for 3 days after achieving Samyak Sneha Lakshana.
Virechana Karma
Virechana Kashaya was prepared by mixing 100 g of Trivrit (Operculina turpethum) Yavakuta, 50 g of Aaragwadha (Cassia fistula) Phalamajja, and 70 ml of Eranda (Ricinus communis) Taila. It was given in the morning at 10 a.m. with 100 ml of Draksha Hima (cole infusion of Vitis vinitera Linn.) as Sahapana.
Samsarjana Krama
Depending upon Shuddhi, Samsarjana Krama was done for 3-7 days in which Peya, Vilepi, Yusha, Ghrita Yukta Krushara, etc., were given after Virechana.
Schedule for Kala Basti Karma (16 Basti = 6 Niruha + 10 Anuvasana)
In the Kala Basti schedule, one alternating with the other, 10 Anuvasana and 6 Niruha Basti were given. In the beginning, one Anuvasana Basti and at the end, three Anuvasana Basti were given for the purpose of oleation. In this group, Niruha Basti was given of Dashmoola Kwatha and Anuvasana by Dashmoola Taila.
Niruha Basti
The Niruha Basti administered was a homogenous colloidal solution measuring totally 480 ml, which contained 60 g Makshika, 5 g Saindhava, 90 ml Tila Taila, 25 g Shatpuspa kalka, and 300 ml Dashmoola Kwatha. Niruha Basti was given in empty stomach after proper digestion of meal taken in the previous night had taken place, at about 8 a.m.-9 a.m. in the morning.
Anuvasana Basti
60 ml of Dashmoola Taila was given after meal at about 10 a.m.-12 noon. After completion of Kala Basti, Arjunadi Ghana Vati was given according to the following posology.
Arjunadi Ghana Vati
Shamana drug was started after 7 days in both the groups. Arjunadi Ghana Vati was given in a dose of 2 tablets (500 mg each) twice in a day with lukewarm water after meal for a period of 30 days.
Diet
Normal routine diet free from excessive Lavana, Sneha, Katu, Amla Rasa, etc.
Criteria for assessment
A. Scoring pattern for assessment of BP[16]
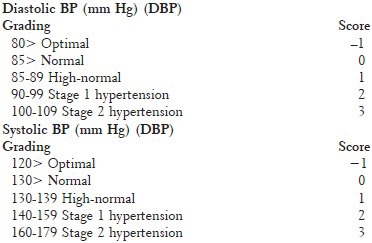
To calculate the % relief in BP, the normal levels of SBP (i.e. <140 mm Hg) and DBP (i.e. <90 mm Hg) were considered to be baseline values, and so percentage relief was calculated at the end by using the formulae:
% Relief in SBP = [(BT − AT)/(BT − 139)]× 100
% Relief in DBP = [(BT − AT)/(BT − 89)]× 100
Here, the BT value shows the BP level before treatment and AT denotes the level achieved after treatment. The after treatment (AT) levels were calculated both after Samsarjana (or 7 days after completion of Virechana and Kala Basti) and after Shamana. All the comparisons were made separately between BT values and AT values achieved after Samsarjana (or 7 days after completion of Virechana and Kala Basti) and between BT values and AT values of Shamana treatment.
Assessment on basis of Systolic and Diastolic blood pressure level
-
(1)
Controlled patients having blood pressure levels within normal limit
-
(2)
Marked relief blood pressure level improved by ≥75% than before treatment
-
(3)
Moderate relief blood pressure level improved by ≥50-74% than before treatment
-
(4)
Mild relief blood pressure level improved by ≥25-49% than before treatment
-
(5)
No relief blood pressure level not improved or improved by <25% than before treatment.
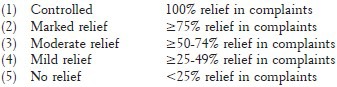
B. Scoring pattern for assessment of signs and symptoms:

Assessment on the basis of relief in complaints
Observations and Results
In this study, all the patients were in the age group of 20-60 years. However, majority of the patients (46.80%) were between 41 to 60 years of age. Majority of the patients (65%) were females, 45% patients were having Vata–Pitta Deha Prakriti, and 72.50% were having Raja Pradhana type of Manas Prakriti. 57.50% of patients were having Mandagni and 35% were having Vishmagni, while 62.5% were having Madhyama Koshtha. Patients of this series have predominantly reported the use of Guru, Snigdha, Ushna, and Vidahi variety of food items, and 70% patients reported Divaswapna. 22.5% were addicted to tobacco, followed by 10% patients who were addicted to alcohol and 7.50% were addicted to cigarette smoking. Out of the Manasika Nidanas, Chinta (82.5%), Shoka (60%), Chittodvega (40%), Krodha (25%), Vishada (32.5%), and Tamogunadhikya (27.5%) were predominantly reported. Patients in this study reported clinical symptoms like Anidra/Alpanidra (92.5%), Shirahshoola (90%), Bhrama (67.5%), Santapa (65%), Buddhi Sammoha (50%), Klama (42.5%), Tamodarshana (17.5%), Arati (32.5%), Akshiraga (40%), and Krodhaprachurata (35%). Vata and Pittadushti were reported in 90% and 85% of patients, respectively. However, Kaphadushti was reported in 80% patients. Pranavaha Srotodushti was reported in 20% patients and Rasavaha Srotodushti was seen in 75% patients. Raktavaha was found in 75%, Medovaha in 85%, Purishavaha Srotodushti in 62.5%, and Swedavaha Srotodushti was found in 37.5% patients. Nearly 42.5% patients were having chronicity (1-3 years). The 32.5% patients reported having SBP between 140 and 159 mm Hg, and 67.5% patients reported an SBP between 160 and 179 mm Hg. DBP of 57.5% patients was between 100 and 109 mm Hg, and 42.5% reported having DBP between 90 and 99 mm Hg.
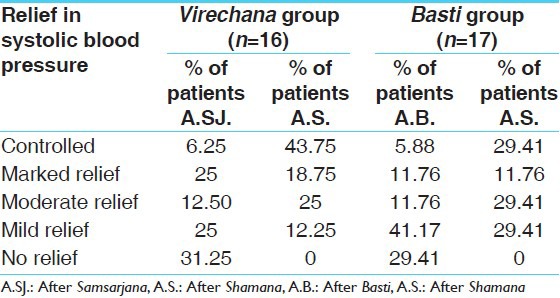
Comparing the effect of therapies on SBP and DBP and other chief and associated complaints, it was seen that effect in Virechana group was better on SBP, Bhrama, Shirahshoola, Klama, Krodhaprachurata, Tamohdarshana, Anidra, and Shrama. Virechana group showed better results in the overall effect of therapy. Thus, the effect of Virechana group is more than that of Basti group and validates involvement of Raktapradosha and Vata Pitta Pradhanata in the pathology of EHT [Tables 1-5].
Table 1.
Effect of Virechana and Basti on systolic and diastolic blood pressure
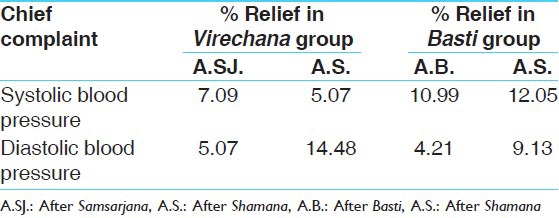
Table 5.
Overall effect of Virechana and Basti on diastolic blood pressure
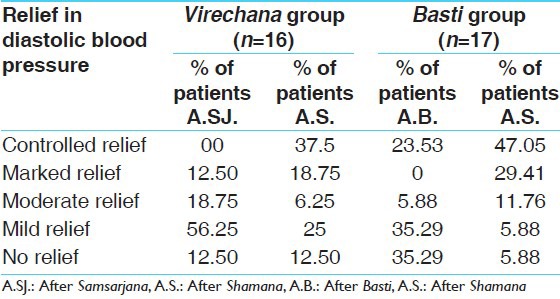
Table 2.
Effect of Virechana and Basti on chief complaints
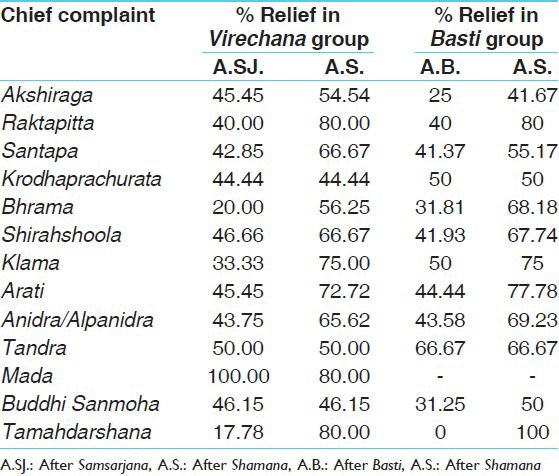
Table 3.
Overall effect of Virechana and Basti on chief and associated complaints
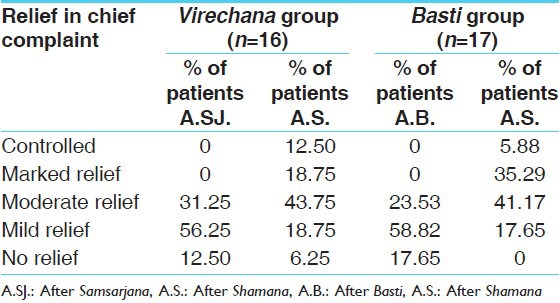
Table 4.
Overall effect of Virechana and Basti on systolic blood pressure
Discussion
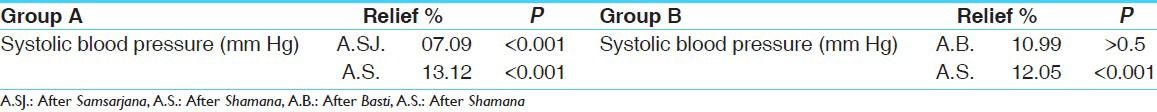
The 7.09% relief in SBP after Samsarjana Krama was reported in Group A and 10.99% relief was reported at completion of Basti in Group B. Total 13.12% relief was recorded after Shamana in group A and 12.05% relief was found after Shamana in Group B. Percentage relief was more in Basti group but was statistically insignificant, and relief was less in Virechana group but was statistically significant, while after Shamana, relief was more in Virechana group and both the groups showed statistically highly significant result [Table 6].
Table 6.
Systolic blood pressure
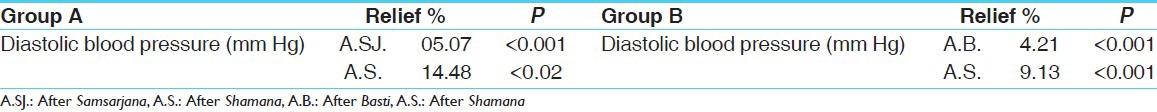
In Virechana group, 5.07% relief was found in DBP after Samsarjana Krama, and 4.21% relief was reported at completion of Basti, while 14.48% relief was recorded after Shamana in Group A and 9.13% relief was found after Shamana in Group B. In Basti group, the results were highly significant both after Basti and Shamana, while in the Virechana group it was statistically highly significant after Samsarjana Krama and statistically significant after Shamana [Table 7].
Table 7.
Diastolic blood pressure
Mode of action of Virechana
The Virechana Karma clears the Margavarodha (obstruction), eliminates the morbid Doshas from Rakta, and regulates the activity and movement of Vata. Thus, it controls the high BP. According to the modern point of view, during Virechana process, the inflammation of intestinal mucosa leads to hyperemia and exudation resulting into increased passage of protein-rich fluids through vessel walls to intestinal lumen. Increase in fluid volume also results in the dilution of toxic material. Evacuation of the fluid from Rasa-Rakta by Virechana is the direct process that leads to decrease in fluid volume.
Few studies correlated acetylcholine with Vata, catecholamine with Pitta, and histamine with Kapha. It has been observed that after Virechana, there is reduction in the plasma catecholamine contents of the patients to a statistically significant level. In that study, it has been observed that the effect of Virechana on neurohumors was highly significant.[17] Virechana evacuates all morbid Doshas from all micro to macro Dhatu channels and regulates Vata, thus decreasing all symptoms of Vata, Pitta, and Kapha on Srotasa level.
Probable mode of action of Basti
It can be understood in the following ways: (1) By absorption mechanism, (2) by system biology concept, and (3) by neural stimulation mechanism.
By absorption mechanism
Dashmoola Taila Anuvasana Basti, after reaching the rectum and colon, causes secretion of bile from gall bladder, which leads to the formation of conjugate micelles which are absorbed through passive diffusion. Especially the middle-chain fatty acid present in Dashmoola Taila of Anuvasana Basti can get absorbed from colon and large intestine part gastrointestinal tract (GIT) and break the pathology of disease.
By system biology concept
The latest concept of system biology makes it clearer how Basti can act on the organ systems. This theory believes that all the organs are interconnected at molecular level. Any molecular incident is transformed at cellular level, then at tissue level and ultimately at organ level. Thus, the effects of Basti on gastrointestinal system will definitely affect another system and help to get the bodily internal homeostasis.
By neural stimulation mechanism
BP is regulated by the feedback of the neural tissue of Vaso-Motor Center (VMC). VMC activity in turn depends upon reflexes from periphery (neural and chemical) and from higher centre. Sympathetic stimulation causes activation of pressure area of VMC, which in turn causes vasoconstriction and leads to rise in BP, while parasympathetic stimulation causes activation of depressor area of VMC, which in turn results in vasodilatation and precipitates decrease in BP.[18]
The long-term regulation of BP occurs through Renin-Angiotensin-Aldosterone (RAA) axis of endocrine mechanisms. Lower part of GIT is richly supplied with parasympathetic nerves which on stimulation with Basti (either by chemical or mechanical receptor) may cause decrease in secretion of RAA complex, and by activating depressor area of VMC which causes vasodilatation and results in decrease in BP.
Enteric Nervous System (ENS) works in synergism with the CNS on stimulation with Basti (either by chemo or mechano receptors) and may lead to activation of depressor area of VMC, which finally causes decrease in BP. It is not mandatory for a drug to remain in contact with the receptor for long time e.g. in proton pump inhibitor mechanism, the drug interacts with receptor and gets flushed out from circulation, it is known as “hit and run module” of kinetics. The same module of kinetics can be hypothesized for Niruha Basti.
Conclusion
As Virechana Karma has shown significant decrease in SBP and DBP, along with fasting and postprandial blood sugar, cholesterol, triglyceride, and increase in HDL level, in conditions where EHT is found to be associated with Sthoulya, Prameha, and hyperlipidemia, Virechana may be the therapy of choice. Basti has shown statistically significant improvement in SBP, DBP, and Shirahshoola, Anidra, Santapa, Bhrama, Buddhi Sanmoha, so in conditions where EHT is found to be associated with the above-mentioned symptoms and other Vata Vyadhis, Basti may be selected as the first line of treatment. Shamana Yoga (Arjunadi Ghanavati) used in this research may be used as a good treatment modality for the management of the EHT. Virechana and Basti Karma provide more relief and synergistic effect in the management of EHT when followed by the Arjunadi Ghanavati. However, the difference in improvement between Virechana and Basti Karma is statically insignificant, but on comparing percentage improvement, Virechana has shown better result.
References
- 1.WHO report of prevention and control for Cardio vascular diseases. 2001-2002. [Last cited on 2002 Aug 25]. Available from: http://www.sld.cu/./pdf/./international_cardiovascular_disease_statistics.page2 .
- 2.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: Analysis of worldwide data. Lancet. 2005;365:217–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 3.WHO World Health Report. [Last cited in 2002]. Available from: http://www.who.int/whr/2002 .
- 4.Agnivesha, Charaka, Dridhabala . In: Charaka Samhita, Sutra Sthana, Trishothiya Adhyaya, 18/44. 2nd ed. Vaidya Jadavji Trikamji Acharya., editor. Varanasi: Chaukhamba Sanskrit Sansthan; 2008. p. 108. [Google Scholar]
- 5.Ibidem. Charaka Samhita, Sutra Sthana Vidhishonitiya Adhyaya, 24/11-16. :124. [Google Scholar]
- 6.Ibidem. Charaka Samhita, Sutra Sthana Vidhishonitiya Adhyaya, 24/5-10. :124. [Google Scholar]
- 7.Vagbhata . Ashtanga Samgraha, Sutra Sthana, 18/14, Hindi Commentary by R.D. Tripathi. 2nd ed. Varanasi: Chaukhamba Sanskrit Sansthan; 1992. [Google Scholar]
- 8.Agnivesha, Charaka, Dridhabala . In: Charaka Samhita, Sutra Sthana, Vidhishonitiya Adhyaya, 24/7. 2nd ed. Vaidya Jadavji Trikamji Acharya., editor. Varanasi: Chaukhamba Sanskrit Sansthan; 2008. p. 124. [Google Scholar]
- 9.Ibidem. Charaka Samhita, Sutra Sthana, Vividhashitpitiya Adhyaya, 28/11. :179. [Google Scholar]
- 10.Ibidem. Charaka Samhita, Sutra Sthana Vidhishonitiya Adhyaya, 24/25-27. :125. [Google Scholar]
- 11.Braunwald E, Isselbacher KJ, Wilson JD, Martin JB, Kasper DL, Hauser SL, et al. 14th ed. Vol. 1. New York: McGraw Hill Publication; 1998. Harrison's Principles of Internal Medicine; p. 1382. [Google Scholar]
- 12.Agnivesha, Charaka, Dridhabala . In: Charaka Samhita, Sutra Sthana Vidhishonitiya Adhyaya, 24/18. 2nd ed. Vaidya Jadavji Trikamji Acharya., editor. Varanasi: Chaukhamba Sanskrit Sansthan; 2008. p. 125. [Google Scholar]
- 13.Ibidem. Charaka Samhita, Chikitsa Sthana, Trimarmiya Chikitsa Adhyaya, 26/29. :598. [Google Scholar]
- 14.Ibidem. Charaka Samhita, Chikitsa Sthana, Vatavyadhi Chikitsa Adhyaya, 28/239. :627. [Google Scholar]
- 15.Shukla GD. Jamnagar: IPGT and RA, Gujarat Ayurved University; 2010. A comparative study of efficacy of Virechana and Basti Karma with Shamana therapy in the management of Essential Hypertension, M.D.(Ayu.) dissertation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Summary of the JNC – V and WHO International Society of Hypertension ISH Special Report. [Last cited in 2004]. Available from: http://www.nhlbi.nih.gov/guidelines/hypertension/phycard.pdf .
- 17.Bhuyan G. Jamnagar: IPGT and RA, Gujarat Ayurved University; 2004. A Critical Study on aetiopathogenesis of Uchharaktachapa (Essential Hypertension) and its management with Virechana Yoga and Shamana Yoga (Herbal Compound) [Google Scholar]
- 18.Dollery CT. Arterial Hypertension. In: Wyngarden JB, Smith LH, editors. Cecil Text Book of Medicine. 17th ed. Chap. 47. Philadelphia: WB Saunders Co; 1985. [Google Scholar]


