Summary
People are diagnosed with cancer sooner nowadays thanks to increased awareness and improvements in cancer screenings. Patients are able to live longer due to cancer treatment regimens; however, they suffer the consequences of living with cancer and therapy-related symptoms. Symptom management is challenging for both patients and family caregivers. Therefore, family members must be integrated in the patient’s care plan. For this review, a literature search was conducted to determine what types of interventions were available that involved family members of cancer patients with the management of cancer and therapy-related symptoms. The following interventions were found that were designed for the family caregivers or both the patient and caregiver to aide with symptom management: pain intervention program, massage therapy, telephone intervention, self-efficacy improvement, coping enhancement and a multidimensional intervention. A positive effect was noted in all the studies, but several had no significance in the patient intervention group but did in the caregiver intervention group. However, studies indicated decreased symptom intensity for various symptoms, decreased symptom distress for both the patient and caregiver, increased self-efficacy of the family member, and increased satisfaction with certain interventions. Further research should be conducted on both existing interventions to better determine their effect and on family symptom management of cancer patients as they need support from healthcare professionals as well.
Keywords: Cancer, Family, Caregiver, Symptom management, Intervention, Nursing
In 2008, the worldwide cancer incidence was an estimated 12.7 million, and 7.6 million cancer deaths are estimated to have occurred [7]. Malignant neoplasms were the second leading cause of death and the projected number one cause of death in 2010 would be cancer [10]. Early detection of cancer and more effective cancer therapies have increased the survival of cancer patients, which has increased the role of symptom management [24].
Cancer and the treatments to eradicate the disease are very detrimental to the patient living with cancer and the family members caring for them. The articles found in the literature review research mostly address the management of pain, nausea and depression of cancer patients and their families combined. However, cancer patients suffer many more symptoms and side effects from the treatment that the patient and family deal with that have not yet been addressed by research. Shorter hospital stays and an increase in outpatient provided-care have shifted the care of the cancer patient to the home, increasing informal care giving and making the family member a primary care provider [4]. Family caregivers are often expected to assume the role of providing personal care and assisting with symptom management [16]. However, research shows that family members feel inadequately prepared to provide physical and psychosocial care [14]. According to Aranda and Hayman-White [1] and Hendrix and Ray [12] caregivers report not feeling confident of the knowledge and skills they have in order to care for their loved ones while managing their symptoms at home. The current healthcare system discharges patients home when they are still in an acute phase and the symptoms are still eventful [12]. This places the burden on the family when assisting the patient with symptom management. Current discharge practices provide the information needed on the day of discharge, not as it ideally should be from admission to discharge [12]. This does not prepare the family caregivers thoroughly for the care-giving task at home.
One caregiver from a study conducted by Hendrix and Ray [12] reported that caregiving in home settings is a partnership between caregivers and patients. This is why it is integral for healthcare professionals to include the family as part of the patient’s care plan. Any education or intervention on symptom management that is given to the patient should also be given to the family caregiver. Symptom management many times falls upon the family caregivers when the patient’s symptoms worsen and they do not have the strength to care for themselves. It is important for these family members to feel that they are equipped with the knowledge to assume the role of symptom manager.
Objectives
The purpose of this review was to summarize the knowledge available on family and/or caregiver symptom management of cancer patients. The following questions were asked:
What types of interventions are available to family, caregivers and patients that aid with symptom management of cancer and therapy related side effects?
What effects do the interventions have on the patient and/ or caregiver in improving cancer symptom management?
Who is best fitted to provide such interventions?
Methods
Search strategies and data sources
For this review, a series of computerized MEDLINE, PUBMED and CINAHL database searches was conducted in June and July of 2012. A general search strategy was developed for each database to determine the information available on family management of cancer patient symptoms. The search was initiated on MEDLINE and yielded 417 results using the following combination of terms: cancer, symptom management, family members, family, caregiver, therapy symptoms, side effects, chemotherapy, radiation therapy oncology, spouses, hair loss, memory changes, infection, pain, and nausea. The same key terms used for the MEDLINE search were applied to CINAHL and PUBMED yielding 77 and 55 articles respectively.
The inclusion criteria were: diagnosis of cancer, experiencing symptoms related to the cancer and/or therapy, family involvement with the patient’s symptom management, English language articles and all types of research designs. Exclusion criteria for the articles were: studies of families whose family member had died from cancer, pediatric cancer patients, nurse administered symptom management of the cancer patient, review articles on the disease process and treatment of cancer and/or cancer symptoms, specified medication treatments and quality of life measurements.
Based on the results a more detailed search was performed on MEDLINE and PUBMED narrowing it to family/ caregiver and/or patient interventions for cancer patient symptom management. The same key terms were used as in the initial search as well as the following: intervention, program, education, training, session, and nurse. Specific key term interventions found from the first search were used too as follows: telephone, FOCUS (family involvement optimistic attitude, coping effectiveness, uncertainty reduction, and symptom management), COPE (creative, optimistic, plan, obtain expert information), and massage therapy.
For this search articles were used that have (i) an intervention for family caregiver and/or the cancer patient; (ii) an intervention implemented by a nurse or trainer and (iii) a positive effect of symptoms or symptom management of the patient and/or family caregiver. Articles that dealt with symptom management post-surgery were excluded.
Data abstraction
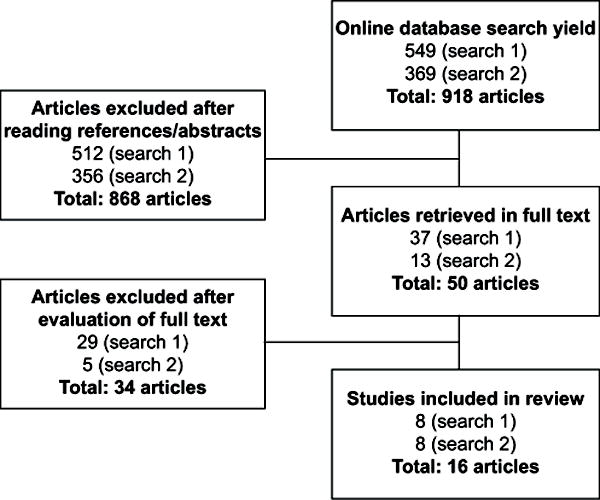
The search in the online databases yielded 549 articles in the initial search and 369 in the second search. From the two searches combined, a total of 868 articles were excluded after the abstracts had been read, as they did not meet the inclusion criteria. Full-text was obtained for 50 articles, and of these 34 were excluded after the articles were read, as they did not meet the inclusion criteria. Eight full-text articles from the initial search and eight from the second were retained for the purpose of this review: a total of 16 articles (Fig. 1).
Fig. 1.
Studies included in the review
Results
The search on symptom management interventions for cancer patients and/or family caregivers has yielded a variety of results. Six subjects that pertain to interventions emerged: pain intervention, massage therapy, telephone counseling, self-efficacy improvement, coping enhancement and a multidimensional intervention. An even distribution of studies was found supporting each one. Both telephone and coping enhancement intervention programs were supported by two studies each and the rest had three supporting studies.
The symptoms targeted in these research articles are the following from most to least addressed: symptoms in general, pain, anxiety, depression, constipation, dyspnea and prostate specific symptoms. Nine studies that target patients receiving cancer treatment, have received treatment or have new or recurring diagnoses; four studies target metastatic/ palliative/hospice patients; two are specific to breast cancer and one to prostate cancer. All of these studies have shown a positive effect for either the patient, the family caregiver or both.
Pain intervention
Pain is the second most common symptom addressed in symptom management studies. It is the only symptom that has an intervention focused on managing a specific symptom. Ferrell et al. [8] and Chou and Lin [5] both provided a pain education booklet to the family caregiver and patient in the first instruction meeting, which was then followed by two follow-up visits. Ferrell et al. [8] created a three-part pain education program (Table 1) that was given in the home and included teaching to the caregivers by a nurse. The caregivers were involved in all nondrug interventions; for example, they were educated on the role of being a support measure in helping the patient use routine analgesia to prevent pain, and they were coached in participating in massage or relaxation exercises [8]. Patients in the experimental group had decreased in the following: pain intensity, perception of pain severity, fear of addiction, anxiety, and an increase in use of pain medications. They also reported improved sleep and knowledge of the subject. The intervention also improved the knowledge of the caregivers, and reduced their fear of addiction to pain medications, giving adequate doses of medications, medicating around the clock rather than as-needed and of respiratory depression [8].
Table 1.
Modified table of pain education program [8]
| Part I: General overview of Pain |
| Defining pain, understanding the cause, assessment, using a preventive approach, involvement of the family |
| Part II: Pharmacologic management of pain |
| Overview of drug management, fears of addiction, fears of drug dependence/tolerance, understanding respiratory depression, talking to the doctor about pain, controlling other symptoms |
| Part III: Nondrug management of pain |
| Importance, use of nondrug modalities as an adjunct to medications, review of previous experiences, Demonstration of heat, cold, massage, relaxation/distraction and imagery |
A study conducted in Taiwan also provided a pain education session to 61 patient-family groups in an outpatient clinic [5]. Families were also provided a pain education booklet and they participated in a 30–40 min education session given by the Research Assistant. An interview was conducted 2 and 4 weeks after the teaching session to complete a questionnaire and to allow patients and family members to ask questions and review information. Contrary to the study by Ferrell et al. [8], this one provided phone numbers in the pain education booklet that caregivers could call if they had any questions. This study analyzed the patient’s satisfaction with pain management with nurses and physicians. An increase in patient satisfaction was noted, which improves adherence to analgesics, according to Chou and Lin [5]. They state “this change in behavior could ultimately result in improvements in the management of cancer pain” [5].
A partner-guided cancer pain management intervention conducted in the patient’s home did not have significant treatment effects for ratings of usual pain and worst pain; however, the intervention group rated their pain lower than the control group [17]. In 3 face-to-face sessions for training in pain management that was taught by a registered nurse-level nurse educator who is knowledgeable about cancer pain, 82 cancer patients and their partners participated. Relevant supplemental written materials, a videotape, and audiotapes were provided. The sessions lasted from 45 to 60 min and they were conducted over the course of 2 weeks. Unlike the patients in the experimental group, the caregivers did exhibit significant positive effects. They projected higher levels of self-efficacy for helping patients control pain and other symptoms. The results show that partners rated their self-efficacy for helping the patient manage pain 25 % higher than the control group and their self-efficacy for helping the patient manage other symptoms as 19 % higher [17]. They also experienced lower levels of caregiver strain and negative mood. The patients in this study were in the terminal phase of their illness, which the authors state that it is very difficult to improve patient’s quality of life during this time. As a result, the partners’ significant improvements in self-efficacy prove to be very remarkable [17].
Massage therapy
Another intervention that has been beneficial in reducing pain in cancer patients is massage therapy [11, 23]. Foot massage promotes relaxation, which decreases the perception of pain and nausea in cancer patients [11]. Two research nurses conducted a foot massage intervention on 87 hospitalized cancer patients. They performed a 10-min massage on two random days and on the third the patient acted as their own control with a quiet activity. For this study, an inverse relationship is seen with relaxation, pain and nausea. Patient reports of increased mean relaxation score was noted while pain and nausea decreased after each massage session. The author stresses the importance of incorporating interested family members by teaching them this simple skill [11].
Family education on massage is evident in Stephenson et al. [23] and Collinge et al. [6]. A 15–30 min foot reflexology teaching session was taught by a Registered Nurse and certified reflexologist in the study by Stephenson et al. [23] to the patient’s caregiver partner. The partner then delivered a 30-min foot massage to the patient in the hospital; the first 10 min focused on relaxation. Pain and anxiety levels decreased significantly in the experimental group compared to the control group, which received usual care plus special attention from their partner. Although the partners’ effects were not measured, some of them reported the experience had social benefits. One wife commented that her husband liked the foot reflexology because it gave them time together during the final 3 weeks of his life [23]. Another wife commented months after the death of her husband, “I’m glad that my husband decided to take part in the study. I think it really helped him. I felt so helpless. [Foot reflexology] was one thing that I could do [for him]” [23].
In the study conducted by Collinge et al. [6], a licensed massage therapist was assigned to two couples to provide a 6-hour standardized structured group workshop. The therapist demonstrated to one caregiver while giving voice-over description of technique, as the other observed. This allowed them to receive the information through kinesthetic, auditory, and visual channels. The partner was then able to practice on the patient under the supervision of the trainer and to receive hands-on correction as needed. The partners were encouraged to practice the manual techniques of their choice at home at least three times a week if possible. Three 2-hour refresher meetings were conducted to provide reinforcement and address people’s experiences and questions. As a result, from baseline to 90-day follow-up, the patient’s mean score of helpfulness doubled, the partner’s mean score for self-efficacy more than doubled, and the duration of massage tripled [6].
Telephone intervention
The telephone is a cost effective way of providing an intervention that pertains easy access of counseling to cancer patients and their family members. It gives nurses an access to patients and caregivers which otherwise they would not be able to [2]. The two studies found, encompass providing counseling to both patient and family caregiver. They vary in that one deals with interpersonal counseling of breast cancer patients and the partner and the other on decision making among elderly cancer patients and their caregivers. Although the focus of neither of these studies is symptom management, they both had a positive effect on the management of symptoms of the patient and caregiver subjects.
Telephone interpersonal counseling (TIP-C) is an experimental study including eight women with breast cancer and their partners. This article presents the case study of one of the subject dyads. The experimental TIP-C group received a modified version of traditional interpersonal psychotherapy supplemented with cancer education. In order to manage the patient’s symptoms, the nurse arranged a series of interpersonal counseling techniques: encouragement of expression of affect, symptom review of depression, permit the client to assume the sick role, decision analysis, role-play, homework assignments and demonstration of positive regard for the patient. This patient is a middle-aged woman experiencing adverse physical and psychological side effects from stress in her interpersonal life and cancer-related treatments. She represents a typical scenario for patients receiving treatment for breast cancer [2]. This patient suffered from depressive symptoms, which is why it was important to consider interpersonal relationships. According to Badger et al. [2], the treatment-related side effects heightened existing interpersonal relationship issues and the side effects from cancer treatments also interposed those relationships [2]. The most common symptoms the patient complained of were poor memory, difficulty concentrating, anxiety, depression, and some fatigue. The nurse counselor was able to educate them on cancer treatment side effects, how to handle specific symptoms and that some of them would clear up after chemotherapy [2].
The husband—as many other partners doubted his participation in the TIP-C—however, admitted to having anxiety about his wife’s condition and the side effects of the treatment. The nurse’s role with the partner in this instance was to address his concerns and enhance his potential as a vital social support of the patient [2]. For example, she advised him to play music or listen to audio books while driving to chemotherapy appointments in order to reduce the anxiety, and she talked to him about the importance of reducing their stress because it interacts with and possibly intensifies side effects. The nurse also educated the husband on strategies to keep his wife from overdoing and getting too stressed out and fatigued [2].
Both the woman and partner reported significant improvements in their own psychological distress and the nature of their relationships with each other and their children [2]. These results were also common in the other participants of the study. Depression and anxiety exacerbate the other therapy-related symptoms. By improving depression and anxiety levels, the nurse was able to assist the patient and husband with the management of other symptoms [2].
A nurse run telephone service to assist elderly cancer patients and family caregivers with decision-making topics also proved beneficial in symptom management [18]. Five Registered Nurses with a Bachelor’s degree, referred to as Cancer Center Nurse Coordinator (CCNC), were available to patients and caregivers via telephone. The patient or caregiver initiated the call. For this study, the researchers contacted the CCNCs and conducted a face-to-face semistructured interview to obtain data from the phone conversations the nurses had with patients and caregivers. There were a total of 41 phone conversations that were included in this study. While 61 % (n = 25) were family caregivers [18], 34 % of the callers (n = 14) were elderly patients. The percentage of family caregivers that called is very important because it shows that more than half the callers were family, which substantiates their involvement in patient care.
The most frequent decision-making topic that the callers needed assistance with was symptom management. The elderly patient or family caregiver called about concerns on treating specific symptoms such as pain, elevated temperature, edema, or flu symptoms [18]. One caregiver called about the pain management of his wife. “She had taken a couple of Tylox an hour ago, had been up all night–had a very bad night’s sleep”. He wanted to know if even though she had had two Tylox at 6 A.M., could she take half a Naprosyn now [18]. Another husband and patient called because they were concerned about getting a blood transfusion from a donor pool. They wanted to know what the risks were of acquiring an infection from the transfusion versus the risks of her symptom of low Hemoglobin from the chemotherapy [18].
This study did not obtain any data directly from the patient or family caregiver; therefore, the effectiveness of this service to them is unknown. However, the CCNCs perceived the need of the caller’s assistance with decisionmaking. From the different topics discussed by the callers and nurses, five types of assistance were determined: clarification of information, reassurance from the CCNCs, listener, permission to alter treatment regimen and help in establishing communication [18]. Callers contacted the nurses for a variety of decision-making questions, but symptom management was the most common reason for calling. This demonstrates the need these patients and caregivers had for obtaining information that helped them with issues related to the management of symptoms. Sometimes they were unsure of a medication they could take and other times they needed help on deciding whether they should take a certain treatment to help eliminate a symptom [18].
Self-efficacy improvement
Three of the studies found [9, 12, 13] drew the foundation of the intervention from Bandura’s Self-Efficacy Theory in which self-efficacy is the trust in your capabilities to organize and apply the action necessary to produce given outcomes [3]. Sources of self-efficacy include live modeling, performance exposure, positive appraisal, and performance mastery [3]. Live modeling allows caregivers to observe someone who has mastered a skill perform an intervention. Performance exposure and positive appraisal then allows them to administer the intervention with the guidance of a healthcare professional and receive formative criticism. Eventually the caregiver is able to successfully perform the intervention [12].
Hendrix and Ray [12] conducted a study to determine feasibility of individualized caregiver training for home care and symptom management that is taught at the bedside of older patients with cancer prior to hospital discharge. Seven informal female caregivers were selected whose patients were close to the discharge date. The training was conducted in one or two sessions that lasted between 3 and 6 hours. An experienced advanced practice nurse conducted the training and encouraged the patients to also take part in the training [12]. The nurse first discussed patient needs and cancer symptoms and proceeded the training by educating in five basic areas of symptom management: prevention of infection, pain control, maintenance of adequate nutrition, prevention and management of constipation or diarrhea, and medication regimen related to cancer symptoms [12] (Table 2). The training was interactive, which required the caregiver, and the patient when present, to be involved and participate in problem solving for specific symptoms or care needs. The training though was adjusted to fit the caregiver and patient needs [12]. The nurse combined didactic teaching and performance of the skills that the caregiver would need once they go home. For example, one of the patients required a gastrostomy tube feeding. The nurse showed the caregiver the proper way to inspect, aspirate, and flush it after feedings. The nurse demonstrated the first feeding, while the caregiver observed, but halfway through the feeding the caregiver was asked to finish it. This allowed the nurse to observe and give positive feedback [12]. However, if the patient did not want to participate, then the nurse would provide the equipment and still go through the same process. At the end of the training, the caregivers received A Manual for Informal Caregivers on Cancer Symptom management, which was written by the primary author. This is an instruction manual that contains a list of nonpharmacologic and supportive interventions for cancer symptom management [12].
Table 2.
Cancer symptom areas in each caregiver training [12]
| Topic | Discussion |
|---|---|
| Prevention of infection | Assessment of caregiver’s knowledge Prevention of infection |
| Discussion of signs and symptoms of infection | |
| Central line care and dressing change, Foley catheter care, and wound care, as applicable | |
| Pain control | Pain assessment |
| Guidelines for pain medication | |
| Nonpharmacologic interventions | |
| Maintenance of adequate nutrition | Assessment of the patient’s problem with nutrition |
| Guidelines for maintaining or increasing caloric intake | |
| Oral care | |
| Tube feeding, if applicable | |
| Prevention and management of constipation or diarrhea | Assessment of patient’s problem with bowel elimination |
| Discussion of strategies that alleviate or prevent constipation or diarrhea | |
| Medication regimen related to cancer symptoms | Assessment of medications |
| Discussion of each medication: purpose and side effects |
The results yielded a unanimous report from the caregivers that they liked the individualized approach to training because it gave them the chance to discuss relevant issues and focus the training on what they really needed to know. All of the caregivers believed that the bedside training that gave them the opportunity to practice skills with the support of a nurse, increased their confidence that they would be able to help their loved ones manage their symptoms [12]. All caregiver subjects also reported that the training was worthwhile and should be given to all cancer caregivers before hospital discharge. The patients were not formally invited to the training session and as a result one caregiver stated that “patients should be invited to participate, citing that caregiving in home settings is a partnership between caregivers and patients” [12].
The individualized caregiver training was also investigated in terms of its effects on caregiver’s self-efficacy and their psychological well-being as well as its impact on the patient’s symptoms in home care and symptom management. The study incorporated an experimental design and data were obtained before and after the training, as well as 1, 2 and 4 weeks after the patient’s hospital discharge [13]. The intervention was offered prior to imminent discharge and provided both didactic and performance training on strategies for managing the patient’s cancer symptoms. These included prevention of infection, pain control, maintenance of nutrition and adequate elimination. The intervention lasted 2–3 hours and was delivered in one or two sessions. The participants were also provided with an instruction manual [13]. The findings indicate that while the training had no effect on the psychological well-being and the patient’s physical symptoms, caregiver self-efficacy significantly increased after receiving the individualized training and had a sustained effect 4 weeks after the patient’s hospital discharge [13].
Another study used a cognitive behavioral intervention (CBI) that drew upon Bandura’s Framework to determine if the severity of symptoms experienced by patients during chemotherapy could be decreased [9]. A total of 118 dyads were randomized into the experimental intervention that was given to both the family caregiver and patient dyad over a 10-contact, 20-week period; the intervention consisted of five in-person visits for the caregiver and patient that coincided with scheduled visits to their oncology center and five via telephone that were done 2 weeks after each in-person visit. Their goal was to evaluate the impact of the intervention for lowering negative reactions of the family members and increase involvement with symptom management of patients receiving chemotherapy [9]. The CBI consisted of information for the patient and caregiver. The patients were given information on self-care, cognitive reframing, coping strategies, and techniques for communicating their needs for assistance to their family members [9]. The caregivers’ intervention focused on the cause of symptoms and strategies to managing them, how to integrate assistance into their daily lives, and how to better communicate with the patient and health care providers regarding symptom management. During the sessions, the intervention nurse and caregiver selected strategies for them to implement in assisting patients to manage symptoms. These were then evaluated at follow-up visits and established whether to continue or discard [9].
It was discovered that patients that received the experimental intervention reported significantly lower symptom severity; likewise, they also experienced lower levels of depressive symptoms and moderating effects of neutropenia [9]. The study’s aim was to increase caregiver involvement with symptom management; however, it did not have the expected effect. Instead, the experimental intervention reduced the caregivers total negative reactions to providing care compared to the conventional care group. This seemed to be as a result of the lower number of symptoms that required assistance due to the decreased symptom severity experienced by the patients. This in turn did not increase involvement with symptom management, but rather decreased it [9].
Coping enhancement
COPE is a problem-solving intervention that is designed for family caregivers. The acronym COPE stands for creativity, optimism, planning, and expert information and encourages the family caregiver to do all of the above [4, 19]. The intervention introduced problem-solving techniques using examples from the Home Care Guide for Advanced Cancer[15] in both of the studies found. Under the four letters of COPE, an aspect of symptom management is addressed. For example, under ‘creativity’, they encourage caregivers to develop new strategies for resolving problems [19]. Expert information consists of teaching family about what they need to know about the nature of the problem, when to get professional help, and what they can do to deal with the problem independently. Symptom assessment is also included under this area because it is important to know about their characteristics and intensity so they know when they must call the healthcare professional [19].
McMillan et al. [19] used a three-group comparative design to determine if the intervention helped hospice caregivers to better manage symptoms experienced by patients with cancer. They had a standard (control) group, standard with friendly support and the experimental group receiving standard care plus COPE. The group receiving the COPE intervention received assistance with assessment and management of patient problems [19]. This study separated the teaching support of caregiver problem solving into three ways. First, written information is organized to facilitate problem solving in the Home Care Guide for Advanced Cancer[15]. They focused on management of pain, dyspnea, and constipation in order to serve as a model for the development of plans for other symptoms and problems [19]. An experienced nurse who was trained in COPE visited the 109 intervention group dyads in their home three times over the course of 9 days to implement the intervention. Second, the nurse demonstrated the use of COPE problem-solving principles; they supported the caregivers with the development of plans. Third, the nurse telephoned the caregivers between each intervention visit to ask about current problems concerning the targeted symptoms, offering help and answering questions [19]. McMillan et al. [19] measured the symptom intensity of the three symptoms, the overall symptom distress, and the quality of life of the patients. Only symptom distress indicated a significant change by the intervention group. Patients from the COPE group did not improve their symptom intensity or quality of life; however, symptom distress decreased. Patients were better able to tolerate symptoms of pain, constipation, and dyspnea, although they were not eliminated. The lack of improvement in symptom intensity is possibly due to the fact that these were hospice patients; hence, the cancer and cancer-related symptoms naturally would have worsened near death [19]. Data on the caregivers also showed that they perceived less distress from symptoms and less burden of caregiving as a result of the COPE intervention [19].
Cameron et al. [4] also conducted a study, using COPE for a problem-solving intervention given to family caregivers of advanced cancer patients while the patient was in the hospital attending a clinical visit. In addition to COPE, the researchers encouraged family members to use the following approach: (i) define the problem; (ii) identify when to get professional help with the problem, (iii) identify what they could do to help; (iv) consider possible barriers to their caregiving plan, and (v) implement and adjust the plan [4]. This intervention was given via a slide presentation on a laptop or using flipcharts and lasted approximately 1 hour [4]. Data were collected at a 4-week follow-up and showed that caregivers had a decreased emotional tension and increased caregiving confidence and positive problem solving [4]. The improvement was not very significant, but considering that the baseline scores were already high, it indicates that the subjects were already good problem-solvers. Cameron et al. [4] suggest that caregivers lacking confidence and problem-solving abilities would benefit more from this intervention. They project that a more comprehensive intervention such as one provided over multiple sessions or in the patient’s home would have a stronger effect [4].
Multidimensional intervention
The FOCUS intervention is designed for the entire family, which includes the caregiver and patient together. The five letters of the acronym FOCUS represent five core areas of the intervention: family involvement, optimistic attitude, coping effectiveness, uncertainty reduction, and symptom management [21, 22]. Two studies were found that gave the intervention over three 90-min home visits and two 30-min telephone sessions: a masters-prepared nurse delivered the intervention [21, 22]. Recent research showed that many elements of the in-person FOCUS program can also be successfully adapted into an interactive web-based format. A trial to evaluate its effect on a variety of psychosocial outcomes is in progress [25].
Both studies encouraged caregiver and patient dyads (spouse and patient in both cases) to work together as a team, maintain open communication, and provide each other with support in order to keep the family involved, with the exception of Northouse et al. [22], which also includes identifying family strengths and helping children in the family [21, 22]. Open communication between a husband and wife [patient] with the guidance of the nurse, helped the couple express their frustrations and develop an understanding [22].
In the area of symptom management, the nurse assessed symptoms and distress experienced by patients and family members, and taught self-care strategies [21, 22]. One study by Northouse et al. [21] is specific to prostate cancer patients and their wives, and also assessed prostate-specific symptoms of the patient related to urinary, bowel, sexual, and hormone problems [21]. In another study by Northouse et al. [22], part of teaching self-strategies involved giving the patients and family members a preprinted symptom management card for each symptom they had from a list of 39 possible symptom cards. Many of the women complained of constant pain; therefore, the nurses educated them on safe pain medication use and discussed the importance of scheduling routine administration of pain medication to control pain before it becomes intolerable. At the same time, the nurses encouraged the family members to care for their own health because it is important for them to stay healthy so they would be able to take care of the patient [22].
The patients in the FOCUS Program reported significantly higher satisfaction with each of the five content areas of the FOCUS Program than patients in the control group. There was more satisfaction with the patients in their family’s involvement in discussions, and information they were provided on symptom management. The FOCUS intervention patients also reported better understanding of their nurses than the control group [22]. Northouse et al. [21] also measured quality of life and symptom distress: no differences were noted between the FOCUS intervention and control patient groups. Spouses in the FOCUS group though did exhibit significantly less general symptom distress of their own than the control spouses, along with higher self-efficacy and better physical quality of life. They also reported to experience less problems related to their husbands’ urinary incontinence [21]. The difference seen between the results of spouses and caregivers is due to a greater need for spouses to have the intervention; they were able to learn how to cope with the stress of caregiving and manage the symptoms experienced by the patients [21]. The results also showed slightly higher satisfaction of the FOCUS Program among family members, but there was only a significant difference between the intervention and control group in the area of family involvement [22].
Another study [20] examined whether the effects of the FOCUS Program on patient-caregiver dyads varied in terms of the intervention dose (brief or extensive) and whether the risk for distress and other antecedent factors moderated the effects of either intervention. The brief FOCUS Program consisted of three contacts with two 90-min home visits and one 30-min phone session, whereas the extensive FOCUS Program consisted of twice as much [20].
The dyads were randomly assigned to the control group (usual care), the brief FOCUS Program or the extensive FOCUS Program. Data were obtained prior to the intervention as well as 3 and 6 months after the intervention. Both the brief and the extensive FOCUS Program had the same content and were 10 weeks in duration. The final sample consisted of 302 dyads which completed all three assessments [20].
The study found that both versions of the FOCUS Program helped the dyads to cope more effectively and maintain their quality of life. Furthermore, the findings suggest that extensive interventions rather than brief interventions are sufficient to improve the self-efficacy of the dyads. On the other hand, brief interventions are sufficient to improve patients’ and caregivers’ use of healthy behaviors. Even though the dyads in both experimental groups had more improvement on the study outcomes than the dyads in the control group, the majority of the effects in both versions of the FOCUS Program occurred at the 3-month follow-up only. According to the researchers, the lack of sustained effects may be related to the increasing demands on caregivers as the patient’s illness progresses or to the decreased sample size at the 6-month follow-up. Since both the brief and the extensive FOCUS Program had almost the same number of effects, neither can be considered more preferable [20]. Contrary to expectations, high-risk distress patient-caregiver dyads in this study did not benefit more from the extensive FOCUS Program. Overall, moderation effects were limited and occurred in the control group only. Thus, the relationship between high-risk distress status and intervention outcomes remains unclear and needs further research [20].
Discussion
There appears to be a strong focus on interventions to manage pain as evidenced by the massage intervention, pain intervention programs, and one of the COPE studies. Pain is one of the most common symptoms the cancer patients suffer from, but there are many other cancer patients on which not much research has been conducted yet. This demonstrates a gap in research on interventions specific to certain symptoms and types of cancer. Further research should be conducted to determine what is best for patients and family members. Many of the studies also concentrate on caregiver’s confidence and self-efficacy. It would be wise to make caregiver empowerment the central intervention with the addition of education on cancer and symptom management.
Another subject that rises with providing symptom management interventions to families and patients is the question as to who can implement it. In all the articles found, except for two, a registered nurse served as the interventionist. It appears that nurses are the professionals that are best equipped for providing education and counseling to families and patients affected by cancer. It is important though to understand that the baseline for performing the interventions is being a Registered Nurse, but in many of the studies found, the nurses had graduate level education and were Advanced Practice Nurses. However, both Registered Nurses and Advanced Practice Nurses had oncology expertise. In the TIP-C study though an advanced practice nurse specialized in psychiatric mental health nursing performed the intervention because it was specific to interpersonal counseling and targeted the management of depression and anxiety. Some of the techniques, however, can be implemented by all nurses [2].
This suggestion can be applied to all intervention nurses. In order to increase the availability of intervention programs for cancer patients and their family members, registered nurses must be equipped with the knowledge to perform these interventions or programs. It is a possibility for a training program being developed for registered nurses to certify them in family focused symptom management of oncology patients.
Conclusion
This literature review, based on 16 research articles, presents the description and results of family based interventions for symptom management of cancer patients. The interventions described in these studies have proved to be helpful for patients, caregivers, or both. There is strong supporting evidence for the positive effects of massage and pain intervention programs, interventions to improve self-efficacy and for the multidimensional intervention. However, the other interventions found, only have two studies each to support their results. Some of them also do not have a positive effect on the patient intervention group, but do on the family caregivers. More research is required on the existing interventions to better determine their effect on patients and caregivers. This review provides an overview of the programs and interventions available to family caregivers of patients with cancer to help them with cancer and therapy-related symptom management. Cancer patients are the main focus of care to healthcare professionals, but the family members must be included in the care plan as well. When a family member suffers from cancer symptoms and treatment side effects, those surrounding or living with them suffer as well because they are inevitably tied to the patient. For this reason, it is critical that health care professionals incorporate family caregivers in the symptom management of the family member with cancer.
Acknowledgments
Disclaimer Ms Hazelwood’s work on this project was supported by “Training in Chronic Illness Research in Georgia and Abroad,” from the National Institute for Minority Health and Health Disparities, National Institutes of Health, Dr. K. Anderson, PI. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Daniela Maria Hazelwood, School of Nursing, Georgia Southern University, Statesboro, Georgia, USA.
Sabine Koeck, Email: sabine.koeck@univie.ac.at, Department of Nursing Science, University of Vienna, Alser Straße 23/12, 1080 Vienna, Austria.
Martin Wallner, Department of Nursing Science, University of Vienna, Alser Straße 23/12, 1080 Vienna, Austria.
Kathryn Hoehn Anderson, School of Nursing, Georgia Southern University, Statesboro, Georgia, USA.
Hanna Mayer, Department of Nursing Science, University of Vienna, Alser Straße 23/12, 1080 Vienna, Austria.
References
- 1.Aranda SK, Hayman-White K. Home caregivers of the person with advanced cancer: an Australian perspective. Cancer Nurs. 2001;24:300–7. doi: 10.1097/00002820-200108000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Badger T, Segrin C, Meek P, et al. A case study of telephone interpersonal counseling for women with breast cancer and their partners. Oncol Nurs Forum. 2004;31:997–1003. doi: 10.1188/04.ONF.997-1003. [DOI] [PubMed] [Google Scholar]
- 3.Bandura A. Self-efficacy: the exercise of control. New York: W.H. Freeman; 1997. [Google Scholar]
- 4.Cameron JI, Shin JL, Williams D, et al. A brief problem-solving intervention for family caregivers to individuals with advanced cancer. J Psychosom Res. 2004;57:137–43. doi: 10.1016/S0022-3999(03)00609-3. [DOI] [PubMed] [Google Scholar]
- 5.Chou P-L, Lin C-C. A pain education programme to improve patient satisfaction with cancer pain management: a randomised control trial. J Clin Nurs. 2011;20:1858–69. doi: 10.1111/j.1365-2702.2011.03740.x. [DOI] [PubMed] [Google Scholar]
- 6.Collinge W, Kahn J, Yarnold P, et al. Couples and cancer: feasibility of brief instruction in massage and touch therapy to build caregiver efficacy. J Soc Integr Oncol. 2007;5:147–54. doi: 10.2310/7200.2007.013. [DOI] [PubMed] [Google Scholar]
- 7.Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 8.Ferrell BR, Rhiner M, Ferrell BA. Development and implementation of a pain education program. Cancer. 1993;72:3426–32. doi: 10.1002/1097-0142(19931201)72:11+<3426::aid-cncr2820721608>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 9.Given B, Given CW, Sikorskii A, et al. The impact of providing symptom management assistance on caregiver reaction: results of a randomized trial. J Pain Symptom Manage. 2006;32:433–43. doi: 10.1016/j.jpainsymman.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 10.GLOBOCAN 2008. Cancer fact sheet. 2010 Zugegriffen: 1 Juli 2011. [Google Scholar]
- 11.Grealish L, Lomasney A, Whiteman B. Foot massage. A nursing intervention to modify the distressing symptoms of pain and nausea in patients hospitalized with cancer. Cancer Nurs. 2000;23:237–43. doi: 10.1097/00002820-200006000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Hendrix C, Ray C. Informal caregiver training on home care and cancer symptom management prior to hospital discharge: a feasibility study. Oncol Nurs Forum. 2006;33:793–8. doi: 10.1188/06.ONF.793-798. [DOI] [PubMed] [Google Scholar]
- 13.Hendrix CC, Landerman R, Abernethy AP. Effects of an individualized caregiver training intervention on self-efficacy of cancer caregivers. West J Nurs Res. 2011 doi: 10.1177/0193945911420742. [DOI] [PubMed] [Google Scholar]
- 14.Hinds C. The needs of families who care for patients with cancer at home: are we meeting them? J Adv Nurs. 1985;10:575–81. doi: 10.1111/j.1365-2648.1985.tb00550.x. [DOI] [PubMed] [Google Scholar]
- 15.Houts PS, Bucher JA. American College of physicians home care guide for advanced cancer. Philadelphia: ACP; 1997. [Google Scholar]
- 16.Kazanowski M. Family caregivers’ medication management of symptoms in patients with cancer near death. J Hosp Palliat Nurs. 2005;7:174–81. [Google Scholar]
- 17.Keefe FJ, Ahles TA, Sutton L, et al. Partner-guided cancer pain management at the end of life: a preliminary study. J Pain Symptom Manage. 2005;29:263–72. doi: 10.1016/j.jpainsymman.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 18.Lewis M, Pearson V, Corcoran-Perry S, et al. Decision making by elderly patients with cancer and their caregivers. Cancer Nurs. 1997;20:389–97. doi: 10.1097/00002820-199712000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Mcmillan SC, Small BJ. Using the COPE intervention for family caregivers to improve symptoms of hospice homecare patients: a clinical trial. Oncol Nurs Forum. 2007;34:313–21. doi: 10.1188/07.ONF.313-321. [DOI] [PubMed] [Google Scholar]
- 20.Northouse LL, Mood DW, Schafenacker A, et al. Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers. Psychooncology. 2012 doi: 10.1002/pon.3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Northouse LL, Mood DW, Schafenacker A, et al. Randomized clinical trial of a family intervention for prostate cancer patients and their spouses. Cancer. 2007;110:2809–18. doi: 10.1002/cncr.23114. [DOI] [PubMed] [Google Scholar]
- 22.Northouse LL, Walker J, Schafenacker A, et al. A family-based program of care for women with recurrent breast cancer and their family members. Oncol Nurs Forum. 2002;29:1411–9. doi: 10.1188/02.ONF.1411-1419. [DOI] [PubMed] [Google Scholar]
- 23.Stephenson NL, Swanson M, Dalton J, et al. Partner-delivered reflexology: effects on cancer pain and anxiety. Oncol Nurs Forum. 2007;34:127–32. doi: 10.1188/07.ONF.127-132. [DOI] [PubMed] [Google Scholar]
- 24.Theobald DE. The strength to fight cancer: a family guide. Indianapolis: Quality of Life Foundation; 2002. [Google Scholar]
- 25.Zulman DM, Schafenacker A, Barr KL, et al. Adapting an in-person patient-caregiver communication intervention to a tailored web-based format. Psychooncology. 2012;21:336–41. doi: 10.1002/pon.1900. [DOI] [PMC free article] [PubMed] [Google Scholar]


