Abstract
Knee osteoarthritis (OA) manifests with pain, joint stiffness, and limited function. In traditional Chinese medicine, knee OA is differentiated into three patterns: yang deficiency and cold coagulation, kidney deficiency, and blood stasis. The objective of this study was to determine whether yang deficiency cold coagulation patients respond better to thermal laser acupuncture treatment than do non-yang deficient patients. Fifty-two patients with OA were allocated to group A (yang deficient, n = 26) or B (non-yang deficient, n = 26). All patients received a 20-min thermal laser acupuncture treatment at acupoint Dubi (ST 35) three times a week for two weeks and twice a week for another four weeks. Outcome assessments were performed immediately after the first treatment, and at weeks 2, 6, and 10. Group A function scores were significantly better than those of Group B at weeks 2 (P = 0.049), 6 (P = 0.046), and 10 (P = 0.042), but no significant differences were found between the two groups in pain and stiffness scores at any time point. No significant adverse effect was observed. The combined 10.6 μm–650 nm laser treatment might be most beneficial to yang deficiency cold coagulation knee OA patients, particularly in improving function.
1. Introduction
Osteoarthritis (OA) manifests clinically as chronic joint pain, stiffness, and swelling accompanied by dysfunction. The knee is the joint most commonly involved, and knee OA is a chronic disease [1]. With aging, the incidence of the disease tends to increase, and pain and dysfunction of the knee can seriously affect life activities [2, 3]. No conventional cure is currently available, which makes knee OA a leading cause of pain and disability worldwide [4]. Pathological changes include loss of local articular cartilage and new bone formation at joint margins where destructive bone loss occurs [4]. Conventional therapies, usually NSAIDs, mainly are used to manage symptoms such as joint pain, improve function, delay the progression of joint damage, and improve patient quality of life [5]. These often have undesirable side effects such as gastrointestinal disorders, making treatment unsustainable [6].
Studies have shown acupuncture is successful in treating joint pain, including knee OA [7]. In Traditional Chinese Medicine (TCM) theory, chronic knee OA is considered to be mainly due to kidney deficiency, blood stagnation, and the retention of damp cold in the knee. Moxibustion, part of traditional acupuncture treatment, involves the burning of an herb (Artemisia argyi) at the site of acupoints; it is commonly used in treating arthritis particularly joint pain caused by cold [8–12]. However, the use of this technique is limited, particularly in the West, because of the smoke and inconvenience of the procedure, and caution is needed to prevent burning the patient's skin.
In recent years, lasers with red and near-infrared wavelengths such as the 650 nm laser have been widely used in clinical settings [13–17]. Several investigators report successful treatment of chronic pain, including knee OA, with these devices [18–23]. We recently developed an appliance that combines laser wave lengths of 10.6 μm and 650 nm to mimic the effects of moxibustion and acupuncture: these wave lengths produce both the needle-like effect of acupuncture and the thermal effect of moxibustion [22, 23]. Because of the nature of the device, we hypothesized that it might be most effective for reducing pain and improving function in the cold syndrome of knee OA. We conducted a patient-centered, nonrandomized outcome effectiveness study to compare the response of yang deficiency cold coagulation pattern knee OA patients to 10.6 μm–650 nm combined laser irradiation with that of OA patients with other TCM patterns.
According to TCM theory, knee OA symptoms are differentiated into (1) yang deficiency cold stagnation, (2) kidney essence deficiency, and (3) blood stasis and collateral stagnation [24]. The main symptoms of yang deficiency cold stagnation are pain, stiffness, and impaired function in the knee joint, worse with cold, and alleviated by warmth. The patient often feels cold, fatigue, and heaviness in the limbs. The tongue is pale with white coating; the pulse is deep, thready, and slow. The main symptoms of kidney essence deficiency are limited range of motion, dizziness, and tinnitus. The tongue is pinkish with a thin coating; the pulse is thready. The main symptoms of blood stasis and collateral stagnation are fixed pain, limited range of motion, dark face, and purplish lips. The tongue is purple and dark; pulse is deep and thready. Of the three TCM patterns, yang deficiency cold stagnation is a cold syndrome and can be alleviated by a warm therapy.
In Chinese acupuncture practice, “warming needles,” in which moxa wool is burned on the handle of an acupuncture needle, is often used on patients with cold syndrome TCM patterns [25, 26]. The thermal effect of the combined 10.6 μm–650 nm laser mimics the warming needle in that the 10.6 μm CO2 laser wavelength has a thermal effect while the 650 nm laser wavelength has a needle-like effect. The purpose of the present study was to determine the usefulness of TCM pattern diagnosis in the effectiveness assessment of this laser treatment and to see whether thermal laser irradiation would be more effective on yang deficiency cold coagulation knee OA.
2. Materials and Methods
2.1. Patient Recruitment
The study was conducted from July 2007 to February 2009 in out-patient settings at two research centers in Shanghai, China: Shuguang Hospital affiliated to Shanghai University of Traditional Chinese Medicine and First People's Hospital affiliated to Shanghai Jiao Tong University. The research protocol was approved by the Institutional Review Board of Shuguang Hospital affiliated to Shanghai University of Traditional Chinese Medicine (no. 2007-N019-01). Each subject provided informed consent.
We recruited subjects by advertising in local newspapers. Interested subjects contacted the study coordinator, who conducted initial telephone screening. Potential subjects then received on-site clinical assessments in the hospital after getting a full description of the study and giving informed consent.
Patients who met the inclusion criteria were included for the trial: male or female, between 50 and 75 years old, diagnosed with knee OA as defined by the American College of Rheumatology (ACR) [24] such as radiographic evidence of at least one osteophyte at the tibiofemoral joint, (Kellgren-Lawrence grade ≥2), moderate or greater knee pain on most days (>50%) during the previous month, and willingness to sign the consent form. Exclusion criteria were presence of serious medical conditions such as kidney or liver disease or deep vein thrombosis that precluded participation in the trial, intra-articular corticosteroid or hyaluronate injections, knee surgery during the past 6 months, participation in other clinical trials within the past six months, and travel or other plans that would interfere with participation in the entire six-week study. Patients were allowed to maintain their baseline pain medications during the course of experiment, and any changes in medication were documented.
2.2. Study Protocol
This was a nonrandomized outcome effectiveness study comparing the response to 10.6 μm–650 nm combined laser irradiation treatment of yang deficient patients (Group A) to that of non-yang deficient patients (Group B). After subjects met the inclusion/exclusion criteria, one experienced TCM doctor carried out a pattern differentiation on each; based on the differentiations, we recruited 26 patients to each group. The yang deficiency cold coagulation pattern was defined as knee pain, aversion to cold in the joint, alleviation of symptoms by warmth, and aggravation by cold [27].
2.2.1. Laser Device
The features of the device and the method of operation have been previously reported [22, 23]. In brief, 10.6 μm–650 nm combined laser irradiation was generated by a semiconductor laser with a 0.65–0.66 μm-long wave transmitted by quartz-glass light fibers (36 mW) and a CO2 laser with 10.6 μm-long wave by a silver halide light fiber (200 mW). Output was set in accordance with the safety criteria of Shanghai Enterprises (Q/KYD012-2004). The output was transmitted to a combined laser tip that irradiated the skin with a single beam 2 mm in diameter. A 2 cm distance between the laser tip and the skin was maintained by a plastic tube, 1 cm in diameter and 2 cm in length, mounted on the tip of the device (Figure 1).
Figure 1.
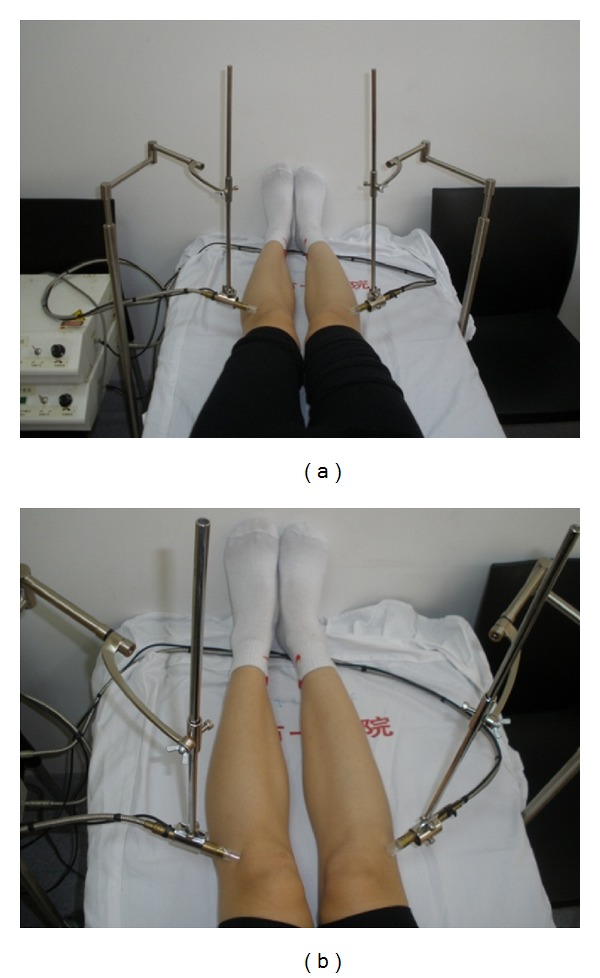
(a) Laser treatment was performed bilaterally. (b) Laser tips were placed at acupuncture point ST35 (Dubi).
2.2.2. Intervention
Laser treatments were performed by trained technicians blinded to the group allocation. During treatment, the room was maintained at a constant 20°C. The patient was instructed to lie supine for 5 min before treatment. The laser tip was placed perpendicularly on the affected knee, or on both knees if both were affected, at acupuncture point ST35 (Dubi) which is located in the depression on the lateral side of the patella and the patellar ligament [28] (Figure 1). ST 35, called Dubi or Xiyan (“eye of the knee”), is commonly used in clinical trials as a major local point for treating knee-related disorders [29–31]. The device was activated for 20 min, and the patient received 10.6 μm laser energy of 120 J and 650 nm laser energy of 43.2 J at each session. Patients were treated three times a week for the first two weeks and twice a week for the next four, a total of 14 treatments in six weeks.
2.2.3. Outcome Assessments
Trained investigators blinded to group allocation used an internationally standard assessment instrument, the Western Ontario and McMaster Universities osteoarthritis index (WOMAC) to determine treatment effectiveness [32]. Assessments were performed at baseline, after the initial treatment and at weeks 2, 6, and 10 after the initiation of treatment. The Chinese version, WOMAC LK3.1, consists of 24 items divided into 3 subscales: pain (5 items), stiffness (2 items), and physical function (17 items). If both knees were affected, the most painful knee was assessed [31, 33–35]. Adverse events were observed by laser technicians and documented at each visit.
2.3. Statistical Analysis
Since this study was a first step to evaluate the usefulness of TCM pattern diagnosis in the effectiveness study of this new laser treatment, we designed a relatively small pilot study with more intensive repeated measures per patients (for improving the power). The sample size requirement for each TCM pattern group is
| (1) |
m is the number of repeated measures per subject, Δ is the effect size, and ρ is the intercorrelation among repeated measures. Some reference values were estimated based on our previously reported clinical trials with this laser device [22, 23]. Since our current study is a pilot study for detecting the relative big signals, the effective size (Δ) for our study is 0.7. The intercorrelation ρ is about 0.8, α = 0.05, with the power (1 − β) of 80%. So, the sample size required for each group is 26. More sample size requirements for rationales with different setting of effect sizes (Δ) and ρ are listed in the appendix. To compare WOMAC score changes pre- and post-treatment, pair t-test was used. To determine the differences between the two TCM pattern groups, change from baseline was compared at each treatment using the equation [(Baseline − Post-treatment)/Baseline × 100%]. Normal distribution test and Levene's test for equality of variances for WOMAC scores of different groups and at different treatment stages were conducted to check their normality and equal variance assumptions. ANOVA was conducted to test difference among groups for each time point of assessment. Statistical significance was set that P value is below 0.05.
Multivariate linear regression for each time point was conducted to determine whether TCM pattern could influence treatment effect after controlling the confounding effects from age, gender, duration of disease, and number of affected knees. The rates of pain, stiffness, and function impairment reduction after treatment were the dependent variable; the other factors were the independent variables. Regression coefficients for TCM patterns are reported for each time points.
3. Results
A total of 103 participants were assessed for eligibility. Fifty-two knee OA patients who met the inclusion/exclusion criteria were included in the study and allocated into the yang deficient (Group A) or the non-yang deficient group (Group B). One patient in Group A dropped out prior to the treatment due to a knee injury. None of the other participants was lost to followup (Figure 2).
Figure 2.
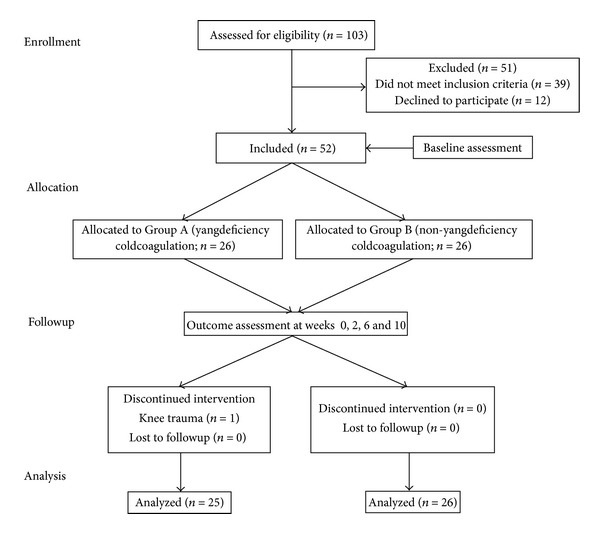
Flow chart of patient recruitment.
There was no statistically significant difference in the baseline characteristics of age, affected knees, and duration of disease between the two groups. Gender distribution was significantly different with more women in the yang deficient group than in the non-yang deficient group (Table 1).
Table 1.
Baseline patient characteristics.
| Group A. Yang deficiency |
Group B. Non-yang deficiency | |
|---|---|---|
| (n = 25) | (n = 26) | |
| Age (years) | 62.36 | 63.04 |
| Gender (F/M) | 20/5 | 14/12* |
| Affected knees (bilateral/single) | 16/9 | 18/8 |
| Durations (year) | 8.08 | 7.46 |
*P < 0.05. There was no difference at baseline in group characteristics except for gender. There were more female patients in Group A.
Patients improved significantly in all three WOMAC score subcategories after week 2 of treatment in all patients combined (Table 2). There were no significant differences between the two groups in WOMAC baseline scores. At each time point of the outcome assessment, there was no statistically significant difference between the two groups in WOMAC pain or stiffness scores. However, WOMAC function scores of [Group A] (yang deficiency cold coagulation) significantly improved compared to those of [Group B] after initial treatment (P = 0.049), at week 2 (P = 0.046) and week 6 (P = 0.042; Table 3). No adverse events were observed in either group.
Table 2.
WOMAC score changes from baseline (Group A and Group B combined, n = 51).
| Pain | Stiffness | Function | |
|---|---|---|---|
| 95% CI | 95% CI | 95% CI | |
| First treatment | −4.98 [−9.38, −0.58]* | −4.27 [−9.34,0.79] | −2.12 [−5.63,1.39] |
| wk 2 | −14.57 [−19.45, −9.70]** | −15.79 [−22.77, −8.82]** | −9.65 [−14.17, −5.12]** |
| wk 6 | −15.29 [−20.63, −9.94]** | −17.76 [−24.04, −11.48]** | −11.75 [−16.61, −6.89]** |
| wk 10 | −17.63 [−23.01, −12.25]** | −19.48 [−25.88, −13.08]** | −13.60 [−18.38, −8.81]** |
*P value < 0.05 compared to baseline.
**P value < 0.001 compared to baseline.
Table 3.
Percentage changes in WOMAC score values from baseline (mean ± SD) [(baseline − posttreatment)/baseline × 100%].
| Group A (diff %) (n = 25) |
Group B (diff %) (n = 26) |
P value | Total (diff %) | ||
|---|---|---|---|---|---|
| Pain | Initial treatment | 8.98 ± 42.46 | −3.07 ± 70.3 | 0.443 | 2.6 ± 58.1 |
| Week 2 | 37.72 ± 36.32 | 32.57 ± 40.63 | 0.634 | 35.09 ± 38.28 | |
| Week 6 | 50.28 ± 35.55 | 30.3 ± 55.59 | 0.132 | 40.10 ± 47.47 | |
| Week 10 | 51.25 ± 40.24 | 42.45 ± 54.95 | 0.516 | 46.76 ± 48.03 | |
|
| |||||
| Stiffness | Initial treatment | −75.7 ± 358.31 | −30.67 ± 110.22 | 0.552 | −54.71 ± 260.86 |
| Week 2 | −2.44 ± 125.39 | −9.13 ± 136.97 | 0.856 | −6.01 ± 130.02 | |
| Week 6 | 30.01 ± 74.74 | 22 ± 67.94 | 0.691 | 25.11 ± 70.42 | |
| Week 10 | 40.29 ± 55.50 | 18.59 ± 111.20 | 0.381 | 27.13 ± 89.36 | |
|
| |||||
| Function | Initial treatment | 10.93 ± 33.68* | −21.5 ± 73.00 | 0.049 | −5.60 ± 58.96 |
| Week 2 | 36.18 ± 29.74* | 12.25 ± 50.85 | 0.046 | 23.98 ± 43.16 | |
| Week 6 | 47.67 ± 29.67* | 24.15 ± 48.32 | 0.042 | 35.68 ± 41.61 | |
| Week 10 | 51.52 ± 34.66 | 33.15 ± 42.71 | 0.098 | 42.15 ± 39.68 | |
*P value < 0.05 compared to Group B.
Regression analysis shows that at weeks 2, 6, and 10, WOMAC function score improvement is significantly associated with TCM pattern; pain and stiffness scores are not (Table 4).
Table 4.
Influence of TCM pattern on WOMAC score improvement rate from baseline using multivariate regression analysis controlling confounding.
| Pain/TCM | Stiffness/TCM | Function/TCM | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient | SE | P | Coefficient | SE | P | Coefficient | SE | P | |
| 1st treatment | −0.134 | 0.169 | 0.432 | 0.115 | 0.791 | 0.885 | −0.296 | 0.17 | 0.089 |
| wk 2 | −0.131 | 0.102 | 0.205 | −0.28 | 0.401 | 0.488 | −0.27 | 0.118 | 0.027* |
| wk 6 | −0.257 | 0.132 | 0.057 | −0.171 | 0.216 | 0.432 | −0.293 | 0.111 | 0.012* |
| wk 10 | −0.15 | 0.139 | 0.288 | −0.408 | 0.260 | 0.123 | −0.265 | 0.108 | 0.019* |
*P < 0.05 indicates a positive correlation between the yang deficiency cold coagulation pattern and treatment effect.
Regression analysis also reveals positive association between symptom improvement and several other factors: the longer the duration of disease and the older the patient, the less improvement in pain and function; the more severe the pain, stiffness, and function impairment, the more effective the treatment (data not shown).
4. Discussion
In our previous two-arm randomized controlled trials, we found the combined 10.6 μm–650 nm laser to be safe and significantly more effective on patients with knee OA than a sham control, as shown by WOMAC pain scores at week 2 [22, 23]. The results of the present trial are consistent with the data of those trials. The WOMAC pain score improvement rate at week 2 of the treatment reached 35%. A rate of 40% improvement was observed after 6 weeks of treatment, and improvement rose to 46.76% during the four-week followup after completion of the treatment (Table 2).
Although randomized controlled trials (RCTs) are still the gold standard for evaluating the safety and efficacy of an intervention, their major limitation is that they might not reflect actual clinical practice [34]. In recent years, suggestions have been raised in the research community regarding the need for patient-centered, pragmatic research under real-life conditions in order to determine which intervention is optimal for which patient [36–38]. Traditional Chinese acupuncture practice often requires individualized treatment based on TCM pattern differentiation [39]. Consequently, treatment can vary from patient to patient and is often complex, involving several modalities such as acupuncture, moxibustion, cupping, or electrical stimulation. In the present study, we employed TCM pattern differentiation to determine whether thermal laser acupuncture is more effective on patients diagnosed with the TCM pattern yang deficiency and cold stagnation than on those with other TCM patterns.
Our results show that although patients in both groups markedly improved from baseline after the laser treatment, a clear trend indicates that more improvement in WOMAC subcategories of pain and stiffness among the yang deficient patients of Group A than among those in the non-yang deficient patients of Group B. In WOMAC function score, Group A significantly improved compared to Group B at almost all assessed time points (Table 3). Furthermore, our secondary regression analysis showed a significant positive correlation between yang deficiency and treatment effect in WOMAC function at all time points after week 2 (Table 4). These findings suggest that TCM pattern differentiation should guide the use of treatment techniques in acupuncture practice and might be important in designing future clinical trials with TCM interventions that might maximize treatment effect [40].
A major limitation of this study is that the patients in this trial were not randomized due to the nature of such study that may cause a selection bias. In order to minimize such bias, we separated TCM practitioner who made the TCM pattern diagnosis from those who performed laser treatments. To control this selection bias, multivariate linear regressions were used to control the potential confounding effects. In future study, we want to use some advanced longitudinal analysis approaches (e.g., random effect models) to evaluate the usefulness of TCM pattern diagnosis in the effectiveness assessment of this laser treatment, controlling not only the confounding effects from observed covariates but also the unobserved heterogeneity across patients. However, such mixed model approach was not carried on in current study due to technical limitation. It was our intention that this study was a first step to evaluate the usefulness of TCM pattern diagnosis in this effectiveness study which reflects daily TCM practice by individual practitioners. A future larger study is needed to confirm the findings of the present study.
We are aware that the improvement rate in function is inconsistent with that of pain, a finding similar to that reported in a large clinical trial of acupuncture on knee OA, in which function but not pain improvement was observed after eight weeks of acupuncture treatment [31]. We speculate a possible reason for this inconsistency is that patients with improved function are likely to increase their physical activity, which might minimize their pain relief. Alternatively, the sample size of the present study might have been insufficient, particularly for a comparative outcome study in which data from two active treatment groups was compared [41].
It is interesting to note that more women are in yang deficient group than in the non-yang deficient group. While we cannot determine the reason for this difference, we speculate that this might be explained by TCM theory that women are overall a yin predominant pattern as compare to men who are generally more in yang predominant pattern. Alternative reason could be our small sample size so that this gender difference did happen by chance.
The mechanisms of laser irradiation have been widely studied in recent years [42, 43]. It has been reported that the 650 nm laser can penetrate the skin to between 10 and 25 mm [13, 17]. Research data also suggest that the significant pain relief in OA patients treated with low level lasers such as the 650 nm is the result of the laser's induction of neurotransmitters, which are important in endogenous pain modulation [44]. Because of its unique characteristics, which are similar to those of acupuncture needle treatment, 650 nm laser irradiation has been used as an alternative for acupuncture [22, 23]. In contrast to the low level laser, the CO2 laser radiation at 10.6 μm wavelength, a far-infrared light, has a fairly persistent thermal effect [45] that can penetrate approximately 50 μm into the body [46]. The radiant energy is absorbed by the superficial layers of the skin, resulting in a rise in skin temperature [47]. The thermal nature of this 10.6 μm laser therefore is similar to the thermal effect of traditional moxibustion.
In conclusion, our study suggests that (1) TCM pattern differentiation, which has been widely practiced for centuries, should play an important role in TCM practice, and (2) thermal laser acupuncture at combined 10.6 μm–650 nm wavelengths is safe and useful in treating yang deficient knee OA patients. Due to the small sample size and possible patient selection bias of this trial, a larger, randomized pragmatic clinical trial is warranted.
Acknowledgments
The authors thank Drs. Yue-long Cao of Shuguang Hospital and Hai-ou Yang of Shanghai First People's Hospital for providing their medical expertise in the trial and thank the students of Shanghai University of Traditional Chinese Medicine Min Wang and Hong Qi for their assistance during the trial. Thanks are to Dr. Xiang-Hua Ying of Shanghai Sixth People's Hospital for providing statistical analysis assistance. The authors would also like to thank Dr. Lyn Lowry for her editorial assistance. The project was supported by the National Basic Research Program of China (2009CB522901), National Natural Science Foundation of China (81202648), the Key Program of State Administration of Traditional Chinese Medicine of China, and the Shanghai Municipal Science Foundation (11DZ1973300 and SZY10010).
Appendix
See Table 5.
Table 5.
Sample sizes for rationales of different effect sizes (Δ) and ρ.
| ρ | Δ (%) | |||
|---|---|---|---|---|
| 50% | 60% | 70% | 80% | |
| 0.5 | 34 | 24 | 18 | 14 |
| 0.6 | 40 | 28 | 21 | 16 |
| 0.7 | 46 | 32 | 23 | 18 |
| 0.8 | 51 | 36 | 26 | 20 |
| 0.9 | 57 | 40 | 29 | 23 |
References
- 1.Bijlsma JWJ, Berenbaum F, Lafeber FPJG. Osteoarthritis: an update with relevance for clinical practice. The Lancet. 2011;377(9783):2115–2126. doi: 10.1016/S0140-6736(11)60243-2. [DOI] [PubMed] [Google Scholar]
- 2.Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis and Rheumatism. 1998;41:778–799. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 3.Felson DT, Lawrence RC, Dieppe PA, et al. Osteoarthritis: new insights—part 1: the disease and its risk factors. Annals of Internal Medicine. 2000;133(8):635–646. doi: 10.7326/0003-4819-133-8-200010170-00016. [DOI] [PubMed] [Google Scholar]
- 4.National Collaborating Centre for Chronic Conditions. Osteoarthritis: National Clinical Guideline for Care and Management in Adults. London, UK: Royal College of Physicians; 2008. http://www.nice.org.uk/CG59. [PubMed] [Google Scholar]
- 5.Tramèr MR, Moore RA, Reynolds DJM, McQuay HJ. Quantitative estimation of rare adverse events which follow a biological progression: a new model applied to chronic NSAID use. Pain. 2000;85(1-2):169–182. doi: 10.1016/s0304-3959(99)00267-5. [DOI] [PubMed] [Google Scholar]
- 6.Silverstein FE, Faich G, Goldstein JL, et al. Gastrointestinal toxicity with Celecoxib vs nonsteroidal anti-inflammatory drugs for osteoarthritis and reumatoid arthritis: the CLASS study: a randomized controlled trial. Journal of the American Medical Association. 2000;284(10):1247–1255. doi: 10.1001/jama.284.10.1247. [DOI] [PubMed] [Google Scholar]
- 7.Cao L, Zhang XL, Gao YS, Jiang Y. Needle acupuncture for osteoarthritis of the knee. A systematic review and updated meta-analysis. Saudi Medical Journal. 2012;33(5):526–532. [PubMed] [Google Scholar]
- 8.Yang C. Acupuncture-Moxibustion Therapeutics. Shanghai, China: Shanghai Science & Technology Press; 1988. [Google Scholar]
- 9.Chen R, Chen M, Xiong J, et al. Is there difference between the effects of two-dose stimulation for knee osteoarthritis in the treatment of heat-sensitive moxibustion? Evidence-Based Complementary and Alternative Medicine. 2012;2012:7 pages. doi: 10.1155/2012/696498.696498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li CD, Huang XY, Yang XG, Wang QF, Huang SQ. Observation on therapeutic effect of warming needle moxibustion on knee osteoarthritis of deficiency-cold type. Zhongguo Zhen Jiu. 2006;26(3):189–191. [PubMed] [Google Scholar]
- 11.Park JS, Kwon SJ, Kwon YS. The effects of Dogbi(ST35) & Sulan moxibustion on knee joint pain, range of motion and discomfort during ADL in the aged. Taehan Kanho Hakhoe Chi. 2006;36(1):189–196. doi: 10.4040/jkan.2006.36.1.189. [DOI] [PubMed] [Google Scholar]
- 12.Vas J, Perea-Milla E, Méndez C. Acupuncture and moxibustion as an adjunctive treatment for osteoarthritis of the knee—a large case series. Acupuncture in Medicine. 2004;22(1):23–28. doi: 10.1136/aim.22.1.23. [DOI] [PubMed] [Google Scholar]
- 13.Ackermann G, Hartmann M, Scherer K, et al. Correlations between light penetration into skin and the therapeutic outcome following laser therapy of port-wine stains. Lasers in Medical Science. 2002;17(2):70–78. doi: 10.1007/s101030200013. [DOI] [PubMed] [Google Scholar]
- 14.Aimbire F, Albertini R, Pacheco MTT, et al. Low-level laser therapy induces dose-dependent reduction of TNFα levels in acute inflammation. Photomedicine and Laser Surgery. 2006;24(1):33–37. doi: 10.1089/pho.2006.24.33. [DOI] [PubMed] [Google Scholar]
- 15.Lopes-Martins RAB, Albertini R, Lopes Martins PSL, Bjordal JM, Faria Neto HCC. Spontaneous effects of low-level laser therapy (650 nm) in acute inflammatory mouse pleurisy induced by carrageenan. Photomedicine and Laser Surgery. 2005;23(4):377–381. doi: 10.1089/pho.2005.23.377. [DOI] [PubMed] [Google Scholar]
- 16.Schubert MM, Eduardo FP, Guthrie KA, et al. A phase III randomized double-blind placebo-controlled clinical trial to determine the efficacy of low level laser therapy for the prevention of oral mucositis in patients undergoing hematopoietic cell transplantation. Supportive Care in Cancer. 2007;15(10):1145–1154. doi: 10.1007/s00520-007-0238-7. [DOI] [PubMed] [Google Scholar]
- 17.Whittaker P. Laser acupuncture: past, present, and future. Lasers in Medical Science. 2004;19:69–80. doi: 10.1007/s10103-004-0296-8. [DOI] [PubMed] [Google Scholar]
- 18.Gungor A, Dogru S, Cincik H, Erkul E, Poyrazoglu E. Effectiveness of transmeatal low power laser irradiation for chronic tinnitus. Journal of Laryngology and Otology. 2008;122(5):447–451. doi: 10.1017/S0022215107009619. [DOI] [PubMed] [Google Scholar]
- 19.Glazov G, Schattner P, Lopez D, Shandley K. Laser acupuncture for chronic non-specific low back pain: a controlled clinical trial. Acupuncture in Medicine. 2009;27(3):94–100. doi: 10.1136/aim.2009.000521. [DOI] [PubMed] [Google Scholar]
- 20.Baxter GD, Bleakley C, McDonough S. Clinical effectiveness of laser acupuncture: a systematic review. JAMS Journal of Acupuncture and Meridian Studies. 2008;1(2):65–82. doi: 10.1016/S2005-2901(09)60026-1. [DOI] [PubMed] [Google Scholar]
- 21.Brosseau L, Robinson V, Wells G, et al. WITHDRAWN: low level laser therapy (Classes III) for treating osteoarthritis. Cochrane Database of Systematic Reviews. 2007;(1) doi: 10.1002/14651858.CD002046.pub3.CD002046 [DOI] [PubMed] [Google Scholar]
- 22.Zhao L, Shen X, Cheng K, et al. Validating a nonacupoint sham control for laser treatment of knee osteoarthritis. Photomedicine and Laser Surgery. 2010;28(3):351–356. doi: 10.1089/pho.2009.2511. [DOI] [PubMed] [Google Scholar]
- 23.Shen X, Zhao L, Ding G, et al. Effect of combined laser acupuncture on knee osteoarthritis: a pilot study. Lasers in Medical Science. 2009;24(2):129–136. doi: 10.1007/s10103-007-0536-9. [DOI] [PubMed] [Google Scholar]
- 24.Hochberg MC, Altman RD, Brandt KD, et al. Guidelines for the medical management of osteoarthritis—part I: osteoarthritis of the hip. Arthritis and Rheumatism. 1995;38(11):1535–1540. doi: 10.1002/art.1780381103. [DOI] [PubMed] [Google Scholar]
- 25.Xiong G-P, Huang Q, Dong Y-F. Thirty cases of knee osteoarthritis treated by acupuncture and warming needle moxibustion. Zhongguo Zhen Jiu. 2011;31(6):551–552. [PubMed] [Google Scholar]
- 26.Ding M-H, Zhang H, Li Y. A randomized controlled study on warming needle moxibustion for treatment of knee osteoarthritis. Zhongguo Zhen Jiu. 2009;29(8):603–607. [PubMed] [Google Scholar]
- 27.Wang SS, Zhang SH, Qiu HM, et al. The National Industrial Standard of Traditional Chinese Medicine: The Treatment Effect Standard of TCM Disease and Syndrome. Beijing, China: Chinese Publication of Traditional Chinese Medicine; 2002. [Google Scholar]
- 28.Cheng X. Chinese Acupuncture and Moxibustion. Beijing, China: Foreign Languages Press; 1999. [Google Scholar]
- 29.Sangdee C, Teekachunhatean S, Sananpanich K, et al. Electroacupuncture versus Diclofenac in symptomatic treatment of osteoarthritis of the knee: a randomized controlled trial. BMC Complementary and Alternative Medicine. 2002;2(article 3) doi: 10.1186/1472-6882-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tukmachi E, Jubb R, Dempsey E, Jones P. The effect of acupuncture on the symptoms of knee osteoarthritis—an open randomised controlled study. Acupuncture in Medicine. 2004;22(1):14–22. doi: 10.1136/aim.22.1.14. [DOI] [PubMed] [Google Scholar]
- 31.Berman BM, Lao L, Langenberg P, Lee WL, Gilpin AMK, Hochberg MC. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee. A randomized, controlled trial. Annals of Internal Medicine. 2004;141(12):901–910. doi: 10.7326/0003-4819-141-12-200412210-00006. [DOI] [PubMed] [Google Scholar]
- 32.Bellamy N. WOMAC Osteoarthritis Index User Guide VII Appendix I 3.1/3.0 VA, (Chinese Mandarin), 2004.
- 33.Vas J, Méndez C, Perea-Milla E, et al. Acupuncture as a complementary therapy to the pharmacological treatment of osteoarthritis of the knee: randomized controlled trial. British Medical Journal. 2004;329:1216–1220. doi: 10.1136/bmj.38238.601447.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bálint GP, Buchanan WW, Ádám A, et al. The effect of the thermal mineral water of Nagybaracska on patients with knee joint osteoarthritis-a double blind study. Clinical Rheumatology. 2007;26:890–894. doi: 10.1007/s10067-006-0420-1. [DOI] [PubMed] [Google Scholar]
- 35.Scharf H-P, Mansmann U, Streitberger K, et al. Acupuncture and knee osteoarthritis: a three-armed randomized trial. Annals of Internal Medicine. 2006;145(1):12–20. doi: 10.7326/0003-4819-145-1-200607040-00005. [DOI] [PubMed] [Google Scholar]
- 36.Witt CM, Huang WJ, Lao L, Bm B. Which research is needed to support clinical decision-making on integrative medicine?—can comparative effectiveness research close the gap? Chinese Journal of Integrative Medicine. 2012;18(10):723–729. doi: 10.1007/s11655-012-1255-z. [DOI] [PubMed] [Google Scholar]
- 37.Wu AW, Snyder C, Clancy CM, Steinwachs DM. Adding the patient perspective to comparative effectiveness research. Health Affairs. 2010;29(10):1863–1871. doi: 10.1377/hlthaff.2010.0660. [DOI] [PubMed] [Google Scholar]
- 38.Tunis SR, Stryer DB, Clancy CM. Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. Journal of the American Medical Association. 2003;290(12):1624–1632. doi: 10.1001/jama.290.12.1624. [DOI] [PubMed] [Google Scholar]
- 39.Zhang GG, Singh B, Lee W, Handwerger B, Lao L, Berman B. Improvement of agreement in TCM diagnosis among TCM practitioners for persons with the conventional diagnosis of rheumatoid arthritis: effect of training. Journal of Alternative and Complementary Medicine. 2008;14(4):381–386. doi: 10.1089/acm.2007.0712. [DOI] [PubMed] [Google Scholar]
- 40.Lu C, Zha Q, Chang A, He Y, Lu A. Pattern differentiation in traditional chinese medicine can help define specific indications for biomedical therapy in the treatment of rheumatoid arthritis. Journal of Alternative and Complementary Medicine. 2009;15(9):1021–1025. doi: 10.1089/acm.2009.0065. [DOI] [PubMed] [Google Scholar]
- 41.Witt CM, Aickin M, Baca T, et al. Effectiveness guidance document (EGD) for acupuncture research—a consensus document for conducting trials. BMC Complementary and Alternative Medicine. 2012;12(article 148) doi: 10.1186/1472-6882-12-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bjordal JM, Couppé C, Chow RT, Tunér J, Ljunggren EA. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Australian Journal of Physiotherapy. 2003;49(2):107–116. doi: 10.1016/s0004-9514(14)60127-6. [DOI] [PubMed] [Google Scholar]
- 43.Yan W, Chow R, Armati PJ. Inhibitory effects of visible 650-nm and infrared 808-nm laser irradiation on somatosensory and compound muscle action potentials in rat sciatic nerve: implications for laser-induced analgesia. Journal of the Peripheral Nervous System. 2011;16(2):130–135. doi: 10.1111/j.1529-8027.2011.00337.x. [DOI] [PubMed] [Google Scholar]
- 44.Brosseau L, Welch V, Wells G, et al. Low level laser therapy for osteoarthritis and rheumatoid arthritis: a metaanalysis. Journal of Rheumatology. 2000;27(8):1961–1969. [PubMed] [Google Scholar]
- 45.Makihara E, Makihara M, Masumi S-I, Sakamoto E. Evaluation of facial thermographic changes before and after low-level laser irradiation. Photomedicine and Laser Surgery. 2005;23(2):191–195. doi: 10.1089/pho.2005.23.191. [DOI] [PubMed] [Google Scholar]
- 46.Biehl R, Treede RD, Bromm B. Pain ratings and short radiant heat pulses. In: Bromm B, editor. Pain Measurement in Man: Neurophysiological Correlates of Pain. Amsterdam, The Netherlands: Elsevier; 1984. pp. 397–408. [Google Scholar]
- 47.Al-Saadi MH, Nadeau V, Dickinson MR. A novel modelling and experimental technique to predict and measure tissue temperature during CO2 laser stimuli for human pain studies. Lasers in Medical Science. 2006;21(2):95–100. doi: 10.1007/s10103-006-0381-2. [DOI] [PubMed] [Google Scholar]


