Abstract
Objective
To cross-validate the psychometric properties of the abbreviated Late-Life Function and Disability Instrument (LL-FDI), a measure of perceived functional limitations and disability.
Design
Baseline and 12-month follow-up assessments conducted across the course of a 12-month exercise program.
Setting
University research community.
Participants
Older healthy adults (N=179; mean ± SD age, 66.43±5.67y) at baseline; 145 were retained at follow-up.
Interventions
Not applicable.
Main Outcome Measures
LL-FDI and functional performance measures.
Results
Factor analyses confirmed the factor structure of the abbreviated LL-FDI, and all subscales met minimal criteria for temporal invariance. Significant correlations also were found between functional limitations subscales and an array of physical function performance measures, supporting the scale’s construct validity.
Conclusions
The abbreviated LL-FDI with some modifications appears to be temporally invariant in community-dwelling older adults. Additionally, moderate relationships between functional limitations and functional performance provide further support for these being conceptually distinct constructs.
Keywords: Geriatrics, Longitudinal studies, Psychometrics, Rehabilitation
The incidence of functional limitations and disability increases with age and chronic disease.1 Such increases have important implications for physical and emotional well-being and quality of life. There have been numerous calls in the medical and gerontologic literature for consistency in defining functional limitations and disability and accuracy in measuring these constructs. This has been compounded by failure to distinguish between functional performance and functional limitations and disability.2,3 Functional performance is the extent to which one is capable of performing everyday activities (eg, walking, using stairs, lifting heavy objects), whereas functional limitations refer to decreased capacity to carry out activities essential to independent living. Disabilities involve the expression of functional limitations within the context of one’s sociocultural and physical environment.4
Haley5 and Jette6 and colleagues developed the LL-FDI as a measure that could provide clinicians and researchers with a resource to assess change in function and disability across a wide variety of life tasks. This measure was based firmly in the disablement models of Nagi7 and Vebrugge and Jette8 and is composed of 2 components. The function component assesses how much difficulty one has doing a particular activity without assistance and is made up of 3 subscales: ALEF, BLEF, and UEF. ALEF is defined as activities that involve a high level of physical ability and endurance, including running a half mile and climbing stairs while carrying groceries. BLEF assesses simpler activities, such as standing, stooping, or walking. UEF reflects an activity that requires the use of one’s hands or arms.5 The disability component of the LL-FDI assesses the frequency of and perceived limitations in performing given life tasks.6
McAuley et al9 examined the LL-FDI’s psychometric properties in a sample of older women, resulting in an abbreviated 31-item version of the original 48-item LL-FDI. The abbreviated version consists of a shorter 15-item Functional Limitations scale, 8-item Disability Frequency scale, and 8-item Disability Limitations scale. McAuley9 noted that scores on the abbreviated measure for function and disability correlated very highly (.76–.97) with the original LL-FDI scores. In addition, construct validity for the abbreviated version was supported by the demonstration of significant associations between functional limitations and disability scales and body mass index, physical function performance, and physical activity. In a more recent study, Motl and McAuley10 confirmed the factor structure of the abbreviated LL-FDI in a sample of persons with multiple sclerosis.
We might note that other self-report measures of perceived physical function and disability also have been used in research with older adults, including the SF-36,11 the 12-Item Short Form Health Survey,12 and the rating of ADLs.13 The SF-36, a short form assessment of Medical Outcomes Study questionnaire, was designed as a generic indicator of health status and health-related quality of life11,14,15 and has a physical function component relative to activity restriction and limitations with basic functions (ie, ADLs). The rating of ADLs13 assesses the relative importance of various ADLs in the daily functioning of sedentary people. However, the LL-FDI is unique in that it focuses purely on functional limitations and disability, rather than reflecting health status in general or only physical functions.
The purpose of the present study was to further examine the psychometric properties of the abbreviated LL-FDI by confirming the factor structure in a community-dwelling sample of healthy older adults and, more importantly, determining whether the factor structure remains invariant across time. We adopted a CFA framework to achieve these objectives. The importance of testing invariance cannot be underestimated because detecting change in a construct implies that participants interpret the meaning of survey items differently across measurement occasions. Thus, longitudinal invariance is absolutely essential for one to draw meaningful conclusions across groups and time,16 a vitally important attribute to researchers and clinicians alike. Testing longitudinal invariance involves first establishing configural invariance (ie, same items are regressed on the same constructs at each occasion a priori). This is followed by a stepwise process of constraining factor loadings (ie, metric or weak invariance), factor variances and covariances (ie, scalar or strong invariance), and residuals (ie, strict invariance) to be equal across time. If at any point in the invariance procedure a model is significantly different from the less restrictive model, constraints may be relaxed to optimize the fit. However, this implies that full invariance at the more restrictive step has not been reached. Expecting the factor pattern to show configural invariance is the minimum requirement for longitudinal invariance,17 but Horn and McArdle18 argued that factor analytic models passed a more restrictive weak invariance test. Because few self-report assessments pass strict invariance, we were interested in establishing the minimal criteria, as defined by Horn and McArdle.18
Therefore, this study had 3 aims. First, to confirm the structural validity of the abbreviated LL-FDI in a sample of community-dwelling older adults. Second, to determine the extent to which the LL-FDI was longitudinally invariant. Finally, we further tested the construct validity of the scale by examining associations between functional limitations subscales and measures of functional performance.
METHODS
Recruitment and Participants
Participants were recruited through local media outlets, including television, radio, and print media advertisements. To participate in the exercise program, participants had to meet the criteria of being physically inactive for at least 6 months preintervention, have no medical conditions exacerbated by physical activity participation, be willing to be assigned to an exercise group, and have their personal physician’s consent. Other exclusionary criteria that are not germane to this article are reported elsewhere.19
After initial contact by telephone, participants completed the prescreening interview to determine whether they met the inclusion criteria and consented to have their physician contacted for approval to participate in the exercise intervention. The sample (N=179) was community-dwelling older adults who volunteered to participate in a 12-month exercise intervention and consisted of 62 men and 117 women with a mean ± SD age of 66.43±5.67 years (range, 58–80y). One hundred forty-five participants completed a 12-month follow-up. Most (58.4%) of the sample had an annual household income greater than $40,000 and most (51.5%) had a college degree or higher. Additionally, most (88.3%) of the sample were white and not of Hispanic or Latino (98.3%) descent. This information, as well as the sample’s medical health history, is listed in table 1.
Table 1.
Characteristics of Study Sample
| Variable | Mean ± SD/Frequency (%) |
|---|---|
| Age (y) | 66.43±5.67 |
| Women | 65.4 |
| College graduate or higher | 51.5 |
| Race | |
| White | 88.3 |
| Black | 8.4 |
| Asian | 3.4 |
| Ethnicity | |
| Hispanic/Latino | 1.7 |
| Non-Hispanic/Latino | 98.3 |
| Income >$40,000 | 58.4 |
| Body mass index (kg/m2) | 28.88±4.42 |
| Cardiovascular disease | 5.6 |
| Heart rhythm disorders | 7.8 |
| Peripheral vascular disease | 1.1 |
| Pulmonary disease (asthma) | 7.3 |
| Central nervous system disorders | 0.0 |
| Osteoporosis | 18.4 |
| Severe back problems | 10.6 |
| Severe arthritis | 10.6 |
| Hypertension | 48.0 |
| Hyperlipidemia | 44.1 |
| Diabetes | 11.8 |
| Anemia or bleeding disorder | 3.9 |
| Phlebitis or emboli | 0.6 |
| Cancer | 18.5 |
| Edema | 10.1 |
Measures
Demographic and medical health status
Each participant completed a brief questionnaire that assessed basic demographic information, including age, sex, race, education, and income. Information and details of medical health history including current medications were obtained by using self-report during the initial telephone interview.
Abbreviated LL-FDI
The abbreviated LL-FDI9 was used to assess the degree to which participants reported difficulty executing discrete activities (function) and the degree to which they could perform socially defined life tasks (disability). The function component is composed of 3 subscales assessing ALEF (5 items), BLEF (5 items), and UEF (5 items). The function component assesses the level of difficulty an individual has carrying out tasks and is scored from 1 (cannot do) to 5 (none). Higher scores on the function scales reflect fewer difficulties performing tasks. The disability frequency component uses 8 items to assess the frequency of performing social (4 items) and personal (4 items) role activities. The disability limitations component uses 8 items to assess the extent to which one feels limited in performing social (4 items) and personal (4 items) role activities. Disability frequency is scored from 1 (never) to 5 (very often), and scores for the disability limitations scale range from 1 (completely) to 5 (not at all). Higher scores on disability components reflect lower levels of disability.
Physical function measures
To assess functional performance, we used the Senior Fitness Test,20 a multifaceted test of upper- and lower-body mobility, strength, flexibility, endurance, and balance. Specifically, lower-body function was assessed by using the 30-second chair stand test and the 8-foot up and go tests, which assess leg strength. All tasks were completed by using the standard administration processes described in the Senior Fitness Test manual. Participants also performed a stair-climbing task in which they were required to walk up and down a flight of 10 stairs as quickly as possible without using the hand rail for assistance. Time (in seconds) to complete each task was recorded on a handheld stopwatch. To assess balance and lower-extremity function, participants were asked to balance on 1 leg for up to 30 seconds. Time was recorded as the second the participant’s opposite foot touched the ground. The balance task was completed on both the right and left legs. Finally, as a measure of endurance, all participants completed the Rockport 1-mile walk protocol.21 Participants walked in groups on an enclosed synthetic track and were instructed to complete the 1-mile walk as quickly as possible without running. Time (in minutes) to complete the test was recorded on a handheld stopwatch.
Procedures
The study was approved by an institutional review board at the University of Illinois Urbana-Champaign, and all participants signed an informed consent document before the start of the exercise program. Participants expressing an initial interest in the study were prescreened by a staff member who determined contact information and whether the prospective participant met inclusion/exclusion criteria. If all initial inclusion criteria were met, a medical health history was collected. No additional study measures were collected at this time. After participants passed screening and received physician approval to participate in the exercise intervention, they completed a baseline questionnaire packet that included the demographic questionnaire and abbreviated LL-FDI. Additionally, participants completed the physical performance tests during a visit to our laboratory. However, the Rockport 1-mile walk was completed on a separate day to avoid fatigue. Participants completed the abbreviated LL-FDI and all functional assessments again at the end of the 12-month intervention.
Data Analysis
Structural validity
We initially assessed the structural validity of the model by examining the fit of the measurement models for the components of the abbreviated LL-FDI using CFA with FIML estimation in Mplus.22,a FIML is an optimal method for the treatment of missing data in structural equation modeling and has yielded accurate parameter estimates and fit indexes with simulated missing data.23,24 Missing data comprised 0% of the total data set at baseline and 19% at follow-up. Item loadings were estimated for 2 latent factors representing disability frequency and limitations components and 3 latent factors representing the function component.
Model fit
Multiple indexes were examined to determine whether the model represented a reasonable fit to the data. The chi-square statistic is a classic test that assesses the exact fit of the model to the data, but because it is sensitive to sample size, use of other fit indexes is recommended.25-27 The SRMR represents the average of the standardized residuals between the specified and obtained variance-covariance matrices. The SRMR should be less than .08 to indicate good model fit.28 The RMSEA represents closeness of fit, with values less than .08 and .05 showing reasonable and close fit of the model to the data, respectively.29 RMSEA values approximating zero show exact fit of the model. Finally, we used the CFI,30 for which a value of .95 or greater indicates good model-data fit and .90 reflects acceptable fit.28,30 Although standard cutoff values may suggest an ill-fitting model when fit indexes are outside the reference range, Babyak and Greene31 cautioned that these fit indexes should be treated as “rough and ready rules of thumb,” rather than absolute criteria. Other measurement specialists also have shown that these criteria are sensitive to sample size and model type.32-34 We therefore followed minimal criteria given our relatively small sample size and model complexity.
Longitudinal invariance
After structural validity at time 1 was determined, longitudinal invariance for the abbreviated LL-FDI from baseline to 12-month follow-up was tested. We used the chi-square statistic, SRMR, RMSEA, and CFI to evaluate model fit.33 Evidence of invariance of parameters between nested models was based on nonsignificant chi-square difference tests, along with change in CFI less than .01.35,36
Construct validity
To assess construct validity, we examined the degree of concordance (convergent validity) by examining correlations between LL-FDI subscales and performance measures.
RESULTS
Structural Validity of the Abbreviated LL-FDI
Preliminary analyses
Data initially were analyzed to assess normality assumptions. Responses to items were mostly normal, but some items showed little variability in responses (eg, scores of only 4 and 5 on a 5-point scale). These dichotomous items were viewed as problematic and were monitored closely in subsequent analyses.
Function component
The original 3-factor model consisting of ALEF, BLEF, and UEF provided a reasonable fit to the data, but one that could be improved on (χ2=188.50 [87]; P<.01; SRMR=.06; RMSEA=.08 [95% CI, .07–.10]; CFI=.90). Further inspection of the items showed lack of variability in items 4 (holding a glass of water) and 15 (walking around home). Note that 95% and 96.1% of our sample (at times 1 and 2, respectively) reported “none” to these respective items, indicating no problems with such tasks; less than 5% indicated “a little” or “some” difficulty. We therefore used exploratory structural equation modeling37 to reassess factor structure without items 4 or 15. This analysis suggested that item 3 (using common utensils) also should be dropped because of its low loading (.25) on the upper-extremity factor. After removal of these items, the model fit well (χ2=75.30 [66]; P=.02; SRMR=.04; RMSEA=.05 [95% CI, .02–.08]; CFI=97). Factor loadings are listed in table 2.
Table 2.
Standardized Factor Loadings for Abbreviated Function Scales at Baseline and 12 Months
| Items | Factor Loadings
|
|
|---|---|---|
| Baseline | 12 mo | |
| ALEF | ||
| Run one-half mile (F2) | .39 | .37 |
| Walk 1 mile with rests (F5) | .54 | .63 |
| Go up and down 1 flight, no rails (F6) | .88 | .86 |
| Go up and down 3 flights inside (F10) | .73 | .76 |
| Carry something while using stairs (F13) | .84 | .90 |
| BLEF | ||
| Get into and out of car (F9) | .76 | .76 |
| Picking up chair and moving (F11) | .67 | .68 |
| Use step stool to reach (F12) | .65 | .57 |
| Bend over to pick up (F14) | .61 | .69 |
| UEF | ||
| Unscrew lid without assistive devices (F1) | .63 | .67 |
| Remove wrapping with hands only (F7) | .80 | .75 |
| Pour from a large pitcher (F8) | .66 | .76 |
NOTE. Item labels reflect those shown in figure 1.
Disability component: frequency items
Attempts to confirm the original factor structure would not produce admissible results (ie, covariance matrix could not be inverted) with the inclusion of item 6 (ability to take care of personal needs; eg, bathing, dressing, toileting). Participants used only 2 categories, “very often” (97.2%) and “often” (2.8%), to indicate how frequently they engaged in personal care. After removing item 6 from the model, a 2-factor structure was confirmed that reflected personal and social roles for the 7-item Disability Frequency component. The model fit the data well (χ2=17.19 [13]; P=.19; SRMR=.05; RMSEA=.04 [95% CI, .00–.09]; CFI=.97). Factor loadings are listed in table 3.
Table 3.
Factor Loadings for 7-Item Disability Frequency Scales at Baseline and 12 Months
| Items | Factor Loadings
|
|
|---|---|---|
| Baseline | 12 mo | |
| Personal | ||
| Take care of household business (D2A) | .49 | .45 |
| Take care of local errands (D7A) | .48 | .51 |
| Prepare meals (D8A) | .37 | .46 |
| Social | ||
| Visit friends (D1A) | .70 | .77 |
| Travel out of town (D3A) | .46 | .55 |
| Invite family and friends into home (D4A) | .67 | .70 |
| Go to public places (D5A) | .56 | .56 |
NOTE. Item labels reflect those shown in figure 1.
Disability component: limitations items
Similarly, inclusion of item 6 in the 2-factor model (personal and social roles) did not converge on an admissible solution. The modified 7-item Disability Limitations model provided adequate fit with the exception of the RMSEA value, which was well outside the reference range (χ2=38.59 [13]; P<.01; SRMR=.09; RMSEA=.11 [95% CI, .07–.14]; CFI=.93). Browne and Cudeck29 suggested that RMSEA indicates a poor-fitting model if values exceed .10, leading us to anticipate difficulties with further longitudinal invariance testing of this particular model. Based on content overlap (ie, item 2, taking care of errands inside the house, and item 7, taking care of errands outside the house), we allowed a correlated uniqueness between these items and reran the model. After these modifications, the model provided an excellent fit to the data (χ2=15.92 [13]; P=.19; SRMR=.03; RMSEA=.04 [95% CI, .00–.09]; CFI=.99). Factor loadings are listed in table 4.
Table 4.
Factor Loadings for 7-Item Disability Limitations Scales at Baseline and 12 Months
| Items | Factor Loadings
|
|
|---|---|---|
| Baseline | 12 mo | |
| Personal | ||
| Take care of household business (D2B) | .72 | .41 |
| Take care of local errands (D7B) | .74 | .77 |
| Prepare meals (D8B) | .31 | .59 |
| Social | ||
| Visit friends (D1B) | .72 | .81 |
| Travel out of town (D3B) | .70 | .69 |
| Invite family and friends into home (D4B) | .76 | .68 |
| Go to public places (D5B) | .74 | .77 |
NOTE. Item labels reflect those shown in figure 1.
In sum, CFAs of baseline measures resulted in an overall decrease in the 31-item abbreviated LL-FDI to a 26-item instrument (fig 1), with 3 subscales that each fit the data well. A 12-item Function scale was retained (items 3, 4, and 15 removed) in addition to 7-item Disability Frequency and Disability Limitations scales (item 6 removed from each component).
Fig 1.
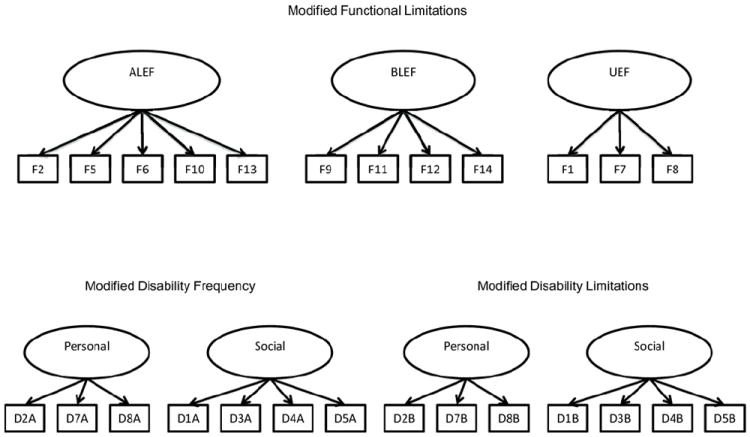
Final model structure for the LL-FDI.
Longitudinal Invariance
Function component
Configural invariance for the modified 3-factor model (ALEF, BLEF, UEF) of the Functional Limitations scale, with items 3, 4, and 15 removed, provided adequate fit to the data (χ2=389.99 [225]; P<.01; SRMR=.07; RMSEA=.06 [95% CI, .05–.08]; CFI=.92). The weak invariance model showed little change in overall fit (χ2=399.63 [234]; P<.01; SRMR=.08; RMSEA=.06 [95% CI, .05–.07]; CFI=.92), and chi-square difference test38 was not significant. Strong invariance also provided similar fit indexes (χ2=416.20 [243]; P<.01; SRMR=.08; RMSEA=.06 [95% CI, .05–.07]; CFI=.91), and chi-square difference was not significant. Thus, we have good evidence for temporal invariance of this component.
Disability component: frequency items
Similar to the procedure above, configural invariance was tested first, and the modified model with item 6 removed provided good fit to the data (χ2=98.53 [64]; P<.01; SRMR=.06; RMSEA=.06 [95% CI, .03–.08]; CFI=.96). Next, the weak invariance model was tested, and this model also provided acceptable fit (χ2=102.84 [69]; P=.01; SRMR=.07; RMSEA=.05 [95% CI, .03–.07]; CFI=.96), and chi-square difference was not significant. Finally, the strong invariance model was tested and showed good fit to the data (χ2=106.64 [74]; P=.01; SRMR=.07; RMSEA=.05 [95% CI, .03–.07]; CFI=.96), and chi-square difference was not significant. Again, we conclude that this component of the abbreviated LL-FDI showed acceptable temporal invariance.
Disability component: limitations items
Configural invariance was tested first to examine the structural integrity of the modified 2-factor Disability Limitations model across time. The model showed adequate fit to the data (χ2=123.27 [62]; P<.01; SRMR=.08; RMSEA=.07 [95% CI, .06–.09]; CFI=.93). However, the weak invariance model did not provide adequate fit to the data (χ2=142.54 [67]; P<.01; SRMR=.11; RMSEA=.08 [95% CI, .06–.10]; CFI=.94), and chi-square difference was significant. We then tested for partial weak invariance by using a backward method of freeing loadings until the weak invariance model no longer significantly differed from the configural model. From this procedure, a model for partial weak invariance on items 1, 3, 4, 5, and 7 across the 2 waves was retained. This model provided better fit to the data (χ2=128.60 [65]; P<.01; SRMR=.10; RMSEA=.07 [95% CI, .06–.09]; CFI=.92), and chi-square difference was not significant. It appears that this component meets the minimal criteria for establishing invariance across time.
Construct Validity: Associations Between Function Limitations and Functional Performance
To assess the convergent validity of our modified LL-FDI, we examined correlations between function component sub-scales with assessments of physical function performance (table 5). Perceptions of ALEF at baseline were significantly (P<.05) related to number of chair stands completed (r=.42), 8-foot up and go time (r=−.45), stairs down (r=−.42) and stairs up time (r=−.44), as well as time an individual could balance on each leg (r=.29, r=.18), Rockport walk time (r=−.42), and number of arm curls completed (r=−.21). These findings suggest that self-assessed ALEF is related primarily to performance on lower-body tasks, but also to tasks that require upper-body strength and balance. Similarly, perceptions regarding BLEF were associated significantly with number of chair stands completed (r=.25), 8-foot up and go time (r=−.27), stairs down (r=−.19) and up time (r=−.23), Rockport time (r=−.19), and number of arm curls completed (r=.21). Perceived UEF at baseline was related significantly to performance on tasks that recruit upper-body strength and flexibility, including arm curls (r=.20) and back scratch (r=−.22). Interestingly, although overall patterns of correlations were similar at baseline and 12 months, there were some differences that perhaps were due to the nature of the intervention. For example, the relationship between UEF and curls was no longer significant (but in the expected direction) at 12 months. Also, BLEF was associated significantly with both right- and left-leg stand at 12 months, but showed no relationship with balance measures at baseline. Together, these findings suggest that the subscales of the modified LL-FDI are associated with relevant physical function performance, and these patterns are similar to those reported in previous research.9
Table 5.
Correlations Between Function Component of the LL-FDI and Physical Function Assessments at Baseline and 12 Months
| Variable | Baseline
|
12 mo
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Chair Stands |
8-ft Up and Go |
Stair Down Time |
Stair Up Time |
Time on Left Leg |
Time on Right Leg |
Total Rockport Time |
No. of Arm Curls |
Back Scratch Length |
No. of Chair Stands |
8-ft Up and Go |
Stair Down Time |
Stair Up Time |
Time on Left Leg |
Time on R ight Leg |
Total Rockport Time |
No. of Arm Curls |
Back Scratch Length |
|
| ALEF at baseline | .42* | −.45* | −.44* | −.42* | .29* | .18† | −.42* | −.21* | .03 | .32* | −.39* | −.45* | .44* | .21† | .08 | −.40* | .19† | −.16 |
| BLEF at baseline | .25* | −.27* | −.19† | −.23* | .13 | .09 | −.19† | .21* | −.01 | .00 | −.10 | −.14 | −.09 | .11 | .01 | −.04 | .05 | −.16 |
| UEF at baseline | .25* | −.14 | −.19† | −.19† | .13 | −.03 | −.12 | .20* | −.22* | −.03 | −.10 | −.12 | −.03 | .138 | .06 | −.07 | .05 | −.29* |
| ALEF at 12 mo | .29* | −.42* | −.41* | −.37* | .36* | .21† | −.46* | .26* | −.06 | .48* | −.45* | −.56* | −.58* | .30* | .25* | −.49* | .25* | −.07 |
| BLEF at 12 mo | .24* | −.29* | −.28* | −.26* | .26* | .15 | −.29* | .32* | −.02 | .20† | −.33* | −.41* | −.42* | .24* | .19† | −.24* | .18† | −.04 |
| UEF at 12 mo | .20† | −.18† | −.15 | −.08 | .25* | .06 | −.19† | .17† | −.26* | .08 | −.18† | −.18† | −.09 | .23* | .15 | −.10 | .16 | −.27* |
Correlation significant at P<.01.
Correlation significant at P<.05.
DISCUSSION
The primary purpose of this study was to examine the psychometric properties of the abbreviated LL-FDI9 during a 12-month period in a sample of community-dwelling older adults. In general, the hypothesized factor structure for the abbreviated LL-FDI was supported with the deletion of several items that were necessary under conditions in which response range was restricted. For example, all participants in the present sample lived free of chronic disabilities; consequently, removing items reflecting disabilities with personal care tasks was a logical approach and improved model fit. Other items were removed from the function component for similar reasons because each item represented tasks performed daily by our independent community-dwelling sample. In previous studies,5,6 99% of participants reported having some degree of limitation or difficulty across all items (most indicated very often and cannot do, respectively), whereas in our sample, approximately two-thirds reported having no limitation or difficulty (most indicated never and none). Together, these modifications may improve the utility of the LL-FDI as a valid assessment of more modest disabilities and functional limitations in populations without chronic disabilities.
In terms of temporal invariance, we were able to meet the minimal longitudinal invariance criteria for all scales and more stringent (strong) invariance was established for the function and disability frequency components. Psychometricians39 have noted that when studying change processes, particularly for older adults, it is possible that although scales may measure the same construct, they may do so with different degrees of efficiency over time. In other words, if there are changes in the magnitude of regressions of the latent variables on the manifest variables, weak and partial weak invariance may be the best that can be obtained with these scales in this population.
Our study represents the first attempt, to our knowledge, to establish temporal invariance of both the function and disability (limitations and frequency) components of the abbreviated LL-FDI. It also is worth noting that our sample included both men and women, in contrast to past studies.9,10 Establishing reliable and temporally invariant measures is crucial for making inferences about change within groups, and with some modifications to the measurement model, our results suggest that for the most part, the abbreviated LL-FDI scale structures do not change over time. However, the need to modify our measurement models suggests that future investigations into LL-FDI scale development are warranted.
Study Limitations
Although this study was, to our knowledge, the first to explore the properties of the abbreviated LL-FDI longitudinally, several limitations must be considered. First, our sample was primarily white (88.3%) and non-Hispanic or Latino (98.3%) in ethnic origin. Thus, our findings may not extend to persons of other racial or ethnic backgrounds. Second, although the sample included men and women, sample size precluded the testing of sex invariance, although there does not appear to be a reason to expect sex differences in perceptions of functional limitations. Third, it also is possible that we may have made a relatively simple questionnaire factor structure overly complex by removing items and adding constraints to fit the data.
One potential direction for future research is to examine a new pool of items that reflects more challenging ADLs, such as carrying heavy objects (eg, >25lb [11.34 kg]) long distances (or across uneven terrain) or tasks that would require a more complex skill set. The present scale does little to address perceived stiffness and flexibility difficulties (eg, twisting and bending motions), a confounding problem with age.40,41 When studying change in perceptions of functional limitations and disabilities in groups of well-functioning older adults, Simonsick et al42(p M644) noted that “measures of capability should lie on the same continuum as measures of limitation.” Our functional fitness tests15 may be viewed as assessments of everyday functioning, yet more challenging measures may be needed to discriminate capabilities in high-functioning older persons.42,43 The possibility of floor/ceiling effects associated with questionnaire assessment of physical function and disability has not been acknowledged previously, and adjustments to the scales may be needed to reflect a greater spectrum of possible physical factors that even well-functioning older adults would acknowledge as a hindrance. Another direction might be to explicitly assess the extent to which ADLs are avoided. Integrating these components may improve the utility and generalizability of the scale. Finally, application of computer-adaptive testing to the abbreviated LL-FDI may further increase the utility of this scale in clinical settings.
CONCLUSIONS
We reported data reflecting the first empirical test of longitudinal invariance in the abbreviated LL-FDI.9 Minimal invariance criteria were established, suggesting that the meaning of its subscales does not appear to change substantively across time. Although this evidence suggests the measure to be of potential use to researchers and clinicians interested in the assessment and surveillance of functional disabilities and limitations in older adults, some caution should be exercised given that several modifications were necessary to fit the data reported by our healthy sample. The construct validity data suggest the functional limitations component to be low to moderately associated with physical function performance, supporting the perspective that the 2 are distinct constructs. Finally, additional measure development may be in order if the LL-FDI is to be applied to relatively high-functioning adults.
Acknowledgments
Supported by the National Institute on Aging (grant no. AG025667).
List of Abbreviations
- ADLs
activities of daily living
- ALEF
advanced lower-extremity function
- BLEF
basic lower-extremity function
- CFA
confirmatory factor analysis
- CFI
Comparative Fit Index
- CI
confidence interval
- FIML
full information maximum likelihood
- LL-FDI
Late-Life Function and Disability Instrument
- RMSEA
root mean square error of approximation
- SF-36
36-Item Short Form Health Survey
- SRMR
standardized root mean square residual
- UEF
upper-extremity function
Footnotes
Supplier
Muthén & Muthén, 3463 Stoner Ave, Los Angeles, CA 90066.
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit on the authors or on any organization with which the authors are associated.
References
- 1.CDC. Physical activity is essential to healthy aging. [January 4, 2010];2009 Available at: http://cdc.gov.
- 2.Stewart AL. Conceptual challenges in linking physical activity and disability research. Am J Prev Med. 2003;25(3 Suppl 2):137–40. doi: 10.1016/s0749-3797(03)00187-9. [DOI] [PubMed] [Google Scholar]
- 3.Guralnik JM, Ferrucci L. Assessing the building blocks of function utilizing measures of functional limitation. Am J Prev Med. 2003;25:112–21. doi: 10.1016/s0749-3797(03)00174-0. [DOI] [PubMed] [Google Scholar]
- 4.Nagi SZ. An epidemiology of disability among adults in the United States. Milbank Q. 1976;54:439–67. [PubMed] [Google Scholar]
- 5.Haley SM, Jette AM, Coster WJ, et al. Late life function and disability instrument: II. Development and evaluation of the function component. J Gerontol A Biol Sci Med Sci. 2002;57:M217–22. doi: 10.1093/gerona/57.4.m217. [DOI] [PubMed] [Google Scholar]
- 6.Jette AM, Haley SM, Coster WJ, et al. Late life function and disability instrument: I. Development and evaluation of the disability component. J Gerontol A Biol Sci Med Sci. 2002;57:M209–16. doi: 10.1093/gerona/57.4.m209. [DOI] [PubMed] [Google Scholar]
- 7.Nagi SZ. Disability concepts revised: implications for prevention. In: Pope AM, Tarlov AR, editors. Disability in America: toward a national agenda for prevention. Washington: National Academy Pr; 1991. [Google Scholar]
- 8.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 9.McAuley E, Konopack JF, Motl RW, Rosengren K, Morris KS. Measuring disability and function in older women: psychometric properties of the late-life function and disability instrument. J Gerontol A Biol Sci Med Sci. 2005;60:901–9. doi: 10.1093/gerona/60.7.901. [DOI] [PubMed] [Google Scholar]
- 10.Motl RW, McAuley E. Longitudinal analysis of physical activity and symptoms as predictors of change in functional limitations and disability in multiple sclerosis. Rehabil Psychol. 2009;54:204–10. doi: 10.1037/a0015770. [DOI] [PubMed] [Google Scholar]
- 11.Ware JE, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey—construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Ware JE, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36): conceptual-framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 13.Ware JE. Measuring patients views—the optimum outcome measure. BMJ. 1993;306:1429–30. doi: 10.1136/bmj.306.6890.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mihalko SL, McAuley E. Strength training effects on subjective well-being and physical function in the elderly. J Aging Phys Activ. 1996;4:56–68. [Google Scholar]
- 15.Jette AM, Keysor JJ. Assessing the field of disability research. Uses of evidence in disability outcomes and effectiveness research. Milbank Q. 2002;80:325–45. doi: 10.1111/1468-0009.t01-1-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meredith W, Horn JL. The role of factorial invariance in modeling growth and change. New methods for the analysis of change. In: Collins LM, Sayer AG, editors. New methods for the analysis of change. Decade of behavior. XXIV. Washington (DC): American Psychological Assoc; 2001. pp. 203–40. [Google Scholar]
- 17.Meredith W. Measurement invariance, factor-anlaysis and factorial invariance. Psychometrika. 1993;58:525–43. [Google Scholar]
- 18.Horn JL, McArdle JJ. A practical and theoretical guide to measurment invariance in aging research. Exp Aging Res. 1992;18:117–44. doi: 10.1080/03610739208253916. [DOI] [PubMed] [Google Scholar]
- 19.McAuley E, Mailey EL, Mullen S, et al. Growth trajectories of exercise self-efficacy in older adults: Influence of measures and initial status. Health Psychol. 2010;30:75–83. doi: 10.1037/a0021567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rikli RE, Jones CJ. Development and validation of a functional fitness test for community-residing older adults. J Aging Phys Activ. 1999;7:129–61. [Google Scholar]
- 21.Kline GM, Porcari JP, Hintermeister R, et al. Estimation of VO2 max from a one-mile track walk, gender, age, and body-weight. Med Sci Sport Exerc. 1987;19:253–9. [PubMed] [Google Scholar]
- 22.Muthén LK, Muthén BO. Mplus user’s guide. 5. Los Angeles: Muthén & Muthén; 2010. [Google Scholar]
- 23.Enders CK. The impact of nonnormality on full information maximum-likelihood estimation for structural equation models with missing data. Psychol Methods. 2001;6:352–70. [PubMed] [Google Scholar]
- 24.Myrtveit I, Stensrud E, Olsson UH. Analyzing data sets with missing data: an empirical evaluation of imputation methods and likelihood-based methods. IEEE Trans Software Eng. 2001;27:999–1013. [Google Scholar]
- 25.Bentler PM, Chou CP. Practical issues in structural modeling. Sociol Method Res. 1987;16:78–117. [Google Scholar]
- 26.Bentler PM, Yuan KH. Structural equation modeling with small samples: test statistics. Multivar Behav Res. 1999;34:181–97. doi: 10.1207/S15327906Mb340203. [DOI] [PubMed] [Google Scholar]
- 27.Bollen KA. A new incremental fit index for general structural equation models. Sociol Method Res. 1989;17:303–16. [Google Scholar]
- 28.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Eq Modeling. 1999;6:1–55. [Google Scholar]
- 29.Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Vol. 21. Newbury Park: Sage; 1993. pp. 230–58. [Google Scholar]
- 30.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238–46. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 31.Babyak MA, Green SB. Confirmatory factor analysis: an introduction for psychosomatic medicine researchers. Psychosom Med. 2010;72:587–97. doi: 10.1097/PSY.0b013e3181de3f8a. [DOI] [PubMed] [Google Scholar]
- 32.Chen FN, Curran PJ, Bollen KA, Kirby J, Paxton P. An empirical evaluation of the use of fixed cutoff points in RMSEA test statistic in structural equation models. Sociol Method Res. 2008;36:462–94. doi: 10.1177/0049124108314720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marsh HW, Hau KT, Wen Z. In search of golden rules: comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Structural Eq Modeling. 2004;11:320–41. [Google Scholar]
- 34.Fan X, Sivo SA. Sensitivity of fit indices to model misspecification and model types. Multivar Behav Res. 2007;42:509–29. [Google Scholar]
- 35.Lance CE, Vandenberg RJ, Self RM. Latent growth models of individual change: the case of newcomer adjustment. Organ Behav Hum Decis Process. 2000;83:107–40. doi: 10.1006/obhd.2000.2904. [DOI] [PubMed] [Google Scholar]
- 36.Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Eq Modeling. 2002;9:233–55. [Google Scholar]
- 37.Asparouhov T, Muthen B. Exploratory structural equation modeling. Structural Eq Modeling. 2009;16:397–438. [Google Scholar]
- 38.Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–14. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Horn JL, McArdle JJ, Mason R. When is invariance not invariant: a practical scientist’s view of the ethereal concept of factorial invariance. South Psychol. 1983;1:179–88. [Google Scholar]
- 40.Fatouros IG, Kambas A, Katrabasas I, et al. Resistance training and detraining effects on flexibility performance in the elderly are intensity-dependent. J Strength Cond Res. 2006;20:634–42. doi: 10.1519/R-17615.1. [DOI] [PubMed] [Google Scholar]
- 41.Bird ML, Hill K, Ball M, Williams AD. Effects of resistance- and flexibility-exercise interventions on balance and related measures in older adults. J Aging Phys Act. 2009;17:444–54. doi: 10.1123/japa.17.4.444. [DOI] [PubMed] [Google Scholar]
- 42.Simonsick EM, Newman AB, Nevitt MC, et al. Measuring higher level physical function in well-functioning older adults: expanding familiar approaches in the Health ABC Study. J Gerontol: Med Sci. 2001;56A:M644–59. doi: 10.1093/gerona/56.10.m644. [DOI] [PubMed] [Google Scholar]
- 43.Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–61. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]


