Abstract
Laryngeal chemoreflexes (LCR), which are elicited by the contact of liquids such as gastric refluxate with laryngeal mucosa, may trigger some cases of sudden infant death syndrome. Indeed, while LCR in mature mammals consist of protective responses, previous animal data have shown that LCR in immature newborns can include laryngospasm, apnea, bradycardia, and desaturation. The present study was aimed at testing the hypothesis that postnatal exposure to cigarette smoke is responsible for enhancing cardiorespiratory inhibition observed with LCR. Eight lambs were exposed to cigarette smoke (20 cigarettes/day) over 16 days and compared with seven control lambs. Urinary cotinine/creatinine ratio was measured at a level relevant to previously published levels in infants. On days 15 and 16, 0.5 ml of HCl (pH 2), milk, distilled water, or saline was injected onto the larynx via a chronic supraglottal catheter during sleep. Results showed that exposure to cigarette smoke enhanced respiratory inhibition (P < 0.05) and tended to enhance cardiac inhibition and decrease swallowing and arousal during LCR (P < 0.1). Overall, these results were observed independently of the state of alertness and the experimental solution tested. In conclusion, 16-day postnatal exposure to cigarette smoke increases cardiorespiratory inhibition and decreases protective mechanisms during LCR in nonsedated full-term lambs.
Keywords: cigarette smoke, sleep, sudden infant death syndrome
in the mature organism, stimulation of the laryngeal mucosa receptor by liquids triggers highly protective reflexes, termed laryngeal chemoreflexes (LCR), which consist of coughing, arousal, and swallowing to prevent tracheal aspiration. In the immature newborn mammal, however, LCR are rather associated with vagal components such as laryngospasm, apnea, bradycardia, and hemoglobin desaturation (51). The hypothesis that LCR can lead to apneas of prematurity, apparent life-threatening events, and sudden infant death syndrome (SIDS) stems from both clinical experience and experimental results (33, 40, 52). We previously showed that LCR are characterized by a major cardiorespiratory inhibition in preterm lambs (46). On the contrary, LCR in healthy full-term lambs are consistently similar to the mature LCR reported in adult mammals and characterized by lower airway protective mechanisms with minimal cardiorespiratory inhibition (45). These observations led us to hypothesize that the development of life-threatening cardiorespiratory events during LCR in a full-term newborn is promoted by certain neonatal conditions, such as postnatal smoke exposure.
After worldwide “Back to Sleep” campaigns, perinatal environmental tobacco smoke (ETS) exposure, especially during pregnancy, is now considered an important risk factor for SIDS (1, 2, 3, 8, 22, 23, 36, 44). Although SIDS has been reported to be increased two- to threefold by postnatal ETS in some studies (4), partitioning the effects of post- from prenatal ETS is not straightforward in a clinical setting, with most infants being exposed to both. Postnatal infusion of nicotine has previously been shown to significantly increase cardiorespiratory inhibition during LCR in newborn lambs, suggesting that postnatal exposure to cigarette smoke may predispose to SIDS via enhancement of LCR (49). However, the clinical relevance of the high dose of nicotine used in that study was questioned by the authors themselves (49). In addition, studies on nicotine alone are likely insufficient to unravel all of the potential effects of ETS, given that cigarette smoke contains at least 4,000 different chemical compounds. Hence, the present study was aimed at testing our hypothesis that postnatal ETS, at a nicotine level equivalent to that reported in human infants, enhances cardiorespiratory inhibition during LCR. We also aimed at assessing whether the state of alertness or type of solution used to trigger the LCR has an effect on the observed responses.
MATERIALS AND METHODS
Animals.
Experiments were performed in 15 lambs born at term by spontaneous vaginal delivery and housed in our animal quarters (day-light cycle 0600–1800) during the days of the experimentation. Lambs were bottle-fed ad libitum with ewe milk three times a day at 8:00 AM, noon, and 5:00 PM. The protocol of the study was approved by the Ethics Committee for Animal Care and Experimentation of our institution.
Secondary tobacco smoke exposure.
Eight lambs were exposed to secondary tobacco smoke (exposure group; 20 cigarettes/day) during the first 16 days of life. The 8-h daily exposure consisted of two periods of 4 h separated by a 30-min pause at noon to bottle-feed the lamb and collect a urine sample for cotinine measurements using a urine bag (U-Bag 24-Hour for newborn; Libertyville, IL). Before and after exposure, the lamb was bottle-fed, its body temperature and weight measured, and a blood sample collected for arterial gas measurements. A cigarette-smoking machine was built in collaboration with the Department of Mechanical Engineering of the Université de Sherbrooke. This custom-made equipment, which is fully programmable, smokes cigarettes automatically according to preset parameters and produces a mixture of mainstream and sidestream smoke (see Ref. 13 for further details). The latter was vented into a 1.2 × 1.2-m Plexiglas exposure chamber, where the nonrestrained lambs stayed for the duration of the exposure. Preliminary experiments had shown that smoking 20 cigarettes/day induced levels of urinary cotinine at the upper limits of the range reported in infants exposed to cigarette smoke postnatally at home (5, 6, 24, 29). Results obtained in the eight lambs exposed to secondary tobacco smoke were compared with a control group (7 lambs), which were exposed to air in the same exposure chamber for 8 h daily and during the first 16 days of life.
Instrumentation of the lambs and recording equipment.
Surgery was performed on the 13th day of smoke exposure (2 days before the first recording) under general anesthesia (2% isoflurane, 30% N2O, and 68% O2), as previously described (46). Briefly, bipolar gold-plated stainless steel electrodes were inserted into the two thyroarytenoid muscles (Ta; a glottal adductor) for recording Ta electrical activity (Ta electromyogram; EMG). Three platinum needle electrodes were inserted, two into the parietal cortex for electroencephalogram (EEG) recording and one under the scalp as a ground. For electrocardiogram (ECG) recordings, two needle electrodes were inserted under the periosteum of the 5th ribs. Leads from all electrodes were subcutaneously tunneled to exit on the back of the lambs. In addition, a supraglottal catheter was inserted transcutaneously to allow injection of liquids onto the larynx 5–7.5 mm above the anterior part of the glottis. A plastic tubing was subcutaneously tunneled in the neck of the lamb and connected to the catheter (15). Finally, an arterial catheter was inserted into the carotid artery for recording systemic arterial pressure. Correct positioning of the electrodes and catheters was systematically verified at autopsy.
Lamb instrumentation was completed immediately before recording in nonsedated lambs. Nasal airflow was recorded by use of a thermocouple wire glued to the side of one nostril. Two platinum needle electrodes were placed subcutaneously near the right eye socket for electrooculogram (EOG) recording. Thoracic and abdominal elastic bands were placed for recording respiratory inductance plethysmography and to provide qualitative assessment of lung volume variations with respiration. A pulse oximeter probe (Masimo Radical; Irvine, CA) was attached at the base of the tail for continuous monitoring of oxygen hemoglobin saturation by pulse oximetry (SpO2) and pulse wave. Finally, the subcutaneous plastic tubing connected to the supraglottal catheter was attached to a custom-designed radiotelemetry-driven injector, where the liquid to be injected was warmed and maintained at the lamb's body temperature. Leads from the EMG, EOG, EEG, and ECG electrodes and the nasal thermocouple were connected to a transmitter attached to the lamb's back immediately before the experiment. Raw EMG, EOG, EEG, and ECG signal, as well as nasal flow, were transmitted by custom-made radiotelemetry equipment (34). The raw EMG signals were moving time averaged (100 ms). All variables were continuously recorded using an acquisition software (AcqKnowledge version 3.2; Biopac Systems, Santa Barbara, CA). Collected data were stored on compact disk for further analysis.
Design of the study.
The study was designed to allow for simultaneous recording of Ta EMG, ECG, EEG, EOG, nasal flow, sum of thoracic and abdominal movements, and SpO2 while triggering LCR by injection of liquids onto the larynx. Recordings were performed in nonsedated lambs on postnatal days 15 and 16 in the evening, following smoke exposure. The lambs were comfortably positioned on a mattress. Baseline values of heart rate (HR), respiratory rate (RR), mean arterial pressure (MAP), SpO2, and temperature were first logged. Each recording day consisted of a random sequence of 0.5-ml injections via the supraglottal catheter of saline (0.9% NaCl, pH 5.5, osmolarity = 326 mosM, [Cl−] = 181 mM), distilled water (pH 5.7), HCl diluted in saline (pH 2, osmolarity = 295 mosM, [Cl−] = 181 mM), and ewe's milk {pH 6.4 (SD 0.2), osmolarity = 336 (SD 92) mosM, [Cl−] = 38 (SD 11) mM}. All solutions were injected once in both quiet sleep (QS) and active sleep (AS) on days 15 and 16 (total of 8 injections per each experimental day). The supraglottal catheter was systematically flushed with 1 ml of saline between two injections, and lambs were given at least 15 min of recovery time between two injections. Events such as cough, arousal, or full awakening were noted by an observer throughout the recording sessions.
Data analysis.
The main objective of the study was to assess the effect of postnatal cigarette smoke exposure on LCR. In addition, we queried whether this effect was different in QS vs. AS and from one experimental solution to another. Analysis of the LCR was performed as described previously within the first minute following each laryngeal injection (45). First, the cardiorespiratory responses were assessed as follows. The percentage of decrease in HR [%dec HR = (HRBL − HRmin)/HRBL × 100] was calculated, with HRBL representing the baseline HR value averaged over 1 min before injection and HRmin representing the minimal HR value observed after injection. The percentage of increase in MAP, decrease in RR, and decrease in saturation were calculated in the same manner. Any presence of bradycardia (defined by a %dec HR >30%) was noted, and the number of bradycardias, total summed duration of bradycardias, and minimal HR value were tabulated. The number of apneas (defined as at least 2 missed breaths relative to baseline breathing) and the total summed duration of apneas were recorded. Moreover, the presence of any apneas longer than 5, 10, and 20 s was also noted. Respiratory LCR duration was measured as the time duration between the onset of the LCR and resumption of three consecutive breaths (53). The time spent with SpO2 below 90 and 85% was calculated, as well as the area under the same SpO2 values. In addition to cardiorespiratory responses, the number of swallows (recognized as a brisk high-amplitude and short-duration Ta EMG) (39) was tallied. In addition, total summed duration of Ta EMG (total Ta EMG duration, indicating laryngeal closure) was calculated. The presence of coughing was also inferred from visual observation and analysis of Ta EMG and respiratory inductance plethysmograph signals. Standard electrophysiological and behavioral criteria were used to define QS and AS from EEG, EOG, and continuous visual observation (41). Cortical arousal from QS was defined by the association of a change in EEG (decrease in amplitude + increase in frequency) for 3 s or more, with at least two of the following modifications: a 10% increase in HR, a change in RR, or a body movement (26). Arousal from AS was recognized by direct observation of the lamb and disappearance of intense EOG activity. Full awakening was defined when the lamb was still awake after 1 min (19). Finally, the number of stimulations with arousal or full awakening was documented.
Urinary cotinine was measured using an ELISA immunoassay kit (Bio-Quant COTININE Direct Elisa; San Diego, CA). Collected samples (3 ml) were stored at −20°C until analysis. Cotinine measurement was preferred to nicotine in this study because of its longer half-life (15–20 h vs. 30 min-2 h, respectively), slow renal elimination, and high urinary concentration (6–25× nicotine concentration). Creatinine was assayed in the Department of Biochemistry of the Université de Sherbrooke Hospital using their standard protocol. Cotinine/creatinine ratio was then calculated.
The larynx was immediately removed after euthanasia and placed in a formaldehyde solution (1/10). Specimens were cut and placed in a cassette for dehydration and fixation in paraffin. Paraffin blocks were cut using a microtome, and slices were placed on a microscope slide for eosin-hematoxylin staining and subsequent observation. Laryngeal inflammation was assessed in three control lambs and four exposure lambs by a pathologist expert in larynx pathology, using a previously described inflammation score based on both epithelial and subepithelial changes (30).
Statistical analysis.
Quantitative variables are expressed as means ± SD, whereas qualitative variables (coughing, arousal, and awakening) were expressed as relative frequency. Statistical analyses were performed on raw data for all variables. For baseline physiological values, the effect of exposure to smoke was assessed using the Student's t-test. For the laryngeal chemoreflexes, quantitative variables were analyzed through a general linear model three-way ANOVA for repeated measures using Proc mixed procedures (SAS software version 9.1.3; Cary, NC) with group, solutions, and sleep states as the independent variables. Qualitative variables were analyzed with a logistic regression model. Differences were deemed significant if P < 0.05. In addition, given the relatively small number of studied lambs (related to both the complexity of the ovine model and ethical constraints), it was decided to give full consideration to the presence of a significant trend, defined as P < 0.1.
RESULTS
A total of 95 stimulations were performed in the control group (QS: 14 saline, 14 distilled water, 13 HCl, 14 milk; AS: 12 saline, 10 distilled water, 9 HCl, 9 milk) and 116 stimulations in the exposure group (QS: 16 saline, 16 distilled water, 16 HCl, 16 milk; AS: 12 saline, 11 distilled water, 15 HCl, 14 milk). Because of technical reasons and difficulties in obtaining AS in some lambs, %dec MAP and saturation indexes could only be measured in 2 and 4 lambs, respectively, of the control group in AS. All other measurements were successfully obtained in at least five lambs in both groups.
Passive smoking lamb model.
All lambs completed the 16-day exposure to cigarette smoke without problems. No differences in arterial blood gases were apparent between the control and exposure groups (results not shown). However, an increase in spontaneous activity was observed in lambs from the exposure group, including head movements to verify surroundings and repeated jumps in the exposure chamber during 20- to 30-min periods. Mean weight increase was similar between both groups from the first postnatal day [control group: 3.1 (0.5) kg; exposure group: 3.6 (0.6) kg] to postnatal day 16 [control group: 5.6 (1.7) kg; exposure group: 6.4 (1.4) kg]. Baseline values of vital signs are detailed in Table 1: whereas RR and MAP were significantly higher in lambs from the exposure group, no differences in HR, SpO2, and temperature were observed. The cotinine/creatinine ratio was significantly higher in the exposure group throughout the exposure [1,116 (832) vs. 15 (12) ng/mg in the control group, P < 0.0001], as well as during the last 2 recording days [891 (506) vs. 11 (11) mg/mg in the control group, P < 0.0001].
Table 1.
Baseline values of vital signs for lambs from the exposure and control groups
| Control | Exposure | |
|---|---|---|
| HR, beats/min | 203 (28) | 217.5 (32) |
| RR, breaths/min | 34 (12) | 44.5 (15)* |
| MAP, mmHg | 81 (11) | 90 (7)* |
| Temperature, °C | 40 (0.3) | 39.5 (0.5) |
| Saturation, % | 98.5 (1) | 98 (2) |
Values are means (SD). HR, heart rate; RR, respiratory rate; MAP, mean arterial pressure.
P < 0.05 vs. control group (P > 0.15 for the other 3 comparisons).
Effects of cigarette smoke exposure on LCR.
Results obtained during LCR are given in Tables 2 and 3. After 2 wk of passive smoking, laryngeal stimulations (all solutions and both sleep states taken together) elicited significantly greater respiratory inhibition compared with the control group, including for the percent decrease in RR, apnea duration, and number of apneas. No interaction was found between groups, sleep states, and solutions for the first two variables. However, a significant interaction was found for the number of apneas in that the latter was greater in the exposure group only when LCR was triggered by water during active sleep (see Table 3). In addition, a tendency toward a greater cardiac inhibition in the exposure group was observed for the number of bradycardias, with no interaction between groups, sleep states, and solutions. No differences were observed for MAP, respiratory LCR duration, total duration of active glottal closure (measured by Ta muscle EMG), and SpO2 variables. Some variables measuring protective mechanisms tended to be decreased in the exposure group, including the number of swallows and arousals. No differences were noted, however, for the number of coughs or awakening.
Table 2.
Overall characteristics of LCR following 16-day exposure to cigarette smoke
| Control | Exposure | |
|---|---|---|
| %dec RR | 51 (18) | 67 (15)* |
| Apnea duration, s | 4.5 (8.3) | 7.8 (8.5)* |
| No. of apneas | 1.1 (2.7) | 2.2 (4.7)*‡ |
| %dec HR | 21 (11) | 28 (14) |
| Bradycardia duration, s | 0.2 (0.7) | 0.3 (0.7) |
| No. of bradycardias | 0.2 (0.7) | 0.5 (1)† |
| Minimum HR, min−1 | 142 (9) | 144 (7) |
| %inc MAP | 23 (16) | 18(10) |
| Respiratory LCR duration, s | 13.2 (10) | 14.8 (8.8) |
| Total Ta EMG duration, s | 2.2 (2.9) | 2.5 (2.9) |
| %dec Saturation | 3 (3) | 3 (3) |
| Saturation, area under 90% | 0.04 (0.2) | 0.06 (0.3) |
| Saturation, area under 85% | 0.01 (0.08) | 0.02 (0.14) |
| No. of swallows | 12 (10) | 8 (7)† |
| Arousal no. of LCR with arousal/total no. of LCR | 76/89 | 83/116† |
| Coughs (no. of LCR with cough/total no. of LCR | 14/94 | 11/116 |
| Awakening (no. of LCR with awakening/total no. of LCR) | 48/76 | 55/83 |
Values are means (SD). Results are means from all laryngeal stimulations (all solutions and all states of alertness) for each group. Values in the control group were available only in 5 lambs for percent increase in MAP (%inc MAP) and saturation indexes and in 6 lambs for the number of swallows and total duration of electrical activity of the thyroarytenoid muscle (Ta EMG duration). %dec HR, %dec RR, and %dec saturation, percent decrease in HR, RR, or O2 saturation, respectively; LCR, laryngeal chemoreflexes.
P < 0.05;
P < 0.1 vs. control.
Significant interaction between sleep state and solution (see Table 3 for details).
Table 3.
Influence of sleep state and solution on the effects of 16-day exposure to cigarette smoke on LCR in lambs
| Quiet Sleep |
Active Sleep |
|||||||
|---|---|---|---|---|---|---|---|---|
| Saline | H2O | HCl | Milk | Saline | H2O | HCl | Milk | |
| %dec RR | ||||||||
| Control | 46.5 (21) | 52 (14.5) | 51.5 (19.5) | 46.5 (20) | 48 (16) | 59 (14.5) | 49.5 (16) | 5.7 (17) |
| Exposure | 56 (22.5) | 69 (13.5) | 67 (12) | 70 (10.5) | 64 (15) | 74 (10.5) | 68 (11.5) | 67.5 (13) |
| No. of apneas | ||||||||
| Control | 0.9 (2) | 0.8 (1) | 1 (1.5) | 0.8 (1) | 0.5 (0.9) | 3.5 (7.5)* | 0.3 (0.7) | 1 (0.9) |
| Exposure | 2.5 (7) | 1 (0.5) | 1.5 (1) | 1.5 (0.9) | 2 (2) | 7.5 (12)* | 1.5 (0.9) | 1.5 (0.9) |
| %dec HR | ||||||||
| Control | 20.5 (7.5) | 25 (13) | 24 (6) | 20 (9) | 14.5 (10) | 18.5 (4.) | 20 (13.5) | 28 (18) |
| Exposure | 24.5 (13) | 27 (6.5) | 36.5 (15) | 28 (10) | 21 (13) | 35 (18) | 25.5 (15) | 27 (16.5) |
| No. of bradycardias | ||||||||
| Control | 0.2 (0.8) | 0.2 (0.4) | 0.4 (0.7) | 0.1 (0.3) | 0 (0) | 0 (0) | 0.5 (0.7) | 0.7 (1.5) |
| Exposure | 0.2 (0.4) | 0.4 (0.6) | 1 (2) | 0.5 (1) | 0.2 (0.4) | 0.5 (0.7) | 0.5 (1.2) | 0.2 (0.4) |
| %inc MAP | ||||||||
| Control | 16.5 (11) | 21.5 (13.5) | 36.5 (20.5) | 28 (14.5) | 10.5 (3) | 18 (4.5) | 8 (5.5) | 31 (14.5) |
| Exposure | 16 (16) | 16 (6) | 18.5 (4) | 15 (7) | 15.5 (10.5) | 20 (10) | 18.5 (9.5) | 22.5 (8) |
| Respiratory LCR duration, s | ||||||||
| Control | 10.5 (8.5) | 13.5 (8.5) | 22 (15) | 13.5 (11.5) | 10.5 (8) | 11.5 (5.5) | 9 (5) | 13 (6.5) |
| Exposure | 14 (9) | 14 (9.5) | 23.5 (11.5) | 13.5 (6) | 9.5 (5.5) | 16 (8.5) | 15.5 (7) | 12.5 (6.5) |
| %dec Saturation | ||||||||
| Control | 1.5 (1.5) | 4 (5.5) | 4.5 (4.5) | 2 (2) | 8 (1.5) | 3 (3.5) | 3 (2.5) | 3 (2.5) |
| Exposure | 3 (3) | 1.5 (1) | 5 (5) | 2.5 (2.5) | 2.5 (3.5) | 2 (1.5) | 3 (1.5) | 3 (3) |
| No. of swallows | ||||||||
| Control | 6 (4.5) | 12 (10) | 23.5 (17) | 13.5 (8.5) | 6 (3) | 7 (5) | 14.5 (7.5) | 10 (5.5) |
| Exposure | 4 (1.5) | 6 (2) | 17 (11) | 8.5 (4.5) | 4.5 (1.5) | 5.5 (2.5) | 12 (7.5) | 8 (4) |
| Arousal (no. of LCR with arousal/total no. of LCR) | ||||||||
| Control | 9/12 | 12/13 | 13/13 | 13/13 | 9/10 | 6/9 | 7/9 | 6/10 |
| Exposure | 9/16 | 14/16 | 13/16 | 13/16 | 6/12 | 10/11 | 10/15 | 8/14 |
| Coughs (no. of LCR with cough/total no. of LCR) | ||||||||
| Control | 3/12 | 2/14 | 4/13 | 3/14 | 2/12 | 10/10 | 9/9 | 10/10 |
| Exposure | 2/16 | 16/16 | 5/16 | 1/16 | 11/12 | 3/12 | 15/15 | 13/13 |
| Awakening (no. of LCR with awakening/total no. of LCR) | ||||||||
| Control | 7/10 | 11/12 | 7/13 | 10/13 | 6/9 | 2/6 | 4/7 | 1/6 |
| Exposure | 6/9 | 13/14 | 2/13 | 12/13 | 4/6 | 4/10 | 7/10 | 7/8 |
Values are means (SD).
Significant interaction between solution and sleep state.
Apneas longer than 10 s were rare events in both the exposure (3 apneas) and control group (2 apneas), with none above 20 s. However, apnea duration between 5 and 9 s was more often observed in the exposure group than in the control group (48 vs. 21 apneas, respectively). In addition, all bradycardias but one were shorter than 5 s. One severe event was observed in one lamb in the exposure group following HCl injection in QS, with marked hypoventilation and a decrease in SpO2 down to 76% (Fig. 1).
Fig. 1.
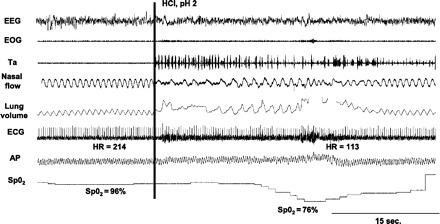
Cardiorespiratory reflexes triggered in a lamb at postnatal day 15 after 2 wk of exposure to cigarette smoke, following instillation of 0.5 ml of HCl onto laryngeal mucosa during quiet sleep. EEG, electroencephalogram; EOG, electrooculogram; Ta, electrical activity of the thyroarytenoid muscle; nasal flow, nasal airflow; lung volume, sum signal of the respiratory inductance plethysmograph, allowing qualitative measurement of respiration (inspiration upward); ECG, electrocardiogram; HR, heart rate (beats/min); AP, arterial pressure; SpO2, oxygen hemoglobin saturation measured by pulse oximetry.
Effects of passive smoking on laryngeal mucosa.
There was no observable effect of cigarette smoke exposure on laryngeal inflammation in the few lambs studied. Indeed, histological analysis showed the presence of moderate inflammation in lambs from both the control (score 9/15, n = 3 lambs) and exposure groups (score 8/15, n = 4 lambs).
DISCUSSION
The present study provides novel findings on LCR triggered in nonsedated full-term lambs following exposure to passive smoking in the early postnatal period. Overall, our findings reveal that LCR after postnatal exposure to environmental tobacco smoke are characterized by enhanced cardiorespiratory inhibition and decreased protective reflexes.
Passive smoking lamb model.
Most studies on the effect of ETS exposure have focused on nicotine alone, despite the fact that tobacco smoke contains at least 4,000 different chemical compounds, many of which are known to be harmful to human health. In the present study, we used our custom-built smoking machine (13) to mimic postnatal parental smoking while ensuring that urinary cotinine level was relevant to previously published levels in infants (5, 6, 24, 29). The increase in baseline respiratory rate is in agreement with previous results on ETS exposure in both the human fetus and newborn (20). The absence of any increase in respiratory rate following postnatal infusion of nicotine in a previous study in newborn lambs (49) suggests that the effect on respiratory control may be shared with other constituents of cigarette smoke.
Effect of passive smoking on LCR.
To our knowledge, despite its clinical importance, only one study has assessed the effect of perinatal ETS on LCR: passive smoking during gestation was shown to induce longer apneas during LCR in newborn rats only if combined with hyperthermia (53). Many methodological differences (prenatal exposure, sedation, injection of distilled water via tracheal catheter), in addition to species differences, can explain discrepant results with the present study. In keeping with our results, however, the authors observed no life-threatening events, even when ETS was added to hyperthermia.
The effect of nicotine alone on the cardiorespiratory components of the neonatal LCR has been addressed in three studies. In two studies conducted in sedated newborn piglets, the effect of one injection of nicotine on LCR was inconsistent, either showing no effect (16) or an enhanced cardiorespiratory inhibition (17). In the third study, in nonsedated newborn lambs injected with intravenous nicotine during several days, an enhanced cardiorespiratory inhibition was reported during LCR in both room air and mild hypoxia (49). However, the authors themselves questioned the clinical relevance of their data in infants submitted to postnatal ETS, due to the high nicotine dose used in their study.
Our present observations that swallowing and coughing were prominent during LCR in control lambs are in agreement with our previous results in healthy full-term lambs (45). Conversely, swallowing was significantly blunted in exposure lambs. Whereas active smoking has been previously shown to decrease reflexive pharyngeal swallowing (10, 11), this is the first observation of a decrease in swallowing induced by passive smoking. Relevance of this observation is related to the fact that decreased swallowing activity during LCR may lead to increased contact time between stimulating liquid and the laryngeal mucosa, leading in turn to enhanced LCR and deleterious cardiorespiratory events in the infant. Although we did not observe any differences in “coughing” in exposure lambs, we must recognize that our study did not allow us to fully assess coughing. Indeed, since we only counted the number of coughs and were not able to discriminate between “real” coughs and laryngeal expiratory reflexes (brisk expiration not preceded by a deep inspiration), we cannot dismiss a decrease in cough efficacy.
Our observation of decreased arousal during LCR following postnatal ETS may also be relevant with regard to the increase in the occurrence of SIDS after ETS. Indeed, arousal plays a critical role in homeostasis (22) and arousal deficiency is likely present in a number of SIDS victims (28,37). Both maternal smoking and nicotine during pregnancy have been shown to affect arousal threshold (22, 42), but the present results represent the first account that postnatal passive smoking decreases arousal induced by laryngeal stimulation. Ability to arouse appears essential during LCR, by relieving cough suppression (32, 48), promoting swallowing (43), and cessation of apnea and bradycardia (50).
Our histological observations suggest that the effects of postnatal ETS on LCR are not related to laryngeal inflammation. In fact, the mechanisms involved in LCR alterations following ETS can be at play anywhere along the LCR neural circuitry, including from the laryngeal receptors to the central modulators of LCR. In addition, although a number of cigarette smoke constituents could contribute to these results, the majority of current knowledge comes from experiments on prenatal nicotine exposure. There is now abundant evidence that nicotine impairs brain development (14), including brain stem neuronal networks. For example, nicotine has been reported to alter brain stem nicotinic or serotonergic receptors involved in the control of cardiorespiratory function, swallowing, and arousal (12, 14, 27), to increase GABA release and GABAA receptor upregulation to respiratory centers (35, 54), and to decrease GABAergic input to cardioinhibitory vagal neurons (38). As for the other constituents of cigarette smoke, an interesting hypothetical mechanism for brainstem network dysfunction relates to the induction of brain inflammation by NNK [4-methylnitrosamino-1-(3-pyridyl)-1-butanone] (18), which is reminiscent of the extensive brain stem inflammation reported in SIDS victims (25).
Influence of various solutions or sleep states on LCR.
Aside from the number of apneas (increased in the exposure group with water and in AS only), no systematic effects of sleep states or solutions on the differences in cardiorespiratory events in the exposure vs. control group were observed. Of note, in a previous study, we also did not find any systemic effects of sleep states on LCR in preterm lambs (46). The fact that LCR can readily be induced by ewe's milk, similar to water or HCl, is in agreement with previous reports in lambs, piglets, and puppies (7, 9, 21, 31, 47).
Clinical implications.
Clinical evidence strongly suggests that LCR can be triggered by numerous liquids, including upper airway secretions, milk bottle-feeding, and both acidic and non-acidic laryngopharyngeal reflux (40). LCR are one of the mechanisms involved in apneas of prematurity, apparent life-threatening events, and probably some cases of SIDS (28, 33, 40). Many neonatal conditions (46, 51, 54) have been shown to enhance cardiorespiratory inhibition during LCR. The present findings show that postnatal ETS, at a level consistent with clinical observations, can also contribute in altering LCR toward more cardiorespiratory inhibition and less protective mechanisms. However, our results suggest that, at least in lambs, postnatal ETS is most often insufficient in itself to trigger potentially dangerous reflexes. Nevertheless, it is important to emphasize that most infants exposed to passive smoking have additional risk factors, which are likely synergistic with LCR for explaining the failing chain of events ultimately leading to SIDS. These include preterm birth, pathological laryngopharyngeal reflux with laryngitis, prone position, respiratory viral infection, and/or hyperthermia. Future studies need to consider these multiple factors. Finally, given that sheep are more precocial than humans, repeating the experiments in our preterm ovine model (46) would also be worthwhile.
GRANTS
The study was supported by grants from the Canadian Institutes for Health Research and the Foundation of Stars (Quebec) (to J.-P. Praud). A.-M. Carreau was an MD-MSc Scholar of the Fonds de la Rrecherche en Santé du Québec (FRSQ). J.-P. Praud is a member of the FRSQ-funded Clinical Research Center Étienne-Le Bel, Sherbrooke University Hospital, and holder of the Canada Research Chair in Neonatal Respiratory Physiology.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
ACKNOWLEDGMENTS
We gratefully acknowledge the expert technical assistance of Jean-Philippe Gagné and Nathalie Samson, as well as Julie Hamon and Larissa Takser for statistical analyses.
REFERENCES
- 1. Adgent MA. Environmental tobacco smoke and sudden infant death syndrome: a review. Birth Defects Res B Dev Reprod Toxicol 77: 69–85, 2006 [DOI] [PubMed] [Google Scholar]
- 2. Alm B, Milerad J, Wennergren G, Skjaerven R, Oyen N, Norvenius G, Daltveit AK, Helweg-Larsen K, Markestad T, Irgens LM. A case-control study of smoking and sudden infant death syndrome in the Scandinavian countries, 1992 to 1995. The Nordic Epidemiological SIDS Study. Arch Dis Child 78: 329–334, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Alm B, Norvenius SG, Wennergren G, Skjaerven R, Oyen N, Milerad J, Wennborg M, Kjaerbeck J, Helweg-Larsen K, Irgens LM. Nordic Epidemiological SIDS Study. Changes in the epidemiology of sudden infant death syndrome in Sweden 1973–1996. Arch Dis Child 84: 24–30, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Anderson HR, Cook DG. Passive smoking and sudden infant death syndrome: review of the epidemiological evidence. Thorax 52: 1003–1009, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Anuntaseree W, Mo-Suwan L, Ovatlarnporn C, Tantana C, Ma-a-Lee A. Exposure to environmental tobacco smoke among infants in southern Thailand: a study of urinary cotinine. Bull Environ Contam Toxicol 80: 34–37, 2008 [DOI] [PubMed] [Google Scholar]
- 6. Blackburn CM, Bonas S, Spencer NJ, Coe CJ, Dolan A, Moy R. Parental smoking and passive smoking in infants: fathers matter too. Health Educ Res 20: 185–194, 2005 [DOI] [PubMed] [Google Scholar]
- 7. Bogg DF, Bartlett JR. Chemical specificity of a laryngeal apneic reflex in puppies. J Appl Physiol 53: 455–462, 1982 [DOI] [PubMed] [Google Scholar]
- 8. DiFranza JR, Aligne CA, Weitzman M. Prenatal and postnatal environmental tobacco smoke exposure and children's health. Pediatrics 11: 1007–1015, 2004 [PubMed] [Google Scholar]
- 9. Downing SE, Lee JC. Laryngeal chemosensitivity: a possible mechanism for sudden infant death. Pediatrics 55: 640–649, 1975 [PubMed] [Google Scholar]
- 10. Dua K, Bardan E, Ren J, Sui Z, Shaker R. Effect of chronic and acute cigarette smoking on the pharyngo-upper oesophageal sphincter contractile reflex and reflexive pharyngeal swallow. Gut 43: 537–541, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dua K, Bardan E, Ren J, Sui Z, Shaker R. Effect of chronic and acute cigarette smoking on the pharyngoglottal closure reflex. Gut 51: 771–775, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Duncan JR, Garland M, Myers MM, Fifer WP, Yang M, Kinney HC, Stark RI. Prenatal nicotine-exposure alters fetal autonomic activity and medullary neurotransmitter receptors: implications for sudden infant death syndrome. J Appl Physiol 107: 1579–1590, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Duvareille C, Beaudry B, St-Hilaire M, Boheimier M, Brunel C, Micheau P, Praud JP. Validation of a new automatic smoking machine to study the effects of cigarette smoke in newborn lambs. Lab Anim 44: 290–297, 2010 [DOI] [PubMed] [Google Scholar]
- 14. Dwyer JB, Broide RS, Leslie FM. Nicotine and brain development. Birth Defects Res C Embryo Today 84: 30–44, 2008 [DOI] [PubMed] [Google Scholar]
- 15. Fortier PH, Reix P, Arsenault J, Dorion D, Praud JP. Active upper airway closure during induced central apneas in lambs is complete at the laryngeal level only. J Appl Physiol 95: 97–103, 2003 [DOI] [PubMed] [Google Scholar]
- 16. Froen FJ, Akre H, Stray-Pedersen B, Saugstad OD. Adverse effects of nicotine and interleukin-1b on autoresuscitation after apnea in piglet: implications for sudden infant death syndrome. Pediatrics 105: e52–e57, 2000 [DOI] [PubMed] [Google Scholar]
- 17. Froen JF, Akre H, Stray-Pedersen Saugstad OD. Prolonged apneas and hypoxia mediated by nicotine and endotoxin in piglets. Biol Neonate 81: 119–125, 2002 [DOI] [PubMed] [Google Scholar]
- 18. Gosh D, Mishra MK, Das S, Kaushik DK, Basu A. Tobacco carcinogen induces microglial activation and subsequent neuronal damage. J Neurochem 110: 1070–1081, 2009 [DOI] [PubMed] [Google Scholar]
- 19. Goto K, Mirmiran M, Adams MM, Longford RV, Baldwin RB, Boeddiker MA, Ariagno RL. More awakening and heart rate variability during supine sleep in preterm infants. Pediatrics 103: 603–609, 1999 [DOI] [PubMed] [Google Scholar]
- 20. Hafstrom O, Mileread J, Sandberg KL, Sundell HW. Cardiorespiratory effects of nicotine exposure during development. Respir Physiol Neurobiol 149: 325–341, 2005 [DOI] [PubMed] [Google Scholar]
- 21. Harding R, Johnson P, McClelland ME. Liquid-sensitive laryngeal receptors in the developing sheep, cat and monkey. J Physiol 277: 409–422, 1978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Horne RS, Franco P, Adamson TM, Groswasser J, Kahn A. Influences of maternal cigarette smoking on infant arousability. Early Hum Dev 79: 49–58, 2004 [DOI] [PubMed] [Google Scholar]
- 23. Hunt CE, Hauck FR. Sudden infant death syndrome. CMAJ 174: 1861–1869, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Joseph DV, Jackson JA, Westaway J, Taub NA, Petersen SA, Wailoo MP. Effect of parental smoking on cotinine levels in newborns. Arch Dis Child 92: F484–F488, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kadhim H, Kahn A, Sebire G. Distinct cytokine profile in SIDS brain: a common denominator in a multifactorial syndrome? Neurology 61: 1256–1259, 2003 [DOI] [PubMed] [Google Scholar]
- 26. Kato I, Franco P, Groswasser J, Scaillet S, Kelmanson I, Togari H, Kahn A. Incomplete arousal processes in infants who were victims of sudden death. Am J Respir Crit Care Med 168: 1298–1303, 2003 [DOI] [PubMed] [Google Scholar]
- 27. Kinney HC, O'Donnal TJ, Kriger P, White WS. Early development changes in (3H) nicotine binding in human brainstem. Neuroscience 55: 1127–1130, 1993 [DOI] [PubMed] [Google Scholar]
- 28. Kinney HC, Thach BT. The sudden infant death syndrome. N Engl J Med 361: 795–805, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kott KS, Salt BH, McDonald RJ, Jhawar S, Bric JM, Joad JP. Effect of secondhand cigarette smoke, RSV bronchiolitis and parental asthma on urinary cysteinyl LTE4. Pediatr Pulmonol 8: 760–766, 2008 [DOI] [PubMed] [Google Scholar]
- 30. Koufman JA. The otolaryngologic manifestations of gastroesophageal reflux disease (GERD); a clinical investigation of 225 patients using ambulatory 24hrs pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope 101: 1–78, 1991 [DOI] [PubMed] [Google Scholar]
- 31. Lee JC, Stoll BJ, Downing SE. Properties of the laryngeal chemoreflex in neonatal piglets. Am J Physiol Regul Integr Comp Physiol 233: R30–R36, 1977 [DOI] [PubMed] [Google Scholar]
- 32. Lee KK, Birring SS. Cough and sleep. Lung 188, Suppl 1: S91–S94, 2010 [DOI] [PubMed] [Google Scholar]
- 33. Leiter JC, Böhm I. Mechanisms of pathogenesis in the sudden infant death syndrome. Respir Physiol Neurobiol 159: 127–138, 2007 [DOI] [PubMed] [Google Scholar]
- 34. Letourneau P, Dumont S, Kianicka I, Diaz V, Dorion D, Drolet R, Praud JP. Radiotelemetry system for apnea study in lambs. Respir Physiol 116: 85–93, 1999 [DOI] [PubMed] [Google Scholar]
- 35. Luo Z, Costy-Bennett S, Fregosi RF. Prenatal nicotine increases the strength of GABA receptor mediated inhibition of respiratory rhythm in neonates. J Physiol 561: 387–393, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. McDonnell M, Mehanni M, McGarvey C, Oregan M, Matthews TG. Smoking: the major risk factor for SIDS in Irish infants. Ir Med J 95: 111–113, 2002 [PubMed] [Google Scholar]
- 37. Moon RY, Horne RS, Hauck FR. Sudden infant death syndrome. Lancet 4: 1578–1587, 2007 [DOI] [PubMed] [Google Scholar]
- 38. Neff RA, Simmens SJ, Evans C, Mendelowitz D. Prenatal nicotine exposure alters central cardiorespiratory responses to hypoxia in rats: implications for sudden infant death syndrome. J Neurosci 24: 9261–9268, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Reix P, Fortier PH, Niyonsenga T, Arsenault J, Letourneau P, Praud JP. Non-nutritive swallowing and respiratory coordination in full-term newborn lambs. Respir Physiol Neurobiol 134: 209–218, 2003 [DOI] [PubMed] [Google Scholar]
- 40. Reix P, St-Hilaire M, Praud JP. Laryngeal sensitivity in the neonatal period: from bench to bedside. Pediatr Pulmonol 42: 674–682, 2007 [DOI] [PubMed] [Google Scholar]
- 41. Renolleau S, Letourneau P, Niyonsenga T, Praud JP. Thyroarytenoid muscle electrical activity during spontaneous apneas in preterm lambs. Am J Respir Crit Care Med 159: 1396–1404, 1999 [DOI] [PubMed] [Google Scholar]
- 42. Richardson HL, Walker AM, Horne RS. Maternal smoking impairs arousal patterns in sleeping infants. Sleep 32: 515–521, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Sato K, Nakashima T. Sleep-related deglutition in children. Ann Otol Rhinol Laryngol 116: 747–753, 2007 [DOI] [PubMed] [Google Scholar]
- 44. Slotkin TA. If nicotine is a developmental neurotoxicant in animal studies, dare we recommend nicotine replacement therapy in pregnant women and adolescents? Neurotoxicol Teratol 30: 1–19, 2008 [DOI] [PubMed] [Google Scholar]
- 45. St-Hilaire M, Nsegbe E, Gagnon-Gervais K, Samson N, Moreau-Bussière F, Fortier PH, Praud JP. Laryngeal chemoreflexes induced by acid, water, and saline in non-sedated newborn lambs during quiet sleep. J Appl Physiol 98: 2197–2203, 2005 [DOI] [PubMed] [Google Scholar]
- 46. St-Hilaire M, Samson N, Nsegbe E, Duvareilles C, Moreau-Bussiere F, Micheau P, Leblond J, Praud JP. Postnatal maturation of laryngeal chemoreflexes in the preterm lamb. J Appl Physiol 102: 1429–1438, 2007 [DOI] [PubMed] [Google Scholar]
- 47. Storey AT, Johnson P. Laryngeal water initiating apnea in the lambs. Exp Neurol 47: 42–55, 1975 [DOI] [PubMed] [Google Scholar]
- 48. Sullivan CE, Murphy E, Kozar LF, Phillipson EA. Waking and ventilatory responses to laryngeal stimulation in sleeping dogs. J Appl Physiol 45: 682–689, 1978 [DOI] [PubMed] [Google Scholar]
- 49. Sundell HW, Karmo H, Milerad J. Impaired cardiorespiratory recovery after laryngeal stimulation in nicotine-exposed young lambs. Pediatr Res 53: 104–112, 2003 [DOI] [PubMed] [Google Scholar]
- 50. Tirsoh E, Libon D, Bader D. The effect of maternal smoking during pregnancy on sleep respiratory and arousal patterns in neonates. J Perinatol 16: 435–438, 1996 [PubMed] [Google Scholar]
- 51. Thach BT. Maturation and transformation of reflexes that protect the laryngeal airway from liquid aspiration from fetal to adult life. Am J Med 111: 69S–77S, 2001 [DOI] [PubMed] [Google Scholar]
- 52. Thach BT. Some aspects of clinical relevance in the maturation of respiratory control in infants. J Appl Physiol 104: 1828–1834, 2008 [DOI] [PubMed] [Google Scholar]
- 53. Van der velde L, Curran AK, Filiano JJ, Darnall RA, Bartlett D, Jr, Leiter JC. Prolongation of the laryngeal chemoreflex after inhibition of the rostral ventral medulla in piglets: a role in SIDS? J Appl Physiol 94: 1883–1895, 2003 [DOI] [PubMed] [Google Scholar]
- 54. Xia L, Crane-Godreau M, Leiter JC, Bartlett D. Gestational cigarette smoke exposure and hyperthermic enhancement of laryngeal chemoreflex in rat pups. Respir Physiol Neurobiol 28: 161–166, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]


