Abstract
The viral warts also known as verruca vulgaris are caused by papova group of viruses. Such warts are commonly seen on the skin but occasionally may appear in the oral cavity. There are three types of warts namely verruca plana; verruca vulgaris and filiform. The incubation period of such warts varies from 6 weeks to a year. The warts spread by autoinoculation and seldom show koebner phenomenon. The majority of mucosal warts are seen in those children who also have warts on hands. In such cases the virus may be transported to the lips and tongue during an act of chewing of warts on hands. A 42-year-old male patient reported with the chief complaint of multiple, nontender, large white finger like projections on the right lateral border of the tongue. The duration of the lesion was approximately 3 years. Patient also had two similar papillary exophytic lesion over achilles tendon of right leg. Excision of the lesion from the right lateral border of the tongue was done under local anaesthesia and sent for histopathology examination, the histopathology report was suggestive of verruca vulgaris. Post-op follow up was done for 1 year, no recurrence of the lesion reported.
Keywords: Human papillomavirus (HPV), HPV2, Oral verrucae, Verruca vulgaris, Common warts, Viral wart
Introduction
Warts or verrucae are benign epidermal proliferations that have been recognized for thousands of years [1]. They were regarded as infectious by the end of the nineteenth century and a viral etiology was suggested in 1907 when CIUFFO [2] demonstrated the transmission of warts by a sterile, cell-free filtrate of wart tissue. Verruca vulgaris (VV), common wart or viral wart, is a virus-induced neoplasm of the skin caused by a human papillomavirus (HPV). As currently known, verruca vulgaris is associated with HPV types 2 and 4, flat warts with HPV-3 and 10, and Butchers’ warts with HPV-7 [3–5]. Oral verruca vulgaris (OVV) lesions appear similar to their cutaneous counterparts. Clinically, they are sessile, circumscribed, exophytic growths with a papillomatous surface. The tumor occurs at any age, with a preference in children and involves the vermilion and mucous membranes of the oral cavity. Presence of HPV in the oral cavity has been demonstrated by means of electron microscopy, immunohistochemistry and molecular biology methods [5–9].
Case Report
A 42-year-old male patient reported to the department of oral and maxillofacial surgery with the chief complaint of multiple fleshy, irregular surfaced, white finger like projections on the right lateral border of the tongue since 3 years (Fig. 1), which were progressively increasing in size and were not accompanied by pain and discharge. Similar lesions were present on the skin over achilles tendon of the right leg (Fig. 5). Examination revealed multiple, non tender, white finger like projections measuring around 2 × 1 cm, situated on the right lateral border of the tongue, which was not associated with lymphadenopathy. Patient was taken up for the surgery on day care basis after getting done normal investigation reports. Tongue stitch has been secured with 3-0 black silk, the wide excision of the lesion from the right lateral border of the tongue was done under local anesthesia (Figs. 2, 3), hemostasis was achieved with cauterization, surgical wound was irrigated with betadine and closed with 3-0 vicryl, then the specimen sent for histopathology examination (Fig. 4), tongue stitch was removed and patient was discharged on the same day after prescribing routine antibiotics and analgesics for 5 days. Histopathology report suggestive of verruca vulgaris and post-operative follow up was done for 1 year, no recurrence of the lesion reported (Fig. 6).
Fig. 1.

Showing lesion on Rt lateral border of tongue
Fig. 5.

Similar exophytic growth on leg
Fig. 2.

Excision of tongue lesion
Fig. 3.

Tongue showing excised lesion
Fig. 4.

Excised tongue specimen
Fig. 6.

One year post-operative
Differential Diagnosis
Squamous papilloma, condylomata accuminatum, exophytic squamous cell carcinoma, keratoacanthoma, exophytic verrucous carcinoma, focal epithelial hyperplasia, verruciform xanthoma [10].
Histopathology
The verruca vulgaris is characterized by a proliferation of hyperkeratotic stratified squamous epithelium arranged into fingerlike or pointed projections with connective tissue cores (Fig. 7). Chronic Inflammatory cells often infiltrate the supporting connective tissue. Elongated rete ridges tend to converge toward the center of the lesion, producing a ‘cupping’ effect. A prominent granular cell layer (hypergranulosis) exhibits coarse, clumped keratohyalin granules. Abundant koilocytes are often seen in the superficial spinous layer. Koilocytes are HPV-altered epithelial cells with perinuclear clear spaces and small, dark nuclei (Pyknosis). Eosinophilic intranuclear viral inclusions are often noted within the cells of the granular layer.
Fig. 7.
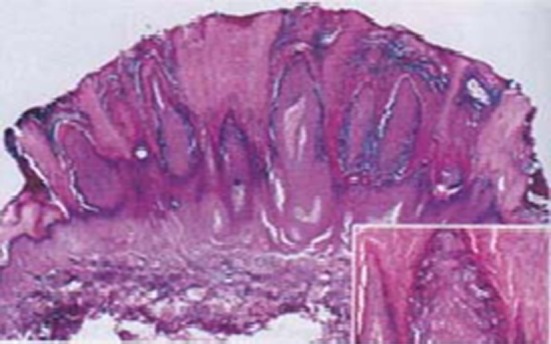
Histopathology of lesions showing papillary projections
Discussion
Lesions of oral verruca vulgaris account for a small percentage of oral papillomatous lesions. When found, they exhibit varied clinical presentations, from exophytic lesions to multiple or spreading verrucous lesions. Koilocytes are a characteristic feature of papillomavirus infection [11], and they were observed in 89% of the oral verrucae examined.
Verruca Vulgaris is frequently discovered in children, but occasional lesions may arise even into middle age. The skin of the hands is usually the site of infection. When the oral mucosa is involved, the lesions are usually found on the vermilion border, labial mucosa or tongue. Typically, the verruca appears as a painless papule or nodule with papillary projections or a rough pebbly surface. It may be pedunculated or sessile. Cutaneous lesions may be pink, yellow or white; Oral lesions are almost always white. Verruca Vulgaris enlarges rapidly to its maximum size and the size remains constant for months or years thereafter unless the lesion is irritated. Multiple or clustered lesions are common. On occasion, extreme accumulation compact keratin may result in a hard surface projection several millimeters in height, termed as cutaneous horn or keratin horn. It is generally believed that condylomata accuminatum and verruca vulgaris are lesions caused by identical viruses, but showing different clinical and pathologic manifestations according to the site of attack [12]. It is demonstrated that inoculation of a bacteria free and cell-free extract of condylomata accuminatum into human skin produces verruca vulgaris or verruca plana and inoculation into mucous membrane produces condylomata. But these two types of warts have much dissimilarity. The condylomata accuminatum is a venereal disease while verruca vulgaris is non venereal; the former responds to podophyllin tincture and the latter to trichloraceticacid. The common skin warts are usually associated with HPV 2&4 whereas flat type harbor HPV 3&10; while condylomata accuminatum is associated with HPV 6&11. Histologically the condylomata accuminatum shows parakeratotic stratified squamous epithelium with lymphocytic infiltrate in subepithelial tissue; the verruca vulgaris shows papillomatosis, alternating hyperkeratosis with parakeratosis and long epithelial ridges which, at the margin of the lesions are bent inwards.
Other treatment modalities [13, 14].
Drugs: Such as cimetidine and levamisole have been tried with varying success rates.
Retinoids: Derived from Vitamin-A, these medications disrupt the wart’s skin cell growth. Available as retinoid cream or oral medication.
-
Other medications
Immunotherapy: Topical immunotherapy medications that may be prescribed for stubborn warts like squaric acid dibutylester (SADBE) and a gel called Imiquimod (Aldara). If the warts are severe and very treatment-resistant, then you may inject interferon-alfa medications directly into wart.
Salicylic acid: Wart medications and patches are available which contains 17% salicylic acid.
Cantharidin: A substance extracted from the blister beetle on the warts. Typically, the extract is mixed with other chemicals painted onto the skin and covered with a bandage.
Duct tape: It consists of covering the wart with duct tape for a total period of two months. The tape is changed every 6 days and left off overnight on the sixth night, and reapplied the next morning for another 6 days.
Freezing (Cryotherapy or liquid nitrogen therapy): Liquid nitrogen to destroy the wart by freezing it. This treatment is not too painful and is often effective, may need repeated treatments.
Laser: Laser surgery can be expensive and it may leave a scar.
Minor surgery: This involves cutting away the wart tissue or destroying it by using an electric needle in a process called electrodessication.
References
- 1.Lowy DR, Androphy EJ. Warts. In: Fitzpatrick TB, Eisen AZ, Wolff K, editors. Dermatology in general medicine; New York: McGraw-Hill; 1987. pp. 2355–2364. [Google Scholar]
- 2.Ciuffo G. Innesto positive con filtrate di verruca volgare. G Ital Mal Venereol. 1907;42:12–17. [Google Scholar]
- 3.Beutner KR. Human papilloma virus infection. J Am Acad Dermatol. 1989;20:114–123. doi: 10.1016/S0190-9622(89)80004-0. [DOI] [PubMed] [Google Scholar]
- 4.Orth G, Favre M, Crossant O. Characterization of a new type of human papillomavirus that causes skin warts. J Virol. 1977;24:108–120. doi: 10.1128/jvi.24.1.108-120.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Orth G, Jablonska S, Favre M, Croissant O, Obalek S, Jarzabek-Chorzelska M, Jibard N. Identification of papillomavirus in butchers’ warts. J Invest Dermatol. 1981;76:97–102. doi: 10.1111/1523-1747.ep12525394. [DOI] [PubMed] [Google Scholar]
- 6.Eversole LR, Laipis PJ, Green TL. Human papillomavirus type 2 DNA in oral labial verruca vulgaris. J Cutan Pathol. 1987;14:319–325. doi: 10.1111/j.1600-0560.1987.tb01531.x. [DOI] [PubMed] [Google Scholar]
- 7.Green TL, Eversole LR, Leider AS. Oral and labial verruca vulgaris: clinical, histologic and immunohistochemical evaluation. Oral Surg Oral Med Oral Pathol. 1986;62:410–416. doi: 10.1016/0030-4220(86)90290-2. [DOI] [PubMed] [Google Scholar]
- 8.Jenson AB, Lancaster WD, Hartmann D, Shaffer EL. Frequency and distribution of papillomavirus structural antigens in verrucae, multiple papillomas and condylomata of the oral cavity. Am J Pathol. 1982;107:212–218. [PMC free article] [PubMed] [Google Scholar]
- 9.Jin YT, Toto PD. Detection of human papovavirus antigen in oral papillary lesions. Oral Surg Oral Med Oral Pathol. 1984;58:702–705. doi: 10.1016/0030-4220(84)90039-2. [DOI] [PubMed] [Google Scholar]
- 10.Terezhalmy GT, Rilley CK, Moore WS. Oral verruca vulgaris. Quintessence Int. 2002;33(2):162–163. [PubMed] [Google Scholar]
- 11.Koss LG, Durfee GR. Unusual patterns of squamous epithelium of the uterine cervix and pathologic study of koilocytotic atypia. Ann NY Acad Sci. 1956;63:1245–1261. doi: 10.1111/j.1749-6632.1956.tb32134.x. [DOI] [PubMed] [Google Scholar]
- 12.Praetorius-Clausen F. Rare oral viral disorders (molloscum-contagiosum, localised keratoacanthoma verrucoe, condyloma acuminatum and focal epithetial hyperplasia) Oral Surg. 1972;34:604–618. doi: 10.1016/0030-4220(72)90344-1. [DOI] [PubMed] [Google Scholar]
- 13.www.mayoclinic.com/health/common-warts/treatment-and-drugs (2009)
- 14.Prasad D, Pandhi R, Juneja A, Negi KS. Verruca vulgaris. Pediatr Dermatol. 2001;18(4):349–352. doi: 10.1046/j.1525-1470.2001.01951.x. [DOI] [PubMed] [Google Scholar]


