Abstract
Background:
Obstructive sleep apnea (OSA) is associated with diverse health risks, including death. However, the role of OSA as a risk factor for death has never been studied in Asians. This study is aimed at evaluating the influence of OSA on the mortality in Korean sleep clinic population.
Methods:
A total of 2,240 patients who underwent in-laboratory full-night polysomnography due to snoring or sleep apnea were included. The patients were categorized based on apnea-hypopnea index (AHI)/hour. Death records were provided from the Statistics Korea. A Cox-proportional hazard regression model and Kaplan-Meier survival curve were used for analysis and demonstration of the all-cause mortality and cardiovascular mortality.
Results:
The all-cause mortality risk adjusted for age, sex, body mass index, diabetes, hypertension, cardiovascular diseases, and previous history of stroke was significantly associated with the increased severity of OSA. The adjusted hazard ratio (HR) for all-cause mortality in the severe OSA group (AHI ≥ 30) vs. reference group (5 < AHI) was 2.47 (95% confidence interval [CI], 1.09-5.57) and the adjusted HR for cardiovascular mortality was 4.66 (CI 1.03-21.08). After adjusting for whether the patients were treated or untreated, the HR for all-cause and cardiovascular mortality in the severe OSA group vs. reference group were 2.14 (p = 0.079) and 4.19 (p = 0.076), respectively.
Conclusions:
The present study showed that the increased mortality was also associated with the increased severity of OSA in Koreans as shown in the studies performed in the Western countries.
Citation:
Lee JE; Lee CH; Lee SJ; Ryu Y; Lee WH; Yoon IY; Rhee CS; Kim JW. Mortality of patients with obstructive sleep apnea in Korea. J Clin Sleep Med 2013;9(10):997-1002.
Keywords: Obstructive sleep apnea, cohort, all-cause mortality, cardiovascular mortality, sleep disordered breathing, Asians
Obstructive sleep apnea (OSA) is a chronic condition characterized by frequent episodes of upper airway collapse during sleep. To date, epidemiologic studies have estimated that the prevalence of adults with apnea-hypopnea index (AHI) ≥ 5 is 17% to 26%.1–4 A population-based cohort study performed in the U.S. showed that the prevalence of mild (5 ≤ AHI < 15), moderate (15 ≤ AHI < 30), and severe OSA (AHI ≥ 30) in middle-aged adults was around 14%, 5%, and 4%, respectively. After the high prevalence of OSA was uncovered in adults, more attention was turned to its clinical significance in health2,5,6; there have been population-based and longitudinal studies to show its natural history and adverse health effects.2–5,7–9 OSA has been shown to be an important risk factor for many clinically important conditions, such as cardiovascular diseases, cerebrovascular diseases, metabolic syndrome, and even death.10–14 Moreover, if left untreated, it may lead to excessive daytime sleepiness, impaired congnitive function, depression, impaired work performance contributing to motor vehicle crashes and job-related accidents, and decrements in health-related quality of life.15
While most of the epidemiologic studies have been performed in Western countries, there have been just a few epidemiologic studies in Asians. Although there was no significant difference between Asians and Caucasians in regard to prevalence, ethnicity might be a factor affecting comorbidities of OSA because there are differences, such as craniofacial morphology and body mass index (BMI).5,16,17 Furthermore, though the significance of OSA as an important risk factor for several diseases is widely accepted, the evidence supporting the association between OSA and mortality is not enough, even in the studies of Western countries.18–22 In the present study, we conducted an observational cohort study to evaluate mortality in the Korean sleep clinic population.
BRIEF SUMMARY
Current Knowledge/Study Rationale: There is a need to identify the relationship between OSA and mortality in Asians. Evidence supporting the influence of severe OSA on increased death risk is not sufficient, even in Western population-based studies. Furthermore, Asians are different from Caucasians in several aspects such as body fat composition and skeletal structure.
Study Impact: In our Korean cohort, we identified that all-cause and cardiovascular mortality was significantly correlated with OSA severity. This study suggests that more attention should be paid to Asians with OSA and emphasizes the need for early detection of OSA and its efficient treatment.
METHODS
Study Sample
An observational cohort in the Sleep Center of Seoul National University Bundang Hospital consisted of patients who visited the center due to snoring or witnessed sleep apnea from January 2003 through January 2009, underwent a full-night in-laboratory polysomnography (PSG), and were ≥ 40 years old. Subjects with total sleep time < 4 h were excluded from the present study. Data regarding demographic parameters, daytime sleepiness (Epworth Sleepiness Scale), and medical risk factors such as hypertension, diabetes, cardiovascular diseases, previous stroke history, and prescribed treatment were collected. Patients with AHI ≥ 5 underwent one of the following specific treatments: continuous positive airway pressure (CPAP); mandibular advancement device (MAD); upper airway surgery; or combination therapy of CPAP, MAD, or surgery. This study has been approved by the Seoul National University Bundang Hospital Institutional Review Board.
Full-Night In-Laboratory Polysomnography
All the subjects underwent a full-night in-laboratory PSG using an Embla N7000 recording system (Embla; Medcare, Reykjavik, Iceland) and standard electrodes and sensors with the supervision of an experienced technician at the sleep center as previously described.23–25 PSG included the following parameters: electroencephalography, electrooculography, submental electromyography, lower leg electromyography, electrocardiography, leg movement, chest and abdominal movement, nasal airflow, mouth airflow (thermistor), pulse oximetry, and body position. Based on the standard criteria, sleep stages were scored in 30-sec epochs. Apnea was defined as absence of the airflow ≥ 10 seconds. Hypopnea was defined as a recognizable reduction of the airflow with reduction of oxygen saturation ≥ 4% from the baseline or an arousal. Patients were categorized into 4 severity groups based on AHI: no OSA (reference, AHI < 5), mild OSA (5 ≤ AHI < 15), moderate OSA (15 ≤ AHI < 30), and severe OSA (AHI ≥ 30).
Mortality Status
Deaths in the cohort having occurred up to December 31, 2011, were identified by matching each subject's Korean Identification Number and name with death records from the Statistics Korea, a national organization for statistics. The date of death and primary cause of death were collected from the national death statistics. The causes of death were categorized into 4 groups described in a previous report26: (1) cardiovascular diseases and stroke, including acute myocardial infarction, acute ischemic heart disease, sudden cardiac arrest, and cardiac dysrhythmias; (2) fatal events including accidents, injuries and falls; (3) cancer; (4) others, including pneumonia, gastrointestinal bleeding, end-stage renal disease, amyloidosis, and so forth.
Statistical Analysis
Kaplan-Meier survival analysis methods were used to compare survival rates according to the severity category with a log-rank test to assess statistical differences. A Cox proportional hazards regression analysis was used to estimate hazard ratios (HR) and 95% confidence interval (CI) adjusted for sex, age, BMI, and medical conditions such as diabetes, hypertension, cardiovascular diseases, previous history of stroke, and treatment for OSA. All significance tests were two-sided, and a value of p < 0.05 was considered statistically significant. SPSS version 18.0 (SPSS Inc., Chicago, IL) software was used.
RESULTS
Baseline Characteristics
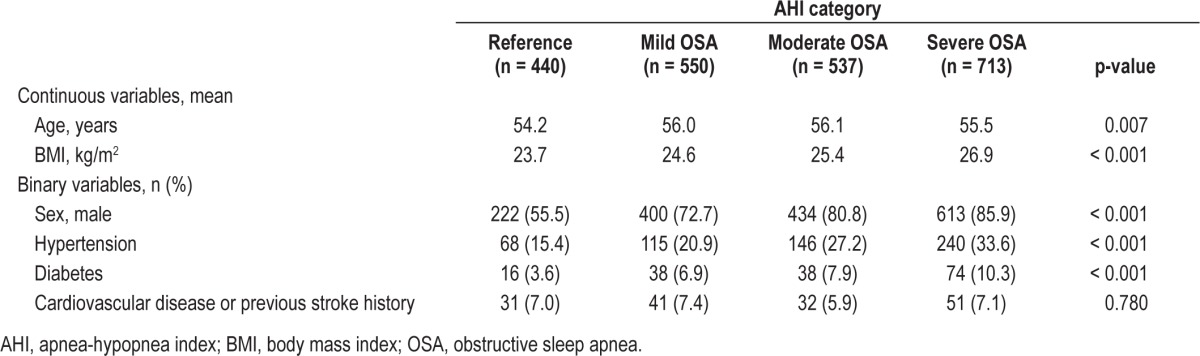
A total of 2,240 subjects (1,669 males and 571 females) were included in the present cohort. The average observation period was 61.4 months (range, 34.0-106.0 months). Of 2,240 subjects, 1,800 patients had AHI ≥ 5/h on PSG. The average age was 55 years (range 40-87 years). Baseline characteristics of the subjects are shown in Table 1. BMI increased as OSA severity increased. The prevalence of hypertension and diabetes mellitus was significantly higher in patients with OSA than in those without OSA (p < 0.001). The initial status of subjects in terms of cardiovascular diseases was not significantly different according to the severity of OSA (p = 0.780).
Table 1.
General characteristics of the patients with OSA and controls
Among 1,800 patients with OSA, 735 patients were treated with CPAP (n = 227), MAD (n = 242), surgery (n = 203), or combined treatment (n = 63). The other 1,065 patients were not specifically treated because they were lost to follow-up, refused such treatments, wanted to reduce body weight, and/or to try to sleep in the lateral decubitus position.
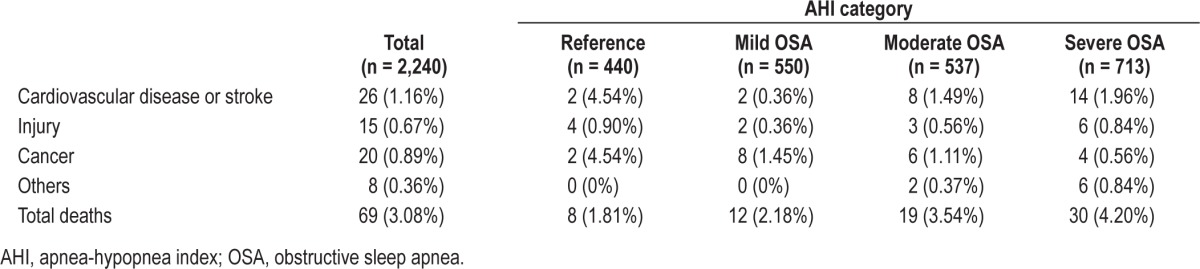
Mortality According to the Severity of OSA
A total of 69 deaths (3.08%) were identified. The median age at death was 66.8 years (range, 42-86 years). All-cause mortality and cause-specific deaths are shown in Table 2. The mortality rate was 1.81%, 2.18%, 3.54%, and 4.20% in no OSA, mild, moderate, and severe OSA groups, respectively. Cardiovascular diseases or stroke accounted for 37.7% (26/69) of all deaths. Death from cardiovascular disease or stroke accounted for 25.0% (2/8), 16.7% (2/12), 42.1% (8/19), and 46.7.0% (14/30) of deaths in no OSA, mild, moderate, and severe OSA groups, respectively.
Table 2.
Cause-specific mortality
Survival Rate and Hazard Ratio
There was no significant difference between males and females in the overall survival (p = 0.725). The increased OSA severity was likely to be associated with a reduction in survival probabilities (p = 0.054; Figure 1), and the difference was significant when patients with AHI < 30 were compared to those with AHI ≥ 30 (p = 0.030; Figure 2).
Figure 1. Kaplan-Meier survival curves for all-cause deaths.
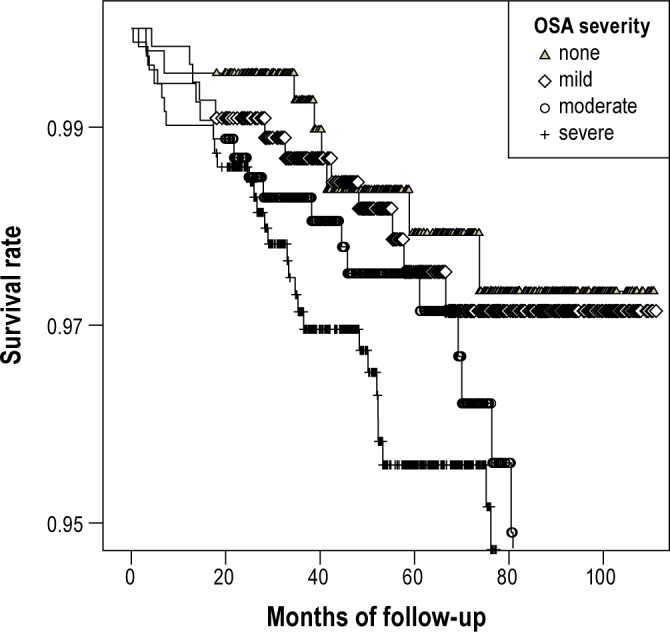
When the patients were classified into 4 groups—none (AHI < 5), mild (5 ≤ AHI < 15), moderate (15 ≤ AHI < 30), and severe (AHI ≥ 30)—the increased OSA severity was likely to be associated with a reduction in survival (p = 0.054). AHI, apnea-hypopnea index; OSA, obstructive sleep apnea.
Figure 2. Kaplan-Meier survival curves for all-cause deaths.
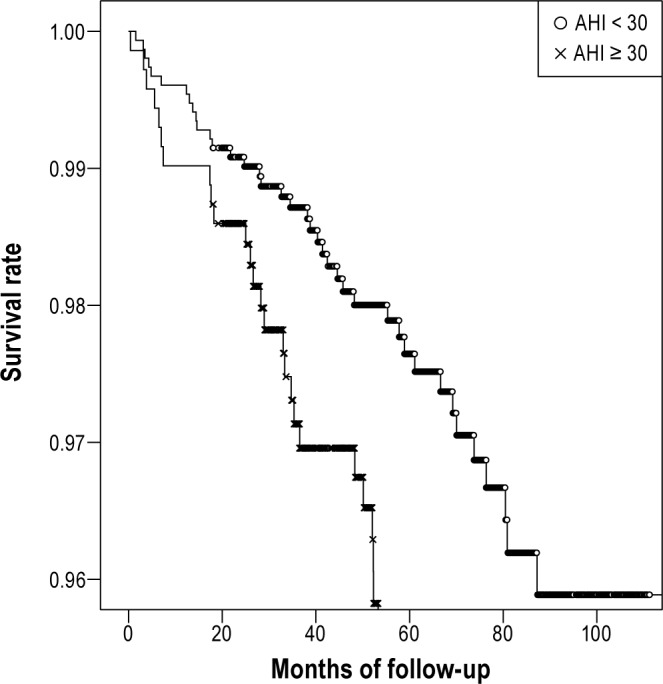
When the patients were classified into 2 groups, there was a significant difference in survival between the patients with AHI < 30 and those with AHI ≥ 30 (p = 0.030). AHI, apnea-hypopnea index; OSA, obstructive sleep apnea.
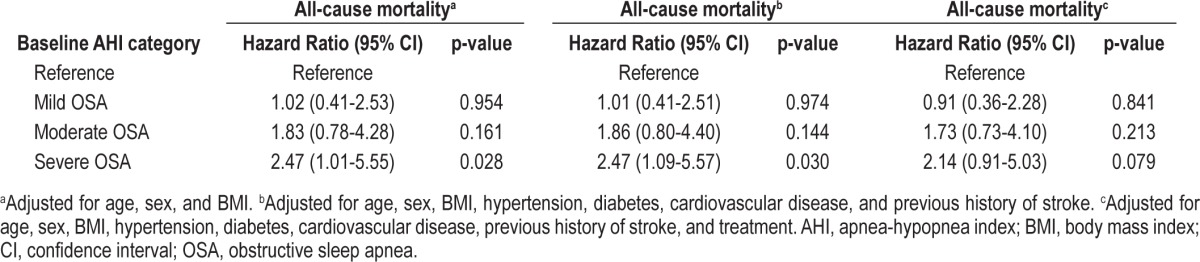
After adjustment for age, sex, and BMI, the trend analysis revealed that OSA retained a statistically significant association with death in a stepwise increasing pattern (Table 3). The adjusted HR for all-cause mortality in the severe OSA group vs. reference group was 2.47 (95% CI 1.01-5.55; p = 0.028). After adjustment for age, sex, BMI, hypertension, diabetes, cardiovascular diseases, and previous history of stroke, the adjusted HR for all-cause mortality in the severe OSA group vs. reference group was 2.47 (95% CI 1.09-5.57; p = 0.030). After adjusting for whether the patients were treated or untreated, the HR for all-cause mortality in the severe OSA group vs. reference group was 2.14 (95% CI 0.91-5.03; p = 0.079).
Table 3.
Hazard ratios for all-cause mortality
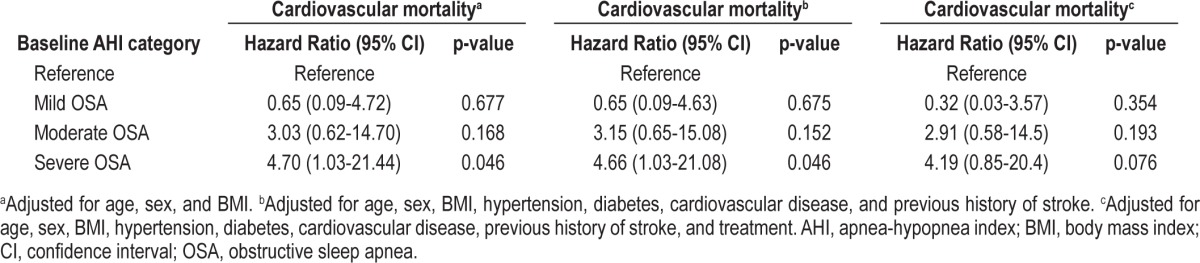
The cardiovascular mortality adjusted for age, sex, BMI, hypertension, diabetes, cardiovascular diseases, and previous history of stroke was significantly elevated in the severe OSA group vs. reference group (HR 4.66; 95% CI 1.03-21.08; p = 0.046; Table 4). After prescription of treatment was added as a covariate to the hazard model, the adjusted HR for cardiovascular mortality was 4.19 (95% CI 0.85-20.4; p = 0.076) in severe OSA group vs. reference group.
Table 4.
Hazard ratios for cardiovascular mortality
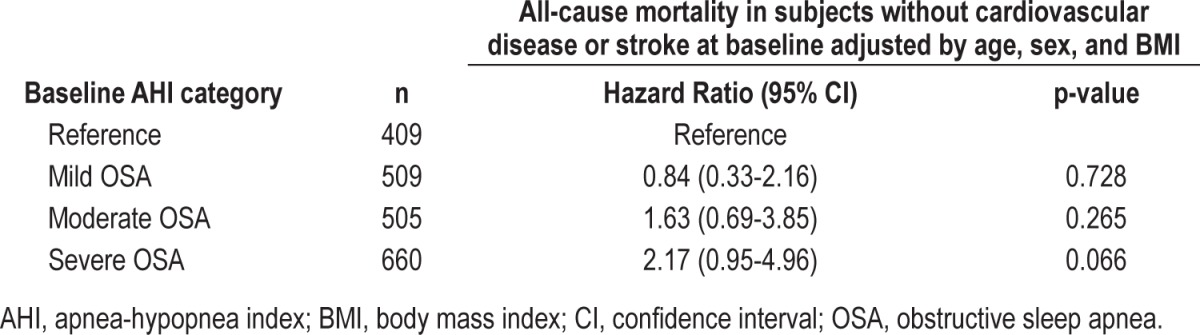
The HR for all-cause death in OSA patients who did not have cardiovascular diseases other than hypertension at enrollment was analyzed. A total of 156 patients had cardiovascular disease at baseline. The HR for mortality adjusted by age, sex, and BMI was 2.17 (95% CI 0.95-4.96; p = 0.066) in the severe OSA group vs. reference group (Table 5).
Table 5.
Hazard ratios for all-cause death in subjects without cardiovascular diseases or history of stroke at baseline
DISCUSSION
This is an observational cohort study conducted in a large Korean sleep clinic population to investigate the influence of OSA on mortality. To our best knowledge, the present study showed a significant association between OSA and mortality in Asians for the first time. The present study demonstrated that OSA may be a significant risk factor for death in Asians as previously shown in the Western population.22,26 Asians are different from Caucasians in some aspects important for OSA. Firstly, Asians are generally known to have a higher percentage of body fat than the Western population at the same BMI level.27 Previous comparative studies of Asian and Caucasian male patients with OSA demonstrated that Asians were less obese despite the presence of severe OSA,28,29 even when matched for risk factors such as age, gender, and BMI. The higher central fat distribution was found at a lower level of BMI in Asians than in Caucasians.30,31 Secondly, Asians have smaller mandibles; therefore, the upper airway may be more collapsible and have propensity for more severe OSA. Cephalometric analysis revealed that the Asians have maxillomandibular protrusion, narrower cranial base angle, larger posterior airway space, and more superiorly positioned hyoid bone compared with Caucasians.29,31 The narrower cranial base in the Asian population may have an important implication in the pathogenesis of OSA because it affects particularly the airway in the nasopharygneal and retropalatal regions. Thus, epidemiologic data of OSA acquired from the Western population cannot be directly applied to Asians, and independent investigations for Asians are mandatory.16,28,30,32
Our study indicated that the all-cause mortality risk was 2.47 times higher in subjects with OSA with AHI ≥ 30 compared to those with AHI < 5, independent of age, sex, BMI, and other chronic diseases. After excluding patients diagnosed as having cardiovascular disease at the time of enrollment, severe OSA tended to be associated with increased all-cause mortality compared to the reference group. In a large population-based study performed in the U.S., the adjusted HR for all-cause mortality in subjects with AHI ≥ 30 in comparison to those with AHI < 5 was 3.0, and it increased to 3.8 when the persons under treatment with continuous positive airway pressure were excluded.26 An observational cohort study of a large population of the U.S. also showed a significant association of OSA with stroke or death.22 In the above study, both OSA patients and controls were recruited from the population referred to sleep centers. In another observational cohort study conducted in Spain, patients with OSA enrolled from a sleep clinic were compared to the general population. It was shown that mortality was significantly higher in subjects with untreated severe OSA than in healthy controls.33,34
Our study also investigated the influences of cardiovascular disease on the association between OSA and cardiovascular mortality by including or excluding the initial status of cardiovascular diseases at baseline. Cardiovascular mortality was significantly higher in the group with severe OSA compared to the reference group. When the initial presence of cardiovascular diseases was adjusted, the severe OSA group tended to be associated with increased all-cause mortality compared to the reference group. This finding suggests that severe OSA may be an independent risk factor increasing cardiovascular mortality in Asians. In addition, an analysis in subjects without cardiovascular diseases or stroke at baseline showed that OSA with AHI ≥ 30 was likely to be a risk factor for death in the above condition.
We also investigated the effect of OSA therapy on mortality irrespective of therapeutic modalities as in the previous studies,11,19,35–38 by evaluating mortality according to whether the patients were treated. Although the risk of death was significantly higher in the severe OSA group, there was no significant difference in mortality between the severe OSA group and reference group after adjusting for the treatment factor. These may indicate the potential beneficial effects of treatment for OSA on mortality associated with severe OSA. This finding is consistent with the results of several other studies, revealing a greater mortality in patients with untreated OSA.21,26,39
Our study has some limitations. Firstly, as our study is not population based, there could be a selection bias resulting in overestimation of the mortality. Secondly, since our public health insurance program does not reimburse the cost of PSG, it is likely that the cohort consisted of patients with somewhat greater income and access to medical service; thus our finding might underestimate the real mortality risk of OSA. Thirdly, the average follow-up period of 61.4 months may not be sufficient to determine the association between OSA severity and mortality. This could lead to underestimation of the risk. Fourthly, we could not exactly assess the effects of treatment on the risk of death according to the therapeutic modality because the adherence and compliance for the treatment were not fully evaluated for all the patients.
CONCLUSION
The present study has a clinical implication that increased mortality, shown in studies in Western countries, is also associated with increased severity of OSA in Asians. In particular, severe OSA (AHI ≥ 30) was an independent risk factor for death. These findings emphasize the need for early detection of OSA and its efficient treatment and follow-up. Since this study has a limitation of an observational cohort study, a longitudinal randomized controlled study is necessary to show the association between OSA and mortality in Asians in the future.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Guilleminault C, Tilkian A, Dement WC. The sleep apnea syndromes. Annu Rev Med. 1976;27:465–84. doi: 10.1146/annurev.me.27.020176.002341. [DOI] [PubMed] [Google Scholar]
- 2.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 3.Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A. Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med. 1998;157:144–8. doi: 10.1164/ajrccm.157.1.9706079. [DOI] [PubMed] [Google Scholar]
- 4.Duran J, Esnaola S, Rubio R, Iztueta A. Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 yr. Am J Respir Crit Care Med. 2001;163:685–9. doi: 10.1164/ajrccm.163.3.2005065. [DOI] [PubMed] [Google Scholar]
- 5.Kripke DF, Ancoli-Israel S, Klauber MR, Wingard DL, Mason WJ, Mullaney DJ. Prevalence of sleep-disordered breathing in ages 40-64 years: a population-based survey. Sleep. 1997;20:65–76. doi: 10.1093/sleep/20.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gislason T, Almqvist M, Eriksson G, Taube A, Boman G. Prevalence of sleep apnea syndrome among Swedish men--an epidemiological study. J Clin Epidemiol. 1988;41:571–6. doi: 10.1016/0895-4356(88)90061-3. [DOI] [PubMed] [Google Scholar]
- 7.Quan SF, Howard BV, Iber C, et al. The Sleep Heart Health Study: design, rationale, and methods. Sleep. 1997;20:1077–85. [PubMed] [Google Scholar]
- 8.Bixler EO, Vgontzas AN, Lin HM, et al. Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med. 2001;163:608–13. doi: 10.1164/ajrccm.163.3.9911064. [DOI] [PubMed] [Google Scholar]
- 9.Redline S, Tosteson T, Tishler PV, Carskadon MA, Millman RP. Studies in the genetics of obstructive sleep apnea. Familial aggregation of symptoms associated with sleep-related breathing disturbances. Am Rev Respir Dis. 1992;145:440–4. doi: 10.1164/ajrccm/145.2_Pt_1.440. [DOI] [PubMed] [Google Scholar]
- 10.Lindberg E, Janson C, Svardsudd K, Gislason T, Hetta J, Boman G. Increased mortality among sleepy snorers: a prospective population based study. Thorax. 1998;53:631–7. doi: 10.1136/thx.53.8.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ancoli-Israel S, Kripke DF, Klauber MR, et al. Morbidity, mortality and sleep-disordered breathing in community dwelling elderly. Sleep. 1996;19:277–82. doi: 10.1093/sleep/19.4.277. [DOI] [PubMed] [Google Scholar]
- 12.Mooe T, Rabben T, Wiklund U, Franklin KA, Eriksson P. Sleep-disordered breathing in men with coronary artery disease. Chest. 1996;109:659–63. doi: 10.1378/chest.109.3.659. [DOI] [PubMed] [Google Scholar]
- 13.Koskenvuo M, Kaprio J, Telakivi T, Partinen M, Heikkila K, Sarna S. Snoring as a risk factor for ischaemic heart disease and stroke in men. BMJ (Clin Res Ed) 1987;294:16–9. doi: 10.1136/bmj.294.6563.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shahar E, Whitney CW, Redline S, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163:19–25. doi: 10.1164/ajrccm.163.1.2001008. [DOI] [PubMed] [Google Scholar]
- 15.Leger D. The cost of sleep-related accidents: a report for the National Commission on Sleep Disorders Research. Sleep. 1994;17:84–93. doi: 10.1093/sleep/17.1.84. [DOI] [PubMed] [Google Scholar]
- 16.Ip MS, Lam B, Lauder IJ, et al. A community study of sleep-disordered breathing in middle-aged Chinese men in Hong Kong. Chest. 2001;119:62–9. doi: 10.1378/chest.119.1.62. [DOI] [PubMed] [Google Scholar]
- 17.Kim J, In K, You S, et al. Prevalence of sleep-disordered breathing in middle-aged Korean men and women. Am J Respir Crit Care Med. 2004;170:1108–13. doi: 10.1164/rccm.200404-519OC. [DOI] [PubMed] [Google Scholar]
- 18.He J, Kryger MH, Zorick FJ, Conway W, Roth T. Mortality and apnea index in obstructive sleep apnea: experience in 385 male patients. Chest. 1988;94:9–14. [PubMed] [Google Scholar]
- 19.Lavie P, Lavie L, Herer P. All-cause mortality in males with sleep apnoea syndrome: declining mortality rates with age. Eur Respir J. 2005;25:514–20. doi: 10.1183/09031936.05.00051504. [DOI] [PubMed] [Google Scholar]
- 20.Campos-Rodriguez F, Pena-Grinan N, Reyes-Nunez N, et al. Mortality in obstructive sleep apnea-hypopnea patients treated with positive airway pressure. Chest. 2005;128:624–33. doi: 10.1378/chest.128.2.624. [DOI] [PubMed] [Google Scholar]
- 21.Wang H, Parker JD, Newton GE, et al. Influence of obstructive sleep apnea on mortality in patients with heart failure. J Am Coll Cardiol. 2007;49:1625–31. doi: 10.1016/j.jacc.2006.12.046. [DOI] [PubMed] [Google Scholar]
- 22.Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:2034–41. doi: 10.1056/NEJMoa043104. [DOI] [PubMed] [Google Scholar]
- 23.Lee CH, Kim JW, Lee HJ, et al. Determinants of treatment outcome after use of the mandibular advancement device in patients with obstructive sleep apnea. Arch Otolaryngol Head Neck Surg. 2010;136:677–81. doi: 10.1001/archoto.2010.106. [DOI] [PubMed] [Google Scholar]
- 24.Lee CH, Kim JW, Lee HJ, et al. An investigation of upper airway changes associated with mandibular advancement device using sleep videofluoroscopy in patients with obstructive sleep apnea. Arch Otolaryngol Head Neck Surg. 2009;135:910–4. doi: 10.1001/archoto.2009.112. [DOI] [PubMed] [Google Scholar]
- 25.Lee CH, Mo JH, Seo BS, Kim DY, Yoon IY, Kim JW. Mouth opening during sleep may be a critical predictor of surgical outcome after uvulopalatopharyngoplasty for obstructive sleep apnea. J Clin Sleep Med. 2010;6:157–62. [PMC free article] [PubMed] [Google Scholar]
- 26.Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31:1071–8. [PMC free article] [PubMed] [Google Scholar]
- 27.Jee SH, Sull JW, Park J, et al. Body-mass index and mortality in Korean men and women. N Engl J Med. 2006;355:779–87. doi: 10.1056/NEJMoa054017. [DOI] [PubMed] [Google Scholar]
- 28.Ong KC, Clerk AA. Comparison of the severity of sleep-disordered breathing in Asian and Caucasian patients seen at a sleep disorders center. Respir Med. 1998;92:843–8. doi: 10.1016/s0954-6111(98)90386-9. [DOI] [PubMed] [Google Scholar]
- 29.Li KK, Powell NB, Kushida C, Riley RW, Adornato B, Guilleminault C. A comparison of Asian and white patients with obstructive sleep apnea syndrome. Laryngoscope. 1999;109:1937–40. doi: 10.1097/00005537-199912000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Li KK, Kushida C, Powell NB, Riley RW, Guilleminault C. Obstructive sleep apnea syndrome: a comparison between Far-East Asian and white men. Laryngoscope. 2000;110:1689–93. doi: 10.1097/00005537-200010000-00022. [DOI] [PubMed] [Google Scholar]
- 31.Villaneuva AT, Buchanan PR, Yee BJ, Grunstein RR. Ethnicity and obstructive sleep apnoea. Sleep Med Rev. 2005;9:419–36. doi: 10.1016/j.smrv.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 32.Sakakibara H, Tong M, Matsushita K, Hirata M, Konishi Y, Suetsugu S. Cephalometric abnormalities in non-obese and obese patients with obstructive sleep apnoea. Eur Respir J. 1999;13:403–10. doi: 10.1183/09031936.99.13240399. [DOI] [PubMed] [Google Scholar]
- 33.Marti S, Sampol G, Munoz X, et al. Mortality in severe sleep apnoea/hypopnoea syndrome patients: impact of treatment. Eur Respir J. 2002;20:1511–8. doi: 10.1183/09031936.02.00306502. [DOI] [PubMed] [Google Scholar]
- 34.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 35.Bliwise DL, Bliwise NG, Partinen M, Pursley AM, Dement WC. Sleep apnea and mortality in an aged cohort. Am J Public Health. 1988;78:544–7. doi: 10.2105/ajph.78.5.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mant A, King M, Saunders NA, Pond CD, Goode E, Hewitt H. Four-year follow-up of mortality and sleep-related respiratory disturbance in non-demented seniors. Sleep. 1995;18:433–8. doi: 10.1093/sleep/18.6.433. [DOI] [PubMed] [Google Scholar]
- 37.Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep. 2008;31:1079–85. [PMC free article] [PubMed] [Google Scholar]
- 38.Punjabi NM, Caffo BS, Goodwin JL, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 2009;6:e1000132. doi: 10.1371/journal.pmed.1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cassar A, Morgenthaler TI, Lennon RJ, et al. Treatment of obstructive sleep apnea is associated with decreased cardiac death after percutaneous coronary intervention. J Am Coll Cardiol. 2007;49:1625–31. doi: 10.1016/j.jacc.2007.06.028. [DOI] [PubMed] [Google Scholar]


