Table 1.
Proposed simplification of diagnostic classification of myelodysplastic syndromes
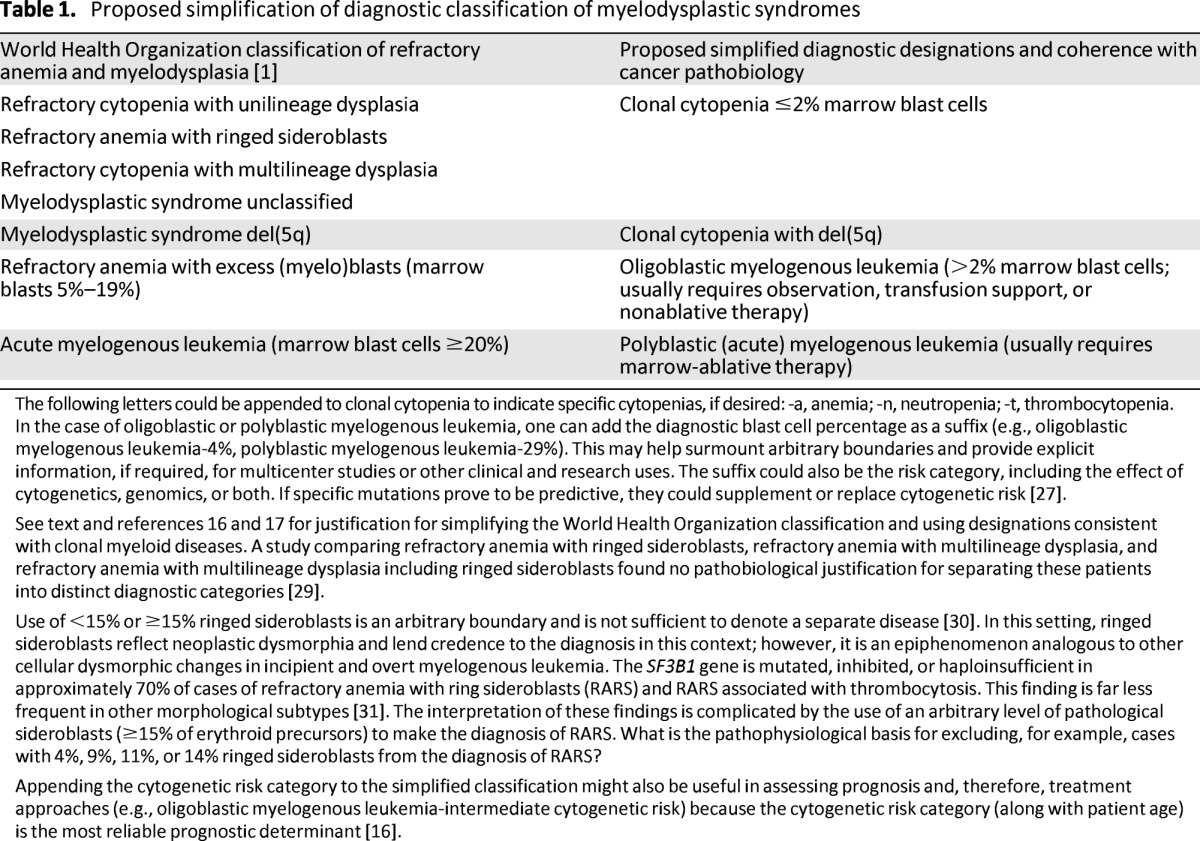
The following letters could be appended to clonal cytopenia to indicate specific cytopenias, if desired: -a, anemia; -n, neutropenia; -t, thrombocytopenia.
In the case of oligoblastic or polyblastic myelogenous leukemia, one can add the diagnostic blast cell percentage as a suffix (e.g., oligoblastic myelogenous leukemia-4%, polyblastic myelogenous leukemia-29%). This may help surmount arbitrary boundaries and provide explicit information, if required, for multicenter studies or other clinical and research uses. The suffix could also be the risk category, including the effect of cytogenetics, genomics, or both. If specific mutations prove to be predictive, they could supplement or replace cytogenetic risk [27].
See text and references 16 and 17 for justification for simplifying the World Health Organization classification and using designations consistent with clonal myeloid diseases. A study comparing refractory anemia with ringed sideroblasts, refractory anemia with multilineage dysplasia, and refractory anemia with multilineage dysplasia including ringed sideroblasts found no pathobiological justification for separating these patients into distinct diagnostic categories [29].
Use of <15% or ≥15% ringed sideroblasts is an arbitrary boundary and is not sufficient to denote a separate disease [30]. In this setting, ringed sideroblasts reflect neoplastic dysmorphia and lend credence to the diagnosis in this context; however, it is an epiphenomenon analogous to other cellular dysmorphic changes in incipient and overt myelogenous leukemia. The SF3B1 gene is mutated, inhibited, or haploinsufficient in approximately 70% of cases of refractory anemia with ring sideroblasts (RARS) and RARS associated with thrombocytosis. This finding is far less frequent in other morphological subtypes [31]. The interpretation of these findings is complicated by the use of an arbitrary level of pathological sideroblasts (≥15% of erythroid precursors) to make the diagnosis of RARS. What is the pathophysiological basis for excluding, for example, cases with 4%, 9%, 11%, or 14% ringed sideroblasts from the diagnosis of RARS?
Appending the cytogenetic risk category to the simplified classification might also be useful in assessing prognosis and, therefore, treatment approaches (e.g., oligoblastic myelogenous leukemia-intermediate cytogenetic risk) because the cytogenetic risk category (along with patient age) is the most reliable prognostic determinant [16].
