Abstract
Background
The Osteoporosis Health Belief Scale (OHBS) is a 42-item questionnaire designed to assess susceptibility, seriousness, calcium benefits, calcium barriers, exercise benefits, exercise barriers, and health motivation related to osteoporosis. We aimed to evaluate its psychometric properties to enable the provision of educational tips regarding osteoporosis.
Methods
All women who had visited the department of obstetrics and gynecology (OBGYN) and whose bone mineral density was measured from January 2010 to December 2011 were enrolled by interview using the OHBS. We also evaluated the women's general clinical characteristics.
Results
One hundred seventy-seven women were enrolled in the present study. In the present study, the barriers to calcium intake subscale had the lowest mean score (15.03±3.02), and the Benefit of Exercise subscale had the highest (23.02±3.03). The scores for participants in their 20s were significantly higher than scores for those in their 70s on the Benefits of Exercise subscale and Barriers to Exercise subscale (P=0.014 and P=0.022, respectively).
Conclusions
Education for health motivation to prevent osteoporosis is important for young women. Additional systematic education programs are needed for the general population.
Keywords: Bone mineral density, Osteoporosis, Questionnaires
INTRODUCTION
Osteoporosis is an important health issue worldwide, in part because of the current focus in healthcare circles on the aging process. Osteoporosis entails microstructural abnormalities and bone density deficiency that cause systemic bone structure disease and broken bone disease as defined by the World Health Organization (WHO).[1]
Osteoporosis is diagnosed using the International Society for Clinical Densitometry (ISCD) or WHO criteria.[1] Recently, the fracture-risk assessment tool (FRAX) using clinical risk factors and measures of femoral neck bone mineral density (BMD) is used to predict the fracture probability.[2] The exact diagnosis and prediction of osteoporosis and identification of osteoporosis risk factors are important; however, prevention is also important. Prevention of osteoporosis should be addressed from a young age.
The importance of eating habits for bone health is widely known in the general population. However, systematic evaluation and education for preventing osteoporosis are not available. With a focus on education for the prevention of osteoporosis, we aimed to evaluate the psychometric properties of an osteoporosis scale in women. The Osteoporosis Health Belief Scale (OHBS) was developed to measure health beliefs related to osteoporosis. It includes items addressing seriousness, susceptibility, health motivation, calcium benefits, calcium barriers, exercise benefits, and exercise barriers related to osteoporosis. A few reports have been published regarding the OHBS.[3]
We administered OHBS to members of the general population who presented at an obstetrics and gynecology clinic to collect data that would allow us to develop educational tools.
METHODS
The present study was conducted at a university hospital. All women who visited the department of obstetrics and gynecology (OBGYN) and whose BMD was measured from January 2010 to December 2011 were evaluated. The resulting sample included 242 patients. All patients gave verbal consent to complete the OHBS questionnaire. A trained interviewer interviewed the patients at the outpatient office. However, in outpatient office setting, there had been many limitation to interviewer such as very little time to interview each patient, and insincerity of many enrolled patient. Therefore, 65 patients were excluded from the present study because of missing data. Finally, the present retrospective study comprised 177 patients whose femoral neck BMD was checked and who completed the questionnaire.
Information regarding patients' background such as age, body weight, height, and BMD T-score, was obtained from the hospital information system. The weight and height recorded at the time of dual energy X-ray absorptiometry (DXA) evaluation were used. BMD was evaluated at the L1-4 lumbar spine and femoral neck using the same DXA machine (Lunar Prodigy Advance, GE Lunar, Medison, WI, USA).
The OHBS is designed to measure seven constructs: susceptibility, seriousness, calcium benefits, calcium barriers, exercise benefits, exercise barriers, and health motivation.[1] Each item in OHBS is scored from 1 (strongly disagree) to 5 (strongly agree). Six questions constitute one category, and the summary scores are calculated by summing up the scores of each category, which results in the possible score range from 6 to 30. The OHBS comprises 42 items: 1-6: susceptibility; 7-12: seriousness; 13-18: benefits of exercise; 19-24: benefits of calcium intake; 25-30: barriers to exercise; 31-36: barriers to calcium intake; and 37-42: health motivation. In present study, we used a Korean version of OHBS which had translated by our research team.
All results are expressed as the mean±standard deviation (SD) unless otherwise stated. Statistical significance was analyzed by one-way analysis of variance followed by Scheffe's test. A P value less than 0.05 was considered statistically significant. Results were analyzed using the SPSS version 18 software package (SPSS Inc., Chicago, IL, USA).
Informed consent was obtained when the research assistant interviewed patients.
RESULTS
One hundred seventy-seven women between the ages of 24 and 78 years (mean age: 52.23, SD: 9.97) were enrolled in the present study. The patient's mean weight and height were 56.46±8.37 kg and 156.90±5.37 cm. The mean body mass index (BMI) was 22.96±3.23 kg/m2 (range from 16.11 to 37.56), and the mean T-score at the femoral neck was -0.96±1.22 (range from -4.09 to -1.97). The possible range of scores for each OHBS subscale is 6 to 30. In the present study, the barriers to calcium intake subscale had the lowest mean score (15.03±3.02), and the Benefit of Exercise subscale had the highest (23.02±3.03). These results are shown in Tables 1-3.
Table 1.
Comparison of Osteoporosis Health Belief Scale scores obtained from normal, osteopenia, and osteoporosis group
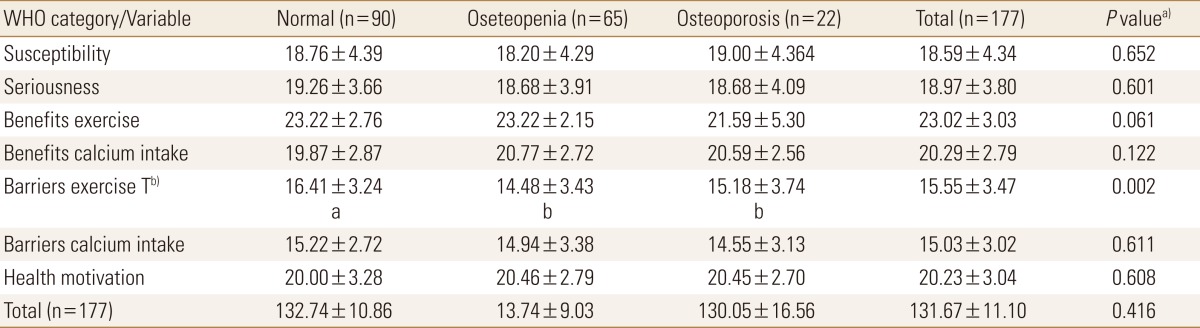
Data are given as mean±SD.
a)Statistical significances were tested by one way analysis of variances among groups. b)The same letters indicate non-significant difference between groups based on Scheffe's multiple comparison test.
Normal: -1.0<T-score, Osteopenia: -2.5<T-score≤-1.0, Osteoporosis: T-score≤-2.5.
Table 3.
Comparison of Osteoporosis Health Belief Scale scores obtained from different weight groups
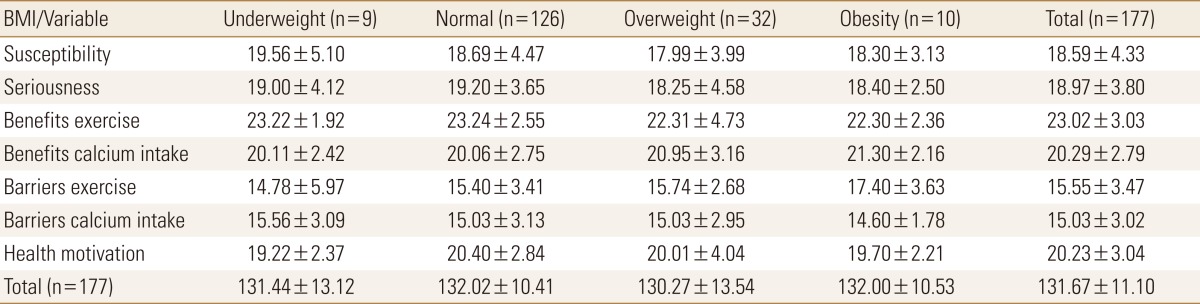
BMI, body mass index, kg/m2.
Underweight: BMI<18.5, Normal: 18.5≤BMI<25, Overweight: 25≤BMI<30, Obesity: 30≤BMI.
A comparison of OHBS scores according to WHO category is shown in Table 1. Significant differences were found between the normal and osteopenia groups and between the normal and osteoporosis groups on the barriers to exercise subscale (P=0.002).
Table 2 shows the OHBS scores according to age group. The scores for participants in their 20s were significantly different from scores for those in their 70s on the Benefits of Exercise subscale and Barriers to Exercise subscale (P=0.014, P=0.022, respectively).
Table 2.
Comparison of Osteoporosis Health Belief Scale scores obtained from different age groups
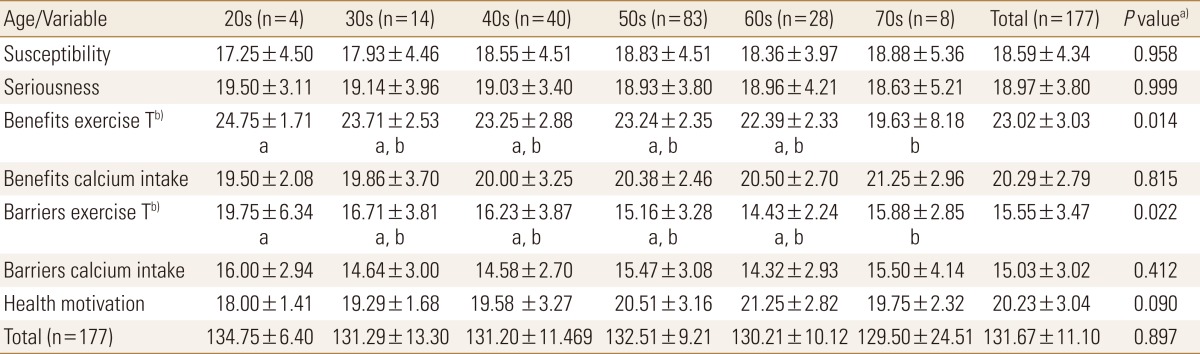
Data are given as mean±SD.
a)Statistical significances were tested by one way analysis of variances among groups. b)The same letters indicate non-significant difference between groups based on Scheffe's multiple comparison test.
Differences in BMI showed no relationship to the OHBS score (Table 3).
DISCUSSION
The OHBS evaluates an individual's recognition of susceptibility to osteoporosis and awareness of the benefits of prevention or preventive activity, such as calcium intake and exercise. Women with T-scores indicating BMD in the normal-range showed significantly greater awareness of the benefits of exercise compared with those in the osteopenia and osteoporosis groups. Women in the 20s age group had more information concerning the benefits of exercise, but they also reported greater barriers to exercise compared with women in the 70s age group.
We reported previously on the difference between the WHO diagnostic criteria and the 2008 ISCD criteria.[1] The WHO diagnostic criteria are less stringent than the ISCD criteria and may be over treated for the patients.[1] The Korean FRAX is a good model for estimating fracture probability. And the 25-hydroxy-vitamin D3 levels in postmenopausal women are also lower in Korean women.[4] A variety of factors related to the prevention of osteoporosis, including osteoporosis education, eating habits, general health habits, and exercise, should be evaluated in the general population.
The mean scores on the OHBS indicated that osteoporosis is a serious problem, and exercise is important to prevent osteoporosis.[5] No statistically significant relationship was found between exercise habits and knowledge about osteoporosis, but awareness of the benefits of exercise and awareness of personal susceptibility to osteoporosis were associated.[5]
Other surveys have also evaluated beliefs regarding the severity of osteoporosis;[5] however, the belief in personal susceptibility to osteoporosis was low in older adults.[6]
A program addressing knowledge about osteoporosis prevention is helpful in encouraging people to learn self-direction, participation in preventative activities, and information seeking related to the prevention of osteoporosis. However, knowledge itself does not change health beliefs. Responses to the OHBS differed between men and women.[7] Women were significantly more likely to recognize the benefits of calcium intake and to be aware of their susceptibility to osteoporosis, but they also reported barriers to exercising.[8] Individuals in the general population who underwent DXA had an increased awareness of their susceptibility to osteoporosis and of the benefits of calcium intake.[9]
The DXA result may provide the motivation and health beliefs necessary to support osteoporosis prevention.[9] We should consider developing an education program based on gender. Our data revealed that individuals in their 20s had good knowledge concerning the benefits of exercise but also reported greater barriers to exercise; young women may be unable to participate in effective exercise because of environmental factors. Young college women considered osteoporosis a moderately severe disease.[10] However, education that increases knowledge about osteoporosis risk factors may decrease the high-risk lifestyle associated with osteoporosis during the college years.[10] Health motivation is needed to encourage young women to exercise for osteoporosis prevention.
The present study has some limitations. It was a single-center study with a small sample size, and it considered only OHBS and BMD, along with general characteristics. We did not collect data regarding dietary calcium, exercise patterns, and general life styles such as social life and economic status. And we could not validate the Korean version of OHBS which had been translated by our research team.
We recommend studying the OHBS with other related osteoporosis factors, such as FRAX scores and food habits, to develop an educational program for preventing osteoporosis.
Acknowledgments
Authors greatly appreciate help from Jaewook Park, Changseok Lee, Haneul Kim, Hyuna Lee, Soonyoung Lee, Minjoo Kang, Younghwa Rho and Jaeyoung Jang in their survey collection and data organization. We also acknowledge Eun-Hee Kim's assistance in manuscript editing.
Osteoporosis Health Belief Scale Question
1. Yours chances of getting osteoporosis are high.
2. Because of your body build, you are more likely to develop osteoporosis.
3. It is extremely likely that you will get osteoporosis.
4. There is a good chance that you will get osteoporosis.
5. You are more likely than the average person to get osteoporosis.
6. Your family history makes it more likely that you get osteoporosis.
7. The thought of having osteoporosis scares you.
8. If you had osteoporosis you would be crippled
9. Your feelings about yourself would change if you got osteoporosis.
10. It would be very costly if you got osteoporosis.
11. When you think about osteoporosis you get depressed.
12. It would be very serious if you got osteoporosis.
13. Regular exercise prevents problems that would happen from osteoporosis.
14. You feel better when you exercise to prevent osteoporosis.
15. Regular exercise helps to build strong bones.
16. Exercising to prevent osteoporosis also improves the way your body looks.
17. Regular exercise cuts down the chances of broken bones.
18. You feel good about yourself when you exercise to prevent osteoporosis.
19. Taking in enough calcium prevents problems from osteoporosis.
20. You have lots to gain from taking in enough calcium to prevent osteoporosis.
21. Taking in enough calcium prevents painful osteoporosis.
22. You would not worry as much about osteoporosis if you took in enough calcium.
23. Taking in enough calcium cuts down on your chances of broken bones.
24. You feel good enough about yourself when you take in enough calcium to prevent osteoporosis.
25. You feel like you are not strong enough to exercise regularly.
26. You have no place where you can exercise.
27. Your spouse of family discourages you from exercising.
28. Exercising regularly would mean starting a new habit which is hard for you to do.
29. Exercising regularly makes you uncomfortable.
30. Exercising regularly upsets your every day routine.
31. Calcium-rich foods cost too much.
32. Calcium-rich foods do not agree with you.
33. You do not like calcium-rich foods.
34. Eating calcium-rich foods means changing your diet which is hard to do.
35. In order to eat more calcium-rich foods you have to give up other foods that you like.
36. Calcium-rich foods have too much cholesterol.
37. You eat a well-balanced diet.
38. You look for new information related to health.
39. Keeping healthy is very important for you.
40. You try to discover health problems early.
41. You have a regular health check-up even when you are not sick.
42. You follow recommendations to keep you healthy.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Chung SH, Lee HH, Kim TH, et al. Difference in the diagnosis of osteoporosis in elderly postmenopausal women according to WHO and the 2008 international society for clinical densitometry diagnostic criteria. J Korean Soc Menopause. 2009;15:87–92. [Google Scholar]
- 2.Kim TH, Lee HH, Chung SH, et al. Routine application of the Korean FRAX model in women: a single-center study. Korean J Bone Metab. 2012;19:29–34. [Google Scholar]
- 3.Kim KK, Horan ML, Gendler P, et al. Development and evaluation of the Osteoporosis Health Belief Scale. Res Nurs Health. 1991;14:155–163. doi: 10.1002/nur.4770140210. [DOI] [PubMed] [Google Scholar]
- 4.Chung SH, Kim TH, Lee HH. Relationship between vitamin D level and bone mineral density in postmenopausal women from Bucheon area. J Korean Soc Osteoporos. 2009;7:198–202. [Google Scholar]
- 5.Taggart HM, Connor SE. The relation of exercise habits to health beliefs and knowledge about osteoporosis. J Am Coll Health. 1995;44:127–130. doi: 10.1080/07448481.1995.9939106. [DOI] [PubMed] [Google Scholar]
- 6.Nayak S, Roberts MS, Chang CC, et al. Health Beliefs about Osteoporosis and Osteoporosis Screening in Older Women and Men. Health Educ J. 2010;69:267–276. doi: 10.1177/0017896910364570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sedlak CA, Doheny MO, Jones SL. Osteoporosis education programs: changing knowledge and behaviors. Public Health Nurs. 2000;17:398–402. doi: 10.1046/j.1525-1446.2000.00398.x. [DOI] [PubMed] [Google Scholar]
- 8.McLeod KM, Johnson CS. A systematic review of osteoporosis health beliefs in adult men and women. J Osteoporos. 2011;2011:197454. doi: 10.4061/2011/197454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sedlak CA, Doheny MO, Estok PJ, et al. DXA, health beliefs, and osteoporosis prevention behaviors. J Aging Health. 2007;19:742–756. doi: 10.1177/0898264307304303. [DOI] [PubMed] [Google Scholar]
- 10.Edmonds E, Turner LW, Usdan SL. Osteoporosis knowledge, beliefs, and calcium intake of college students: utilization of the health belief model. Open J Prev Med. 2012;2:27–34. [Google Scholar]