Abstract
OBJECTIVE
We aimed to determine the associations of waist circumference (WC) and BMI with all-cause mortality among patients with diabetes.
RESEARCH DESIGN AND METHODS
The sample included 847 white and 553 African American patients (18–69 years of age) with diabetes. Height, weight, and WC were measured, and the BMI (kg/m2) was calculated. Cox regression was used to analyze the associations of BMI and WC with mortality, adjusting for age, sex, race, examination year, smoking status, alcohol consumption, and physical activity. Hazard ratios (HRs) are expressed per standard deviation of each independent variable.
RESULTS
A total of 86 deaths occurred during 6.7 years of follow-up. After adjustment for covariates, WC (HR 1.40 [95% CI 1.14–1.72]) and BMI (1.29 [1.04–1.61]) demonstrated significant relationships with mortality.
CONCLUSIONS
The results indicate that maintaining a healthy WC and BMI are both important for individuals living with diabetes.
The number of individuals in the U.S. living with diabetes continues to rise (1), and these patients have an increased risk of cardiovascular complications and premature mortality (2). Obesity is associated with the development of type 2 diabetes (3,4); however, the relationship between the most common measure of obesity, the BMI, and mortality among patients with diabetes is less clear. To date, studies have reported positive associations (5), negative associations (6–9), U-shaped associations (10,11), or no association (12) between BMI and mortality among patients with diabetes. However, the BMI has some limitations as an indicator of obesity (13), and no study has been reported on the relationship with other indicators of adiposity. Thus, the purpose of this prospective cohort study was to determine the associations of waist circumference (WC) and BMI with all-cause mortality.
RESEARCH DESIGN AND METHODS
Sample
The sample included 847 white and 553 African American diabetic adults (18–69 years of age) from the Pennington Center Longitudinal Study (PCLS), which is an investigation of the effects of obesity and lifestyle factors on the development of chronic diseases and premature mortality. The sample is composed of volunteers who participated in studies conducted at the Pennington Biomedical Research Center (PBRC) in Baton Rouge, Louisiana, between 1994 and 2009 (14,15). Each participant was seen once at baseline, and mortality outcomes were assessed by linkage with the National Death Index. Written informed consent was provided, and all procedures were approved by the PBRC Institutional Review Board.
Baseline exposures
Diabetes status was determined using a combination of self-reported physician diagnosis, fasting blood glucose (≥126 mg/dL), and diabetic medications. Height and weight were measured after outer clothing, heavy pocket items, and shoes were removed, and BMI was calculated (weight [kg]/height [m2]). WC was measured at the midpoint between the inferior border of the ribcage and the superior aspect of the iliac crest.
Covariates
Age was computed from birth and observation dates, and year of examination was included as a covariate to account for potential temporal trends in baseline measurements. Smoking status, alcohol consumption, and leisure-time physical activity were self-reported by questionnaire.
Ascertainment of mortality status
The vital status of all participants was determined by linkage to the National Death Index (16). The primary end point for this analysis was deaths from all causes that occurred between 6 months after the baseline assessment and 31 December 2009. The average length of follow-up was 6.7 years (SD 3.6; maximum 15.8).
Statistical analysis
Cox proportional hazards regression was used to assess the associations of WC and BMI with all-cause mortality, adjusting for age, sex, race, baseline examination year, smoking status, alcohol consumption, and physical activity. Model 1 included age, sex and baseline examination year as covariates, and model 2 additionally included race (white, African American) smoking status (never, former, current, unknown), alcohol consumption (no, yes, unknown), and leisure-time physical activity (<4 h/week, ≥4 h/week, unknown). Hazard ratios (HRs) are expressed per SD of each independent variable (WC = 15 cm; BMI = 7 kg/m2). The presence of interactions was tested by including race, sex, WC, and BMI interaction terms in the models. To compare dose-response associations, HRs were calculated across tertiles of WC and BMI.
RESULTS
A total of 86 deaths (33 from cardiovascular disease, 23 from cancer, and 30 from other causes) occurred during 9,316 person-years of follow-up. At baseline, decedents were significantly older (57.0 [SD 7.5] vs. 53.3 [9.5] years), had a higher mean WC (115.4 [16.0] vs. 110.2 [15.1] cm) than survivors, and a lower percentage were women (48.8 vs. 66.7%; Supplementary Table). Mean BMI did not differ between decedents and survivors (36.3 [7.1] vs. 35.4 [6.6] kg/m2) nor did the percentage of African Americans (39.5 vs. 39.5%).
In models adjusted for age, sex, and examination year, WC (HR 1.41 [95% CI 1.15–1.73]) and BMI (1.32 [1.07–1.64]) were significantly associated with mortality. In multivariable-adjusted models, WC (1.40 [1.14–1.72]) and BMI (1.29 [1.04–1.61]) remained significant predictors. Higher death rates were observed in men (1.78 [1.12–2.81]) and African Americans (1.69 [1.08–2.66]) after adjustment for WC. Higher death rates were similarly observed after adjustment for BMI. However, no significant race or sex interactions were observed.
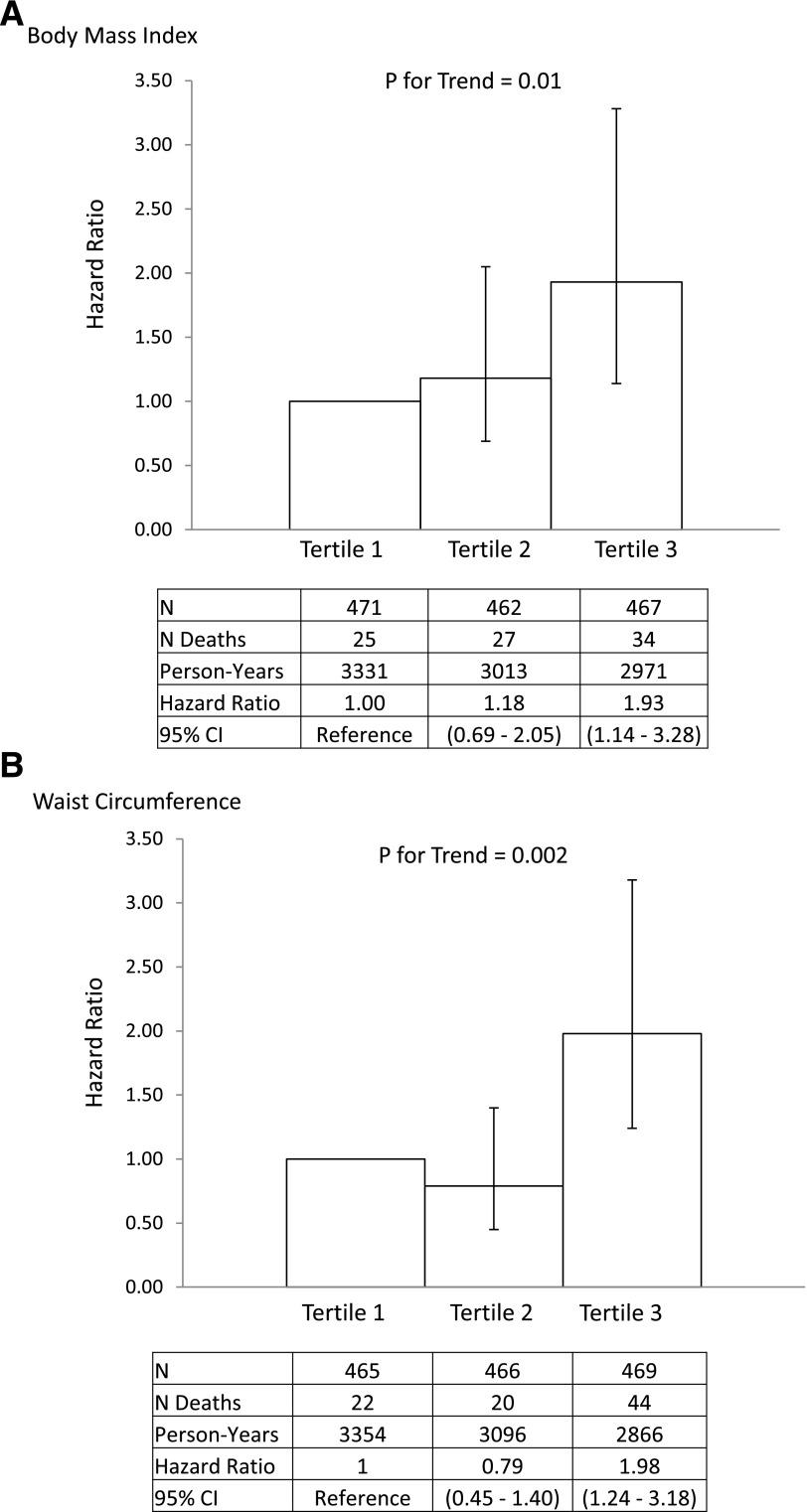
The results of the categorical analyses are presented in Fig. 1. There were significant linear trends for mortality across tertiles of both WC and BMI. In both cases, participants in tertile 3 had a significantly elevated risk of mortality compared with tertile 1.
Figure 1.
HRs for all-cause mortality across tertiles of BMI (A) and WC (B) are shown among patients with diabetes in the Pennington Center Longitudinal Study. Error bars represent the 95% CI. Cutoffs for the tertiles were 32 and 38 kg/m2 for BMI and 104 and 116 cm for WC. HRs are adjusted for age, year of examination, sex, race, smoking, alcohol consumption, and physical activity.
CONCLUSIONS
The results of this study indicate a significant, positive association between BMI and mortality rates in this biracial sample of patients with diabetes. This is in contrast to some previous studies that have documented inverse (6–9) or U-shaped associations (10,11). However, our results are similar to those from Finnish patients with diabetes, where the HRs across successive tertiles of BMI were 1.00 (reference), 0.94 (95% CI 0.80–1.10), and 1.20 (1.02–1.40) (5). The reasons for different associations across studies are not clear; however, the samples differed at baseline by mean level of BMI, health status, ethnicity, and duration of diabetes.
To our knowledge, the role of obesity in predicting mortality among patients with diabetes has not been explored using measures other than BMI. Our results indicate that decedents had a higher WC but not a higher BMI than survivors at baseline. Further, the association between WC and mortality was similar to that with BMI.
This study has several strengths and weaknesses. The reliance on direct assessments of WC and BMI and the linkage to the National Death Index are marked strengths. However, the relatively small, nonrepresentative sample and the lack of information on duration of diabetes and comorbidities are limitations. The sample size was not sufficient to allow for cause-specific analyses.
In conclusion, the results of this study indicate that maintaining a healthy WC and BMI are important for individuals living with diabetes. The association with WC was similar to that of BMI.
Acknowledgments
P.T.K. is supported, in part, by the Louisiana Public Facilities Authority Endowed Chair in Nutrition. C.B. is supported, in part, by the John W. Barton Sr. Chair in Genetics and Nutrition.
No potential conflicts of interest relevant to this article were reported.
P.T.K. conceptualized the study and wrote the manuscript. G.H., W.T.C., and C.B. contributed to the discussion and reviewed and edited the manuscript. E.M. researched and analyzed data. P.T.K. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank the contributions of the many clinical scientists and staff of the Pennington Biomedical Research Center who have contributed data to the Pennington Center Longitudinal Study. The Pennington Center Longitudinal Study is registered at ClinicalTrials.gov (Identifier NCT00959270).
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc13-0219/-/DC1.
References
- 1.Centers for Disease Control and Prevention (CDC) Increasing prevalence of diagnosed diabetes—United States and Puerto Rico, 1995-2010. MMWR Morb Mortal Wkly Rep 2012;61:918–921 [PubMed] [Google Scholar]
- 2.American Diabetes Association Standards of medical care in diabetes—2013. Diabetes Care 2013;36(Suppl. 1):S11–S66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kodama S, Horikawa C, Fujihara K, et al. Comparisons of the strength of associations with future type 2 diabetes risk among anthropometric obesity indicators, including waist-to-height ratio: a meta-analysis. Am J Epidemiol 2012;176:959–969 [DOI] [PubMed] [Google Scholar]
- 4.Vazquez G, Duval S, Jacobs DR, Jr, Silventoinen K. Comparison of body mass index, waist circumference, and waist/hip ratio in predicting incident diabetes: a meta-analysis. Epidemiol Rev 2007;29:115–128 [DOI] [PubMed] [Google Scholar]
- 5.Hu G, Jousilahti P, Barengo NC, Qiao Q, Lakka TA, Tuomilehto J. Physical activity, cardiovascular risk factors, and mortality among Finnish adults with diabetes. Diabetes Care 2005;28:799–805 [DOI] [PubMed] [Google Scholar]
- 6.Carnethon MR, De Chavez PJ, Biggs ML, et al. Association of weight status with mortality in adults with incident diabetes. JAMA 2012;308:581–590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Doehner W, Erdmann E, Cairns R, et al. Inverse relation of body weight and weight change with mortality and morbidity in patients with type 2 diabetes and cardiovascular co-morbidity: an analysis of the PROactive study population. Int J Cardiol 2012;162:20–26 [DOI] [PubMed] [Google Scholar]
- 8.Kokkinos P, Myers J, Faselis C, Doumas M, Kheirbek R, Nylen E. BMI-mortality paradox and fitness in African American and Caucasian men with type 2 diabetes. Diabetes Care 2012;35:1021–1027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McEwen LN, Kim C, Karter AJ, et al. Risk factors for mortality among patients with diabetes: the Translating Research Into Action for Diabetes (TRIAD) Study. Diabetes Care 2007;30:1736–1741 [DOI] [PubMed] [Google Scholar]
- 10.Khalangot M, Tronko M, Kravchenko V, Kulchinska J, Hu G. Body mass index and the risk of total and cardiovascular mortality among patients with type 2 diabetes: a large prospective study in Ukraine. Heart 2009;95:454–460 [DOI] [PubMed] [Google Scholar]
- 11.So WY, Yang X, Ma RC, et al. Risk factors in V-shaped risk associations with all-cause mortality in type 2 diabetes-The Hong Kong Diabetes Registry. Diabetes Metab Res Rev 2008;24:238–246 [DOI] [PubMed] [Google Scholar]
- 12.McEwen LN, Karter AJ, Waitzfelder BE, et al. Predictors of mortality over 8 years in type 2 diabetic patients: Translating Research Into Action for Diabetes (TRIAD). Diabetes Care 2012;35:1301–1309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heymsfield SB, Cefalu WT. Does body mass index adequately convey a patient’s mortality risk? JAMA 2013;309:87–88 [DOI] [PubMed] [Google Scholar]
- 14.Katzmarzyk PT, Bray GA, Greenway FL, et al. Racial differences in abdominal depot-specific adiposity in white and African American adults. Am J Clin Nutr 2010;91:7–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Katzmarzyk PT, Mire E, Bray GA, Greenway FL, Heymsfield SB, Bouchard C. Anthropometric markers of obesity and all-cause mortality in white and African American adults: The Pennington Center Longitudinal Study. Obesity (Silver Spring) (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.MacMahon B. The National Death Index. Am J Public Health 1983;73:1247–1248 [DOI] [PMC free article] [PubMed] [Google Scholar]