Abstract
Myxomas of the head and neck are rare tumors of uncertain histogenesis. Odontogenic myxomas in maxilla are less common but behave more aggressively, as it spreads through maxillary antrum. It therefore reaches considerable size before being detected. The current case arouses particular interest due to the rapid growth and infiltrating nature of the lesion in a 25-year-old female patient, who denied any leading symptoms, even with the lesion involving extensively. Radiographic and microscopic similarities to a number of entities make diagnostic interpretation of odontogenic myxoma challenging. Therefore sound knowledge of clinical, radiographic and histopathologic features is important to establish an appropriate treatment aimed at a good clinical course and patient cure.
Keywords: Aggressive, infiltration, maxillary antrum, myxoma, odontogenic
INTRODUCTION
Odontogenic myxoma (OM) is a non-encapsulated benign tumor of the jaws that occurs very rarely.[1] According to the literature, OMs represent between 1% and 17.7% of all odontogenic tumors.[2]
Since its original description by Thoma and Goldman in 1947,[3] the nature of OM has been a matter of controversy. Several studies have been performed in order to define its precise nature, but at present there is no universally accepted theory about its probable histogenesis. Based on the presence of occasional small islands of odontogenic epithelium, its occurrence almost exclusively in the jawbones and the histomorphological similarity to the mesenchymal component of the developing tooth; an odontogenic origin has been proposed and particularly from the dental follicle or the periodontal ligament.[2]
This tumor may present at any age, but is most frequently discovered in the 2nd to 4th decades and occur more frequently in the mandible than in the maxilla.[4] There is no apparent sex predilection. Although most of these tumors grow at a relatively slow pace, some may exhibit rapid growth.[5] Cortical expansion and perforation are common findings; however, maxillary lesions tend to obliterate the maxillary sinuses as an early feature. Radiographically, OMs appear as unilocular or multilocular radiolucency, sometimes showing a fine soap bubble or honey comb appearance occasionally with fine trabeculations.[6] Root resorption is rarely seen although displacement of teeth is relatively common. Further, it frequently displays aggressive infiltration of the adjacent tissues as well as tendency to re-occur after surgical removal.[7] Variations in radiographic presentation make a radiological differential interpretation of OM challenging because the radiographic features overlap with those of other benign and malignant neoplasms.[8] A biopsy is therefore necessary to ascertain an accurate diagnosis.
In view of its rarity, the present case of odontogenic myxoma of the maxillary posterior segment in a 25-year-old female infiltrating the maxillary antrum and adjacent tissues is herewith reported.
CASE REPORT
A 25-year-old female was referred to our service for the evaluation of a painless swelling on the right mid-facial region with rapid evolution since one month. Extra-oral examination revealed a diffuse swelling with respect to right mid-facial region that was firm and non tender on palpation causing significant facial asymmetry. Intra-oral examination revealed a firm, non tender swelling expanding the buccal cortex of right maxilla extending from the right first molar to third molar obliterating the buccal vestibule [Figure 1a and b]. No palpable cervical lymphadenopathy was present.
Figure 1.
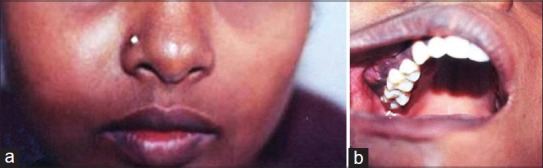
(a) Diffuse extra-oral swelling on the right mid-facial region, (b) Intra-oral swelling expanding the buccal cortex of right maxillary posterior segment obliterating the buccal vestibule
Maxillary occlusal view revealed radiolucent lesion with respect to right maxillary posterior region with interlaced bony trabeculae resulting in a multilocular spider web appearance; on basis of which a working diagnosis of odontogenic myxoma was made. Further to delineate the extent of the lesion, a computed tomography (CT) scan was carried out. CT scan (axial and coronal views) demonstrated a hypodense ill-defined expansile lesion of the right maxilla with expansion and thinning of the overlying buccal cortex and involvement of the right maxillary antrum. Destruction of the bony margins of medial and lateral walls of the right maxillary antrum, with extension into the nasal cavity resulting in the partial occlusion of the nasal passage was evident. CT scan also revealed destruction of the bony margin of posterior wall of the right maxillary antrum and lateral pterygoid plate. Right infra-orbital margin was seen pushed upwards with erosion of the medial wall of the orbit [Figure 2a and b]. Irregular calcific strands were evident within the lesion [Figure 2c].
Figure 2.
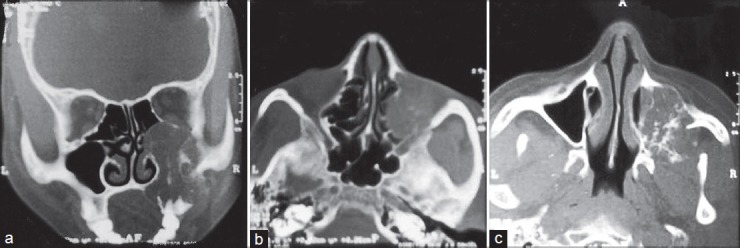
(a) Coronal CT view depicting an expansile lesion of the right maxilla with expansion and thinning of the overlying buccal cortex and involvement of the right maxillary antrum. Erosion of the medial wall of the orbit was also seen (b) Axial CT view showing extension of the lesion into the nasal cavity (c) Axial CT view depicting irregular calcific strands within the lesion
Subsequently, an incisional biopsy was performed and the specimen was submitted for the histopathological examination. The specimen appeared macroscopically as soft gelatinous yellowish white mass with cut surface exhibiting characteristic slimy appearance. Light microscopic examination of the sections stained with H-E revealed spindle and stellate shaped fibroblastic cells set in a myxoid background with delicate haphazardly arranged collagen fibers interspersed with a variable number of tiny capillaries [Figure 3a]. Few areas show isolated foci of residual bone [Figure 3b]. Odontogenic islands, binucleated cells, cellular pleomorphism and mitotic figures were not appreciated. The histopathological features were consistent with the diagnosis of odontogenic myxoma. The tumor was surgically excised with partial enbloc resection of the maxilla. The postoperative course was uneventful. The patient has since been kept on regular follow-up, and treatment planning for dental rehabilitation is currently underway.
Figure 3.
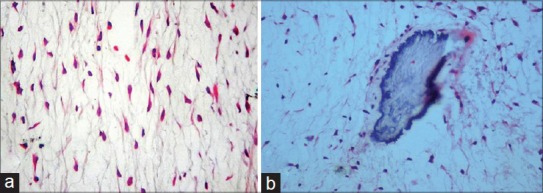
(a) Photomicrograph of the histopathologic section reveals stellate shaped fibroblastic cells set in a myxoid background with delicate haphazardly arranged collagen fibers (H and E, ×200) (b) Photomicrograph of the histopathologic section reveals foci of residual bone within myxoid background (H and E, ×200)
DISCUSSION
Odontogenic myxoma (OM), as its name implies, is peculiar to the jaws. Enzinger and Weiss suggest that myxoid tumors elsewhere in the body arise from the modified fibroblasts that produce excessive amounts of glycosaminoglycans, which in turn may inhibit polymerization of collagen. Myxomas of the jaws, by contrast, show a close structural resemblance to dental mesenchyme, occasionally contain epithelial rests, affect the tooth-bearing areas of the jaws, and a tooth is frequently absent.[9]
The tumor occurs across the age group that varies from 22.7 to 36.9 years. It is rare in patients younger than 10 years or older than 50 years of age.[10] The present case in a 25-year old female is in confirmatory with that reported in the literature. OM is commonly described as a slow growing tumor and generally symptomless. Rapidly growing odontogenic myxomas are rare, but have been reported in the literature. Rapid growth of OM may be attributed to the accumulation of mucoid ground substance, as mitoses are rarely seen.[11] However, as it advances in size, OM may present with disturbing symptoms. Bony perforation, with subsequent invasion into the soft tissues, reported to be common in large OMs,[1] was also observed in the present case.
OMs can be extensive, involving half of the maxilla or mandible including the ramus and the condyle.[4,12] Though OMs of the maxilla are less frequent but behaves more aggressively than that of the mandible.[10] However, tumors of the maxilla tend to enlarge and often fill the maxillary antrum before presenting as a facial swelling[13] as noticed in the present case. Further, the maxillary sinus filled with tumor mass can lead to exophthalmos,[12] the finding that was not appreciated in the present case; although right infra-orbital margin was seen pushed upwards with erosion of the medial wall of the orbit as evident on the CT scan. Lesions infiltrating the nasal cavity are rare;[14] but in the present case, intrusion of the lesion into the nasal cavity resulted in the partial occlusion of the nasal passage. Even with the lesion involving this extensively, the patient denied any such leading symptoms.
Radiologically, OM may appear as an unilocular or multilocular radiolucency with either honeycomb or soap-bubble pattern with cortical expansion and tooth displacement.[1] From the differential diagnostic point of view pathologies such as ameloblastoma, odontogenic keratocyst, central giant cell granuloma, intra-osseous hemangioma, aneurysmal bone cyst, metastatic tumor and, in cases of unilocular lesions, simple cysts should be included.[8,15]
It has been proposed that OM should as well be considered in the differential diagnosis of mixed radiolucent-radiopaque lesions. Such appearance is ascribed to the presence of calcifications, representing foci of residual bone rather than new bone formation.[4,16] A biopsy is, therefore, necessary to ascertain an accurate diagnosis.
Root resorption is rare, but displacement of teeth is a relatively common finding in OM.[12] But none of the regional teeth were displaced. The lack of tooth extrusion in the present case is probably the result of growth encroaching upon the maxillary sinus and infiltrating the adjacent structures.
OM is strikingly similar microscopically to myxoid enlarged or ‘hyperplastic’ dental follicle and the dental papilla of a developing tooth. In maxillary cases, confusion with nasal polyps is a risk. The microscopic differential diagnosis should also include myxoid nerve sheath tumors, chondromyxoid fibroma[6] together with myxomatous degeneration as observed in fast-growing neoplasms, particularly fibrosarcomas, chondrosarcomas and liposarcomas.[17] Evaluation of the clinical and radiographic features, however, will prevent over-diagnosis of these lesions as myxomas.
The tendency of OM to permeate into marrow spaces makes effective enucleation and curettage difficult. Small lesions have been successfully treated in this way but larger lesions may require complete excision with free margins. Recurrence rates from various studies average about 25%.[6] Despite the fact that odontogenic myxoma shows aggressive local growth, it is believed that it never undergoes malignant transformation or gives rise to metastasis.[16]
In the delineation of differential entities, the clinical facts and radiologic findings are of utmost importance in the diagnostic evaluation of the lesion and must be considered along with the histologic findings; so that appropriate treatment can be instituted to the specific pathology.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Simon EN, Merkx MA, Vuhahula E, Ngassapa D, Stoelinga PJ. Odontogenic myxoma: a clinicopathological study of 33 cases. Int J Oral Maxillofac Surg. 2004;33:333–7. doi: 10.1016/j.ijom.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Martinez-Mata G, Mosqueda-Taylor A, Carlos-Bregni R, deAlmeida OP, Contreras-Vidaurre E, Vargas PA, et al. Odontogenic myxoma: Clinico-pathological, immunohistochemical and ultrastructural findings of a multicentric series. Oral Oncol. 2008;44:601–7. doi: 10.1016/j.oraloncology.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 3.Thoma KH, Goldman HM. Central myxoma of the jaw. Oral Surg Oral Med Oral Pathol. 1947;33:B532–40. doi: 10.1016/0096-6347(47)90315-3. [DOI] [PubMed] [Google Scholar]
- 4.Kaffe I, Naor H, Buchner A. Clinical and radiological features of odontogenic myxoma of the jaws. Dentomaxillofac Radiol. 1997;26:299–303. doi: 10.1038/sj.dmfr.4600261. [DOI] [PubMed] [Google Scholar]
- 5.Gnepp DR. 2nd ed. Philadelphia: WB Saunders; 2009. Diagnostic Surgical Pathology of the Head and Neck; pp. 829–31. [Google Scholar]
- 6.Barnes L, Eveson JW, Reichart P, Sidransky D. Pathology and Genetics of Head and Neck Tumors. Lyon: IARC Press; 2005. World Health Organization Classification of Tumors; pp. 316–7. [Google Scholar]
- 7.Altug HA, Gulses A, Sencimen M. Clinico-radiographic examination of odontogenic myxoma with displacement of unerupted upper third molar: review of the literature. Int J Morphol. 2011;29:930–3. [Google Scholar]
- 8.Noffke CE, Raubenheimer EJ, Chabikuli NJ, Bouckaert MM. Odontogenic myxoma: review of the literature and report of 30 cases from South Africa. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:101–9. doi: 10.1016/j.tripleo.2007.01.026. [DOI] [PubMed] [Google Scholar]
- 9.Cawson RA, Binnie WH, Speight P, Barrett AW, Wright JM. 5th ed. New York: Churchill Livingstone; 1998. Lucas's Pathology of Tumors of the Oral Tissues; pp. 315–7. [Google Scholar]
- 10.Sivakumar G, Kavitha B, Saraswathi TR, Sivapathasundharam B. Odontogenic myxoma of maxilla. Indian J Dent Res. 2008;19:62–5. doi: 10.4103/0970-9290.38934. [DOI] [PubMed] [Google Scholar]
- 11.Kramer IR, Pindborg JJ, Shear M. 2nd ed. Vol. 31. Berlin: Springer-Verlag; 1991. Histological Typing of Odontogenic Tumours; p. 23. [Google Scholar]
- 12.Chrcanovic BR, do-Amaral MB, de-Andrade Marigo H, Freire-Maia B. An expanded odontogenic myxoma in maxilla. Stomatologija. 2010;12:122–8. [PubMed] [Google Scholar]
- 13.Wachter BG, Steinberg MJ, Darrow DH, McGinn JD, Park AH. Odontogenic myxoma of the maxilla: A report of two pediatric cases. Int J Pediatr otorhinolaryngol. 2003;67:389–93. doi: 10.1016/s0165-5876(02)00349-x. [DOI] [PubMed] [Google Scholar]
- 14.MacDonald-Jankowsky DS, Yeung R, Lee KM, Li TK. Odontogenic myxoma in the Hong Kong Chinese: clinico radiological presentation and systematic review. Dentomaxillofac Radiol. 2002;31:71–83. doi: 10.1038/sj.dmfr.4600678. [DOI] [PubMed] [Google Scholar]
- 15.Peltola J, Magnusson B, Happoren RP, Boman H. Odontogenic myxoma-a radiological study of 21 tumours. Br J Oral Maxillofac Surg. 1994;32:298–302. doi: 10.1016/0266-4356(94)90050-7. [DOI] [PubMed] [Google Scholar]
- 16.Barros RE, Dominguez FV, Cabrini RL. Myxoma of the jaws. Oral Surg Oral Med Oral Pathol. 1969;27:225–36. doi: 10.1016/0030-4220(69)90177-7. [DOI] [PubMed] [Google Scholar]
- 17.Reichart PA, Philipsen HP. London: Quintessence Publishing Co Ltd; 2004. Odontogenic Tumors and Allied Lesions; pp. 189–97. [Google Scholar]


