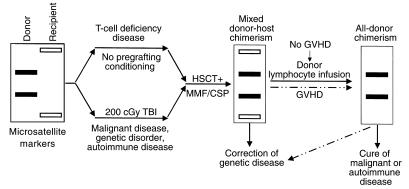
Figure 1.
Schematic illustration of nonmyeloablative HSCT-induced mixed donor-host chimerism. Successful transplantation generally requires some level of host immunosuppression, except in cases of T-cell deficiency. This has often involved harsh TBI, but there is great interest in reducing the dosage to low, easily tolerated levels, such as the 200 cGy shown here, or even replacing this step entirely with other forms of conditioning. This process leads first to a state of mixed chimerism, in which both donor and recipient cells are detectable in the subject’s lymphoid and myeloid compartments and thymus. To correct recessive genetic diseases, this state of mixed chimerism may suffice, whereas other conditions, such as malignancy and autoimmune disease, may require the complete replacement of host cells with donor cells. Such a state of all-donor chimerism can be initiated either in a spontaneous episode of graft-versus-host disease or through an infusion of donor lymphocytes.