Abstract
Low health literacy is common among Medicare recipients and affects their understanding of complex medication regimens. Interventions are needed to improve medication use among older adults, while addressing low health literacy. Community-dwelling older adults in this study were enrolled in an inner-city adult day center. They completed a baseline measure of health literacy, medication self-efficacy, and medication adherence. They were provided with a personalized, illustrated daily medication schedule (PictureRx™). Six weeks later, their medication self-efficacy and adherence were assessed. Among the 20 participants in this pilot project, 70% had high likelihood of limited health literacy and took an average of 13.2 prescription medications. Both self-efficacy and medication adherence increased significantly after provision of the PictureRx cards (p<0.001 and p<0.05, respectively). Al participants rated the PictureRx cards as very helpful in terms of helping them remember the medication’s purpose and dosing. Illustrated daily medication schedules improve medication self-efficacy and adherence among at-risk, community-dwelling older adults.
Background
Health literary is the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions (Institute of Medicine [IOM], 2004). Low health literacy adversely affects health and health care utilization, and it contributes to health disparities (IOM, 2004). Limited health literacy is associated with a substantial increase in mortality among community-dwelling elders (Sudore et al., 2006), and is a factor in predicting all-cause mortality and cardiovascular death in older adults (Baker et al., 2007).
Low health literacy is prevalent among Medicare enrollees (Gazmararian et. al, 1999) who experience a large burden of chronic illness (Gazmararian, J., Williams, M., Peel, J., & Baker, D., 2003;Hoffman, Rice & Sung, 1996). Forty-two percent of Medicare recipients read at less than a 6th grade level (National Network of Libraries of Medicine [NNLM] 2008), which is a determinant in understanding health instruction such as dosing schedules and can lead to medication errors (Davis et. al., 2006; Davis, Michielutte, Askov, Williams & Weiss, 1998). Older adults take two to three times the amount of prescribed medications as compared to the general public (Kutner, Greenburg, & Baer, 2005). In one large study, 54.3% of Medicare enrollees with limited health literacy skills were unable to understand a relatively simple medication instruction such as, “take on an empty stomach,” and 47.5% of the sample erroneously described medication dosing (Gazmararian et. al, 1999).
Approaches to improve medication understanding and use among the elderly are needed. Such efforts should address the pervasive issue of low health literacy in this population. Here we describe a quality improvement pilot to provide at-risk, community-dwelling elders with illustrated medication instructions. We evaluated the effect of this intervention on their confidence in managing their medications, as well as their self-reported adherence.
Methods
Overview
The quality improvement project was conducted through an adult day center, an evidenced based model of care located in an inner-city health facility sponsored by Catholic Charities Archdiocese in New Orleans. The project followed The Evidence-Based Practice Improvement Model: problem description, formulation of the clinical question, review and appraisal of the literature for evidence, and development of the aim/goal for change (Levin et al., 2009).
Medication errors resulting from misunderstanding instructions were identified as a problem among the facility’s population. In medical appointments at the facility, patients expressed difficulty understanding which medications to take and at what time to take each one (S. S., personal communication, March 4, 2010).
A needs assessment was conducted to identify the scope of the problem. After a literature review, it was decided to provide the adult day care center’s participants with PictureRx™ illustrated medication instructions. The goal was to facilitate understanding of medication instructions and improve medication safety.
The conceptual framework is based on the Institute of Medicine Health Literacy Framework (2004) which places health literacy as the supporting entity for understanding and expressing health needs. Health contexts, culture and society, health systems, and education systems are individualized components that can determine health outcomes and service utilization costs; intervention strategies at these points can improve health outcomes.
Prior to project initiation, a risk analysis was conducted using the SWOT method to identify strengths, weaknesses, opportunities, and threats (Lewis, 2005). Project strengths included the plan to address an identified need by providing medication health education, as well as support from organizational management. A potential weakness or threat was interruption of nurse case managers’ and social workers’ scheduled activities, as the lead author planned to work primarily with these health professionals prior to and during project implementation.
The change process in a system usually encounters some type of resistance; therefore it is important to identify strategies to overcome the anticipated barriers to change (Lightner, 2011). Three staff development sessions using the American Medical Association Health Literacy Toolkit (AMA, 2007) were conducted to instruct staff in evidenced-based communication strategies; use of plain language and teach-back (Egbert & Nanna, 2009; Oates & Paasche-Orlow, 2009; AMA, 2007; Marcus, 2006). Additionally, a focus group was conducted with the nurse case managers and social workers to actively listen to any concerns or issues. Potential benefits of the project were clearly articulated – improved patient safety through a clearer understanding of medication instructions.
The project was approved by the facility executive director and medical director. Project implementation began in June 2010 and ended in October 2010.
Screening and enrollment
Registered nurse case managers and social workers identified potential participants from those who regularly attended the health center. Exclusion criteria included non-English speaking and documented diagnosis of severe dementia. Severe dementia was defined as severe impairment or loss of intellectual capacity per the adult day care center’s criteria (S. S., personal communication, March 4, 2010). Participation was voluntary.
The project was introduced to potential participants through a face-to-face meeting at the day center. For elders who expressed interest, a letter of project introduction and intent to participate was sent home to family members or caregivers, asking them to agree or decline participation. If the family member and or caregiver agreed to the project, an additional individual meeting was held with the potential participant to review project methodology. Twenty elders provided written consent. One participant’s family member was involved in the project from initiation to completion.
Baseline data were collected, including age, gender, race, level of education, cognitive function, medical co-morbidities, number of prescribed medications, and health literacy. Level of education was assessed as completion of grade school (grades 1–5), junior high school (grades 6–8), high school (grades 9–12), some college, or college graduate. Measurements of cognitive function, using the Mini Mental Status Exam, were extracted through chart reviews.
Health literacy was assessed using the Newest Vital Sign (NVS) (Weiss et al., 2005). The NVS tests prose literacy and numeracy by the patient answering six structured questions after reading a nutrition label; one point is awarded for each correct answer. A score greater than four indicates adequate literacy skills, a score of less than four indicates possible limited health literacy, and a score of less than two indicates greater than 50% chance of having limited health literacy.
At baseline and at a follow-up visit six weeks after delivery of the intervention, participants completed measures of medication adherence and self-efficacy. For each measure, the lead author read the questions out loud, and participants responded from the available answer choices, referring to answer cards printed in large font for ease of reading. Adherence was measured using the Adherence to Refills and Medications Scale (ARMS) (Kripalani, Risser, Gatti, & Jacobson, 2009). The 12-item instrument was reduced to 10 items after removal of 2 items not applicable to this population; scores on the reduced instrument can range from 10 to 40, with lower scores indicating better adherence. The ARMS has high internal consistency reliability (Cronbach’s α = 0.81) and has previously shown a significant correlation with the Morisky adherence scale (Spearman’s rho = −0.651, P <0.01), as well as refill adherence calculated from pharmacy claims data (P <0.01). Lexile analysis found that the tool’s reading level is below 8th grade.
Self-efficacy was measured pre and post intervention using the Self-Efficacy for Appropriate Medication Use Scale (SEAMS), a 13-item measure (Risser, Jacobson, & Kripalani, 2007); scores range from 13 to 39, with higher scores indicating greater self-efficacy. The scale has high internal consistency reliability (Cronbach’s α = 0.89) and also correlates significantly with self-reported adherence.
Intervention
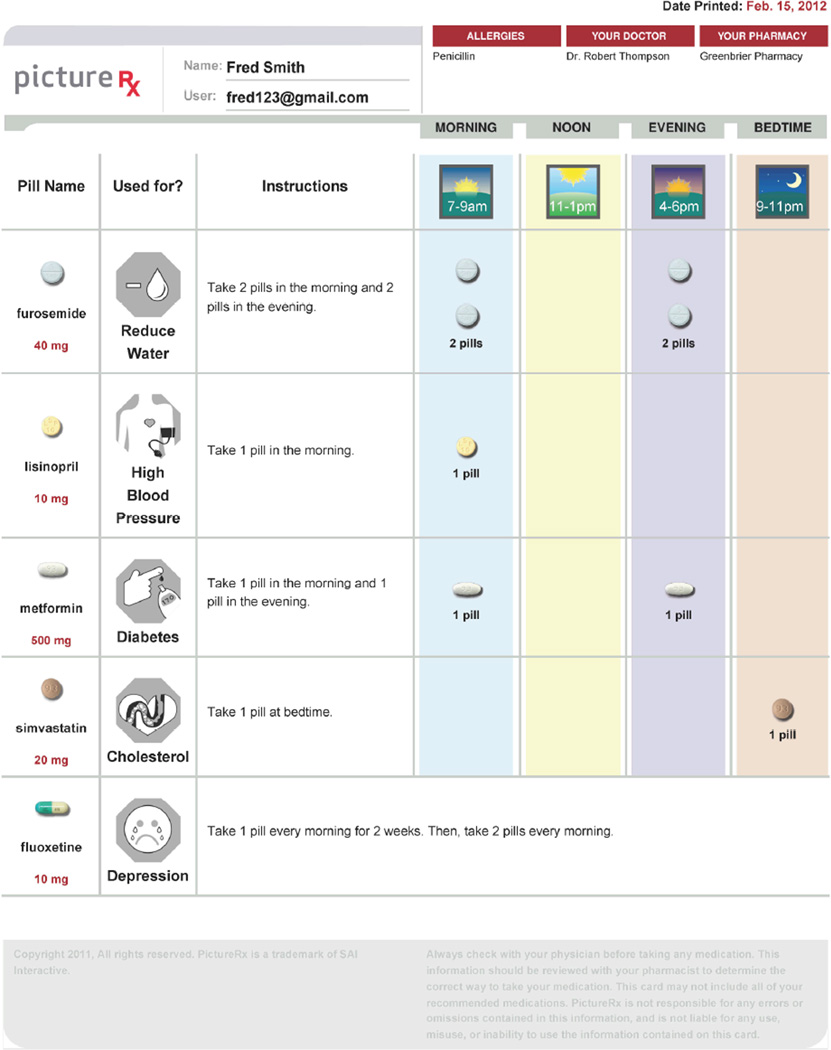
Participants received an illustrated depiction of their daily medication schedule PictureRX™ (Picture Rx, 2009) (Figure I). This educational aid shows the patient’s medications pictorially, uses plain language for instructions, and has icons to aid patients in understanding the purpose and dosing schedule. Previous studies show that concise language in medication instructions is better understood, especially among patients with limited health literacy (Davis et al., 2008; Davis et al., 2006). Prior research showed that the tool was rated as very helpful by patients and pharmacists (Blake, McMorris, Jacobson, Gazmararian, & Kripalani, 2010) for clarifying and reinforcing medication instructions.
Figure 1.
Sample Picture Rx Illustrated Daily Medication Schedule
To make the PictureRx cards, each participant’s medication regimen was first reconciled by a clinic pharmacist, referring to the facility’s pharmacy database. The lead author, a Doctor of Nursing Practice candidate, then made the PictureRx card, using a web-based interface. The cards were printed on letter size paper in color on a laser printer and enclosed in a clear plastic sleeve for protection. Patients were oriented briefly to the card, and they received educational instruction regarding the picture icons and dosing instructions, ending with a teach-back to confirm understanding (Walker, Pepa, & Gerard, 2010). The participants used their PictureRx cards for six weeks and were then surveyed to re-assess self-efficacy and adherence, as well as their perceptions about the usefulness of the PictureRX cards.
Statistical Analysis
Descriptive statistics of mean, standard deviation (SD), percentages, and frequency were calculated. The Related Samples Wilcox Signed Rank Test was used to evaluate the ARMS and SEAMS responses. Analysis was computed using the SPSS version 19.0. for Windows.
Results
Participant characteristics are described in Table I. The mean age was 75.3 (SD=8.8) and ranged from 59 to 89 years. Participants’ highest level of education was grade school (55%), high school (25%), some college preparation (15%), and college graduate (5%). Mini Mental Status Exam scores ranged from 18 to 30 (mean=24.5, SD=3.5). Per chart review, 25% of the participants were diagnosed with dementia. Results of Newest Vital Sign revealed that 70% of participants had a high likelihood of limited health literacy, while 25% had the possibility of limited health literacy. One participant’s score revealed adequate health literacy skills. The number of prescribed medications ranged from 4 to 21 (mean=13.2, SD=4.7).
Table I.
Participant Characteristics (N = 20)
| Characteristic | Valuea | |
|---|---|---|
| Age | ||
| Mean ± SD | 75.25 ± 8.77 | |
| Range | 59 – 89 | |
| Gender | ||
| Male | 7 (35) | |
| Female | 13 (65) | |
| Race/ethnicity | ||
| African American | 19 (95) | |
| Caucasian | 1 (5) | |
| Education | ||
| Grade school | 11 (55) | |
| High school | 5 (25) | |
| Some college | 3 (15) | |
| College graduate | 1 (5) | |
| Mini Mental Status Exam, mean ±SD | 24.55 ± 3.50 | |
| Number of Chronic Illnesses | ||
| Mean ± SD | 3.70 ± 1.38 | |
| Range | 2 – 7 | |
| Chronic Illnesses | ||
| CKD | 4 (20) | |
| CVA | 3 (15) | |
| Dementia | 5 (25) | |
| DM | 8 (40) | |
| HTN | 19 (95) | |
| hyperlipidemia | 14 (70) | |
| SD | 7 (35) | |
| Prescribed Medications | ||
| Mean ± SD | 13.20 ± 4.72 | |
| Range | 4 – 21 | |
| Health Literacy | ||
| High likelihood (50% or more) of limited literacy |
14 (70) | |
| Possibility of limited literacy | 5 (25) | |
| Adequate literacy | 1 (5) | |
Values represent number (percentage) unless otherwise noted.
At pretest, patients commonly reported non-adherence, such as forgetting to take their medications or skipping doses intentionally. After provision of PictureRx cards, patients less often reported such forms of non-adherence. Overall ARMS scores improved significantly after receipt of the intervention (pretest mean=13.3, SD=3.2; posttest mean=11.1, SD=3.1; p = .046 (Table II).
Table II.
Adherence to Refills and Medications Scale Results (N=20)
| Pre Intervention | Post Intervention | |||
|---|---|---|---|---|
| Count | Column N % |
Count | Column N % |
|
| 1. How often do you forget to take your medications? | ||||
| None of the time | 9 | 45% | 18 | 90% |
| Some of the time | 11 | 55% | 2 | 10% |
| Most of the time | ||||
| All of the time | ||||
| 2. How often do you decide not to take your medications? | ||||
| None of the time | 15 | 75% | 18 | 90% |
| Some of the time | 5 | 25% | 2 | 10% |
| Most of the time | ||||
| All of the time | ||||
| 3. How often do you forget to get prescriptions filled? | ||||
| None of the time | 19 | 95% | 18 | 90% |
| Some of the time | 1 | 5% | 2 | 10% |
| Most of the time | ||||
| All of the time | ||||
| 4. How often do you run out of medicine? | ||||
| None of the time | 15 | 75% | 18 | 90% |
| Some of the time | 5 | 25% | 2 | 10% |
| Most of the time | ||||
| All of the time | ||||
| 5. How often do you skip a dose of your medicine before you go to the doctor? | ||||
| None of the time | 11 | 55% | 18 | 90% |
| Some of the time | 9 | 45% | 2 | 10% |
| Most of the time | ||||
| All of the time | ||||
| 6. How often do you miss taking your medicine when you feel better? | ||||
| None of the time | 12 | 60% | 18 | 90% |
| Some of the time | 8 | 40% | 2 | 10% |
| Most of the time | ||||
| All of the time | ||||
| 7. How often do you miss taking your medicine when you feel sick? | ||||
| None of the time | 12 | 60% | 18 | 90% |
| Some of the time | 8 | 40% | 2 | 10% |
| Most of the time | ||||
| All of the time | ||||
| 8. How often do you miss taking your medicine when you are careless? | ||||
| None of the time | 14 | 70% | 18 | 90% |
| Some of the time | 6 | 30% | 2 | 10% |
| Most of the time | ||||
| All of the time | ||||
| 9. How often do you change the dose of your medication to suit your needs? | ||||
| None of the time | 14 | 70% | 18 | 90% |
| Some of the time | 6 | 30% | 2 | 10% |
| Most of the time | ||||
| All of the time | ||||
|
10. How often do you forget to take your medicine when you are supposed to take it more than once a day? | ||||
| None of the time | 14 | 70% | 17 | 85% |
| Some of the time | 6 | 30% | 3 | 15% |
| Most of the time | ||||
| All of the time | ||||
At pretest, self-efficacy for taking medications correctly was relatively low, with a mean score of 28.4 (SD=9.1) out of a possible 39. Patients commonly expressed lack of confidence with taking their medications, for example, when they had many medications to take, multiple times of day in which to take them, or had a change in their regimen or routine. After the intervention, confidence improved in each of these areas. Overall, SEAMS scores improved significantly after the intervention (posttest mean=35.8, SD=5.8, p < .001) (Table III).
Table III.
Self-Efficacy for Appropriate Medication Use Scale Results (N=20)
| Pre Intervention | Post Intervention | |||
|---|---|---|---|---|
| Count | Column N % | Count | Column N % | |
| 1. When you take several different medicines each day? | ||||
| not confident | 3 | 15% | ||
| somewhat confident | 11 | 55% | 5 | 25% |
| very confident | 6 | 30% | 15 | 75% |
| 2. When you have a busy day planned? | ||||
| not confident | 3 | 15% | ||
| somewhat confident | 9 | 45% | 5 | 25% |
| very confident | 8 | 40% | 15 | 75% |
| 3. When you are away from home? | ||||
| not confident | 3 | 15% | ||
| somewhat confident | 9 | 45% | 5 | 25% |
| very confident | 8 | 40% | 15 | 75% |
| 4. When no one reminds you to take the medicine? | ||||
| not confident | 4 | 20% | ||
| somewhat confident | 8 | 40% | 5 | 25% |
| very confident | 8 | 40% | 15 | 75% |
| 5. When you take medicines more than once a day? | ||||
| not confident | 4 | 20% | ||
| somewhat confident | 8 | 40% | 5 | 25% |
| very confident | 8 | 40% | 15 | 75% |
| 6. When the schedule to take the medicine is not convenient? | ||||
| not confident | 4 | 20% | ||
| somewhat confident | 8 | 40% | 5 | 25% |
| very confident | 8 | 40% | 15 | 75% |
| 7. When your normal routine gets messed up? | ||||
| not confident | 3 | 15% | ||
| somewhat confident | 9 | 45% | 5 | 25% |
| very confident | 8 | 40% | 15 | 75% |
|
8. When you get a refill of your old medicines and some of the pills look different than usual? | ||||
| not confident | 4 | 20% | ||
| somewhat confident | 9 | 45% | 5 | 25% |
| very confident | 7 | 35% | 15 | 75% |
| 9. When you are not sure how to take the medicine? | ||||
| not confident | 4 | 20% | ||
| somewhat confident | 9 | 45% | 5 | 25% |
| very confident | 7 | 35% | 15 | 75% |
| 10. When you are not sure what time of the day to take your medicine? | ||||
| not confident | 4 | 20% | ||
| somewhat confident | 9 | 45% | 5 | 25% |
| very confident | 7 | 35% | 15 | 75% |
| 11. When your doctor changes your medicines? | ||||
| not confident | 3 | 15% | ||
| somewhat confident | 10 | 50% | 5 | 25% |
| very confident | 7 | 35% | 15 | 75% |
| 12. When they cause some side effects? | ||||
| not confident | 4 | 20% | ||
| somewhat confident | 9 | 45% | 5 | 25% |
| very confident | 7 | 35% | 15 | 75% |
| 13. When you are feeling sick (like having a cold or the flu)? | ||||
| not confident | 4 | 20% | ||
| somewhat confident | 10 | 50% | 5 | 25% |
| very confident | 6 | 30% | 15 | 75% |
In the assessment of participants’ opinions, the PictureRX cards were rated as very easy to understand (Table IV); 100% of participants rated PictureRx cards as very helpful. The cards were felt to be most helpful in understanding the medication purpose (40%), dosing schedule (30%), and name (25%). Several participants requested an updated PictureRx card for use after the pilot project ended. Two participants revealed that they took their card to an appointment with a cardiologist and requested the physician to continue using this type of medication instruction.
Table IV.
Use and Perceived Utility of PictureRx Cards
| Count | Column N % | |
|---|---|---|
| 1. How often did you use your pill card when you first got it? | ||
| Every day | 20 | 100% |
| Every few days (more than once a week) | ||
| Once a week | ||
| Every few weeks | ||
| Once a month or less often | ||
| Never | ||
| 2. How often do you use your pill card now? | ||
| Every day | 8 | 40% |
| Every few days (more than once a week) | 7 | 35% |
| Once a week | 5 | 25% |
| Every few weeks | ||
| Once a month or less often | ||
| Never | ||
|
3. How easy is it to understand the pill card, in terms of when and how to take your medicines? | ||
| Very easy | 20 | 100% |
| Somewhat easy | ||
| Not easy | ||
| 4. Where did you keep your pill card most of the time? | ||
| On the refrigerator | 1 | 5% |
| In the bathroom | 3 | 15% |
| In my bedroom | 2 | 10% |
| Pocketbook, wallet, or pocket | ||
| Some other place where I keep my medicines | 14 | 70% |
| Other | ||
| 5A. Has the pill card helped you remember which medicines you are supposed to take? | ||
| Yes | 20 | 100% |
| No | ||
| 5B. Has the pill card helped you remember the names of the medicines? | ||
| Yes | 20 | 100% |
| No | ||
| 5C. Has the pill card helped you remember what the medicines are for? | ||
| Yes | 20 | 100% |
| No | ||
| 5D. Has the pill card helped you remember how many pills to take? | ||
| Yes | 20 | 100% |
| No | ||
| 5E. Has the pill card helped you remember what time to take each medicine? | ||
| Yes | 20 | 100% |
| No | ||
| 6. Which one of these has the pill card helped you with the most? | ||
| Remembering which medicines you are supposed to take |
||
| Remembering the names of the medicines | 5 | 25% |
| Remembering what the medicines are for | 8 | 40% |
| Remembering how many pills to take | 1 | 5% |
| Remembering what time to take each medicine | 6 | 30% |
| Other | ||
| 7. Overall, how helpful is the pill card? | ||
| Very helpful | 20 | 100% |
| Somewhat helpful | ||
| Not at all helpful | ||
Discussion
In this pilot study, we demonstrated that illustrated medication schedules (PictureRx cards), along with educational instruction using the teach-back methodology, significantly improved medication-related self-efficacy and adherence among community-dwelling elders. Participants rated the educational tool highly and used it regularly. The results of this study are consistent with other published literature which shows that illustrated medication instructions significantly increase patient satisfaction, understanding, recall, and adherence.
That self-efficacy improved in this population with multiple comorbidities, including dementia, is significant. The patients had substantial prior experience in taking medications, yet were unsure of how to do so. Provision of illustrated medication schedules improved their confidence with taking medications daily. For example, confidence in taking several medications each day improved from 30% to 75%; confidence in taking mediations more than once a day improved from 40% to 75%.
Patients with limited health literacy and who have chronic diseases benefit from focused education, as co-morbidities require complex medication and disease management (Fang, Matchtinger & Wang, 2006; Schillinger et. al., 2002). In this study, participants suffered from hypertension, hyperlipidemia, diabetes mellitus, chronic kidney disease, and dementia, resulting in daily complex medication regimens. Medication non-adherence is a risk factor for morbidity and mortality (Simpson et. al, 2006), and is frequently found among patients with cardiovascular and associated diseases (Ho, Bryson, & Rumsfield, 2009).
The NVS proved to be a straightforward tool for assessing health literacy. It was created for use in clinical settings (Johnson & Weiss, 2008; Weiss, et. al, 2005) and has been shown reliable and valid (Osborn et. al, 2007; Weiss, et. al, 2005). Health literacy screening took approximately three minutes per patient to complete, similar to the time reported in previous studies (Shah, West, Bremmeyer & Savoy-Moore, 2010; Vangeest, Welch, & Weiner, 2010; Johnson & Weiss, 2008; Monachos, 2007).
The results of this pilot project were presented to administrative and clinical staff. The case managers noted increased awareness of the scope and effects of limited health literacy as a result of staff development using the AMA Health Literacy Toolkit (2007). Communication strategies and the teach-back method are now being used by the case managers as advocated by the American Medical Association, The Joint Commission, and the Centers for Medicare and Medicaid Services (CMS). For example, the case managers verbalized that health instruction of dosing is now given in plain language; BID dosing is now given as “Take in the morning and at night” rather than “Take one twice daily.” Medication instruction also now includes a focused discussion of intent and purpose, using the teach-back method. The purposeful dialogue is an important factor in medication safety.
A limitation of this study is that it was conducted as pilot project, with a pre-post evaluation, using a small convenience sample of Medicare patients in a single health facility. These factors limit the generalizability of the findings. A second limitation is that 25% of the participants had clinical documentation of dementia, and this may have affected the validity of the self-report responses. However, we do not believe this to be the case, as each participant was able to complete the informed consent process and was able to teach-back medication instructions. Additional research is warranted to confirm this experience, as well as assess the effect of such an intervention on clinical outcomes.
These limitations notwithstanding, the project suggests a valuable model for improving medication use in clinical practice. Individualized health instruction, performed in a shame-free environment, with illustrated medication instructions and teach-back, promotes patient safety. The Joint Commission (2007) recommends using the teach-back method of communication as well as drawings to communicate health instruction. CMS (2010) advocates a reader-centered strategy in written health instruction for older adults who may experience decreased cognitive skills. Clear communication is a health initiative by the National Institutes of Health (NIH, 2009).
Dissemination of scientifically based best practices, including details of the journey, can increase quality of health care (Levin, Keefer, Marren, Vetter, Lauder & Sobolewski, 2009). Mancuso (2009) conducted a review of literature from 1991–2006 to identify psychometric properties of health literacy screening tools, noting that all articles and a majority of citations were from medical journals, not nursing journals. Professional nurses, and gerontological nurses specifically, should more often publish health literacy and quality improvement research in professional nursing journals to contribute to best practices, thus improving patient safety.
Baccalaureate nursing education includes provision of knowledge and skill sets in quality improvement and patient safety, as these are essential components of professional practice American Association of Colleges of Nursing (AACN, 2008). Incorporating health literacy awareness in curricula to prepare student nurses to address needs of the population in which they serve is an important task of nurse educators (Scheckel, Emery, & Nosek, 2010; Cormier, & Kotrlik, 2009; Owens, & Walden, 2007). As a nurse educator, this author will integrate health literacy awareness and related issues in the curriculum among undergraduate senior nursing students to promote patient-centered communication.
Funding Acknowledgements
This work was supported in part by R43 MD004048 from the National Institute for Minority Health and Health Disparities. The views expressed are solely those of the authors and do not necessarily represent those of the NIH.
Footnotes
Conflict of interest disclosure:
Dr. Kripalani is a consultant to and holds equity in PictureRx, LLC. The terms of this agreement were reviewed and approved by Vanderbilt University in accordance with its conflict of interest policies.
References
- American Association of Colleges of Nursing (AACN) The Essentials of Baccalaureate Education for Professional Nursing Practice. 2008 Retrieved from American Association of Colleges of Nursing website: http://www.aacn.nche.edu/education/bacessn.htm.
- American Medical Association (AMA) Health literacy and patient safety: Help patients understand. 2007 Retrieved from the American Medical Association website: http://www.ama-assn.org/ama1/pub/upload/mm/367/hl_monograph.pdf.
- Baker D, Wolf M, Feinglass J, Thompson J, Gazmararian J, Huange J. Health literacy and mortality among elderly persons. Archives of Internal Medicine. 2007;167(14):1503–1509. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- Blake S, McMorris K, Jacobosn K, Gazmararian J, Kripalani S. A qualitative evaluation of a health literacy intervention to improve medication adherence for underserved pharmacy patients. Journal of Health Care for the Poor and Undeserved. 2010;21(2) doi: 10.1353/hpu.0.0283. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services (CMS) Toolkit for Making Written Material Clear and Effective. 2010 Retrieved from Centers for Medicare and Medicaid Services website: https://www.cms.gov/
- Cormier C, Kotrlik J. Health literacy knowledge and experiences of senior baccalaureate nursing students. The Journal of Nursing Education. 2009;48(5):237–248. doi: 10.3928/01484834-20090416-02. [DOI] [PubMed] [Google Scholar]
- Davis T, Federman A, Bass P, Jackson R, Middlebrooks M, Parker R, et al. Improving patient understanding of prescription drug label instructions. Journal of General Internal Medicine. 2008;24(1):57–62. doi: 10.1007/s11606-008-0833-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis T, Wolf M, Bass P, Middlebrooks M, Kennen E, Baker D, et al. Low literacy impairs comprehension of prescription drug warning labels. Journal of General Internal Medicine. 2006;21(8):847–851. doi: 10.1111/j.1525-1497.2006.00529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis T, Michielutte R, Askov E, Williams M, Weiss B. Practical assessment of adult literacy in health care. Health Education & Behavior. 1998;25:613–623. doi: 10.1177/109019819802500508. [DOI] [PubMed] [Google Scholar]
- Egbert N, Nanna K. Health literacy: Challenges and strategies. OJIN: The Online Journal of Issues in Nursing. 2009;14(3) [Google Scholar]
- Fang M, Matchtinger E, Wang F. Health literacy and anticoagulation-related outcomes among patients taking Warfarin. Journal of General Internal Medicine. 2006;21:841–846. doi: 10.1111/j.1525-1497.2006.00537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazmararian J, Williams M, Peel J, Baker D. Health literacy and knowledge of chronic disease. Patient Education and Counseling. 2003;51(3):267–275. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- Gazmararian J, Baker D, Willams M, Parker R, Scott T, et al. Health literacy among Medicare enrollees in a managed care organization. Journal of the American Medical Association. 1999;281:545–551. doi: 10.1001/jama.281.6.545. [DOI] [PubMed] [Google Scholar]
- Ho M, Bryson C, Rumsfield J. Medication adherence: It’s importance on cardiovascular outcomes. Circulation. 2009;119:3028–3035. doi: 10.1161/CIRCULATIONAHA.108.768986. [DOI] [PubMed] [Google Scholar]
- Hoffman C, Rice D, Sung HY. Persons with chronic conditions: Their prevalence and costs. Journal of the American Medical Association. 1996;276:1473–1479. [PubMed] [Google Scholar]
- Nielsen-Bohlman L, Panzer A, Kindig D, editors. Institute of Medicine of the National Academies (IOM) Committee on health literacy. Health literacy: A prescription to end confusion. Washington, DC: National Academies Press; 2004. Apr, Retrieved from Institute of Medicine of the National Academies website: http://www.nap.edu/openbook.php?isbn=0309091179&page=R1. [PubMed] [Google Scholar]
- Johnson K, Weiss B. How long does it take to assess literacy skills in clinical practice? Journal of the American Board of Family Medicine. 2008;21(3):211–214. doi: 10.3122/jabfm.2008.03.070217. [DOI] [PubMed] [Google Scholar]
- Kripalani S, Risser J, Gatti M, Jacobson T. Development and evaluation of the adherence to refills and medications scale (ARMS) among low-literacy patients with chronic disease. Value in Health. 2009;12(1):118–123. doi: 10.1111/j.1524-4733.2008.00400.x. [DOI] [PubMed] [Google Scholar]
- Kutner M, Greenburg E, Baer J. A first look at the Literacy of America’s Adults in the 21st Century. National Center for Education Statistics: U.S. Department of Education; 2005. [Google Scholar]
- Levin R, Keefer J, Marren J, Vetter M, Lauder B, Sobolewski S. Evidenced-based practice improvement: Merging 2 paradigms. Journal of Nursing Care Quality. 2009;11:1–10. doi: 10.1097/NCQ.0b013e3181b5f19f. [DOI] [PubMed] [Google Scholar]
- Mancuso J. Assessment and measurement of health literacy: An integrated review of the literature. Nursing and Health Sciences. 2009;11:77–90. [Google Scholar]
- Marcus E. The silent epidemic: The health effects of illiteracy. The New England Journal of Medicine. 2006;355(10):1076–1078. doi: 10.1056/NEJMp058328. [DOI] [PubMed] [Google Scholar]
- Monachos C. Assessing and addressing low health literacy among surgical outpatients. AORN Journal. 2007;86(3):373–383. doi: 10.1016/j.aorn.2007.08.006. [DOI] [PubMed] [Google Scholar]
- National Institute of Health (NIH) Clear communication: An NIH health literacy initiative. 2009 Retrieved from National Institute of Health website: http://www.nih.gov/clearcommunication/healthliteracy.htm.
- National Network of Libraries of Medicine (NNLM) Health Literacy. 2008 Jun; Retrieved from National Network of Libraries of Medicine website: http://nnlm.gov/outreach/consumer/hlthlit.html.
- Oates D, Paasche-Orlow M. Health literacy: Communication strategies to improve patient comprehension of cardiovascular health. Circulation. 2009;119:1049–1051. doi: 10.1161/CIRCULATIONAHA.108.818468. [DOI] [PubMed] [Google Scholar]
- Osborn C, Weiss B, Davis T, Skripkaukas S, Rodrigue C, Bass P, et al. Measuring adult health literacy in health care: Performance of the newest vital sign. American Journal of Health Behavior. 2007;31(S1):S36–S46. doi: 10.5555/ajhb.2007.31.supp.S36. [DOI] [PubMed] [Google Scholar]
- Owens L, Walden D. Health literacy: The new essential in nursing education. Nurse Educator. 2007;32(6):238–239. doi: 10.1097/01.NNE.0000299472.26691.f6. [DOI] [PubMed] [Google Scholar]
- Pace Greater New Orleans (PACE GNO) 2010 Retrieved from Pace Greater New Orleans website: http://www.ccano.org/pace.htm.
- PictureRX™. Pill card. 2009 Retrieved from PictureRX™ website: http://mypicturerx.com/info/
- Risser J, Jacobson T, Kripalani S. Development & psychometric evaluation of the self-efficacy for appropriate medication use scale (SEAMS) in low-literacy patients with chronic disease. Journal of Nursing Measurement. 2007;15(3):203–219. doi: 10.1891/106137407783095757. [DOI] [PubMed] [Google Scholar]
- Scheckel M, Emery N, Nosek C. Addressing health literacy: the experiences of undergraduate nursing students. Journal of Clinical of Nursing. 2010;19(5-6):794–802. doi: 10.1111/j.1365-2702.2009.02991.x. [DOI] [PubMed] [Google Scholar]
- Schillinger D, Grumback K, Piette J, Wang F, Osmond D, Daher C, et al. Association of health literacy with diabetic outcomes. Journal of the American Medical Association. 2002;228(4):475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- Shah L, West P, Bremmeyer K, Savoy-Moore R. Health literacy instrument in family medicine: The newest vital sign ease of use and correlates. The Journal of the American Board of Family Medicine. 2010;23(2):195–203. doi: 10.3122/jabfm.2010.02.070278. [DOI] [PubMed] [Google Scholar]
- Simpson S, Eurich D, Majumdar S, Padwal R, Tsuyki R, Varney J, et al. A meta- analysis of the association between adherence to drug therapy and mortality. British Medical Journal. 2006;333:15. doi: 10.1136/bmj.38875.675486.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudore R, Yaffe K, Satterfield S, Harris T, Mehta K, Simonsick, et al. Limited literacy and mortality in the elderly. Journal of General Internal Medicine. 2006;21:806–812. doi: 10.1111/j.1525-1497.2006.00539.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Joint Commission. (TJC) What did the doctor say? Improving health literacy to protect patient safety. 2007 Feb; Retrieved from The Joint Commission website: http://www.jointcommission.org/What_Did_the_Doctor_Say/
- Vangeest J, Welch V, Weiner S. Patient’s perceptions of screening for health literacy: Reactions to the newest vital sign. Journal of Health Communication. 2010;15:402–412. doi: 10.1080/10810731003753117. [DOI] [PubMed] [Google Scholar]
- Walker J, Pepa C, Gerard P. Assessing the health literacy levels of patients using selected hospital services. Clinical Nurse Specialist. 2010;24(1):31–37. doi: 10.1097/NUR.0b013e3181c4abd0. [DOI] [PubMed] [Google Scholar]
- Weiss B, Mays M, Martz W, Castro K, DeWalt D, Pignone M, et al. Quick assessment of literacy in primary care: The newest vital sign. Annals of Family Medicine. 2005;3(6):514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]