Abstract
Background
Pain is the most common but severe physical symptom among cancer patients. This study aimed to identify correlation between pain and psychological symptoms for terminal cancer patients.
Methods
The total sample consisted of 69 subjects who were recruited through two hospice wards, limited to patients who were mentally alert and had no psychiatric diseases. The subjects were divided into two groups according to the numerical rating scale: the pain-free group, 0 to 3 points; and the pain group, 4 to 10 points. We used the Beck depression inventory (BDI), Beck anxiety inventory (BAI), mini-mental status examination-Korea (MMSE-K), and short form 36 health survey (SF-36). Logistic regression analysis was performed to verify the correlation between pain and other psychosocial disorders.
Results
The mean scores of BDI in the pain-free and pain groups were 25.7 and 31.5; mean BAI scores were 23.4 and 34.7; mean MMSE-K scores were 25.7 and 21.8, respectively. There were no significant differences between the two groups in SF-36 score except scores of body pain. The results of logistic regression analysis adjusted for age, sex, marital status, types of cancer, history of chemotherapy, or radiotherapy showed significant correlation between pain and depression (BDI ≥ 24; odds ratio [OR], 4.199; 95% confidence interval [CI], 1.171 to 15.060), and pain and cognitive impairment (MMSE < 24; OR, 5.495; 95% CI, 1.449 to 20.843); but not between pain and anxiety (BAI ≥ 22; OR, 3.011; 95% CI, 0.907 to 9.997).
Conclusion
Pain significantly affects depression and cognitive impairment among advanced cancer patients in the hospice ward. Accordingly, more aggressive treatment of pain is required to reduce not only physical suffering but also physiological distress.
Keywords: Terminal Cancer, Hospices, Pain, Depression, Anxiety, Cognition
INTRODUCTION
With the rapid increase in the elderly population in recent years, the prevalence and mortality rate of various cancers are also rapidly increasing.1) A terminal cancer patient is defined as a patient with incurable advanced cancer requiring palliative care for quality of life in whom meaningful life extension cannot be anticipated with current medicine and who is expected to expire within a few months. It is known that life expectancy of terminal cancer patients is about 3 to 6 months.2) According to a report conducted in 1998, when Korean people reported a preference for dying at home, the death rate at home was 61%, but this rate has decreased to 20%, and the death rate in health care institutions or social welfare institutions has increased to 75% in 2011.3) Furthermore, a study regarding preferred place of death that was conducted with the Korean elderly revealed that they preferred hospitals or hospices to home.4) Therefore, admission care in hospice will expand in the future.
In cancer patient care, pain is one of important issues; it is reported that 30% to 50% of cancer patients experience cancer pain,5) and cancer-related pain significantly increases to 60% to 90% in case of metastasis.6,7) Even in Korea, it is reported that pain is the most common and severe complaint among terminal cancer patients and aggressive management is required in 93.7% of them, highlighting the significance of pain.8) Another significant issue in cancer patients is psychological problems such as depression or anxiety. It is known that the most common psychopathologies in cancer patients are anxiety and depression.9) A Chinese study demonstrated that more than 26% of Chinese cancer patients had psychological problems such as depression and anxiety10) and another study conducted in a Western country also showed that more than a third of lung cancer patients had depression and anxiety.11) Pain is an aggravating factor for mood disorders such as depression and anxiety; the risk of mood disorders such as depression and anxiety in patients with chronic peripheral neuropathy is 4.21 to 6.9 times higher than the general population,12) and psychological disorders such as depression, anxiety, and dysthymia are commonly accompanied in patients with chronic pain.13) However, associations between pain and depression and anxiety in terminal cancer patients are controversial. A Dutch study conducted in palliative care wards failed to demonstrate a significant correlation between pain and depression and anxiety14) whereas a Taiwanese study showed that physical symptoms including pain were significantly higher in depressed cancer patients,15) and a study conducted in the United States also showed that mood disorders such as depression, anxiety, and anger were significantly higher in the patient group with cancer-related pain.16) A Korean study reported that depression levels were associated with the most severe pain and the current pain but not significantly correlated with the minimal pain and analgesia responses,17) and another Korean study conducted with elderly cancer patients demonstrated a significant correlation between the mean pain score over 24 hours and depression.18) However, it is hard to find other Korean studies regarding association between pain and depression, and there is a lack of studies considering anxiety, cognitive function, and quality of life in terminal cancer patients. Hence, this study aimed to evaluate associations between pain and depression, anxiety, and cognitive impairment in terminal cancer patients admitted to hospice wards and the impact of pain on them.
METHODS
1. Subjects
This study was conducted from May in 2011 to May in 2012, in the hospice wards in Kyungpook National University Medical Center and Daegu Veteran's Hospital with patients who were mentally alert and were able to express themselves and to fill in a questionnaire. Admission criteria were terminal cancer patients with life expectancy less than 6 months in whom active cancer treatments are no longer beneficial and the general condition is deteriorating. Patients with other physical health problems, patients who cannot be evaluated accurately due to drug dependency, and patients with a history of psychological disorders including depression were excluded from this study. This study was approved by the institutional review board of Kyungpook National University Medical Center.
2. Psychometric Assessment Instruments
Medical records including cancer types, the presence of metastasis, and treatments were reviewed and psychological assessment was performed by family medicine doctors using assessment tools via direct interviews on admission.
1) Pain assessment
To assess pain, the numerical rating scale (NRS) which was developed to objectify subjective pain levels and widely used for pain assessment, was utilized. The score ranges from 0 to 10; zero indicates no pain and ten indicates the most excruciating pain that a patient has ever experienced in his/her lifetime. NRS for a week was recorded and the subjects were divided into two groups at the point of NRS 4.
2) Depression assessment
To assess depression, the Beck depression inventory (BDI) was utilized. The BDI was developed in 1961 and has been used worldwide, and its reliability was verified in Korea. The BDI includes a total of 21 items and scores less than 9 are normal; scores between 10 and 15 indicate mild depression; scores between 16 and 23 indicate moderate depression; and scores between 24 and 63 indicate severe depression. In the present study, the cut-off score was 24.19)
3) Anxiety assessment
To assess anxiety, the Beck anxiety inventory (BAI) was used. The BAI includes 21 items and each item yields a score of 0 to 4; a total score greater than 22 indicates anxiety requiring close observation and intervention.20)
4) Quality of life assessment
To assess quality of life with respect to health, the medical outcomes study 36-item short-form health survey (SF-36) which was developed by Ware and Sherbourne21) and whose reliability and validity was proved by Koh et al.22) in the Korean version was utilized. Each category yields a score of 0 to 100 and higher scores indicate a higher level of quality of life.21, 23)
5) Cognitive function assessment
To assess cognitive function, MMSE-K, which was devised to assess cognitive function within a short period of time, was used. MMSE-K has 11 items. The total score is 30 and scores less than 24 indicate cognitive impairment.24, 25)
3. Statistical Analysis
The subjects were divided into a pain-free group including patients with NRS 0 to 3 and a pain group including patients with NRS 4 to 10. Independent t-test, Pearson's chi-square test and Fisher's exact test were used to compare characteristics of the two groups, and logistic regression analysis was performed to evaluate the association between pain and depression, anxiety, and cognitive impairment. All statistical analyses were performed using IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA). Statistical significance was defined as P-value < 0.05.
RESULTS
1. General Characteristics
Of 75 candidates who met the eligibility criteria, 6 patients with a history of depression were excluded and a total of 69 patients were finally enrolled. There were 51 male (73.9%) and 18 female patients (26.1%), and the mean age was 64.7 years old. This study included various diagnoses such as gastric cancer, lung cancer, and colorectal cancer. The subjects were divided into two groups at the NRS score of 4: the pain-free group (n = 48) and the pain group (n = 21). The mean ages of the pain-free group and the pain group were 64.1 years and 66.1 years, and the percentage of male patients was 79.2% and 61.9%, respectively. There were no significant differences in age, sex, marital status, cancer type, presence of metastasis, history of surgical interventions, chemotherapy, or radiotherapy between the groups (Table 1).
Table 1.
Clinical characteristics of the subjects between pain groups
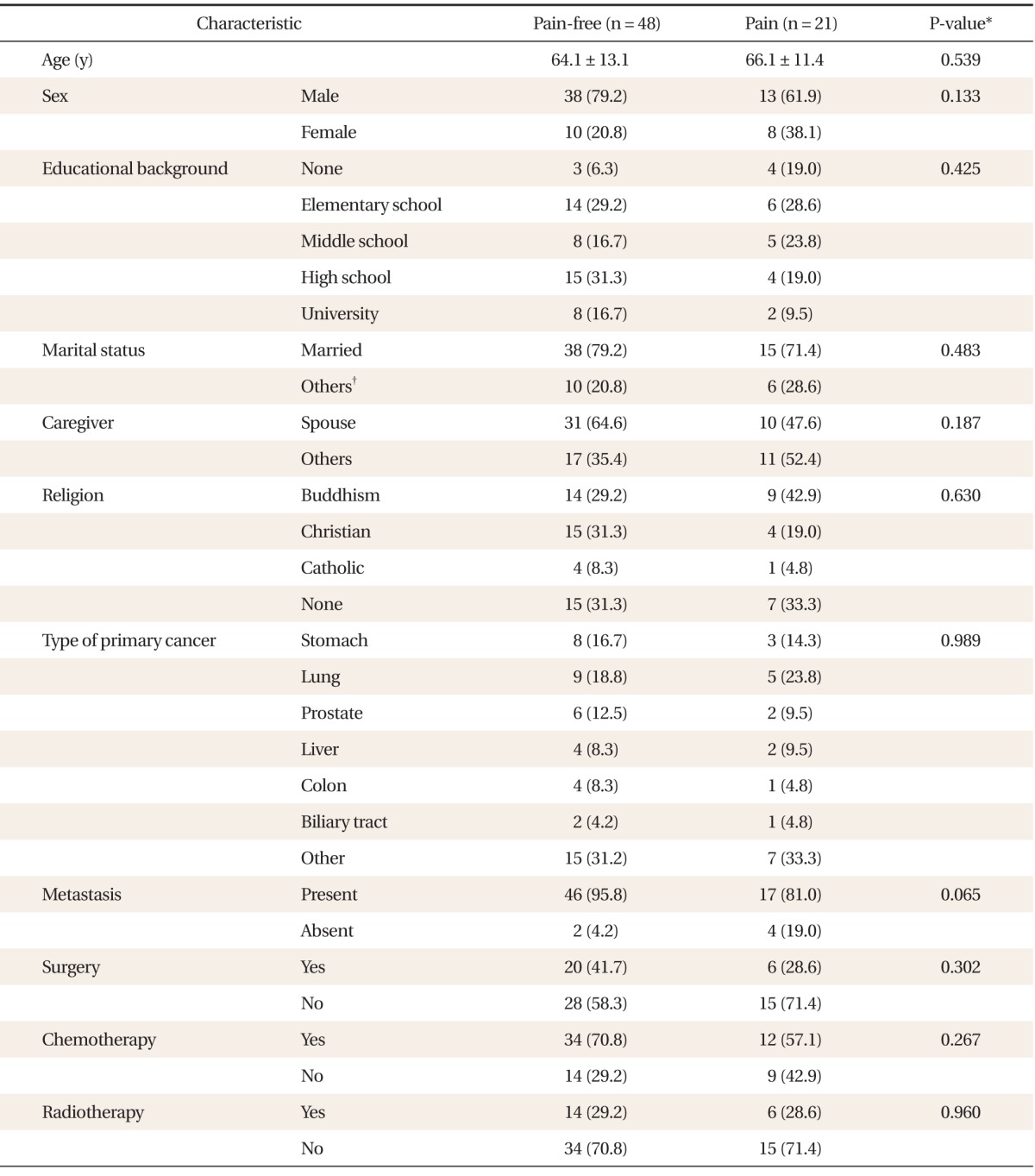
Values are presented as mean ± SD or number (%).
*Independent t-test for continuous variables, and Pearson's chi-square test or Fisher's exact test for discrete variables. †Including divorced, widowed, and unmarried subjects.
2. Use of Painkiller and Laboratory Test Results
The rate of subjects using narcotic analgesics on admission in the pain-free group and the pain group, excepting fentanyl patch, was 62.5% and 76.2% (P = 0.776), respectively. The dose of narcotic analgesics was higher in the pain group than the pain-free group, but there was no statistical significance (56.2 and 82.4 mg oral morphine equivalents/d, respectively; P = 0.248). There were no statistically significant differences in laboratory tests including white blood cell, hemoglobin, platelets, serum creatinine, and liver enzymes between the two groups (Table 2).
Table 2.
Comparisons of the painkiller use and laboratory findings between pain groups
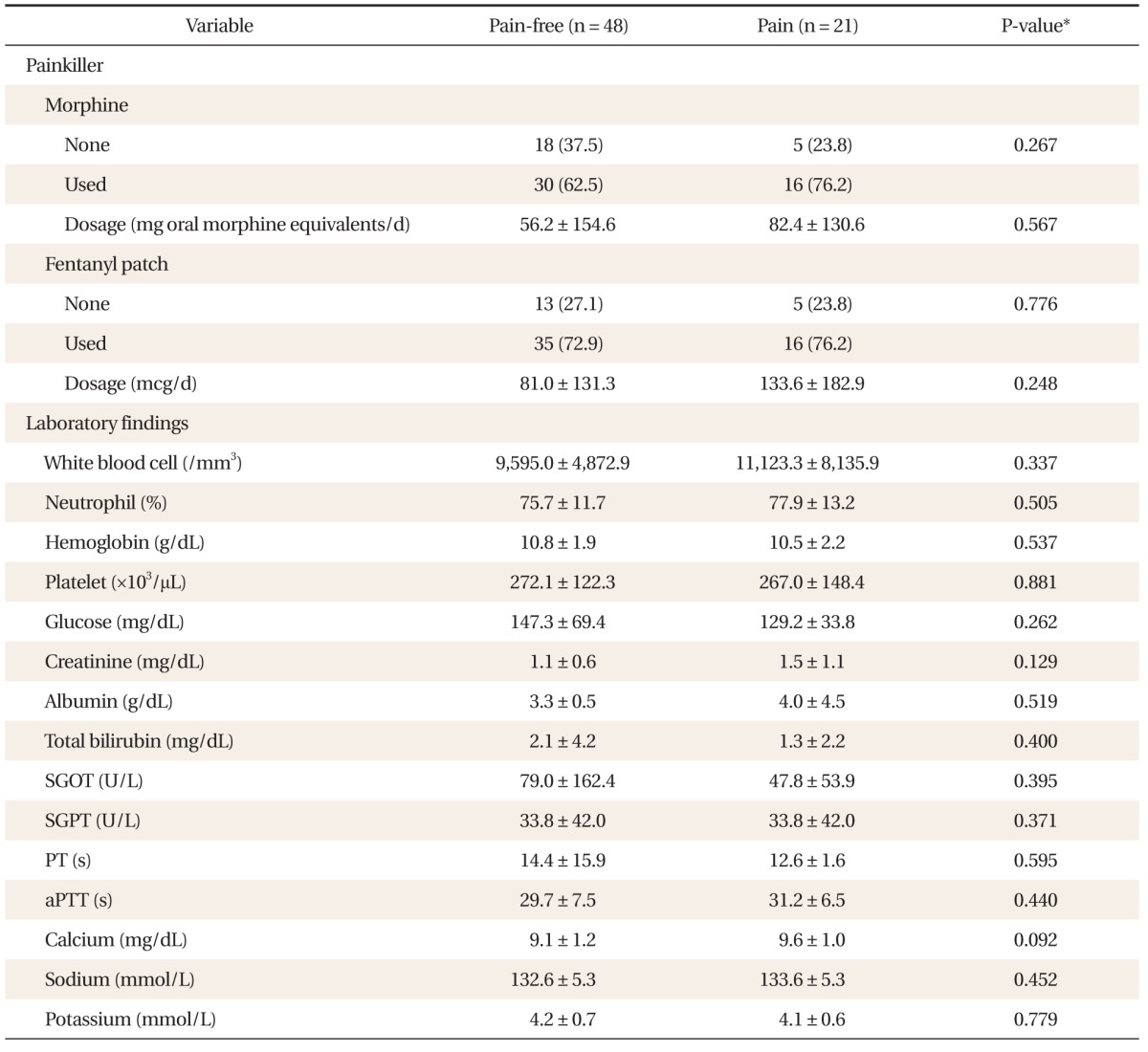
Values are presented as number (%) or mean ± SD.
SGOT: serum-glutamic-oxaloacetic transaminase, SGPT: serum-glutamic-pyruvic transaminase, PT: prothrombin time, aPTT: activated partial thromboplastin time.
*Independent t-test for continuous variables, and Pearson's chi-square test for discrete variables.
3. Depression, Anxiety, Cognitive Function, and Quality of Life
The mean NRS score of the pain-free group and the pain group was 1.7 and 5.0, respectively. The mean BDI score of the pain-free group and the pain group was 25.7 and 31.5, respectively. The mean BAI score of the pain-free group and the pain group was 23.4 and 34.7, respectively. The mean MMSE score of the pain-free group and the pain group was 25.7 and 21.8, respectively. Patients with BDI score greater than 24, indicating severe depression, and BAI score greater than 22, indicating anxiety, were 52.1% and 76.2% in both groups, respectively. Patients with MMSE score less than 24, indicating cognitive impairment, were 18.8% in the pain-free group and 47.6% in the pain group. The mean SF-36 scores were 31.8 and 29.3; there were no significant differences in the mean score of each category but body pain was significantly lower in the pain group with a score of 31.7 compared to the pain-free group with a score of 40.1 (P = 0.004) (Table 3).
Table 3.
Comparisons of the results of psychosocial tests between pain groups
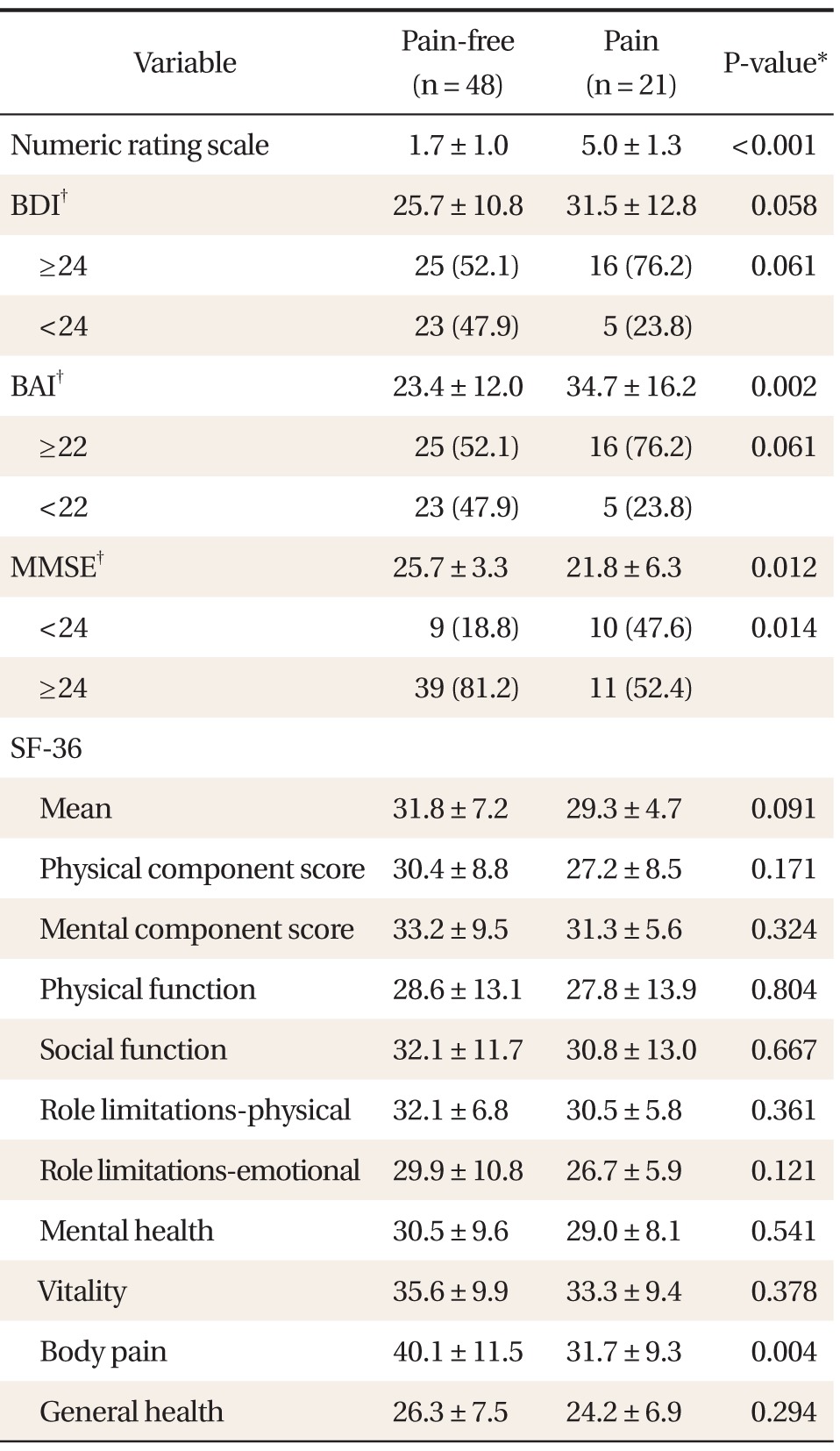
Values are presented as mean ± SD or number (%).
BDI: Beck depression inventory, BAI: Beck anxiety inventory, MMSE: mini-mental status examination, SF-36: short form-36 health survey.
*Independent t-test for continuous variables, and Pearson's chi-square test for discrete variables. †BDI ≥ 16, presence of significant depression; BAI ≥ 22, presence of anxiety that needs clinical intervention; MMSE < 24, presence of cognitive impairment.
4. The Relation between Pain and Depression, Anxiety, and Cognitive Impairment
With the dependent variables including depression with BDI score ≥ 24, anxiety with BAI ≥ 22, and cognitive impairment with MMSE < 24, logistic regression analysis was performed using the pain group as the independent variable. Marital status, cancer type, history of cytotoxic chemotherapy, or radiation therapy, which are known to be influential factors for depression and anxiety,26,27) were adjusted (model 3) in addition to age and sex. Odds ratio (OR) for depression was 4.199 (95% CI, 1.171 to 15.060) and OR to cognitive impairment was 5.495 (95% CI, 1.449 to 20.843), showing significance, but OR to anxiety was 3.011 (95% CI, 0.907 to 9.997), failing to show statistical significance (Table 4).
Table 4.
The associations between pain and depression, anxiety and cognitive function decline
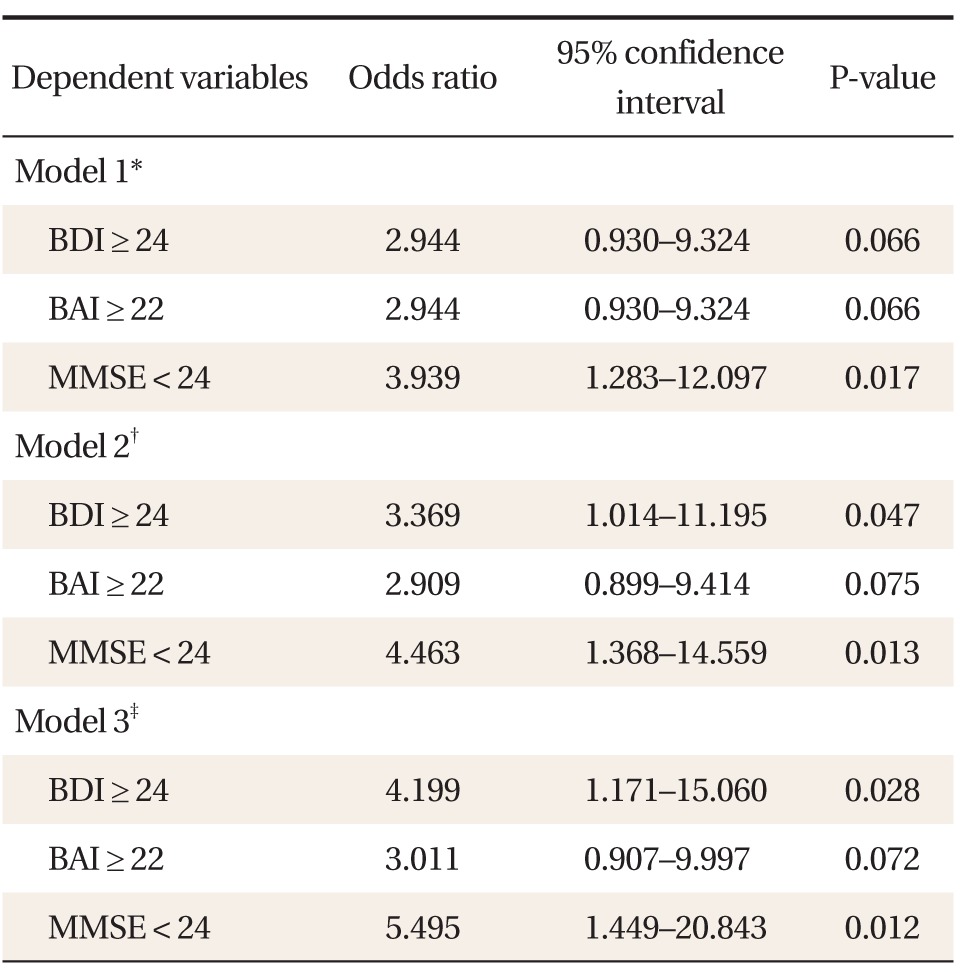
BAI, Beck anxiety inventory; BDI, Beck depression inventory, MMSE, mini-mental status examination.
*Simple logistic regression analysis, pain group as independent variable. †Based on model 1, model 2 was further adjusted for age and sex. ‡Based on model 2, model 3 was further adjusted for marital status, types of cancer, history of chemotherapy, and history of radiotherapy.
DISCUSSION
This cross-sectional study was conducted with terminal cancer patients in hospice wards to determine the association between pain and depression, anxiety, and cognitive impairment. The results showed that pain has a significant correlation with severe depression and cognitive impairment.
Pain is the most common symptom in terminal cancer patients and it is known that pain is more severe in the advanced stages of cancers.5-8) Depression and anxiety are also commonly found mood disorders.9) In the present study, patients who demonstrated severe depression with BDI greater than or equal to 24 and anxiety with BAI greater than or equal to 22 requiring intervention were about 60%, which was rather higher than previous studies,10,11) which reported about 30%. However, since the previous studies were based on outpatient clinics, direct comparison with the present study that was conducted with only terminal cancer patients is considered to be irrational. In fact, a study conducted with patients in hospice wards in the United States28) reported that the incidence of depression was about 70%, and a study conducted with patients in hospice wards in the United Kingdom29) also reported that the incidence of depression or anxiety was 64%. Thus, the high incidence of depression and anxiety in the present study might be due to patient selection. Furthermore, considering the fact that the incidence of depression becomes higher in more advance cancer patients and patients without supportive family members,26) it is possible that a higher percentage of terminal metastastic cancer patients and a high percentage of single patients who were divorced or bereaved (23%) in this study might have contributed to the higher incidence of depression and anxiety.
It is known that there is a significant correlation among depression, anxiety, and pain.15-18) The present study results also demonstrated that the patient group with severe pain showed a higher level of depression and anxiety compared to the patient group without pain or mild pain, which was consistent with previous studies. The percentage of patients with significant depression and anxiety was also relatively higher in the pain group. With adjustment of influential factors that may affect depression or anxiety, including age, sex, marital status, cancer types, histories of chemotherapy, or radiation therapy, risk of severe depression increased 4.2 times with pain, showing significant correlation between pain and depression. This is not limited only to cancer patients. In fact, the risks of depression and anxiety increase 6.9 times and 4.21 times, respectively, in patients with chronic pain, implying that pain is significantly related to depression and anxiety.12) It is not surprising that pain is associated with psychosocial factors. Pain conveys messages to the brain via complex pathways. Several factors such as sensory, immediate emotions, and secondary emotions are involved in the pathways and psychological factors, in particular, regulate various areas of pain.30) Therefore, psychological issues contributing to pain are as significant as physical pain itself. In a study conducted with patients with a similar level of pain by Turk et al.,31) psychosocial impairment was observed in 81% of metastatic cancer patients, 84% of cancer patients without metastasis, and 85% of patients with non-cancerous chronic pain. This shows that pain is a process involutedly related with psychological issues. However, in the present study, multivariate analysis failed to show statistical significance with respect to anxiety. A previous Dutch study conducted with 79 patients14) also failed to demonstrate significant associations between pain and depression and anxiety. Therefore, it is judged that the insignificant result of the present study stemmed from the small sample size, and positive results are expected in larger studies.
The interesting finding of the present study is that pain has a significant impact on cognitive impairment in terminal cancer patients. The MMSE-K score was significantly lower in the pain group with a difference of 4, and the presence of significant cognitive impairment was also significantly higher in the pain group with a rate of 47.6% compared to the pain-free group with a rate of 18.8%. In addition, multivariate analysis adjusted for associated factors of cognitive impairment revealed that the risk of cognitive impairment increased to 5.5 times in the presence of pain. In fact, the relationship between pain and cognitive impairment has been proven in clinical trials and experimental studies. Cognitive impairments related to pain include impaired concentration, deteriorated learning ability and memory, slowed information processing, psychomotor deterioration, and reduced performance.32) Previous studies using MMSE33-36) also showed significantly lower MMSE scores in pain groups as shown in the present study. In previous studies, mean MMSE scores ranged from 26 to 28, which were rather better than the mean MMSE score of the present study. It is thought that this difference stemmed from the fact that the current study was conducted with terminal cancer patients in hospice wards. Direct correlation between cancer and cognitive impairment has not yet been demonstrated. However, since it is possible that cancer treatments-especially chemotherapy or endocrine therapy-can induce short-term or long-term cognitive impairment,37,38) the influence of cancer treatment on low MMSE scores cannot be completely excluded in the present study.
The mean quality of life score was slightly lower in the pain group in the present study, with scores of 29.3 in the pain group and 31.8 in the pain-free group, but there was no statistical significance. There were no significant differences in the other 8 subcategories but a significantly lower 'body pain' score was seen in the pain group. This is an expected result since the pain group has greater pain. Previous studies demonstrated a significant correlation between pain and low quality of life score in terminal cancer patients39,40) and a consistent result is expected when the sample size increases.
The present study has following limitations. First, as mentioned above, the sample size is small. The hospice wards in the two hospitals where this study was conducted have only 20 beds each and it is difficult to expect fast bed turnover rate due to the nature of hospice wards. Moreover, patients with alert mental status who were able to participate in the survey were limited which resulted in small number of subjects. Second, survey research itself has limitations. To minimize limitations of survey research, patient interviews were conducted by attending doctors upon admission. Nonetheless, the mean age was 64.7 years old and the subjects older than 60 years were 71.0%. Patients without formal school education were 10.1% and there were patients who could not understand objectified sentences. In this case, questions were re-explained in easier sentences. Error occurrence secondary to subjective ideas was possible. Third, since this study was conducted as a cross-sectional study, it is difficult to determine the order of the incident. This means that pain is related to depression and cognitive impairment but it is difficult to infer that pain induces depression or cognitive impairment. Fourth, on application of Bonferroni correction, odds ratio of pain to depression was not statistically significant (P = 0.084). Bonferroni correction was not applied because this study was conducted as an exploratory cross-sectional study, but it is difficult to judge whether the results are confirmative. Fifth, although there was no significant difference in analgesia between the groups, analgesic effects, the most significant factor, were not adjusted in this study.
However, this study is considered to be significant since it was conducted with terminal cancer patients in hospice wards with higher levels of pain intensity using various psychological tests related to pain, whereas previous studies were conducted regardless of cancer stage, or were conducted with cancer patients visiting outpatient clinics. In addition, in the present study, analyses were performed after fundamental factors and factors such as chemotherapy or radiotherapy were adjusted to minimize influential factors on both pain and psychological status, and the results showed that there are significant associations between pain and depression and cognitive function. The relationship between cognitive impairment and pain, in particular, still showed statistical significance (P = 0.039) upon application of Bonferroni correction; therefore, pain has a close relationship with cognitive impairment. The present study is significant because studies on associations between pain and cognitive impairment in terminal cancer patients hardly exist and have not been performed in Korea.
In conclusion, incidence of depression, anxiety, and cognitive impairment in terminal cancer patients staying in hospice wards were high, and pain was significantly correlated with depression and cognitive impairment. These results were consistent even after adjustment for factors such as sex, chemotherapy, or radiotherapy. Since depression and anxiety commonly accompany mood disorders in terminal cancer patients, health care teams should understand this and provide psychological intervention such as cognitive behavioral therapy as well as drug treatment using anti-depressants or anti-anxiety medication at the earliest stages. Health care teams in hospice wards in particular should acknowledge that pain is one of the most influential factors exacerbating mood disorders and cognitive impairment, and pay special attention to pain control management. We hope that there will be further large scale prospective studies regarding the impact of pain on psychological disorders.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Statistics Korea. KOSIS: annual report on the cause of death statistics [Internet] Daejeon: Statistics Korea; c2011. [cited 2012 Oct 20]. Available from: http://kostat.go.kr/portal/korea/kor_ki/1/1/index.action?bmode=read&cd=S004001. [Google Scholar]
- 2.Youn YH. Comprehension of advanced cancer patients and approach family medicine. J Korean Acad Fam Med. 1998;19:979–986. [Google Scholar]
- 3.Statistics Korea. KOSIS: deaths by place of death, 1998-2011 [Internet] Daejeon: Statistics Korea; [cited 2012 Oct 20]. Available from: http://kosis.kr/abroad/abroad_01List.jsp?parentId=D. [Google Scholar]
- 4.Choi JH, Byeon JJ, Lee S, Han SH. Preferred place of death of elderly women in Seoul. J Korean Acad Fam Med. 2001;22:939–945. [Google Scholar]
- 5.Portenoy RK, Lesage P. Management of cancer pain. Lancet. 1999;353:1695–1700. doi: 10.1016/S0140-6736(99)01310-0. [DOI] [PubMed] [Google Scholar]
- 6.Daut RL, Cleeland CS. The prevalence and severity of pain in cancer. Cancer. 1982;50:1913–1918. doi: 10.1002/1097-0142(19821101)50:9<1913::aid-cncr2820500944>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 7.Foley KM. The treatment of cancer pain. N Engl J Med. 1985;313:84–95. doi: 10.1056/NEJM198507113130205. [DOI] [PubMed] [Google Scholar]
- 8.Kwon YC, Yun YH, Lee KH, Son KY, Park SM, Chang YJ, et al. Symptoms in the lives of terminal cancer patients: which is the most important? Oncology. 2006;71:69–76. doi: 10.1159/000100450. [DOI] [PubMed] [Google Scholar]
- 9.Davies RK, Quinlan DM, McKegney FP, Kimball CP. Organic factors and psychological adjustment in advanced cancer patients. Psychosom Med. 1973;35:464–471. doi: 10.1097/00006842-197311000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Song H, Li J, Lu Y, Deng L, Sun XL. Investigation of mental health and its influence on Chinese cancer patients using a multidisciplinary screening flow: an epidemiological survey in the west of China. Chin Med J (Engl) 2013;126:61–67. [PubMed] [Google Scholar]
- 11.Arrieta O, Angulo LP, Nunez-Valencia C, Dorantes-Gallareta Y, Macedo EO, Martinez-Lopez D, et al. Association of depression and anxiety on quality of life, treatment adherence, and prognosis in patients with advanced non-small cell lung cancer. Ann Surg Oncol. 2013;20:1941–1948. doi: 10.1245/s10434-012-2793-5. [DOI] [PubMed] [Google Scholar]
- 12.Radat F, Margot-Duclot A, Attal N. Psychiatric co-morbidities in patients with chronic peripheral neuropathic pain: A multicentre cohort study. Eur J Pain. 2013 May 29; doi: 10.1002/j.1532-2149.2013.00334.x. [Epub]. http://dx.doi.org/10.1002/j.1532-2149.2013.00334.x. [DOI] [PubMed] [Google Scholar]
- 13.Castro M, Kraychete D, Daltro C, Lopes J, Menezes R, Oliveira I. Comorbid anxiety and depression disorders in patients with chronic pain. Arq Neuropsiquiatr. 2009;67:982–985. doi: 10.1590/s0004-282x2009000600004. [DOI] [PubMed] [Google Scholar]
- 14.Teunissen SC, de Graeff A, Voest EE, de Haes JC. Are anxiety and depressed mood related to physical symptom burden?: a study in hospitalized advanced cancer patients. Palliat Med. 2007;21:341–346. doi: 10.1177/0269216307079067. [DOI] [PubMed] [Google Scholar]
- 15.Chen ML, Chang HK. Physical symptom profiles of depressed and nondepressed patients with cancer. Palliat Med. 2004;18:712–718. doi: 10.1191/0269216304pm950oa. [DOI] [PubMed] [Google Scholar]
- 16.Glover J, Dibble SL, Dodd MJ, Miaskowski C. Mood states of oncology outpatients: does pain make a difference? J Pain Symptom Manage. 1995;10:120–128. doi: 10.1016/0885-3924(94)00073-t. [DOI] [PubMed] [Google Scholar]
- 17.Yang MJ, Jeon YW, Han SI, Han CW, Eom HS. Depression and pain in patients with cancer: a preliminary study. J Korean Neuropsychiatr Assoc. 2000;39:1122–1131. [Google Scholar]
- 18.Yu SJ, Kim HS. The study of pain and depression in elderly cancer patients. J Korean Gerontol Nurs. 2000;2:154–166. [Google Scholar]
- 19.Park HJ, Kim HN, Kim IB, Jeon SA. Reliability of the Beck depression inventory in adolescence. J Korean Acad Fam Med. 2000;21:244–253. [Google Scholar]
- 20.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 21.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 22.Koh SB, Chang SJ, Kang MG, Cha BS, Park JK. Reliability and validity on measurement instrument for health status assessment in occupational workers. Korean J Prev Med. 1997;30:251–266. [Google Scholar]
- 23.McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-item short-form health survey (SF-36): II. psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Park JH, Kwon YC. Standardization of Korean of the minimental state examination (MMSE-K) for use in the elderly: Part II. diagnostic validity. J Korean Neuropsychiatr Assoc. 1989;28:508–513. [Google Scholar]
- 25.Kwon YC, Park JH. Korean version of mini-mental state examination (MMSE-K) J Korean Neuropsychiatr Assoc. 1989;28:125–135. [Google Scholar]
- 26.Noorani NH, Montagnini M. Recognizing depression in palliative care patients. J Palliat Med. 2007;10:458–464. doi: 10.1089/jpm.2006.0099. [DOI] [PubMed] [Google Scholar]
- 27.Ellis J, Lin J, Walsh A, Lo C, Shepherd FA, Moore M, et al. Predictors of referral for specialized psychosocial oncology care in patients with metastatic cancer: the contributions of age, distress, and marital status. J Clin Oncol. 2009;27:699–705. doi: 10.1200/JCO.2007.15.4864. [DOI] [PubMed] [Google Scholar]
- 28.Rao S, Ferris FD, Irwin SA. Ease of screening for depression and delirium in patients enrolled in inpatient hospice care. J Palliat Med. 2011;14:275–279. doi: 10.1089/jpm.2010.0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilkinson SM, Love SB, Westcombe AM, Gambles MA, Burgess CC, Cargill A, et al. Effectiveness of aromatherapy massage in the management of anxiety and depression in patients with cancer: a multicenter randomized controlled trial. J Clin Oncol. 2007;25:532–539. doi: 10.1200/JCO.2006.08.9987. [DOI] [PubMed] [Google Scholar]
- 30.Price DD, Verne GN, Schwartz JM. Plasticity in brain processing and modulation of pain. Prog Brain Res. 2006;157:333–352. doi: 10.1016/s0079-6123(06)57020-7. [DOI] [PubMed] [Google Scholar]
- 31.Turk DC, Sist TC, Okifuji A, Miner MF, Florio G, Harrison P, et al. Adaptation to metastatic cancer pain, regional/local cancer pain and non-cancer pain: role of psychological and behavioral factors. Pain. 1998;74:247–256. doi: 10.1016/s0304-3959(97)00187-5. [DOI] [PubMed] [Google Scholar]
- 32.Moriarty O, McGuire BE, Finn DP. The effect of pain on cognitive function: a review of clinical and preclinical research. Prog Neurobiol. 2011;93:385–404. doi: 10.1016/j.pneurobio.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 33.Oosterman JM, Derksen LC, van Wijck AJ, Veldhuijzen DS, Kessels RP. Memory functions in chronic pain: examining contributions of attention and age to test performance. Clin J Pain. 2011;27:70–75. doi: 10.1097/AJP.0b013e3181f15cf5. [DOI] [PubMed] [Google Scholar]
- 34.Povedano M, Gascon J, Galvez R, Ruiz M, Rejas J. Cognitive function impairment in patients with neuropathic pain under standard conditions of care. J Pain Symptom Manage. 2007;33:78–89. doi: 10.1016/j.jpainsymman.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 35.Weiner DK, Rudy TE, Morrow L, Slaboda J, Lieber S. The relationship between pain, neuropsychological performance, and physical function in community-dwelling older adults with chronic low back pain. Pain Med. 2006;7:60–70. doi: 10.1111/j.1526-4637.2006.00091.x. [DOI] [PubMed] [Google Scholar]
- 36.Meyer JS, Thornby J, Crawford K, Rauch GM. Reversible cognitive decline accompanies migraine and cluster headaches. Headache. 2000;40:638–646. doi: 10.1046/j.1526-4610.2000.040008638.x. [DOI] [PubMed] [Google Scholar]
- 37.Hede K. Chemobrain is real but may need new name. J Natl Cancer Inst. 2008;100:162–163. 169. doi: 10.1093/jnci/djn007. [DOI] [PubMed] [Google Scholar]
- 38.Ahles TA, Saykin AJ. Candidate mechanisms for chemotherapy-induced cognitive changes. Nat Rev Cancer. 2007;7:192–201. doi: 10.1038/nrc2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mystakidou K, Parpa E, Tsilika E, Pathiaki M, Gennatas K, Smyrniotis V, et al. The relationship of subjective sleep quality, pain, and quality of life in advanced cancer patients. Sleep. 2007;30:737–742. doi: 10.1093/sleep/30.6.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schultheis K, Hofheinz RD, Gencer D, Blunk JA, Benrath J. Quality of life and symptom evaluation in daily oncology practice: a survey of 150 patients with advanced gastrointestinal tumours receiving palliative chemotherapy. Onkologie. 2013;36:33–37. doi: 10.1159/000346670. [DOI] [PubMed] [Google Scholar]


