Abstract
Background:
A highly standardized screening test for newly diagnosis diabetes and pre-diabetes is necessary. the study goal was to clarify the power and efficacy of glycated hemoglobin (HbA1c) in the diagnosis of diabetes and pre-diabetes by comparing against the other American Diabetes Association (ADA) diagnostic criteria of fasting plasma glucose (FPG) and oral glucose tolerance test (OGTT).
Methods:
This is a retrospective study. A total of 27,001 individuals attended to the internal medicine outpatient clinic between 2006 and 2010 years were screened. All diabetic patients and those using drugs associated with the development of diabetes were excluded. The results of FPG, OGTT and HbA1c for 1814 individual were analyzed and all grouped as diabetic patients, glucose intolerant (pre-diabetes) patients and non-diabetic patients according to new ADA criteria for the diagnosis of diabetes.
Results:
The prevalence of newly diagnosed diabetes was 69.6% and 54% by using HbA1c alone, 64.2% and 28.2% with 2-h OGTT alone and 43.2% and 60.3%, respectively with FPG alone. Differences between FPG versus 2-h OGTT, FPG versus A1c and OGTT versus A1c were statistically significant (P < 0.0001, P < 0.0001 and P = 0.02, respectively). Diagnostic sensitivity of all diabetic criteria was 69.6% for A1c; Nearly, 64.2% for OGTT and only 43.1% for FPG respectively. In terms of diagnostic ratio of glucose intolerance; difference between HbA1C and OGTT was statistically significant (P < 0.0001).
Conclusions:
As a screening tool for newly diagnosed diabetes and pre-diabetes, the HbA1C level performed better than FPG and 2-h OGTT in this general Saudi population. High diagnostic power of A1C may contribute to the decrease in the number of undiagnosed patients.
Keywords: Diabetes mellitus, fasting plasma glucose, glycated haemoglobin, oral glucose tolerance test
INTRODUCTION
The international diabetes federation estimates that 285 million people have diabetes internationally,[1] with this number expected to rise to 438 million over the next 20 years, at a rate of a 7 million people annually.
The current criteria for the diagnosis of diabetes require a fasting plasma glucose (FPG) and 75-g oral glucose tolerance test (OGTT); a method that is time-consuming, requires fasting and effected by acute perturbations in glucose levels and short-term life-style changes.[2] Fasting and post-challenge blood glucose levels were found to predict the risk of diabetic retinopathy; so these tests have been the international standard for diagnosis.[3] FPG and OGTT are commonly used as criteria to identify subjects at risk of type 2 diabetes, whereas, many diabetic subjects may be far from matching these criteria. Therefore, many diabetic or pre-diabetic subjects remained undiagnosed and may have chronic complications of diabetes mellitus at the time of diagnosis.
Impaired fasting glucose (IFG) and impaired glucose tolerance (IGT) are currently used for diagnosis of high-risk glucose levels below the diabetic range. In addition, assigning a type of diabetes to an individual often depends on the circumstances present at the time of diagnosis and many diabetic individuals do not easily fit into a single class.[4]
In 2009, International Expert Committee proposed new diagnostic criteria based on glycated hemoglobin (HbA1c); with HbA1c ≥6.5% for diabetes and 6.0-6.4% for “high risk” of progression to diabetes.[5] Following this, The American Diabetes Association (ADA) proposed A1c ≥6.5% for the diagnosis of diabetes and 5.7-6.4% for the highest risk to progress to diabetes.[6] The proposed diagnostic threshold of 6.5% was based on retinopathy risk at different levels of HbA1c.[5]
HbA1c testing is highly standardized, exhibits low intra-individual variation, can be obtained at any time, require no patient preparation, and are relatively stable at room temperature after collection.[7] However, this new criteria's accuracy is controversial and has not yet been adopted internationally.[8]
In this study, we aimed to clarify the power and efficacy of HbA1c in the diagnosis of diabetes and pre-diabetes by comparing against the other ADA diagnostic criteria of FPG and OGTT.
METHODS
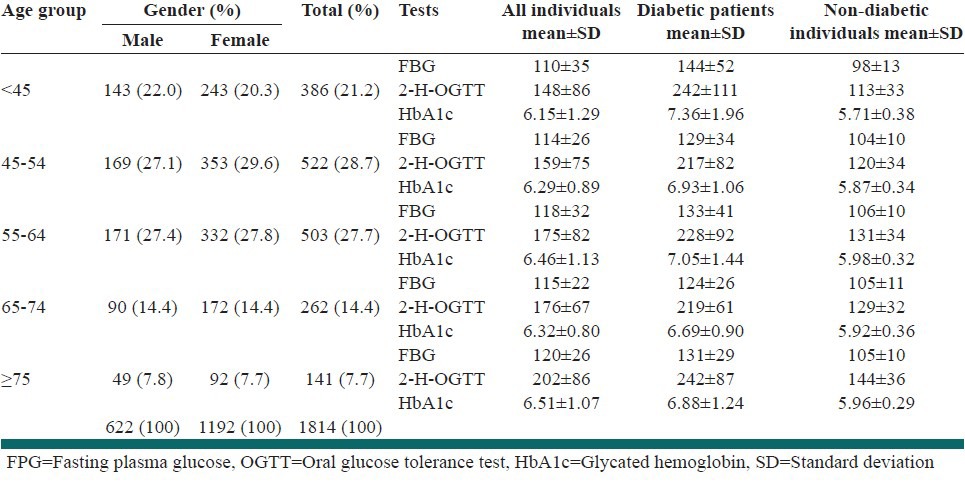
In this retrospective study, we screened 27,001 individuals attended to the internal medicine outpatient clinic for any problem between 2006 and 2010 years by the Nexusus (Hospital Information Administration System/Oracle Partner Network). Only those with concurrent FPG, OGTT and A1c results and diabetes mellitus suspicion were included. OGTT is routinely obtained in our hospital if there is a suspicion of diabetes mellitus. Diabetic subjects and patients who had been using drugs associated with the development of diabetes were excluded. After these exclusions, 1814 individuals remained. Finally, we evaluated all of the 1814 individuals with diabetes mellitus suspicion that attended to our outpatient clinic. The study group consisted of 622 males (34.3%) and 1192 females (65.7%). Mean age of the subjects was 54.3 ± 13.6 years (male 54.4 ± 13.6, female 54.2 ± 13.7) [Table 1].
Table 1.
Frequency of individuals and distribution of mean FPG, 2-h OGTT and HbA1c values of the diabetic patients and non-diabetic individuals according to age groups
FPG, OGTT, A1c levels of subjects were obtained Armed forces Hospital's patient database. All individuals subjects (n = 1814) were grouped as diabetic patients, glucose intolerant (pre-diabetes) patients and non-diabetic patients according to new ADA criteria for the diagnosis of diabetes. The current diagnostic criteria proposed by ADA for diabetes are: A1c ≥ 6.5%, FPG ≥ 126 mg/dl (7.0 mmol/l), 2nd h plasma glucose ≥200 mg/dl (11.1 mmol/l) during an OGTT an in a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, a random plasma glucose ≥ 200 mg/dl (11.1 mmol/l). IFG was defined as FPG with 100 mg/dl (5.6 mmol/l)-125 mg/dl (6.9 mmol/l). IGT was defined as 2-h glucose with 140 mg/dl (7.8 mmol/l)-199 mg/dl (11.0 mmol/l) or A1c values between 5.7% and 6.4%.
According to our hospital's biochemistry department's certified quality standards FPG, OGTT and A1c tests are performed with the following steps:
FPG: After 12 h fasting period, blood samples were drawn by standard phlebotomy into regular blood (serum) test-tubes between 08:00 and 10:00 AM and serum glucose level was measured by an enzymatic method (hexokinase).
OGTT: All subjects were informed to take at least 150 g of carbohydrate each day, for at least 3 days before this test. After 12 h fasting period, 75 g of glucose were given to each individual to ingest in the form of a cool drink. Blood samples were taken by standard phlebotomy into regular blood (serum) test tubes at time 0 and 120 min by a health-care provider.
HbA1C: Blood samples were obtained by standard phlebotomy into ethylenediaminetetraacetic acid-containing tubes following a 10 h fast concurrently with FPG. High performance liquid chromatography method (HPLC) was used in the analysis of HbA1c. The HbA1c result was calculated as a ratio to total hemoglobin by HPLC (A1C%).
Statistical analysis
All results were shown as mean ± standard deviation. P values were based on two-sided tests with a cut off for statistical significance of 0.05. The Chi-square test, The Kolmogorov-Smirnov test and analysis of covariance test were used to evaluate values. All statistical analyses were performed with The MedCalc Statistical Software Version 10.1.6.0 Licensed ti MedCalc Turkey 020931118117.
RESULTS
Diabetes
According to new ADA criteria; we determined 760 diabetic patients among 1814 individuals (41.8%). However, 190 diabetic patients (25.0%) met all ADA criteria. All results are shown in Tables 1 and 2. 529 diabetic patients (69.6%) were diagnosed by A1c alone, 488 diabetic patients (64.2%) with 2-h OGTT alone, and 328 (43.2%) diabetic patients were diagnosed with FPG alone [Table 2]. Differences between FPG versus 2-h OGTT, FPG versus A1c and OGTT versus A1c were statistically significant (P < 0.0001, P < 0.0001 and P = 0.02, respectively). Diagnostic sensitivity of all diabetic criteria was 69.6% for A1c; 64.2% for OGTT and only 43.1% for FPG respectively.
Table 2.
Prediabetes and diabetes frequencies
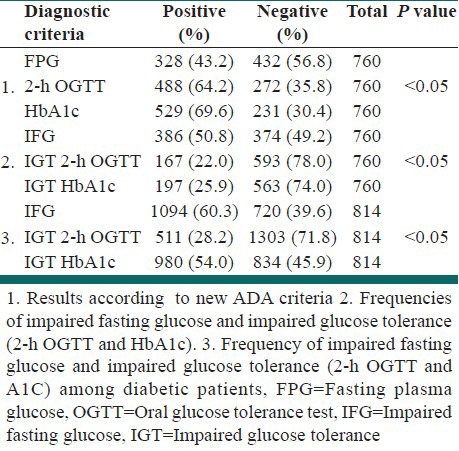
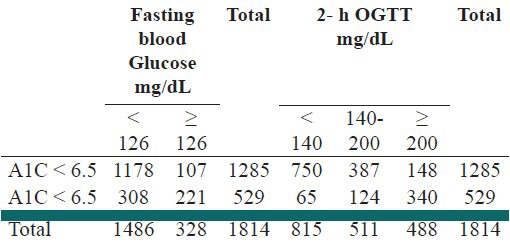
IFG and glucose intolerance: According to new ADA criteria, of the 1814 subjects tested, 1094 (60,3%) were classified as having IFG, 511 (28.2%) as having IGT following OGTT and 980 (54.0%) as having IGT by A1c. In terms of diagnostic ratio of glucose intolerance; difference between A1c and OGTT was statistically significant (P < 0.0001) [Tables 2 and 3].
Table 3.
Distribution of all diabetic patients according to FBG, 2-H OGTT and HbA1c
DISCUSSION
An international committee of diabetes experts has recommended that the Hemoglobin A1c assay, now routinely used to monitor the course of the disease in patients with diabetes and signals the pending development of diabetic complications; should become the new “gold standard” for diagnosing diabetes.[9] A1c assay is more convenient than OGTT because it has little inter-individual variation if there is not any hematologic disease and easy to use in daily routine practice because it does not need any fasting and diet preparation. Recently, World Health Organization experts have also accepted the use of A1c for diagnosing diabetes.[10] We determined 760 diabetic patients according to new proposed ADA criteria. On the other hand, if FPG and OGTT were used as the sole diagnostic tool, we would diagnose only 328 and 488 of the diabetic patients. According to these results, diagnostic power of A1c criterion is higher than FPG and 2-h OGTT. FPG and OGTT have a lower sensitivity, failing to diagnose 56.0% and 35.7% of the diabetic patients respectively. In only 190 patients, all ADA criteria were positive (25% of 760 diabetic patients).
IFG and IGT are significant predictors of pre-diabetes. It is considerably important to detect subjects in the pre-diabetic state for the purpose of taking preventative measures prior to the development of diabetic complications. According to our study, of the 1814 patients tested, 1094 (60.3%) were classified as having IFG, 511 (28.2%) as having IGT following OGTT and 980 (54.0%) as having IGT by A1c. Therefore, it is clear that the A1c criterion can result in a substantially lower prevalence of undiagnosed and total diabetes and being at high risk for diabetes than prevalence estimated from FPG or 2-h glucose.[7] Within our population, we would have missed the diagnosis of pre-diabetes in 469 (25.8%) patients if we had relied only on 2-h OGTT rather than A1c.
As mentioned above, accurate and time appropriate diagnosis of diabetes is imperative, since chronic complications of diabetes may be prevented or delayed by early diagnosis and effective treatment. We indicate that the use of FPG or OGTT alone in the diagnosis of diabetes lead to a large number false negatives, potentially resulting in a greater diabetic complication rate. The epidemic of diabetes is a serious and growing public health problem that results in reduced life expectancy and increased morbidity.[11] Despite significant advances in hyperglycemia treatment, blood glucose monitoring and markers of glycemic control, debilitating vascular complications develop in most diabetic patients.[12] Furthermore, the results of the advance and the action to control cardiovascular risk in diabetes (ACCORD) trials raise questions about whether extremely tight glucose control is beneficial in all diabetic patients with ACCORD finding that tight glucose control resulted in increased mortality in high risk type 2 diabetic patients.[13,14] However, the results of the United Kingdom Prospective Diabetes Study (UKPDS) were unable to show a significant effect of strict glycemic control on myocardial infarction.[15] A recent follow-up of the same study confirmed the utility of long-term hyperglycemic control in type 2 diabetes for preventing cardiovascular disease.[16] This apparent discrepancy between glycemic control and incidence and severity of diabetic complications has been termed as the “metabolic memory.”[17] Shown to be present in type 2 diabetes mellitus, metabolic memory is the concept that early glycemic environment is remembered in the target organs (i.e., eye, kidney, heart, extremities). Follow-up data from the UKPDS have shown that type 2 diabetic patients, like type 1 diabetic patients in the diabetes control and complications trial/epidemiology of diabetes interventions and complications, who were on the standard treatment regimen during the study still have a higher incidence of micro-vascular and cardiovascular complications compared with their counterparts receiving intensive therapy throughout the trial and the follow-up period.[16] This suggests that early metabolic control has enduring beneficial effects also in type 2 diabetes. We can say that recognition and effective treatment of at the earliest opportunity is paramount in preventing complications. We can speculate that high diagnostic power of A1c can lead to a decrease in undiagnosed patients and early detection of diabetes that may result in fewer long term diabetic complications.
CONCLUSIONS
Using A1c as the diabetes criterion would reclassify the diabetes diagnosis of nearly 50 million Americans. It is imperative that clinicians and health systems understand the differences and similarities in using A1c or FPG and 2-h OGTT in diagnosis of diabetes mellitus and pre-diabetes.
The proposed A1c diagnostic criteria have greater diagnostic than FPG and 2-h OGTT regarding diagnosis of diabetes mellitus.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Groop LC, Bonadonna RC, DelPrato S, Ratheiser K, Zyck K, Ferrannini E, et al. Glucose and free fatty acid metabolism in non-insulin-dependent diabetes mellitus. Evidence for multiple sites of insulin resistance. J Clin Invest. 1989;84:205–13. doi: 10.1172/JCI114142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2009;32(Suppl 1):S62–7. doi: 10.2337/dc09-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Uldry M, Thorens B. The SLC2 family of facilitated hexose and polyol transporters. Pflugers Arch. 2004;447:480–9. doi: 10.1007/s00424-003-1085-0. [DOI] [PubMed] [Google Scholar]
- 4.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 1997;20:1183–97. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- 5.International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009;32:1327–34. doi: 10.2337/dc09-9033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–9. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cowie CC, Rust KF, Byrd-Holt DD, Gregg EW, Ford ES, Geiss LS, et al. Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988-2006. Diabetes Care. 2010;33:562–8. doi: 10.2337/dc09-1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kilpatrick ES, Bloomgarden ZT, Zimmet PZ. Is haemoglobin A1c a step forward for diagnosing diabetes? BMJ. 2009;339:b4432. doi: 10.1136/bmj.b4432. [DOI] [PubMed] [Google Scholar]
- 9.Mitchell D. Diabetes experts recommend A1C testing for diabetes diagnosis “Switch Would Eliminate Need for Pretest Fasting” American academy of family physicians news. 2009. [Last accessed 2012 Dec 01]. Available from: http://www.aafp.org/online/en/home/publications/news/news-now/clinical-care-research/20090624A1C-diab-dx.html .
- 10.World Health Organization. Use of Glycated Haemoglobin (HbA1C) in the diagnosis of diabetes mellitus abbreviated report of a WHO consultation. 2011 [PubMed] [Google Scholar]
- 11.Colagiuri S, Cull CA, Holman RR UKPDS Group. Are lower fasting plasma glucose levels at diagnosis of type 2 diabetes associated with improved outcomes?: U.K. prospective diabetes study 61. Diabetes Care. 2002;25:1410–7. doi: 10.2337/diacare.25.8.1410. [DOI] [PubMed] [Google Scholar]
- 12.Ceriello A, Ihnat MA, Thorpe JE. Clinical review 2: The “metabolic memory”: Is more than just tight glucose control necessary to prevent diabetic complications? J Clin Endocrinol Metab. 2009;94:410–5. doi: 10.1210/jc.2008-1824. [DOI] [PubMed] [Google Scholar]
- 13.ADVANCE Collaborative Group. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560–72. doi: 10.1056/NEJMoa0802987. [DOI] [PubMed] [Google Scholar]
- 14.Gerstein HC, Miller ME, Byington RP, Goff DC, Jr, Bigger JT, et al. Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545–59. doi: 10.1056/NEJMoa0802743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 16.Holman RR, Paul SK, Bethel MA, Neil HA, Matthews DR. Long-term follow-up after tight control of blood pressure in type 2 diabetes. N Engl J Med. 2008;359:1565–76. doi: 10.1056/NEJMoa0806359. [DOI] [PubMed] [Google Scholar]
- 17.Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643–53. doi: 10.1056/NEJMoa052187. [DOI] [PMC free article] [PubMed] [Google Scholar]


