Abstract
Background
A well-established body of literature demonstrates concurrent associations between personality traits and major depressive disorder (MDD), but there have been relatively fewer investigations of their dynamic interplay over time.
Methods
Prospective interrelationships between late adolescent personality and MDD in early adulthood were examined in a community sample of male and female twins from the Minnesota Twin Family Study (N = 1252). Participants were classified into naturally occurring MDD groups based on the timing (adolescent- versus adult-onset) and course (chronic/recurrent versus remitting) of MDD. MDD diagnoses were assessed at ages 17, 20, 24, and 29, and personality traits (Negative Emotionality [NEM], Positive Emotionality [PEM], Constraint [CON]) were assessed at ages 17, 24, and 29.
Results
Multilevel modeling analyses indicated that higher age-17 NEM was associated with the subsequent development of MDD, and any MDD, regardless of onset or course, was associated with higher NEM through age 29. Moreover, the chronic/recurrent MDD groups failed to show the normative decrease in NEM from late adolescence to early adulthood. Lower age-17 PEM was also associated with the subsequent development of MDD, but only among the chronic/recurrent MDD groups. Finally, the adolescent-onset MDD groups reported lower age-17 CON relative to the never depressed and adult-onset MDD groups.
Conclusions
Taken together, results speak to the role of personality traits for conferring risk for the onset of MDD in late adolescence and early adulthood, as well as the pernicious implications of chronic/recurrent MDD, particularly when it onsets during adolescence, for adaptive personality development.
Keywords: Major depressive disorder, personality traits, personality-depression models, recurrence, adolescence
Depressive disorders are a major public health concern (see Kessler, 2012; Sartorius, 2001; Üstün et al., 2004). Major depressive disorder (MDD) is among the most frequently occurring psychiatric disorders (16.6% lifetime prevalence; Kessler et al., 2005), and has tremendous negative implications for functioning and quality of life, including concurrent and prospective associations with impaired interpersonal relationships, academic and occupational functioning, and physical health (Kessler, 2012). Given its pervasive and deleterious consequences, extensive research has sought to identify factors that confer risk for developing MDD or influence its course and severity (see Burcusa & Iacono, 2007). One particularly promising approach has been investigation of associations between individual differences in personality and MDD (see Clark, 2005; Tackett, 2006). In the present study, we examined prospectively interrelationships between late adolescent personality and MDD in early adulthood, and considered whether personality trait trajectories during this period differed as a function of the timing (adolescent- versus adult-onset) and course (chronic/recurrent versus remitting) of MDD.
Interrelationships Between Personality Traits and MDD
A well-established literature demonstrates links between personality traits and psychiatric disorders among adults (see Kotov et al., 2010). Negative Emotionality/Neuroticism (NEM; a tendency to experience negative mood states) is implicated as a nonspecific personality trait that confers general vulnerability for psychopathology, while (low) Positive Emotionality/Extraversion (PEM; a tendency to experience positive mood states) is posited to be specifically associated with MDD (Clark & Watson, 1991). Studies demonstrate concurrent associations between high NEM and low PEM and depressive symptoms among children (Brown et al., 1998; Joiner & Lonigen, 2000; Lonigan et al., 1999) and adolescents (Lonigan et al., 1999; Wetter & Hankin, 2009), and depressive symptoms and MDD diagnosis among adults (De Fruyt et al., 2006; Kotov et al. 2010; Watson et al., 2005). Although less frequently considered, there is also some evidence that (low) Constraint/Conscientiousness (CON; a tendency to inhibit impulsive, risky behavior) is concurrently associated with depressive symptoms among children (John et al., 1994) and MDD diagnosis among adults (Kotov et al., 2010).
Models of personality-depression associations
Although there is evidence that personality traits are concurrently associated with depressive symptoms and disorders, determining the interplay of personality traits and MDD, and particularly their causal relationships over time, can be complex (see Klein et al., 2011). Prospective studies of personality-depression associations have focused predominantly on NEM and PEM. Results consistently indicate that higher NEM predicts MDD, consistent with a vulnerability model in which personality traits confer risk for the development of MDD. In contrast, results have been less straightforward for PEM, with mixed evidence that PEM acts as a vulnerability factor for MDD. On the other hand, there is evidence that PEM is associated with the course and severity of MDD, consistent with a pathoplasty model in which personality traits are associated with MDD presentation or outcome. Notably, the vast majority of studies on personality-depression associations have been conducted with adults. Although several prospective studies provide evidence that higher NEM and lower PEM predict sub-threshold depressive symptoms during childhood and adolescence (Lonigen et al., 2003; Wetter & Hankin, 2009; but see also Joiner & Lonigan, 2000), to our knowledge, no prospective studies with younger samples have considered MDD diagnoses, nor personality-MDD associations during adolescence and the transition to adulthood.
The lack of prospective studies with adolescents is unfortunate because this is likely a particularly informative period for investigations of personality-depression associations. Adolescence is a time of rapid change, increasing independence, and emerging responsibilities. The vast majority of adolescents makes the transition into adulthood smoothly, but an important subset fails to master the developmental milestones of this period. Many cases of MDD onset during adolescence (Costello et al., 2003; Kessler et al., 2005). Given evidence that the timing of MDD onset may be related to its severity and course (Hammen et al., 2008; Weissman et al., 1999), studies of first-onsets of MDD among adults may include less severe cases, and thus report attenuated estimates of personality-depression associations. Moreover, because personality traits become increasingly stable with age (Blonigen et al., 2008; Roberts & DelVecchio, 2000), studies with adults may capture already established personality-depression patterns, whereas studies with younger samples may be better suited to examining the dynamic influences of personality and MDD over time.
Continuity and change in personality traits
Although there is evidence of rank-order consistency in personality traits over time (Roberts & DelVecchio, 2000), there is also evidence of normative developmental changes during adolescence and adulthood (Roberts et al., 2006). On average, NEM decreases, while CON increases (“the maturity principle;” Caspi et al., 2005). However, a significant minority does not evidence this normative, adaptive developmental change, or instead evidences maladaptive change (Blonigen et al., 2008). Developmentally salient events, including a major depressive episode, may be particularly influential for personality trajectories during earlier developmental periods, when personality traits show greater variability (Roberts & DelVecchio, 2000), making adolescence an optimal period for prospective investigations of associations between personality traits and MDD.
Present Study
We examined prospectively interrelationships between personality and the onset and course of MDD during the transition from adolescence to adulthood in a large, community sample. Specifically, we examined whether NEM, PEM, and CON were associated with the timing (adolescent- versus adult-onset) and course (chronic/recurrent versus remitting) of MDD, and whether the timing and course of MDD were associated with differing trajectories of NEM, PEM, and CON from ages 17 to 29. We defined five naturally occurring groups based on the trajectories of MDD diagnoses from adolescence to early adulthood: MDD onset during (a) adolescence (by age 17) or (b) early adulthood (between ages 18 and 24) that either (c) remitted by or (d) persisted to age 29, and (e) no MDD through age 29. We addressed the following questions: Are personality traits differentially associated with MDD that onsets during adolescence versus early adulthood? Are personality traits differentially associated with MDD that evidences a chronic/recurring versus remitting course? And, are these naturally occurring MDD groups differentially associated with personality trait trajectories over time? Evidence that personality traits are associated with the subsequent development of MDD would lend support to the vulnerability model, while evidence that personality traits are associated with different courses of MDD would lend support to the pathoplasty model. Evidence that MDD is associated with differing trajectories of personality traits would suggest that the experience of MDD has implications for normative personality development during the transition from adolescence to adulthood. By considering whether MDD groups defined by onset and course were distinguishable from one another in terms of personality trait trajectories, we sought to identify premorbid personality risk factors, as well as characterize personality outcomes for individuals with differing MDD trajectories.
Method
Participants and Procedures
Participants were same-sex male and female twins from the Minnesota Twin Family Study (MTFS) (54% female). The MTFS is an ongoing community-based, longitudinal study of reared-together twins and their parents; the study design and sample, including inclusion and exclusion criteria, have been described extensively elsewhere (see Iacono & McGue, 2002; Iacono et al., 2006) and are only briefly reviewed here. The present study included a cohort of twins first recruited for participation at age 17. Consistent with the demographic makeup of Minnesota during the targeted birth years, families were predominately Caucasian (98%). The MTFS design includes assessments at target ages of 17 (M = 17.48, SD = 0.46), 20 (M = 20.67, SD = 0.57), 24 (M = 24.70, SD = 0.97), and 29 years (M = 29.62, SD = 0.61). Diagnostic data were collected at the age-17 (n = 1252), −20 (n = 1105), −24 (n = 1108), and −29 (n = 1168) assessments; 1051 participants (84%) had diagnostic data at all four assessments. Personality data were collected at the age-17 (n = 1111), −24 (n = 1013), and −29 (n = 1093) assessments; 842 participants (67%) had personality data at all three assessments. Chi-squared tests indicated that participants with MDD at age 17 were no less likely to provide personality data at intake or follow-up assessments (all ps > .05). Participants with MDD at age 17 were less likely to provide diagnostic data at age 20, χ2(1) = 7.16, p = .007; 96% without MDD provided diagnostic data at age 20, whereas 91% with MDD did. However, participants with MDD at age 17 were not less likely to provide diagnostic data at age 24, χ2(1) = 2.12, p = .145, meaning that missing age-20 diagnostic data were largely obtained at the age-24 assessment. Participants with MDD at age 17 were less likely to provide diagnostic data at age 29, χ2(1) = 3.87, p = .049; 90% without MDD provided diagnostic data at age 29, whereas 84% with MDD did, indicating only a small difference based on age-17 MDD status and suggesting that attrition effects were at most minimal.
Measures
MDD
MDD diagnoses and information on the onset and course of MDD symptoms were assessed at age 17 in semi-structured interviews with participants’ mothers using the Diagnostic Interview for Children and Adolescents—Revised (DICA-R; Reich & Welner, 1988) and with participants using the Structured Clinical Interview for DSM-III-R (SCID; Spitzer et al., 1987). A best-estimate procedure was used to assign age-17 diagnoses if symptoms were endorsed by either mother or participant. MDD diagnoses were assessed at ages 20, 24, and 29 with participants using the SCID. MDD diagnoses were based on DSM-III-R criteria in order to maintain continuity with the diagnostic system used at intake. Lifetime MDD symptoms were assessed at the age-17 assessment and MDD symptoms experienced at any time during the interval since the prior assessment were assessed at the age−20, −24, and −29 assessments. Diagnostic interviews were conducted by interviewers who had received extensive training in psychiatric interviewing, and who held a bachelor’s or master’s degree in psychology or a related discipline. All interviews were reviewed in case conferences, and consensus was required prior to assigning each symptom. Computer algorithms were used to assign diagnoses. Interrater reliability was assessed on a randomly selected subsample of 600 MTFS participants (kappa = .81 for MDD). MDD diagnoses were assigned if criteria were met at a “definite” (i.e., 5 or more DSM-III-R criteria met) or “probable” (i.e., 4 or more DSM-III-R criteria met) level using Research Diagnostic Criteria (Spitzer et al., 1978) guidelines that allow for the fact that most participants were not symptomatic at the time of the diagnostic assessment, meaning that they relied on memory when reporting past symptoms1. The cumulative lifetime prevalence of MDD (definite and probable cases) in the present sample was 13% at age 17, 21% at age 20, 28% at age 24, and 33% at age 29.
In order to examine effects of MDD onset and course, participants were classified into 1 of 5 naturally occurring, mutually exclusive MDD groups. The never depressed group (n = 726; 72%) did not meet criteria for MDD at any assessment point. The adolescent-onset, remitting group (n = 91; 9%) met lifetime criteria for MDD at age 17, but did not meet criteria at the age-29 assessment; 14 (15%) and 13 (14%) participants met criteria at the age-20 and/or age-24 assessments, respectively. The adolescent-onset, chronic/recurrent group (n = 49; 5%) met lifetime criteria for MDD at age 17 and at the age-29 assessment; 23 (47%) and 26 (53%) participants also met criteria at the age-20 and/or age-24 assessments, respectively. The adult-onset, remitting group (n = 99; 10%) met criteria for MDD at the age-20 (n = 49; 50%) and/or age-24 (n = 59; 60%) assessments, but did not meet criteria at the age-29 assessment. The adult-onset, chronic/recurrent group (n = 48; 5%) met criteria for MDD at the age-20 (n = 27; 56%) and/or age-24 (n = 34; 71%) assessments, and also met criteria at the age-29 assessment. A total of 1013 (81%) participants were classified into MDD groups; 239 participants were excluded from subsequent analyses because they could not be classified due to one or more missing assessments. Independent-samples t-tests indicated that participants who were not assigned to an MDD group reported higher age-24 CON, t(1011) = 2.49, p = .013, and age-29 NEM, t(1091) = 2.95, p = .003.
Personality
Participants reported on their personality traits at ages 17, 24, and 29 using the 198-item version of the Multidimensional Personality Questionnaire (MPQ; Tellegen, 2006). The MPQ includes NEM, PEM, and CON scales, which have demonstrated good criterion and convergent validity, and high internal consistency in the present sample and others (Hopwood et al., 2011; Tellegen, 2006).
Statistical Analysis
We conducted multilevel modeling (MLM) analyses that accounted for the repeated measures and nested nature of the data to examine whether personality traits were associated with the timing and course of MDD, and whether the timing and course of MDD was associated with differing personality trait trajectories. Specifically, we conducted three-level multilevel models comprised of time-varying variables (personality traits assessed at ages 17, 24, and 29) at level-1, nested within individual participants at level-2, nested within families at level-3. First, we fit a series of group trajectory models to estimate effects of age at level-1 for each personality trait, separately for each of the MDD groups. We used age in years as the unit of time to account for variation in age at each assessment. Age was centered at age 17 so that the intercept of each model reflects the age-17 level of the personality trait and the slope represents change from ages 17 to 29. These models quantify personality trait trajectories for each of the MDD groups. Next, we fit a series of group comparison models that explicitly tested whether personality trait trajectories differed among the MDD groups by adding simultaneously dummy coded variables representing each MDD group to the intercept and slope parameters at level-2 (a cross-level interaction between MDD group and age); we systematically compared each of the MDD groups by recoding the reference group. Effects at the intercept speak to whether personality traits at age 17 differ between the MDD group and the reference group, and effects at the slope speaks to whether the rates of change from ages 17 to 29 differ. We included participant sex as a covariate by adding a dummy term to the intercept and slope parameters at level-22. In each model, the variance component for the level-1 intercept was allowed to vary randomly across participants; variance components for all other parameters were fixed. All analyses were conducted with Scientific Software International’s HLM 6.04 (Raudenbush et al., 2004) using full maximum likelihood estimation.
Results
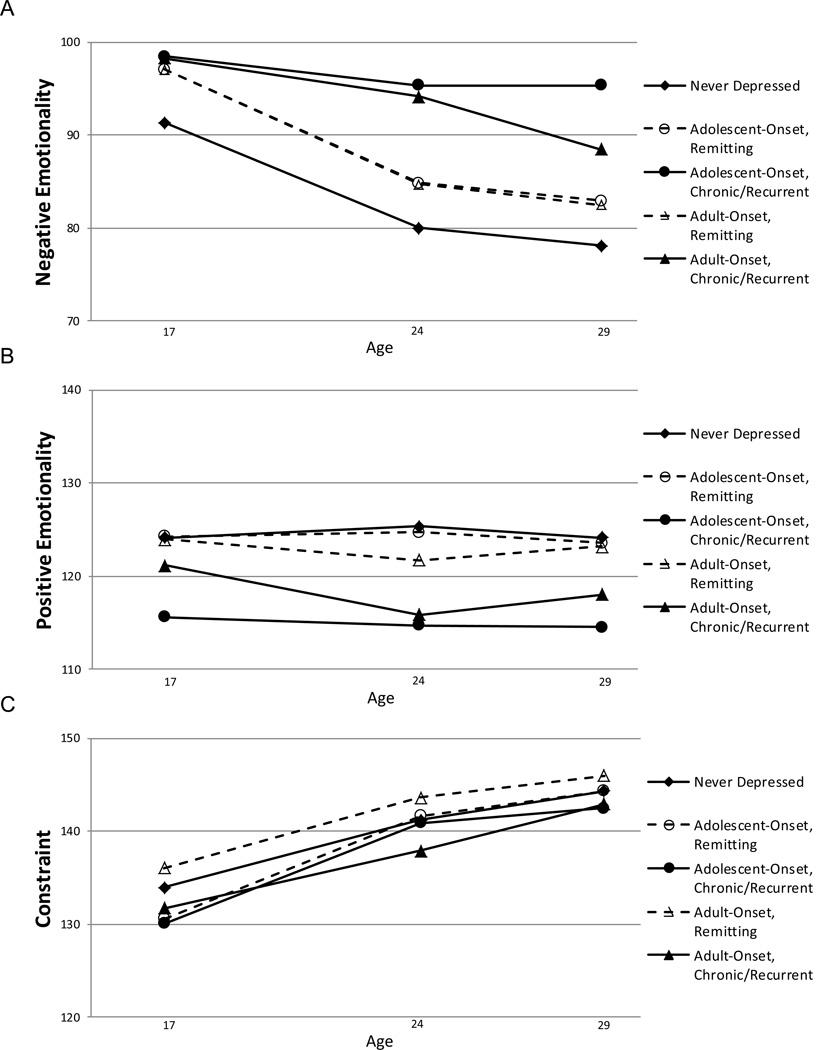
Means and standard deviations for personality traits at each age and by MDD group status are presented in Table 1, and mean-level personality trait trajectories for each MDD group are depicted in Figure 1. MLM analyses were used to (1) model personality trait trajectories from ages 17 to 29 for each MDD group and (2) explicitly test whether the MDD groups differed in their trajectories. Results of MLM analyses are summarized in Table 2.
Table 1.
Descriptive Statistics for Personality Traits at Ages 17, 24, and 29 Among MDD Groups
| MDD Group |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Personality Trait |
Age | n | Never Depressed |
n | Adolescent-Onset, Remitting |
n | Adolescent-Onset, Chronic/Recurrent |
n | Adult-Onset, Remitting |
n | Adult-Onset, Chronic/Recurrent |
| 17 | 648 | 91.33 (12.75) | 83 | 97.08 (12.66) | 42 | 98.50 (14.81) | 91 | 97.10 (14.31) | 45 | 98.29 (15.72) | |
| NEM | 24 | 620 | 79.98 (12.78) | 75 | 84.84 (12.44) | 42 | 95.38 (15.69) | 86 | 84.74 (13.25) | 43 | 94.17 (17.17) |
| 29 | 696 | 78.07 (12.60) | 90 | 82.90 (12.43) | 46 | 95.39 (14.15) | 96 | 82.48 (13.69) | 46 | 88.47 (13.52) | |
| 17 | 648 | 124.16 (13.08) | 83 | 124.29 (14.10) | 42 | 115.62 (18.64) | 91 | 123.96 (15.15) | 45 | 121.16 (12.27) | |
| PEM | 24 | 620 | 125.37 (12.75) | 75 | 124.71 (12.19) | 42 | 114.69 (14.77) | 86 | 121.71 (13.51) | 43 | 115.87 (14.22) |
| 29 | 696 | 124.17 (12.95) | 90 | 123.54 (12.41) | 46 | 114.50 (14.39) | 96 | 123.16 (12.37) | 46 | 118.05 (15.70) | |
| 17 | 648 | 133.92 (15.39) | 83 | 130.60 (19.78) | 42 | 130.07 (19.89) | 91 | 136.03 (16.86) | 45 | 131.71 (17.33) | |
| CON | 24 | 620 | 141.21 (15.47) | 75 | 141.64 (17.29) | 42 | 140.87 (15.01) | 86 | 143.63 (14.74) | 43 | 137.87 (17.86) |
| 29 | 696 | 144.33 (15.36) | 90 | 144.31 (15.40) | 46 | 142.48 (17.60) | 96 | 145.98 (16.32) | 46 | 142.92 (14.96) | |
Note. Mean (standard deviation). MDD = Major Depressive Disorder. NEM = Negative Emotionality. PEM = Positive Emotionality.
CON = Constraint.
Figure 1.
Mean levels of personality traits by MDD group at ages 17, 24, and 29 years. A: Negative Positive Emotionality. C: Constraint.
Table 2.
Summary of Results of MLM Analyses for Personality Trait Trajectories
| NEM |
PEM |
CON |
||||
|---|---|---|---|---|---|---|
| Intercept (age 17) |
Slope (change from age 17 to 29) |
Intercept (age 17) |
Slope (change from age 17 to 29) |
Intercept (age 17) |
Slope (change from age 17 to 29) |
|
| Model | Coef (SE) | Coef (SE) |
Coef (SE) | Coef (SE) |
Coef (SE) | Coef (SE) |
| Group trajectories | ||||||
| Never depressed | 89.58 (.76)*** | −1.19 (.06)*** | 124.33 (.88)*** | −.06 (.06) | 137.83 (.95)*** | .96 (.08)*** |
| Adolescent-onset, remitting | 97.65 (1.81)*** | −1.44 (.15)*** | 122.29 (1.75)*** | −.07 (.16) | 133.91 (2.63)*** | 1.28 (.21)*** |
| Adolescent-onset, chronic/recurrent | 97.60 (2.70)*** | −.40 (.22) | 113.57 (3.07)*** | −.07 (.23) | 130.08 (3.30)*** | 1.06 (.24)*** |
| Adult-onset, remitting | 97.65 (2.16)*** | −1.38 (.13)*** | 123.25 (2.52)*** | −.17 (.20) | 139.95 (2.38)*** | .86 (.19)*** |
| Adult-onset, chronic/recurrent | 99.12 (3.16)*** | −.90 (.21)*** | 119.07 (2.00)*** | −.52 (.24)* | 135.48 (2.74)*** | .92 (.25)*** |
| Group comparisons | ||||||
| Never versus adol remit | 5.22 (1.44)*** | −.05 (.12) | .42 (1.41) | −.04 (.13) | −4.08 (2.03)* | .26 (.17) |
| Never versus adol chron/rec | 5.85 (2.49)* | .83 (.21)*** | −8.04 (2.67)** | −.08 (.21) | −7.24 (2.96)* | .16 (.24) |
| Never versus adult remit | 5.74 (1.45)*** | −.11 (.11) | −.11 (1.60) | −.03 (.14) | .64 (1.76) | −.03 (.14) |
| Never versus adult chron/rec | 8.35 (2.21)*** | .35 (.18)* | −4.10 (1.84)* | −.21 (.18) | −3.49 (2.71) | −.03 (.20) |
| Adol remit versus adol chron/rec | .63 (2.90) | .88 (.23)*** | −8.46 (2.89)** | −.04 (.23) | −3.16 (3.36) | −.10 (.27) |
| Adol remit versus adult chron/rec | 3.13 (2.55) | .40 (.21)† | −4.51 (2.18)* | −.18 (.21) | .60 (3.28) | −.29 (.25) |
| Adult remit versus adol remit | −.52 (1.93) | .07 (.15) | .52 (1.95) | −.01 (.18) | −4.72 (2.50) | .29 (.20) |
| Adult remit versus adol chron/rec | .11 (2.79) | .94 (.22)*** | −7.93 (3.14)* | −.05 (.24) | −7.88 (3.22)* | .19 (.26) |
| Adult remit versus adult chron/rec | 2.60 (2.47) | .46 (.20)* | −3.99 (2.40) | −.18 (.22) | −4.12 (3.16) | .00 (.24) |
| Adult chron/rec versus adol chron/rec | −2.50 (3.21) | .48 (.26) | −3.94 (3.05) | .13 (.26) | −3.75 (3.87) | .19 (.29) |
Note. Group trajectory models quantify personality trait trajectories for each MDD group; in these models, the intercept indicates the average personality trait score for each group at age 17, and the slope indicates the change in the personality trait score per year, with significant values indicating that the age-17 score differs significantly from zero (intercept) or changes significantly from ages 17 to 29 (slope). Group comparison models test whether the groups in the comparison differ; these models include dummy coded variables representing each MDD group entered simultaneously and recoding the reference group in order to systematically compare each group, with positive values indicating that the age-17 score for the second group is significantly larger than that for the first group (intercept) or changes at a significantly faster (when the overall trajectory is positive) or slower (when the overall trajectory is negative) rate from ages 17 to 29 (slope). All models include participant sex as a covariate. NEM = Negative Emotionality. PEM = Positive Emotionality. CON = Constraint. Coef = coefficient. SE = standard error.
All results for analyses including definite and probable MDD cases were comparable to those including only definite cases with the single noted exception, which was significant when only definite cases were included.
p < .05.
p < .01.
p < .001.
NEM
MLM analyses quantify the trajectories of NEM over time for each group depicted in Figure 1A, as well as differences in these trajectories; a summary of MLM results for NEM trajectories for each group is presented in the upper portion of Table 2, and for comparisons between groups in the lower portion. MLM results for NEM trajectories for each group map onto the trajectories shown in Figure 1A; the significant positive coefficients for the intercepts of these models indicate that age-17 NEM for each group differed significantly from zero, and the negative coefficients for the slopes indicate that all of the groups evidenced normative decreases in NEM from ages 17 to 29 except the adolescent-onset, chronic/recurrent group, which showed no changes in NEM over time. Results for comparisons between groups indicated significant differences in age-17 levels and trajectories of NEM. The significant positive coefficients for the intercepts of comparisons for all MDD groups with the never depressed group indicate that age-17 NEM was significantly higher for groups that experienced any MDD, regardless of timing or course; in contrast, the nonsignificant coefficients for the intercepts of comparisons of MDD groups with one another indicate that none of the MDD groups differed significantly in age-17 NEM. This pattern of results clearly supports the vulnerability model in that even groups that were free of MDD at age 17 but who subsequently developed MDD in adulthood reported higher NEM at age 17. Moreover, because NEM showed an overall decreasing trajectory over time, the significant positive coefficients for the slopes of comparisons between the chronic/recurrent groups and the never depressed and remitting groups indicate that the adult-onset, chronic/recurrent group showed a more modest decrease in NEM from ages 17 to 29, while the adolescent-onset, chronic/recurrent group failed to show any decrease in NEM over time. Taken together, results support the vulnerability model in indicating that higher NEM is associated with the subsequent development of MDD, regardless of whether onset is during adolescence or early adulthood. Moreover, although any MDD, regardless of timing and course, is associated with higher NEM, results also suggest that MDD that follows a chronic/recurrent course has particularly pernicious implications in its disruption of the normative decreases in NEM from late adolescence to early adulthood.
PEM
A summary of MLM results for PEM trajectories for each group are presented in the upper portion of Table 2, and for comparisons between groups in the lower portion. Consistent with the trajectories in Figure 1B, the significant positive coefficients for the intercepts of the group trajectory models indicate that age-17 PEM for each group differed significantly from zero, and the nonsignificant coefficients for the slopes indicate that PEM remained stable from ages 17 to 29 for all groups except the adult-onset, chronic/recurrent group, which showed decreases in PEM from ages 17 to 29. Results for comparisons between groups indicated significant differences in age-17 levels of PEM. The significant negative coefficients for the intercepts of comparisons between the chronic/recurrent groups with the never depressed and remitting groups indicate that age-17 PEM was significantly lower for groups with chronic/recurrent MDD. The nonsignificant coefficients for the slopes of all comparisons between groups indicate that no groups differed in their PEM trajectories, though PEM was consistently lower in the chronic/recurrent groups. Taken together, results offer some support for the vulnerability model in indicating that lower PEM is associated with the subsequent development of MDD in early adulthood, but only for chronic/recurrent MDD. Moreover, results support the pathoplasty model in that lower PEM is specific to MDD that follows a chronic/recurrent course; in fact, the remitting group showed levels of PEM comparable to the never depressed group.
CON
A summary of MLM results for CON trajectories for each group are presented in the upper portion of Table 2, and for comparisons between groups in the lower portion. The significant positive coefficients for the intercepts of the group trajectory models indicate that age-17 CON for each group differed significantly from zero, and the positive coefficients for the slopes indicate that all of the groups evidenced normative increases in CON from ages 17 to 29, as depicted in Figure 1C. Results for comparisons between groups indicated significant differences in age-17 levels of CON for the adolescent-onset groups. The significant negative coefficients for the intercepts of comparisons between the adolescent-onset groups with the never depressed and adult-onset, remitting groups indicate that age-17 CON was significantly lower for groups with adolescent-onset MDD. The nonsignificant coefficients for the slopes of all comparisons between groups indicate that no groups differed in their CON trajectories; CON showed normative increases from ages 17 to 29 for all groups. Taken together, results suggest that MDD is associated with lower CON, but only MDD that onsets during adolescence. There was no evidence that CON was associated with the subsequent development of MDD, nor with the course of MDD. Moreover, there was no evidence that MDD, regardless of whether it onset during adolescence or adulthood, or followed a remitting or chronic/recurrent course, had implications for the normative development of CON from adolescence to early adulthood.
Discussion
Extensive research has investigated links between personality traits and psychiatric disorders. NEM has emerged as a key nonspecific risk factor for psychiatric disorders, including MDD (Kotov et al., 2010). In contrast, although implicated in theoretical models as a risk factor specific to MDD (Clark & Watson, 1991), (low) PEM has received less consistent empirical support, while CON has been only rarely considered. The field has been increasingly moving beyond simple examination of concurrent links between personality traits and depressive disorders to prospective studies and experimental designs that consider the dynamic interplay of these constructs over time (see Klein et al., 2011). The present study makes an important contribution to the existing literature by examining prospectively associations between NEM, PEM, and CON and the timing and course of MDD during a key developmental period, the transition from late adolescence to early adulthood. In general, the adolescents in our sample evidenced decreasing NEM and increasing CON as they transitioned into adulthood, consistent with maturational growth processes marked by adaptive response to the developmental tasks that characterize this period. However, MDD was associated with important differences in developmental trajectories of personality traits that were further differentiated by whether MDD onset during adolescence or adulthood, and followed a chronic/recurrent or remitting course.
Consistent with previous research in samples of children, adolescents, and adults (see Klein et al., 2011; Tackett, 2006), results of the present study demonstrate that any MDD, regardless of timing or course, was associated with higher NEM. Moreover, consistent with the vulnerability model, higher NEM was associated with the subsequent development of MDD. Results for PEM were more nuanced. There was some support for the vulnerability model, in that PEM was associated with the subsequent development of MDD, but only MDD that followed a chronic/recurrent course. Consistent with the pathoplasty model, lower PEM was associated with chronic/recurrent, but not remitting, MDD. Adolescent-onset MDD was associated with lower CON. Taken together, results clearly speak to the pernicious implications of chronic/recurrent MDD, particularly when it onsets during adolescence. At age 17, the adolescent-onset, chronic/recurrent group was characterized by high NEM, low PEM, and low CON. Moreover, because the adolescent-onset, chronic/recurrent group failed to show the normative decrease in NEM from ages 17 to 29 evidenced by all other groups, this group continued to report high levels of NEM and low levels of PEM through age 29. The present study adds to a relatively small but important body of literature on the implications of adolescent-onset MDD for subsequent functioning (Hammen et al., 2008; Weissman et al., 1999). Notably, although results are consistent with evidence of the deleterious outcomes of adolescent-onset MDD, they also suggest these may be a function less of its early onset, per se, than of its associated increased incidence of severe, chronic, and recurrent MDD into adulthood (Hammen et al., 2008; Rohde et al., 2013; Weissman et al., 1999). That the adolescent-onset and adult-onset chronic/recurrent groups generally differed from the never depressed and remitting groups but did not differ from one another is consistent with evidence that recurrent MDD is prospectively associated with psychosocial impairment, regardless of whether it onsets in adolescence or early adulthood (Hammen et al., 2008).
Although the results of the present study are sobering in speaking to the deleterious implications of chronic/recurrent MDD for adaptive personality development, they also offer some hope in suggesting that the personality trait trajectories of both adolescents and adults who remit from MDD are remarkably similar to trajectories of individuals who never experienced MDD. This is consistent with evidence that young adults who remit from childhood- and adolescent-onset MDD show psychosocial outcomes that are comparable to those for never-depressed youth (Hammen et al., 2008). Moreover, results dovetail with our group’s recent investigation of prospective links between alcohol use disorders and NEM and (low) CON (Hicks et al., 2011), suggesting that remission from MDD and desistance from alcohol use during adolescence and early adulthood are associated with at least some personality “recovery.” Taken together, results point to the importance of targeted intervention efforts during this developmental period that can help adolescents with MDD get “back on track” in terms of adaptive personality development and psychosocial functioning.
The present study has a number of strengths, including a large, community-based sample and a prospective design, and high participation rates over 12 years with minimal attrition bias, though it also has limitations that prompt caution in interpreting the results and suggest directions for future research. Given that the median age of onset for mood disorders is 25 to 32 years (Kessler et al., 2005), it is likely that some participants classified as never depressed will eventually be diagnosed with MDD, and some classified as chronic/recurrent will remit while some classified as remitting will relapse. We measured personality in late adolescence, at age 17, and results may differ for personality assessed at earlier ages. Moreover, although repeated assessment of personality allowed us to model linear personality trait trajectories from late adolescence to adulthood, additional personality and MDD assessments would allow for a more fine-grained examination of the potentially nonlinear course of personality traits and MDD, and would allow for a more direct test of personality-depression associations. Because the majority of participants were not currently symptomatic at the diagnostic assessment, we cannot examine the extent to which MDD has mood-dependent “state” effects on personality traits. Moreover, because, by definition, the adolescent-onset MDD groups had experienced MDD by the age-17 assessment, we are unable to definitively rule out a “scarring” effect of MDD by examining pre-and post-morbid personality levels in these groups. Our assessment of MDD diagnoses was somewhat coarse, in that participants were classified as having chronic/recurrent MDD if they reported experiencing MDD at multiple assessment points that persisted to the age-29 assessment. Although this approach yields information on the ongoing presence of MDD and allows us to contrast these participants with those with remitting MDD, it does not allow for a more fine-grained examination of MDD chronicity or recurrence (see Burcusa & Iacono, 2007; Klein, 2010, for reviews). Although beyond the scope of the present paper, future investigations that take advantage of twin designs to model genetic and environmental influences on personality-MDD associations during the transition from adolescence to adulthood will prove informative (e.g., Hopwood et al. 2011; Kendler et al. 2006). Finally, although representative of the demographic makeup of Minnesota during the targeted birth years, our sample lacks racial or ethnic diversity, thereby limiting generalizability.
In conclusion, the present study highlights the dynamic interplay of personality and MDD in demonstrating that personality traits confer risk for the onset of MDD, while MDD has important implications for adaptive personality development during the transition from adolescence to adulthood. Results speak to the importance of intervention efforts targeted toward individuals at high risk for the subsequent development of MDD by virtue of high NEM and low PEM. Moreover, results add to growing research on the heterogeneity of MDD, with naturally occurring groups defined by MDD onset and course evidencing different personality trajectories and indicating that chronicity/recurrence, in addition to adolescent onset, are important determinants of MDD outcome.
Acknowledgements
This work was supported by grants DA 05147 of the National Institute on Drug Abuse, AA 09367 of the National Institute on Alcohol Abuse and Alcoholism, and MH 017069 of the National Institute of Mental Health (DiRago).
Footnotes
We also conducted analyses including only participants who met MDD criteria at the definite level; with one exception (noted in Table 2), results were the same as for analyses including both definite and probable cases of MDD.
We also tested for interactions between participant sex and MDD group status; of the 30 interaction effects examined, only one was significant, indicating that, by and large, associations between MDD and personality trait trajectories are comparable for males and females. For ease of presentation we present results only for main effects of MDD group.
The authors have no financial involvement or affiliation with any organizations whose financial interests may be affected by material in this work, or that might potentially bias it.
Contributor Information
Sylia Wilson, Department of Psychology, University of Minnesota, Minneapolis, Minnesota.
Ana C. DiRago, Union City, California
William G. Iacono, Department of Psychology, University of Minnesota, Minneapolis, Minnesota
References
- Blonigen DM, Carlson MD, Hicks BM, Krueger RF, Iacono WG. Stability and change in personality traits from late adolescence to early adulthood: A longitudinal twin study. Journal of Personality. 2008;76:229–266. doi: 10.1111/j.1467-6494.2007.00485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Burcusa SL, Iacono WG. Risk for recurrence in depression. Clinical Psychology Review. 2007;27:959–985. doi: 10.1016/j.cpr.2007.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Roberts BW, Shiner RL. Personality development: Stability and change. Annual Review of Psychology. 2005;56:453–484. doi: 10.1146/annurev.psych.55.090902.141913. [DOI] [PubMed] [Google Scholar]
- Clark LA. Temperament as a unifying basis for personality and psychopathology. Journal of Abnormal Psychology. 2005;114:505–521. doi: 10.1037/0021-843X.114.4.505. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- De Fruyt F, Van Leeuwen K, Bagby RM, Rolland JP, Rouillon F. Assessing and interpreting personality change and continuity in patients treated for major depression. Psychological Assessment. 2006;18:71–80. doi: 10.1037/1040-3590.18.1.71. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan PA, Keenan-Miller D, Herr NR. Early onset recurrent subtype of adolescent depression: Clinical and psychosocial correlates. Journal of Child Psychology and Psychiatry. 2008;49:433–440. doi: 10.1111/j.1469-7610.2007.01850.x. [DOI] [PubMed] [Google Scholar]
- Hicks BM, Durbin CE, Blonigen DM, Iacono WG, McGue M. Relationship between personality change and the onset and course of alcohol dependence in young adulthood. Addiction. 2011;107:540–548. doi: 10.1111/j.1360-0443.2011.03617.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Donnellan MB, Blonigen DM, Krueger RF, McGue M, Iacono WG, Burt SA. Genetic and environmental influences on personality trait stability and growth during the transition to adulthood: A three-wave longitudinal study. Journal of Personality and Social Psychology. 2011;100:545–556. doi: 10.1037/a0022409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacono WG, McGue M. Minnesota Twin Family Study. Twin Research. 2002;5:482–487. doi: 10.1375/136905202320906327. [DOI] [PubMed] [Google Scholar]
- Iacono WG, McGue M, Krueger RF. Minnesota Center for Twin and Family Research. Twin Research and Human Genetics. 2006;9:978–984. doi: 10.1375/183242706779462642. [DOI] [PubMed] [Google Scholar]
- John OP, Caspi A, Robins RW, Moffitt TE, Stouthamer-Loeber M. The “Little Five”: Exploring the nomological network of the five-factor model of personality in adolescent boys. Child Development. 1994;65:160–178. [PubMed] [Google Scholar]
- Joiner TE, Lonigan CJ. Tripartite model of depression and anxiety in youth psychiatric inpatients: Relations with diagnostic status and future symptoms. Journal of Clinical Child Psychology. 2000;29:372–382. doi: 10.1207/S15374424JCCP2903_8. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gatz M, Gardner CO, Pedersen NL. Personality and major depression. Archives of General Psychiatry. 2006;63:1113–1120. doi: 10.1001/archpsyc.63.10.1113. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The costs of depression. Psychiatric Clinics of North America. 2012;35:1–14. doi: 10.1016/j.psc.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Klein DN. Chronic depression: Diagnosis and classification. Current Directions in Psychological Science. 2010;19:96–100. [Google Scholar]
- Klein DN, Kotov R, Bufferd SJ. Personality and depression: Explanatory models and review of the evidence. Annual Review of Clinical Psychology. 2011;7:269–295. doi: 10.1146/annurev-clinpsy-032210-104540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Gamez W, Schmidt F, Watson D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychological Bulletin. 2010;136:768–821. doi: 10.1037/a0020327. [DOI] [PubMed] [Google Scholar]
- Lonigan CJ, Hooe ES, David CF, Kistner JA. Positive and negative affectivity in children: Confirmatory factor analysis of a two-factor model and its relation to symptoms of anxiety and depression. Journal of Consulting and Clinical Psychology. 1999;67:374–386. doi: 10.1037//0022-006x.67.3.374. [DOI] [PubMed] [Google Scholar]
- Lonigan CJ, Phillips BM, Hooe ES. Relations of positive and negative affectivity to anxiety and depression in children: Evidence from a latent variable longitudinal study. Journal of Consulting and Clinical Psychology. 2003;71:465–481. doi: 10.1037/0022-006x.71.3.465. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS, Cheong Y, Congdon RT. HLM 5: Hierarchical linear and nonlinear modeling. Lincolnwood, IL: Scientific Software International; 2004. [Google Scholar]
- Reich W, Welner Z. Revised version of the Diagnostic Interview for Children and Adolescents (DICA-R) St. Louis, MO: Washington University School of Medicine, Department of Psychiatry; 1988. [Google Scholar]
- Roberts BW, DelVecchio WF. The rank-order consistency of personality traits from childhood to old age: A quantitative review of longitudinal studies. Psychological Bulletin. 2000;126:3–25. doi: 10.1037/0033-2909.126.1.3. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Walton KE, Viechtbauer W. Patterns of mean-level change in personality traits across the life course: A meta-analysis of longitudinal studies. Psychological Bulletin. 2006;132:1–25. doi: 10.1037/0033-2909.132.1.1. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Klein DN, Seeley JR, Gau JM. Key characteristics of major depressive disorder occurring in childhood, adolescence, emerging adulthood, and adulthood. Clinical Psychological Science. 2013;1:41–53. doi: 10.1177/2167702612457599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sartorius N. The economic and social burden of depression. Journal of Clinical Psychiatry. 2001;62:8–11. [PubMed] [Google Scholar]
- Spitzer RL, Endicott J, Robins E. Research diagnostic criteria: rationale and reliability. Archives of General Psychiatry. 1978;35:773–782. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First M. Structured Interview for DSM-III-R (SCID) New York: Biometrics Research; 1987. [Google Scholar]
- Tackett JL. Evaluating models of the personality? Psychopathology relationship in children and adolescents. Clinical Psychology Review. 2006;26:584–599. doi: 10.1016/j.cpr.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Tellegen A. Manual for the Multidimensional Personality Questionnaire. Minneapolis: University of Minnesota Press; 2006. [Google Scholar]
- Üstün TB, Ayuso-Mateos JL, Chatterji S, Mathers C, Murray CJL. Global burden of depressive disorders in the year 2000. British Journal of Psychiatry. 2004;184:386–392. doi: 10.1192/bjp.184.5.386. [DOI] [PubMed] [Google Scholar]
- Watson D, Gamez W, Simms LJ. Basic dimensions of temperament and their relation to anxiety and depression: A symptom-based perspective. Journal of Research in Personality. 2005;39:46–66. [Google Scholar]
- Weissman MM, Wolk S, Goldstein RB, Moreau D, Adams P, Greenwald S, Klier CM, Ryan ND, Dahl RE, Wickramaratne P. Depressed adolescents grown up. Journal of the American Medical Association. 1999;281:1707–1713. doi: 10.1001/jama.281.18.1707. [DOI] [PubMed] [Google Scholar]
- Wetter EK, Hankin BL. Mediational pathways through which positive and negative emotionality contribute to anhedonic symptoms of depression: A prospective study of adolescents. Journal of Abnormal Child Psychology. 2009;37:507–520. doi: 10.1007/s10802-009-9299-z. [DOI] [PMC free article] [PubMed] [Google Scholar]