Abstract
Objectives
Previous observations propose that risk-taking behaviors such as cigarette smoking are prevailing among young people with chronic conditions including diabetes. The purpose of this study was to examine whether cigarette smoking is more prevalent among diabetics than non-diabetics and whether it differs by age at the time of diagnosis with diabetes from young adulthood (YAH) to adulthood (AH).
Methods
We used US panel data from the National Longitudinal Study of Adolescent Health (Add Health Study) during the years 2001 to 2002 (Wave III, YAH) and 2007 to 2008 (Wave IV, AH). Multivariate logistic regression models were applied to estimate odds ratios (ORs) and 95% confidence intervals (CIs) of cigarette use behaviors according to age at the time of diagnosis with diabetes, after adjusting for demographic and selected behavioral factors.
Results
Of 12 175 study participants, 2.6% reported having been diagnosed with diabetes up to AH. Early-onset diabetics (age at diagnosis <13 years) were more likely than non-diabetics to report frequent cigarette smoking (smoking on ≥20 days during the previous 30 days) in YAH (OR, 3.34; 95% CI, 1.27 to 8.79). On the other hand, late-onset diabetics (age at diagnosis ≥13 years) were more likely than non-diabetics to report heavy cigarette smoking (smoking ≥10 cigarettes per day during the previous 30 days) in AH (OR, 1.54; 95% CI, 1.03 to 2.30).
Conclusions
The current study indicated that diabetics are more likely than non-diabetics to smoke cigarettes frequently and heavily in YAH and AH. Effective smoking prevention and cessation programs uniquely focused on diabetics need to be designed and implemented.
Keywords: Young adult, Health behavior, Smoking, Diabetes mellitus
INTRODUCTION
The detrimental health effects of cigarette smoking have been demonstrated conclusively over the last few decades [1,2]. In the US, extensive public health efforts to reduce the burden of smoking-attributable morbidity and mortality have been made. As a result, outstanding achievements in the reduction of cigarette smoking prevalence have been reported [3]. Nonetheless, cigarette smoking remains the most important modifiable cause of death and disease in the US [4]. According to the 2010 US Surgeon General's report, the number of deaths from smoking-related diseases among US adults is approximately 443 000 each year [5]. The US Centers for Disease Control and Prevention reported that the total economic burden of cigarette smoking in the US during the years 2000 to 2004 was approximately 193 billion dollars per year, when accounting for direct health care expenditures (approximately 96 billion dollars) and productivity losses (approximately 97 billion dollars) [6].
Cigarette smoking is well-recognized to cause insulin resistance and chronic inflammation, which can hasten macrovascular and microvascular complications, including nephropathy [5]. There have been consistent results from both cross-sectional and prospective studies, indicating elevated risks for macrovascular and microvascular complications as well as premature mortality from the combined effects of cigarette smoking and diabetes [7]. On the basis of the significant body of evidence, the American Diabetes Association through its position statement has accentuated the importance of counseling on smoking prevention and cessation and well-organized systems for delivery of smoking cessation for people with diabetes [8]. However, a report on the achievement of goals in diabetes care in the US from 1999 to 2010 demonstrated that although there were notable advancements in risk factor control and adherence to preventive practices, tobacco use in this vulnerable population remained considerable [9].
Several observations propose that risk-taking behaviors, such as cigarette smoking, alcohol consumption, and illicit drug use, are prevailing among young people with chronic conditions including diabetes [10,11]. These data have suggested that the presence of chronic conditions does not deter young people from engaging in risk-taking behaviors, but it rather carries additional risks for risk-taking behaviors.
Previous studies on cigarette use behaviors among adults with diabetes in the US have revealed that young people, aged 18 to 44 years, with diabetes were more likely than their counterparts without the disease to report cigarette smoking [12-14]. One of these studies [12], which examined the secular trends in the prevalence of cigarette smoking from 1990 to 2001, showed that significant decreases in the prevalence of cigarette smoking occurred among diabetics aged ≥65 years, but not among young people with the disease. However, a relatively small number of studies, conducted in the US [15,16], Italy [17], and Chile [18], have addressed the prevalence of cigarette use behaviors among diabetic adolescents. Furthermore, hardly any study has investigated the association between cigarette smoking and diabetes status or specific characteristics of the disease, such as age at the time of diagnosis, during the transition to adulthood (AH) using longitudinal data. Therefore, the purpose of this study was to examine whether cigarette smoking is more prevalent among diabetics than non-diabetics and whether it differs by age at the time of diagnosis with diabetes from young adulthood (YAH) to AH, using nationally representative longitudinal data.
METHODS
Study Population
The National Longitudinal Study of Adolescent Health (Add Health Study) is a nationally representative study of youths in the US, followed up with multiple interview waves into AH. The study design and sampling method of the Add Health Study have been described in detail elsewhere [19]. For the in-school survey conducted in 1994, a sample of 80 high schools and 52 feeder schools (junior high and middle schools) was selected with unequal probability of selection. In-home interviews were also carried out to gather multiple panels of data: the first wave of data (Wave I, 1994 to 1995) included 20 745 adolescents, who were 7 to 12 graders, from the pool of participants in the in-school survey; the second wave of data (Wave II) was obtained after a 1-year interval, which comprised 14 738 adolescents in grades 8 to 12; the third wave of data (Wave III, 2001 to 2002), representing data in YAH, was collected from 15 197 young adults, aged 18 to 26 years, who enrolled in the Wave I in-home survey; and the fourth wave of data (Wave IV, 2007 to 2008), representing data in AH, was collected from 15 701 adults from the Wave I in-home survey, now aged 24 to 32 years. Data from two points in time-in YAH (Wave III) and AH (Wave IV)-from the Add Health Study were used to evaluate the engagement in cigarette smoking in YAH and AH according to age at diagnosis with diabetes. We restricted the sample to participants interviewed at both time points with valid measures of data at each time point: participants who had missing data on variables such as age at diagnosis with diabetes, or cigarette smoking in both YAH and AH, were excluded from the analyses, as were participants without sampling weights. As a result, our final analysis sample totaled 12 175 participants.
Assessment of Diabetes
Diabetes status and age at diagnosis with diabetes were assessed using the following questions from Wave IV: 1) "Has a doctor, nurse, or other health care provider ever told you that you have or had high blood sugar or diabetes?"; and 2) "How old were you when the doctor, nurse, or other health practitioner first told you about your high blood sugar or diabetes (if female add, 'when you were not pregnant')?" According to the answers to the questions, the study participants were classified into three groups: non-diabetics (no diagnosis), early-onset diabetics (age at diagnosis <13 years), and late-onset diabetics (age at diagnosis ≥13 years). The cut-off value of age at diagnosis with diabetes was determined by the starting point of the teens, considering not only that there is no clinical cut-off value for differentiating two types of diabetes mellitus, type 1 and type 2, but also that teens are regarded to be in a period of multiple transitions involving social, psychological, and physical development.
Assessment of Cigarette Use Behaviors
Smoking initiation was determined using the following question from Wave III: "How old were you the first time you smoked an entire cigarette?" Smoking an entire cigarette for the first time before 13 years of age was considered to be early smoking initiation. Frequent and heavy cigarette use behaviors in YAH and AH were determined using the following questions from Wave III and IV, respectively: "During the previous 30 days, on how many days did you smoke cigarettes?"; "During the previous 30 days, on the days you smoked, how many cigarettes did you smoke each day?" Smoking on ≥20 days during the previous 30 days was considered to be current frequent cigarette use. Smoking ≥10 cigarettes per day during the previous 30 days was considered to be current heavy cigarette use. As for the above-mentioned three smoking indices, the definitions of cigarette use behaviors of the Youth Risk Behavior Surveillance System, a nationwide monitoring system of risk-taking behaviors among youths in the US, were adopted [20].
Covariates
Information on demographic characteristics such as gender, race / ethnicity, birth year, education level, and socioeconomic status was obtained from the Wave III reports. Education level was grouped as follows according to academic degrees or diplomas: low level (no academic degrees or diplomas, general equivalency diploma or high school equivalency degree, or high school diploma), middle level (associate or junior college degree, or bachelor's degree), and high level (master's degree, doctoral degree, or professional degree). Socioeconomic status was grouped as follows according to annual household income before taxes: low level (<10 000 dollars), middle level (10 000 to 29 999 dollars), and high level (≥30 000 dollars). Frequent alcohol use was assessed using the following question from Wave III: "During the previous 12 months, on how many days did you drink alcohol?" According to the answer to the question, the study participants were divided into five groups: once a month or less, 2 or 3 days a month, 1 or 2 days a week, 3 to 5 days a week, and every day. Heavy alcohol use was assessed using the following question from Wave III: "Think of all the times you have had a drink during the previous 12 months. How many drinks did you usually have each time?" According to the answer to the question, the study participants were divided into two groups: <5 drinks vs. ≥5 drinks on a single occasion (which was considered to be heavy alcohol use). Suicidal ideation was determined by the answer to the following question from Wave III: "During the previous 12 month, did you ever seriously think about committing suicide?"
Statistical Analysis
Data were expressed as frequencies and weighted percentages for categorical variables. Chi-square tests were used to test the differences in proportions between groups. Multivariate logistic regression models were applied to estimate odds ratios (ORs) and 95% confidence intervals (CIs) of early smoking initiation or frequent and heavy cigarette use behaviors in both YAH and AH according to age at diagnosis with diabetes, after adjusting for gender, race / ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, Asian /Pacific islander, and Native American), birth year (1982 to 1983, 1980 to 1981, 1978 to 1979, 1976 to 1977, and 1974 to 1975), education level (low, middle, and high), socioeconomic status (low, middle, and high), heavy alcohol use (yes and no), and suicidal ideation (yes and no). In multivariate analyses, missing data on the adjustment variables (education level, socioeconomic status, heavy alcohol use, and suicidal ideation) were included as an additional category of each variable. Given that cigarette use behaviors can differ by demographic factors [20], stratified analyses were additionally carried out according to gender and race / ethnicity (whites and non-whites).
In order to evaluate statistical significance, a two-sided significance level of 0.05 was used. All of the statistical analyses were performed using SAS version 9.2 (SAS Inc., Cary, NC, USA), a statistical software program that is capable of analyzing data derived from complex sampling designs. In the current study, design-based statistical tests (using the SURVEYFREQ, SURVEYMEANS, and SURVEYLOGISTIC SAS procedures), which incorporated the sample design into the analyses, were used to ensure statistically valid inferences for the population. This study was performed in accordance with the guidelines of the Declaration of Helsinki and approved by the institutional review boards of Daegu Catholic University Medical Center in Korea.
RESULTS
Of 12 175 study participants, 2.6% reported having been diagnosed with diabetes up to AH. The baseline characteristics of the study participants (Wave III, 2001 to 2002) according to current frequent cigarette use are illustrated in Table 1. Of 12 175 study participants, the weighted percentage of current frequent cigarette users was 28.9%. The distributions of gender and race / ethnicity differed by the presence of current frequent cigarette smoking (p-value, 0.002 and <0.001, respectively). The distributions of education level and socioeconomic status of the two cigarette smoking groups differed as well (all p-values, <0.001). Current frequent cigarette users were more likely to be current frequent and heavy alcohol users than were those who were not current frequent cigarette users. More current frequent cigarette users than those who were not current frequent cigarette users had seriously thought about committing suicide during the previous 12 months.
Table 1.
Baseline characteristics of the study participants according to current frequent cigarette use1: the Add Health Study (Wave III, 2001 to 2002)
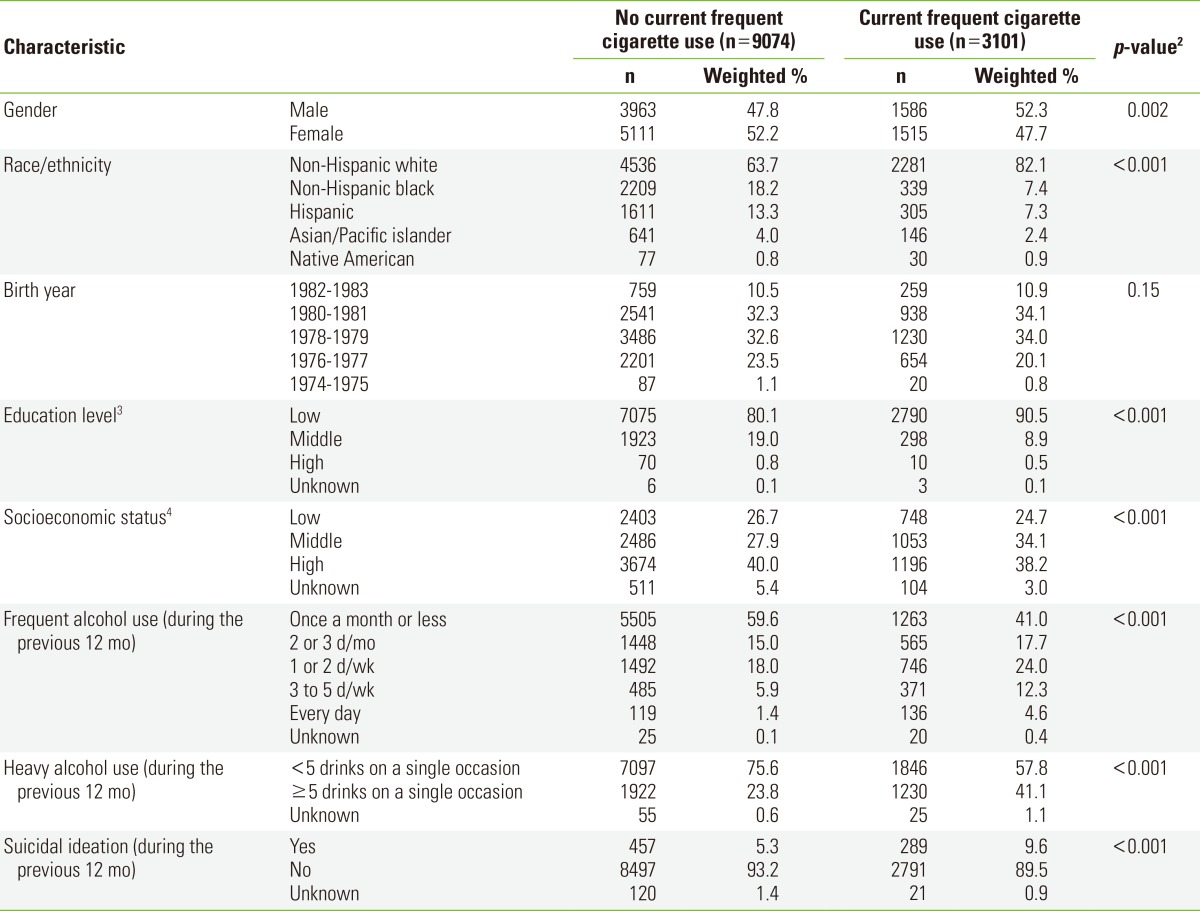
1Smoking cigarettes on ≥20 days during the previous 30 days.
2Calculated by chi-square tests.
3Education level was grouped as follows according to academic degrees or diplomas: low level, no academic degrees or diplomas, general equivalency diploma or high school equivalency degree, or high school diploma; middle level, associate or junior college degree, or bachelor's degree; high level, master's degree, doctoral degree, or professional degree.
4Socioeconomic status was grouped as follows according to annual household income before taxes: low level, <10 000 dollars; middle level, 10 000 to 29 999 dollars; high level, ≥30 000 dollars.
Table 2 shows the weighted percentages and adjusted ORs of current frequent cigarette use in YAH and AH according to age at diagnosis with diabetes. The percentages of current frequent cigarette use in both YAH and AH were higher among early-onset diabetics (at Wave III, 64%; at Wave IV, 38.2%) than among non-diabetics (at Wave III, 28.9%; at Wave IV, 27.6%) or late-onset diabetics (at Wave III, 26.4%; at Wave IV, 30.0%). The current frequent cigarette smoking rate decreased from YAH to AH among non-diabetics (from 28.9% to 27.6%) and early-onset diabetics (from 64.0% to 38.2%); in contrast, the rate increased among late-onset diabetics (from 26.4% to 30.0%). In the subgroup analyses by gender and race / ethnicity, the rate increased from YAH to AH among late-onset diabetics who were females (from 27.8% to 34.7%) and whites (from 27.3% to 36.5%). When controlling for gender, race / ethnicity, birth year, education level, socioeconomic status, heavy alcohol use, and suicidal ideation, the adjusted OR of current frequent cigarette use in YAH among early-onset diabetics was 3.34 (95% CI, 1.27 to 8.79) compared with non-diabetics. In the subgroup analyses by gender and race / ethnicity, statistically significant associations between current frequent cigarette use and diabetes status were observed in the subgroups of females (at Wave III, early-onset diabetics vs. non-diabetics, adjusted OR, 5.43; 95% CI, 1.29 to 22.9); at Wave IV, late-onset diabetics vs. non-diabetics, adjusted OR, 1.63; 95% CI, 1.05 to 2.54) and whites (at Wave III, early-onset diabetics vs. non-diabetics, adjusted OR, 3.30; 95% CI, 1.08 to 10.1).
Table 2.
Weighted percentages and adjusted ORs1 of current frequent cigarette use in young adulthood (Wave III) and adulthood (Wave IV) among the study participants according to age at diagnosis with diabetes
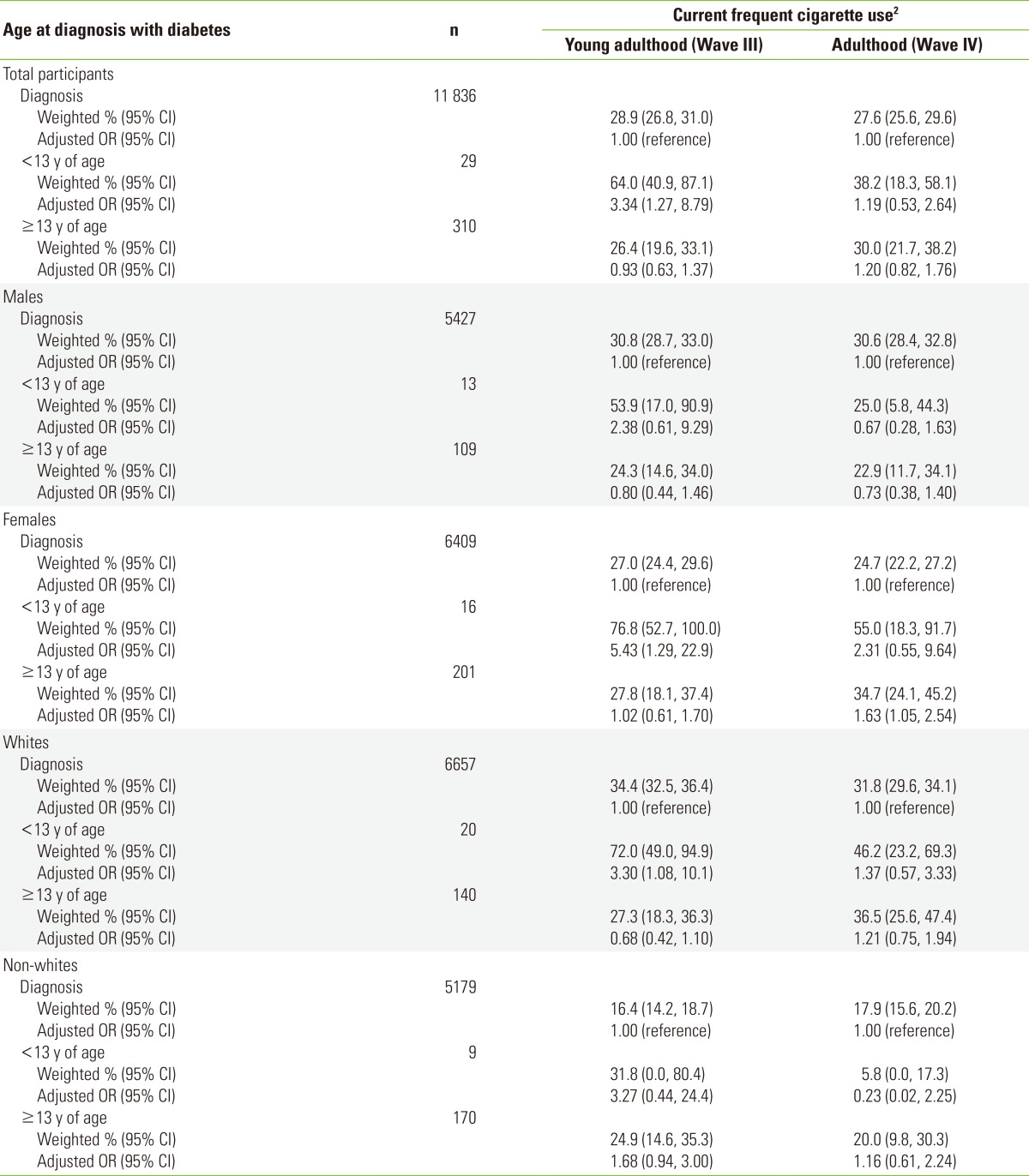
OR, odds ratio; CI, confidence interval.
1Multiple logistic regression models were applied to estimate ORs and 95% CIs of cigarette use behaviors, after adjusting for gender, race/ethnicity, birth year, education level, socioeconomic status, heavy alcohol use, and suicidal ideation.
2Smoking cigarettes on ≥20 days during the previous 30 days.
Table 3 presents the weighted percentages and adjusted ORs of current heavy cigarette use in YAH and AH according to age at diagnosis with diabetes. The percentages of current heavy cigarette use in both YAH and AH were the highest among early-onset diabetics (at Wave III, 47.0%; at Wave IV, 33.9%) and the lowest among non-diabetics (at Wave III, 20.8%; at Wave IV, 20.2%). The current heavy cigarette smoking rate decreased from YAH to AH among non-diabetics (from 20.8% to 20.2%) and early-onset diabetics (from 47.0% to 33.9%); in contrast, the rate increased among late-onset diabetics (from 22.0% to 25.2%). In the subgroup analyses by gender and race/ ethnicity, the rate increased from YAH to AH among late-onset diabetics who were males (from 19.6% to 23.9%), females (from 23.7% to 26.1%), and whites (from 25.3% to 32.6%). When controlling for demographic and selected behavioral factors, the adjusted OR of current heavy cigarette use in AH among late-onset diabetics was 1.54 (95% CI, 1.03 to 2.30) compared with non-diabetics. In the subgroup analyses by gender and race / ethnicity, statistically significant associations between current heavy cigarette use and diabetes status were observed in the subgroups of females (at Wave III, early-onset diabetics vs. non-diabetics, adjusted OR, 9.18; 95% CI, 2.10 to 40.1; at Wave IV, late-onset diabetics vs. non-diabetics, adjusted OR, 1.95; 95% CI, 1.18 to 3.22) and non-whites (at Wave III, late-onset diabetics vs. non-diabetics, adjusted OR, 2.26; 95% CI, 1.10 to 4.65).
Table 3.
Weighted percentages and adjusted ORs1 of current heavy cigarette use in young adulthood (Wave III) and adulthood (Wave IV) among the study participants according to age at diagnosis with diabetes
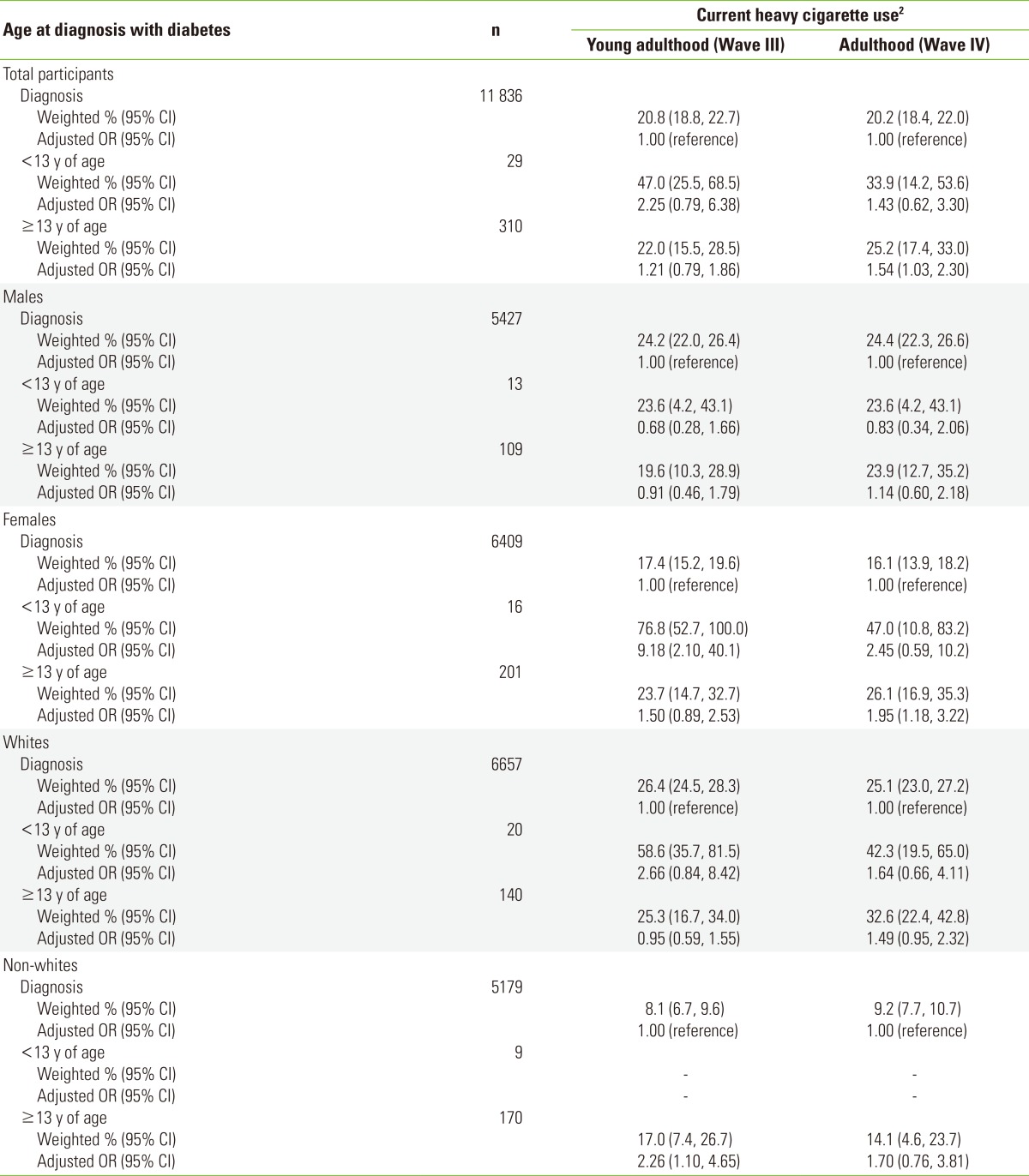
OR, odds ratio; CI, confidence interval.
1Multiple logistic regression models were applied to estimate ORs and 95% CIs of cigarette use behaviors, after adjusting for gender, race/ethnicity, birth year, education level, socioeconomic status, heavy alcohol use, and suicidal ideation.
2Smoking cigarettes ≥10 cigarettes per day during the previous 30 days.
Table 4 presents the weighted percentages and adjusted ORs of early smoking initiation according to age at diagnosis with diabetes. The weighted percentage of those who smoked an entire cigarette for the first time before 13 years of age was higher among early-onset diabetics (22.6%) than among non-diabetics (9.4%) or late-onset diabetics (6.5%). However, when controlling for demographic and selected behavioral factors, there was no statistically significant difference in early smoking initiation according to age at diagnosis with diabetes. In the subgroup analyses by gender and race / ethnicity, however, a statistically significant association between early smoking initiation and diabetes status was observed in the subgroup of non-whites (early-onset diabetics vs. non-diabetics, adjusted OR, 9.42; 95% CI, 1.04 to 84.9).
Table 4.
Weighted percentages and adjusted ORs1 of early smoking initiation among the study participants according to age at diagnosis with diabetes
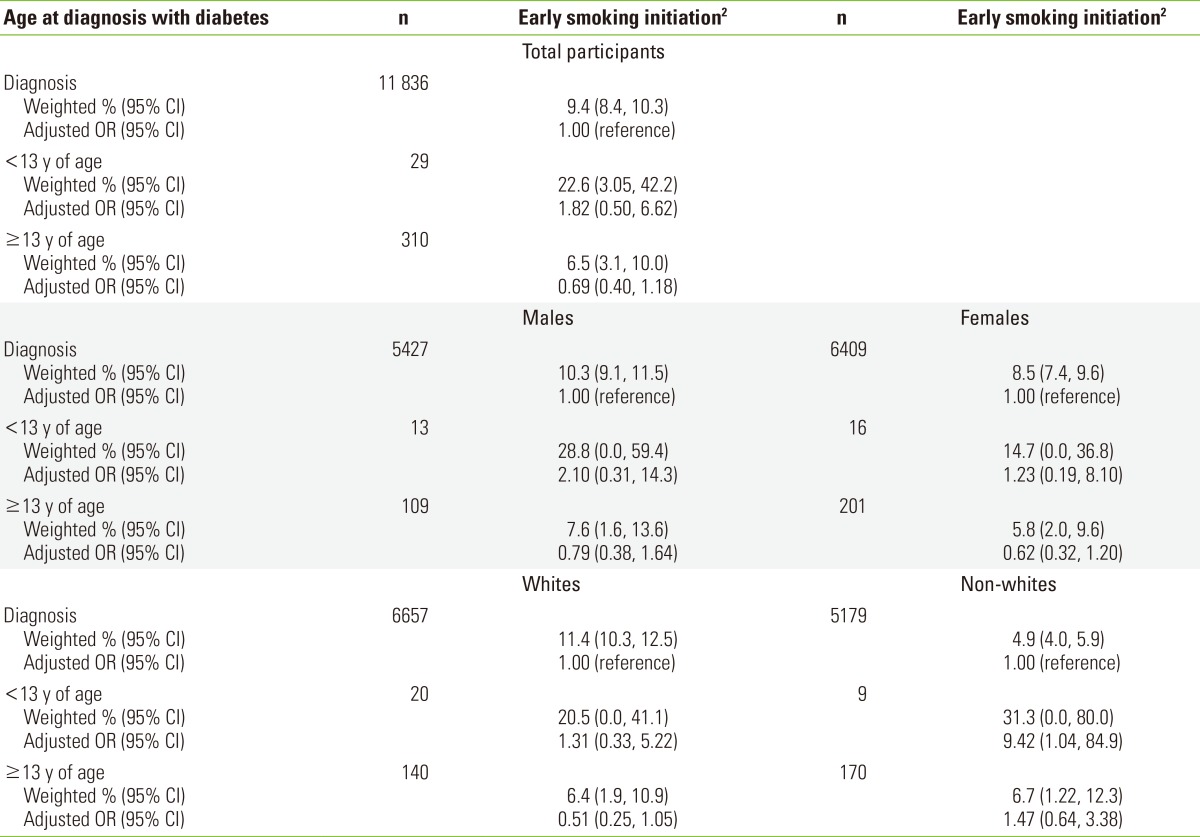
OR, odds ratio; CI, confidence interval.
1Multiple logistic regression models were applied to estimate ORs and 95% CIs of cigarette use behaviors, after adjusting for gender, race/ethnicity, birth year, education level, socioeconomic status, heavy alcohol use, and suicidal ideation.
2Smoking an entire cigarette for the first time before 13 years of age.
DISCUSSION
The current study indicated that early-onset diabetics were more likely than non-diabetics to smoke cigarettes frequently in YAH; on the other hand, late-onset diabetics were more likely than non-diabetics to smoke cigarettes heavily in AH. In the demographic subgroup analyses, early-onset diabetics were more likely than non-diabetics to report frequent (in females and whites) and heavy (in females) cigarette use in YAH. Meanwhile, in AH, late-onset diabetics were more likely than non-diabetics to report frequent (in females) and heavy (in females) cigarette use. These findings appear to be related to the decreasing smoking rates among early-onset diabetics and increasing smoking rates among late-onset diabetics from YAH to AH. Current frequent and heavy cigarette smoking rates tended to increase from YAH and AH among late-onset diabetics (for current frequent cigarette use, in the total participants, females, and whites; for current heavy cigarette use, in the total participants, males, females, and whites). On the other hand, among non-diabetics or early-onset diabetics, these increasing trends in current frequent and heavy cigarette smoking rates were not noted, but the rates rather tended to decrease. In addition to these findings, early-onset diabetics were more likely than non-diabetics to report early smoking initiation (in non-whites).
People with diabetes are particularly susceptible to the detrimental effects of cigarette smoking, because they carry elevated risks for cardiovascular morbidity and mortality than those without diabetes. Previous studies have indicated that cigarette smoking among diabetics is associated with the deterioration of glycemic control and heightened risks for microvascular and macrovascular complications and death [21-24]. Cigarette smoking among diabetics may enhance the responses of counter-regulatory hormones, such as growth hormone and cortisol, to insulin-induced hypoglycemia, which lead to higher blood glucose and glycated hemoglobin (HbA1c, a marker of glycemic control) levels [25]. Besides, the vasoactive effects of cigarette smoking, inducing the release of vasoconstrictor sympathetic neurotransmitters and repeated episodes of acute renal hypoperfusion, may explain the early onset of microalbuminuria and the acceleration of diabetic nephropathy among diabetics who smoke [22,23]. Notwithstanding strong and consistent evidence on the harmful effects of cigarette smoking, as shown in the current study and reported previously [12-15,17], this chronically ill population appears to smoke cigarettes as frequently and heavily as, or even more frequently or heavily than their counterparts without the disease do.
In a qualitative study conducted among Swedish adolescents, Regber and Kelly [26] evaluated why adolescents with diabetes choose to smoke, despite presumed awareness of health risks. Reasons for their cigarette use behaviors included pure experimentation, identity development, the need to conform to group norms, and denial of health risks. The same study also found that few adolescents reported taking advice from health professionals regarding cigarette smoking. Studies have suggested that young people with chronic conditions are more vulnerable and subjected to more pressures to conform to group norms [26,27]. Young people with chronic conditions may feel more needs to be accepted by their healthy counterparts, with engagement in risk-taking behaviors including cigarette smoking serving to substantiate their fitness and reinforce their self-esteem [28]. In order to better understand and control cigarette use behaviors among diabetics, further investigations are needed to identify diabetes-specific motivations for initiating and quitting cigarette smoking.
In the current study, statistically significant associations between diabetes status and frequent and heavy cigarette use behaviors were noted in females, but not in males. Several studies have also demonstrated gender differences in smoking predictors and diabetes-specific factors such as adaptability to living with the disease [29,30]. The gender difference noted in the association between diabetes status and cigarette smoking in the current study may be also explained by lower self-esteem in girls than in boys [31], especially girls with diabetes, and cigarette smoking as a means of boosting their self-esteem. Although the study participants were classified into whites and non-whites due to the small number of diabetics, not allowing comparisons of cigarette use behaviors among different race / ethnic groups, race / ethnic differences in the association between diabetes status and cigarette smoking were also observed in the current study, as reported in previous studies [12-14]. A better understanding of demographic and psychosocial factors may be of help to indentify diabetics who are at especially high risk of cigarette smoking.
Surprisingly, hardly any study has investigated the bi-directionality in the relationship between diabetes status and cigarette smoking using longitudinal data. In the current study, statistically significant associations between diabetes status and cigarette use behaviors were observed in both early-onset diabetes and late-onset diabetes. Among early-onset diabetics, having a chronically ill condition may have been the predictor of early smoking initiation and frequent and heavy cigarette use behaviors in YAH. As they aged and the duration of the disease was prolonged, however, adverse health consequences caused by cigarette smoking may have deterred them from cigarette use behaviors in AH [14]. Among late-onset diabetics, on the other hand, the progression of their cigarette use behaviors during the transition to AH may have been related to the development of the disease. Several population-based prospective studies have consistently demonstrated that cigarette smoking is associated with the development of type 2 diabetes [32].
It is also worth noting that the study results revealed that the pattern of cigarette smoking during the transition to AH differed by the onset of diabetes (early-onset and late-onset). In a 10-year follow-up study of an onset cohort of children and adolescents with type 1 diabetes [33], young adults, aged 19 to 26 years, with type 1 diabetes reported lower self-esteem than young adults with acute illness (the control group), indicating the possibility of psychosocial maladjustment. Evidence from other studies among adults with diabetes has shown that diabetes is associated with an increased prevalence of psychiatric conditions including depression [34,35]. One of the studies, conducted in the US, showed that the mean age of onset of depression differed by the type of diabetes [35]. Namely, the mean age of onset of depression was 22.1 years among type 1 diabetics and 28.6 years among type 2 diabetics (which was similar to that in the general population [27 to 35 years]). Psychiatric conditions in chronically ill populations are known to be associated with engagement in risk-taking behaviors including cigarette smoking [36,37]. A cross-sectional study revealed that the number of cigarettes smoked was a significant predictor of the severity of depressive symptoms among people with diabetes [37]. An early age at diagnosis with diabetes is regarded as a phenotypic feature consistent with type 1 diabetes. However, the classification of early-onset and late-onset diabetics in the current study could not differentiate type 1 diabetics from type 2 diabetics, considering recent changes in diabetes classification including the recognition of latent autoimmune diabetes in adults [38]. Nevertheless, both significantly higher cigarette smoking rates in YAH among early-onset diabetics and significantly higher cigarette smoking rates in AH among late-onset diabetics observed in the current study may stem in part from their psychological maladjustment or psychiatric conditions.
The limitations of this study include self-reported diabetes status and age at diagnosis with diabetes, which were not derived from medical charts or clinical examinations, and the possibility of under-reporting in the assessment of diabetes status and cigarette use behaviors due to the reliance on self-reports. The type (e.g., type 1 and type 2) and duration of diabetes were not taken into account when analyzing data from the Add Health Study. Nonetheless, to the best of our knowledge, this is the first report on the association between diabetes status and cigarette smoking using data from the Add Health Study. The current study, which was conducted using nationally representative data, added further evidence on the patterns of cigarette use behaviors among diabetics over time.
In conclusion, the current study indicated that diabetics are more likely than non-diabetics to smoke cigarettes frequently and heavily in YAH and AH. Evidence from this study proposes that special attention should be paid to emphasizing the importance of smoking prevention and cessation in diabetes care. Behavioral changes can result in substantial increases in health and quality of life, and the benefits of smoking cessation are significant [39]. In particular, diabetic smokers represent a population that could potentially benefit even more than their counterparts without the disease from smoking cessation [40]. Early identification of cigarette use behaviors among diabetes is imperative so that counseling on smoking prevention and cessation can prevent devastating health consequences that might be incurred. It is also important to note that this chronically ill population may need specific strategies for overcoming their unique problems during smoking cessation, such as post-cessation weight gain and depression [7,39,40]. Effective smoking prevention and cessation programs uniquely focused on diabetics need to be designed and implemented.
ACKNOWLEDGEMENTS
This study was funded by a grant from Catholic University of Daegu School of Medicine.
Footnotes
The authors have no conflicts of interest with the material presented in this paper.
References
- 1.US Department of Health, Education, and Welfare. Smoking and health: report of the advisory committee to the Surgeon General of the Public Health Service. Washington, DC: US Government Printing Office; 1964. pp. 25–40. [Google Scholar]
- 2.Yanbaeva DG, Dentener MA, Creutzberg EC, Wesseling G, Wouters EF. Systemic effects of smoking. Chest. 2007;131(5):1557–1566. doi: 10.1378/chest.06-2179. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Tobacco use: United States, 1900-1999. MMWR Morb Mortal Wkly Rep. 1999;48(43):986–993. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) Current cigarette smoking among adults: United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(44):889–894. [PubMed] [Google Scholar]
- 5.US Department of Health and Human Services. How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease. A report of the Surgeon General. Rockville: US Department of Health and Human Services; 2010. pp. 647–654. [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) Smoking-attributable mortality, years of potential life lost, and productivity losses: United States, 2000-2004. MMWR Morb Mortal Wkly Rep. 2008;57(45):1226–1228. [PubMed] [Google Scholar]
- 7.Haire-Joshu D, Glasgow RE, Tibbs TL. Smoking and diabetes. Diabetes Care. 1999;22(11):1887–1898. doi: 10.2337/diacare.22.11.1887. [DOI] [PubMed] [Google Scholar]
- 8.Haire-Joshu D, Glasgow RE, Tibbs TL American Diabetes Association. Smoking and diabetes. Diabetes Care. 2004;27(Suppl 1):S74–S75. doi: 10.2337/diacare.27.2007.s74. [DOI] [PubMed] [Google Scholar]
- 9.Ali MK, Bullard KM, Saaddine JB, Cowie CC, Imperatore G, Gregg EW. Achievement of goals in U.S. diabetes care, 1999-2010. N Engl J Med. 2013;368(17):1613–1624. doi: 10.1056/NEJMsa1213829. [DOI] [PubMed] [Google Scholar]
- 10.Miauton L, Narring F, Michaud PA. Chronic illness, life style and emotional health in adolescence: results of a cross-sectional survey on the health of 15-20-year-olds in Switzerland. Eur J Pediatr. 2003;162(10):682–689. doi: 10.1007/s00431-003-1179-x. [DOI] [PubMed] [Google Scholar]
- 11.Surís JC, Michaud PA, Akre C, Sawyer SM. Health risk behaviors in adolescents with chronic conditions. Pediatrics. 2008;122(5):e1113–e1118. doi: 10.1542/peds.2008-1479. [DOI] [PubMed] [Google Scholar]
- 12.Ford ES, Mokdad AH, Gregg EW. Trends in cigarette smoking among US adults with diabetes: findings from the Behavioral Risk Factor Surveillance System. Prev Med. 2004;39(6):1238–1242. doi: 10.1016/j.ypmed.2004.04.039. [DOI] [PubMed] [Google Scholar]
- 13.Malarcher AM, Ford ES, Nelson DE, Chrismon JH, Mowery P, Merritt RK, et al. Trends in cigarette smoking and physicians' advice to quit smoking among people with diabetes in the U.S. Diabetes Care. 1995;18(5):694–697. doi: 10.2337/diacare.18.5.694. [DOI] [PubMed] [Google Scholar]
- 14.Ford ES, Malarcher AM, Herman WH, Aubert RE. Diabetes mellitus and cigarette smoking. Findings from the 1989 National Health Interview Survey. Diabetes Care. 1994;17(7):688–692. doi: 10.2337/diacare.17.7.688. [DOI] [PubMed] [Google Scholar]
- 15.Jaser SS, Yates H, Dumser S, Whittemore R. Risky business: risk behaviors in adolescents with type 1 diabetes. Diabetes Educ. 2011;37(6):756–764. doi: 10.1177/0145721711422610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frey MA, Guthrie B, Loveland-Cherry C, Park PS, Foster CM. Risky behavior and risk in adolescents with IDDM. J Adolesc Health. 1997;20(1):38–45. doi: 10.1016/S1054-139X(96)00162-0. [DOI] [PubMed] [Google Scholar]
- 17.Scaramuzza A, De Palma A, Mameli C, Spiri D, Santoro L, Zuccotti GV. Adolescents with type 1 diabetes and risky behaviour. Acta Paediatr. 2010;99(8):1237–1241. doi: 10.1111/j.1651-2227.2010.01813.x. [DOI] [PubMed] [Google Scholar]
- 18.Martínez-Aguayo A, Araneda JC, Fernandez D, Gleisner A, Perez V, Codner E. Tobacco, alcohol, and illicit drug use in adolescents with diabetes mellitus. Pediatr Diabetes. 2007;8(5):265–271. doi: 10.1111/j.1399-5448.2007.00307.x. [DOI] [PubMed] [Google Scholar]
- 19.Chantala K. Guidelines for analyzing add health data. 2006. [cited 2013 May 14]. Available from: http://www.cpc.unc.edu/projects/addhealth/data/guides/wt-guidelines.pdf.
- 20.Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, et al. Youth risk behavior surveillance: United States, 2011. MMWR Surveill Summ. 2012;61(4):1–162. [PubMed] [Google Scholar]
- 21.Hofer SE, Rosenbauer J, Grulich-Henn J, Naeke A, Fröhlich-Reiterer E, Holl RW, et al. Smoking and metabolic control in adolescents with type 1 diabetes. J Pediatr. 2009;154(1):20–23. doi: 10.1016/j.jpeds.2008.07.052. [DOI] [PubMed] [Google Scholar]
- 22.Scott LJ, Warram JH, Hanna LS, Laffel LM, Ryan L, Krolewski AS. A nonlinear effect of hyperglycemia and current cigarette smoking are major determinants of the onset of microalbuminuria in type 1 diabetes. Diabetes. 2001;50(12):2842–2849. doi: 10.2337/diabetes.50.12.2842. [DOI] [PubMed] [Google Scholar]
- 23.Baggio B, Budakovic A, Dalla Vestra M, Saller A, Bruseghin M, Fioretto P. Effects of cigarette smoking on glomerular structure and function in type 2 diabetic patients. J Am Soc Nephrol. 2002;13(11):2730–2736. doi: 10.1097/01.asn.0000032422.81130.68. [DOI] [PubMed] [Google Scholar]
- 24.Bryden KS, Peveler RC, Stein A, Neil A, Mayou RA, Dunger DB. Clinical and psychological course of diabetes from adolescence to young adulthood: a longitudinal cohort study. Diabetes Care. 2001;24(9):1536–1540. doi: 10.2337/diacare.24.9.1536. [DOI] [PubMed] [Google Scholar]
- 25.Chiodera P, Volpi R, Capretti L, Speroni G, Necchi-Ghiri S, Caffarri G, et al. Abnormal effect of cigarette smoking on pituitary hormone secretions in insulin-dependent diabetes mellitus. Clin Endocrinol (Oxf) 1997;46(3):351–357. doi: 10.1046/j.1365-2265.1997.1470945.x. [DOI] [PubMed] [Google Scholar]
- 26.Regber S, Kelly KB. Missed opportunities-adolescents with a chronic condition (insulin-dependent diabetes mellitus) describe their cigarette-smoking trajectories and consider health risks. Acta Paediatr. 2007;96:1770–1776. doi: 10.1111/j.1651-2227.2007.00566.x. [DOI] [PubMed] [Google Scholar]
- 27.Surís JC. Chronic conditions and adolescence. J Pediatr Endocrinol Metab. 2003;16(Suppl 2):247–251. [PubMed] [Google Scholar]
- 28.Valencia LS, Cromer BA. Sexual activity and other high-risk behaviors in adolescents with chronic illness: a review. J Pediatr Adolesc Gynecol. 2000;13(2):53–64. doi: 10.1016/s1083-3188(00)00004-8. [DOI] [PubMed] [Google Scholar]
- 29.Williams C. Doing health, doing gender: teenagers, diabetes and asthma. Soc Sci Med. 2000;50(3):387–396. doi: 10.1016/s0277-9536(99)00340-8. [DOI] [PubMed] [Google Scholar]
- 30.Van den Bree MB, Whitmer MD, Pickworth WB. Predictors of smoking development in a population-based sample of adolescents: a prospective study. J Adolesc Health. 2004;35(3):172–181. doi: 10.1016/j.jadohealth.2003.09.021. [DOI] [PubMed] [Google Scholar]
- 31.Kling KC, Hyde JS, Showers CJ, Buswell BN. Gender differences in self-esteem: a meta-analysis. Psychol Bull. 1999;125(4):470–500. doi: 10.1037/0033-2909.125.4.470. [DOI] [PubMed] [Google Scholar]
- 32.Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2007;298(22):2654–2664. doi: 10.1001/jama.298.22.2654. [DOI] [PubMed] [Google Scholar]
- 33.Jacobson AM, Hauser ST, Willett JB, Wolfsdorf JI, Dvorak R, Herman L, et al. Psychological adjustment to IDDM: 10-year follow-up of an onset cohort of child and adolescent patients. Diabetes Care. 1997;20(5):811–818. doi: 10.2337/diacare.20.5.811. [DOI] [PubMed] [Google Scholar]
- 34.Lustman PJ, Penckofer SM, Clouse RE. Recent advances in understanding depression in adults with diabetes. Curr Psychiatry Rep. 2008;10(6):495–502. doi: 10.1007/s11920-008-0079-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lustman PJ, Griffith LS, Gavard JA, Clouse RE. Depression in adults with diabetes. Diabetes Care. 1992;15(11):1631–1639. doi: 10.2337/diacare.15.11.1631. [DOI] [PubMed] [Google Scholar]
- 36.Geist R, Grdisa V, Otley A. Psychosocial issues in the child with chronic conditions. Best Pract Res Clin Gastroenterol. 2003;17(2):141–152. doi: 10.1016/s1521-6918(02)00142-7. [DOI] [PubMed] [Google Scholar]
- 37.Haire-Joshu D, Heady S, Thomas L, Schechtman K, Fisher EB., Jr Depressive symptomatology and smoking among persons with diabetes. Res Nurs Health. 1994;17(4):273–282. doi: 10.1002/nur.4770170406. [DOI] [PubMed] [Google Scholar]
- 38.Zimmet P, Turner R, McCarty D, Rowley M, Mackay I. Crucial points at diagnosis. Type 2 diabetes or slow type 1 diabetes. Diabetes Care. 1999;22(Suppl 2):B59–B64. [PubMed] [Google Scholar]
- 39.Tibbs TL, Haire-Joshu D. Avoiding high-risk behaviors: smoking prevention and cessation in diabetes care. Diabetes Spectr. 2002;15(3):164–169. [Google Scholar]
- 40.Sherman JJ. The impact of smoking and quitting smoking on patients with diabetes. Diabetes Spectr. 2005;18(4):202–208. [Google Scholar]


