Abstract
Mitral regurgitation (MR) is defined as the loss of the smooth and adequate trimming closure of the mitral valve, which results in the reflux of blood from the left ventricle into the left atrium during systole. The functional competence of the mitral valve relies on the proper and coordinated interaction of the following structures: the mitral annulus, and leaflets, chordate tendineae, papillary muscles, left atrium and the left ventricles.
This article will describe the echocardiography assessment of the mitral valve regurgitation with special emphasis on the trans-esophageal and 3D echocardiography. The echocardiography images were all original with special attention to the unique surgical view of the images.
Keywords: Echocardiography of the mitral regurgitation, 3D echo
1. Etiology of the mitral regurgitation
The etiology of Mitral regurgitation is variable, Myxomatous degenerative or floppy mitral valve accounts (20–70%), rheumatic heart disease (3–40%), ischemic heart disease (13–40%) and infectious endocarditis (10–12%) (Enriquez-Sarano et al., 2009) (see Table 1).
Table 1.
Etiology of mitral regurgitation.
| Valvular-leaflets | Annulus |
| • Myxomatous mitral valve disease | • Calcification |
| • Rheumatic endocarditis | • Endocarditis |
| • Endocarditis | Papillary muscles |
| • Congenital-cleft | • Ischemia |
| Chordae | • Infiltrative disorders |
| • Fused/inflammatory | Left ventricular dilatation & functional regurgitation |
| • Torn/Trauma | |
| • Degenerative | |
| • Endocarditis |
Carpentier et al. (1980) had proposed three pathoanatomic types of mitral regurgitation, based on leaflet and chordal motion: (1) normal leaflet (chordal) motion, (2) leaflet prolapse (excessive chordal motion) and (3) restricted leaflet or chordal motion.
2. MR echocardiography
The echocardiographic assessment of the mitral valve can first provide a baseline evaluation to identify etiology and quantify the severity of MR. It will assess and quantify the left ventricular function and dimensions. It provides annual surveillance of the left ventricular function, estimated ejection fraction (EF) and the left ventricular end-systolic dimension (LVESD) in asymptomatic sever MR. Finally the role of echocariography is to assess the adequacy of the surgical correction of the MR intraoperatively and postoperatively.
Echocardiography is the diagnostic tool of choice to assess the patients with MR. The identification of the etiology behind the mitral dysfunction is of paramount importance for the management decisions. The use of trans-esophageal echo and particularly intra-operatively, provides a precise assessment of the different components of the mitral valve and all the contributing factors to the failed function of the mitral valve function and helps the surgical decision on the most appropriate technique in achieving the best result of surgical repair (Figs. 1–18).
Figure 1.
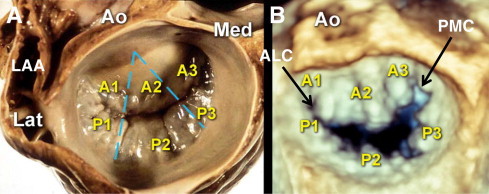
(A) Surgical view of the mitral valve after left atriotomy. Note: left atrial appendage (LAA) is located at the left side of the surgeon towards the head of the patient lying on the operating table, and aorta (AO) is located anterior. (B) Corresponding view acquired by 3D TEE zoom mode. Ao = aorta, ALC = anterolateral commissure, PMC = posteromedial commissure, A1 = anterolateral segment, A2 = anteromiddle segment, A3 = anteromedial segment, P1 = posterolateral scallop, P2 = posteromiddle scallop, P3 = posteromedial scallop, Lat = lateral of the patient, Med = medial of the patient.
Figure 2.
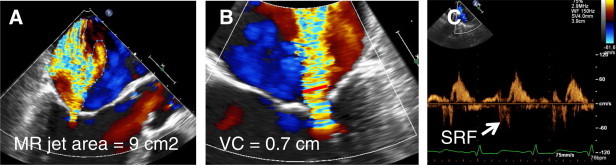
Transesophageal Echo (TEE) views showing severe mitral regurgitation. (A) TEE long axis view demonstrating severe ischemic mitral regurgitation (MR) with color flow MR jet area = 9 cm2 compatible with severe MR. (B) TEE 4-chamber view of the same patient measuring vena contracta width (VC) at 0.7 cm (red line) confirming severe MR. (C) Pulmonary venous inflow Doppler sampling right upper pulmonary vein showing systolic reversal flow (SRF) which is persistent with severe MR.
Figure 3.
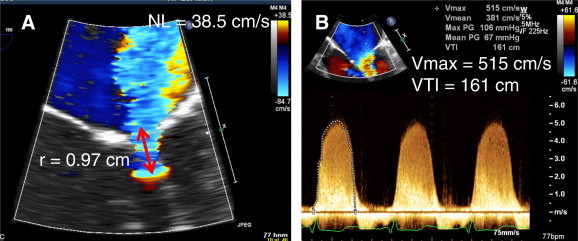
Quantitative grading of the severity of mitral regurgitation (MR) in same patient of Fig. 2, using PISA method. Effective Regurgitant Orifice Area (EROA) = 2 tc^X NL/Vmax which comes 0.44 cm2, compatible with severe MR. Regurgitant nvolume = EROA X VTI which is calculated as 71 ml/beat confirming severe MR. NL = Nyquist limit, r = radius of proximal isovelocity surface area (red arrow), Vmax = maximum velocity of MR jet, VTI = velocity time integral.
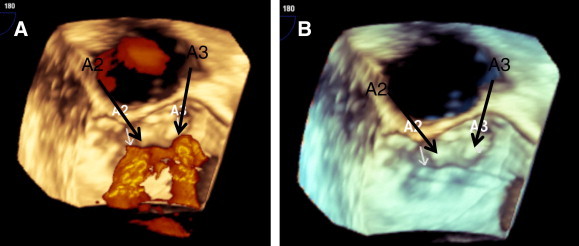
Figure 4.
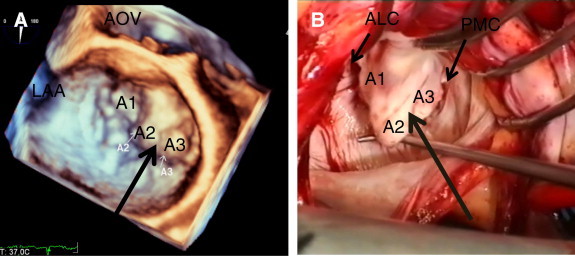
3D TEE- surgery correlation of a patient with severe prolapse of A2 and A3 (two large arrows) in a degenerative (myxomatous) mitral valve. (A) 3D TEE surgical view of the mitral valve with severe prolapse of the anterior mitral leaflet at A2, A3 segments. (B) Corresponding view of surgical demonstration of mitral valve showing severe prolapse of the A2 and A3 due to elongated chorda. AOV = aortic valve, LAA = left atrial appendage, A1 = lateral segment of the anterior mitral leaflet, A2 = middle segment of the anterior mitral leaflet, A3 = medial segment of the anterior mitral leaflet, ALC = anterolateral mitral valve commissure, PMC = posteromedial mitral valve commissure.
Figure 5.
Surgical view of the mitral valve, same patient of Fig. 4. (A) Two jets of severe mitral regurgitation (MR) is noted directed posteriorly, originating from the severe prolapse/ partial flail middle (A2) and medial (A3) segments of the anterior mitral leaflet (AMVL). Note: no color flow seen originating from lateral segment of the AMVL or posterior mitral leaflet. (B) same view with suppressed color to visualize origins of MR.
Figure 6.
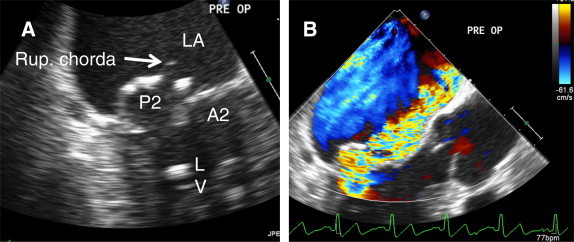
2D TEE long axis view of the mitral valve (MV) in a patient with myxomatous degenerative changes. (A) Flail middle scallop (P2) of the posterior MV leaflet noted (PMVL) with ruptured chorda. (B) Color flow is showing severe eccentric anteriorly directed jet of MR. LA = left atrium, A2 = middle segment of the anterior mitral leaflet, LV = left ventricle.
Figure 7.
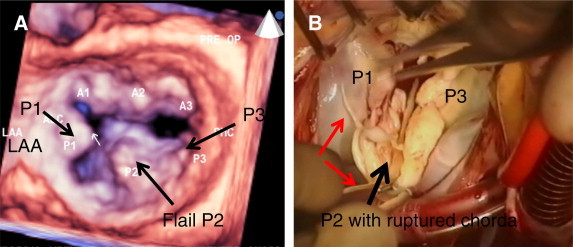
3D TEE- surgery correlation of the mitral valve (MV) with flail middle scallop (P2) of the posterior mitral valve leaflet (PMVL) in the same patient of Fig. 6. (A) 3D TEE surgical view of the MV with large bulky flail P2. (B) Corresponding view of the surgical demonstration of the MV during quadrangular resection of the flail P2. Note: multiple ruptured chordae tendineae (red arrows). P1 = lateral scallop of the PMVL, LAA = left atrial appendage, P3 = medial scallop of the PMVL.
Figure 8.
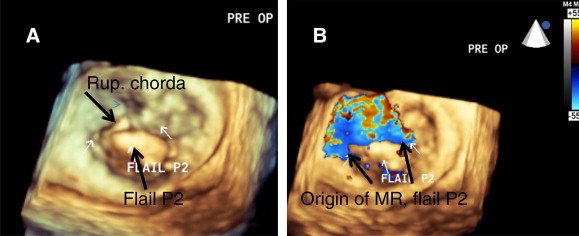
3D TEE full volume acquisition of the mitral valve of same patient of Fig. 7. (A) Surgical view with suppressed color is showing flail P2 with ruptured chorda. (B) Same view with color flow demonstrating eccentric anteriorly directed jet of severe MR originating from the large gap, created due to flail P2 (large arrows). Rup. chorda = ruptured, P2 = middle scallop of the posterior mitral leaflet.
Figure 9.
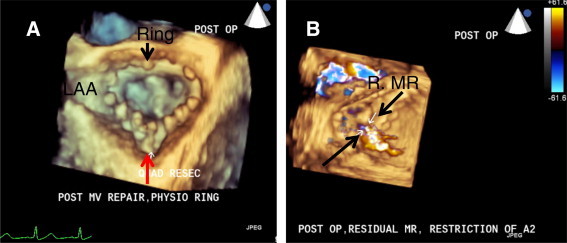
3D TEE surgical view of the previous mitral valve after repair. (A) Quadrangular resection of the flail P2 was done. Suture line of the repair is noted (red arrow). Complete ring (Physio ll annuloplsty ring) was sutured for preventing future dilatation. (B) Color flow is showing trivial residual mitral regurgitation originating from the site of the quadrangular resection repair. LAA = left atrial appendage, R. MR = residual mitral regurgitation.
Figure 10.
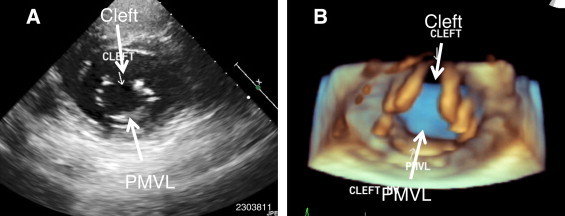
Isolated cleft mitral valve in a 39-year-old female with severe mitral regurgitation. (A) Transthoracic 2D echo in parasternalphort axis view showing cleft anterior mitral leaflet in diastole. Note: isolated cleft usually opens towards the aorta while in cleft associated with atrioventricular septal defect, opening is towards the tricuspid valve. (B) Transthoracic 3D echo study in same view showing the cleft (trifoliate mitral valve).
Figure 11.
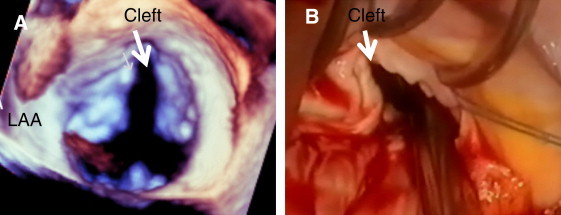
3D TEE- Surgery correlation of the cleft mitral valve in the same patient of Fig. 10. (A) 3D TEE surgical view of the trifoliate mitral valve with complete cleft at the middle of the anterior mitral valve leaflet. (B) corresponding view of the surgical demonstration of the cleft with thickened irregular free margins. LAA = left atrial appendage.
Figure 12.
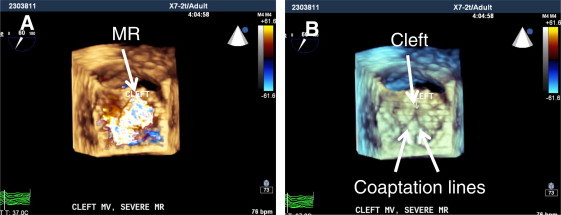
3D TEE full-volume acquisition of the mitral valve (MV) in same patient of Fig. 10, showing surgical view of the cleft MV. (A) mitral valve in systole demonstrating severe mitral regurgitation (MR) mostly origination from the cleft site of anterior mitral leaflet (arrow). Note: in older patients with cleft, due to secondary changes in coaptation line with posterior mitral leaflet (PMVL) and dilatation of the mitral annulus, degree of MR will progress. (B) Same view of mitral valve with color suppress to visualize site of the cleft and line of coaptation with PMVL (arrows).
Figure 13.
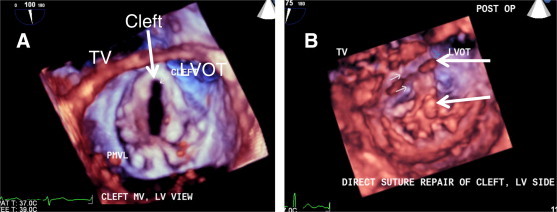
Pre and post- op comparison of the left ventricular (LV) side of the mitral valve MV) in same patient with cleft MV. (A) Pre-op, 3D TEE zoom-mode acquisition of the MV at systole showing cleft of the anterior mitral leaflet oriented towards LVOT. (B) Post-op, same view of the MV in systole after direct suture closure of the cleft (arrows).
Figure 14.
2D TEE views of mitral valve in a 11- year- old female with severe mitral regurgitation. (A) 4-chamber view showing thickened mitral valve leaflets with diastolic doming (hokey-teak shape, arrows). Mitral annulus is severely dilated. (B) Same view with color Doppler demonstrating severe central and posteriorly directed jet of mitral regurgitation. LV = left ventricle, RV = right ventricle.
Figure 15.
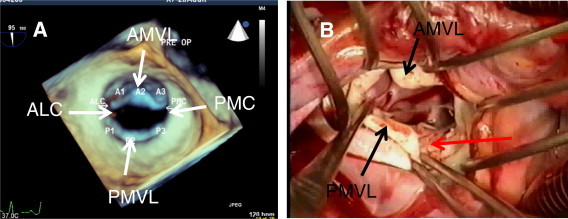
3D TEE-surgery correlation of the same patient of Fig. 14. (A) 3D TEE surgical view of mitral valve (MV) showing diastolic doming and mildly restricted leaflets. (B) Surgical demonstration of the MV prior to repair. Note: calcified free margins of the mitral leaflets. Verrucous non-bacterial endocarditis and erosion of the free margins of mitral leaflets are pathognomonics of rheumatic involvement of the MV (red arrow). 3D TEE is not very sensitive to detect calcification of the leaflets due to poor spatial resolution. ALC = anterolateral commissure, PMC = posteromedial commissure, AMVL = anterior mitral valve leaflet, PMVL = posterior mitral valve leaflet.
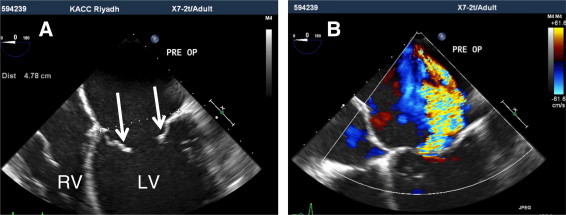
Figure 16.
Transthoracic echo in a 60-year-old male with severe functional mitral regurgitation (ischemic mitral regurgitation). (A) Apical 4-chamber view in systole showing mitral valve with structurally normal leaflets. Mitral leaflets are coapting in LV side due to severe tethering. (B) Color Doppler with lower Nyquist limit is demonstrating severe mitral regurgitation (MR) reaching right upper pulmonary vein (red arrow). PISA radius (r) is 1.0 cm which is compatible with severe MR. LV = left ventricle, LA = left atrium.
Figure 17.
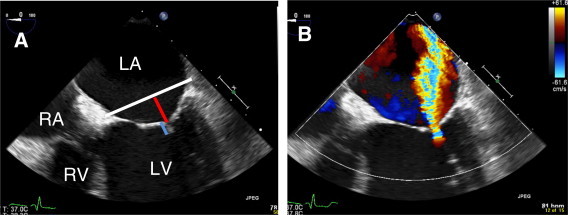
2D TEE views of same patient of Fig. 16. (A) 4-chamber view of mitral valve showing severe tethering of mitral leaflets. Coaptation depth = 1.1 cm (blue line) and coaptation length = 0.6 cm. (B) same view with color Doppler demonstrating severe central and posteriorly directed jet of mitral regurgitation (MR) due to lack of leaflets coaptation as is seen in functional and ischemic MR. LV = left ventricle, RV = right ventricle, LA = left atrium, RA = right atrium.
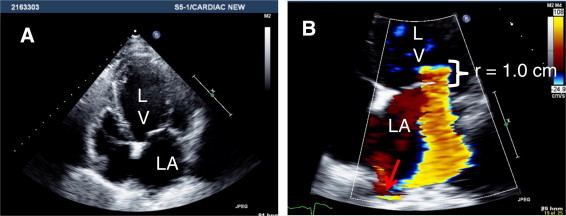
Figure 18.
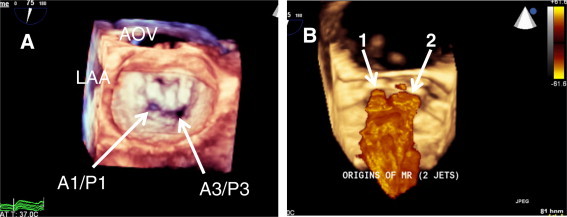
3D TEE surgical view of the mitral valve (MV) in the same patient of Fig. 16. (A) Full-volume acquisition of the MV at mid systole showing two gaps at the coaptation line, one between A1 and P1 and second larger, between A3 and P3. (B) same view with full-volume color Doppler demonstrating two jets of posteriorly directed severe mitral regurgitation. Note: Smaller jet (1) is originating between A1 and P1 and larger jet (2) between A3 and P3. AOV = aortic valve, LAA = left atrial appendage, A1 = lateral segment of the anterior mitral valve leaflet (AMVL), A3 = medial segment of the AMVL, P1 = lateral scallop of the posterior mitral valve leaflet (PMVL), P3 = medial scallop of the PMVL.
The echocardiographic assessment and quantification of MR severity is often challenging and may requite both a qualitative and quantitative approach. Proper assessment of the mitral valve structure, Doppler echocardiography and quantitative parameters should all be considered to assess the severity of MR. There are specific signs of severity that have been recognized. The specific signs include the presence of the vena contracta width of >0.7 cm with a central regurgitant jet cover > 40% of the left atrium, and a systolic flow reversal in the pulmonary veins, a prominent flail mitral valve leaflet and ruptured chordate. The quantitative parameters include an effective regurgitate orifice area > 40 cm2, a regurgitate volume > 60 ml, and a regurgitant fraction > 50%. In order to adequately assess the severity of MR, all these parameters should be assessed in addition to the measurement of the pulmonary artery pressure and LV function and dimensions (Thomas et al., 1999).
References
- Carpentier A., Chauvaud S., Fabiani J.N. Reconstructive surgery of mitral incompetence:ten-year appraisal. J. Thorac. Cardiovasc. Surg. 1980;79:338–348. [PubMed] [Google Scholar]
- Enriquez-Sarano M., Atkins C.W., Vahanian A. Mitral regurgitation. Lancet. 2009;373:1382–1394. doi: 10.1016/S0140-6736(09)60692-9. [DOI] [PubMed] [Google Scholar]
- Thomas L., Foster E., Hoffman J.E., Schiller N.B. The mitral regurgitation index: an echocardiographic guide to severity. J. Am. Coll. Cardiol. 1999;33(7):2016–2022. doi: 10.1016/s0735-1097(99)00111-4. [DOI] [PubMed] [Google Scholar]


