Abstract
Objective
We examined receipt of cervical cancer screening and determinants of screening for women with intellectual disabilities in one Southeastern state.
Methods
Using medical records data from 2006 through 2010 for community-dwelling women with intellectual disabilities who were 18–65 years of age (n=163), we employed descriptive and bivariate statistics and a multivariate regression model to examine receipt of cervical cancer screening and the determinants of cervical cancer screening across women's sociodemographic and health-care provider characteristics.
Results
Of women 18–65 years of age with intellectual disabilities, 55% received a Papanicolaou (Pap) test during 2008–2010, markedly below the Healthy People 2020 targets or rates of Pap test receipt of women without intellectual disabilities. Women with intellectual disabilities who lived in residential facilities, those who lived in rural communities, and those who had an obstetrician/gynecologist had higher rates of receipt of care than other women with intellectual disabilities.
Conclusions
Assertive measures are required to improve the receipt of cervical cancer screening among women with intellectual disabilities. Such measures could include education of women with intellectual disabilities, as well as their paid and family caregivers, and incentives for health-care providers who achieve screening targets.
Cervical cancer, once the leading cause of U.S. women's cancer deaths, is now treatable if detected early. Death rates have declined in the past 50 years due largely to an increased number of administered Papanicolaou (Pap) tests,1,2 which detect precancerous and cancerous cervical cells. An estimated 85% of U.S. women received a Pap test according to clinical guidelines in 2008, which is lower than the Healthy People 2020 target screening goal of 93%.3
Some women, including those who are uninsured, still face barriers to receipt of Pap screening.4 Cost leads some women to forgo these screenings.5 For many U.S. women, reproductive health care is delivered separately from primary care,6 which leads to fragmented care.4,7,8 Further, the specialty of a woman's provider is important; women who receive some care from a gynecologist have higher rates of Pap test receipt than women who see generalists.8,9
Women from vulnerable subpopulations, including women with a range of disabilities, do not receive preventive screenings at the recommended rates.10–12 Women with intellectual disabilities (defined as women with an IQ two or more standard deviations below the mean who have difficulties in two or more adaptive areas of daily living evident before age 18 years)13 have lower-quality health care (e.g., receipt of care when needed and satisfaction with care) and overall health than women without intellectual disabilities,10,14,15 including low rates of Pap test screenings.16–18 One national study found that women with intellectual disabilities were 72% less likely than women without disabilities to have received screening for cervical cancer.18 Thirty-nine percent of women in another study had Pap tests within the past three years.10
Unique barriers impede women with intellectual disabilities from receiving Pap tests, including the patients' limited transportation to and from appointments19–21 as well as their anxiety and lack of knowledge about pelvic exams.22,23 Health professionals often use medical equipment that is inaccessible to people with mobility impairments, lack training and knowledge about intellectual disabilities,15,19 or hold discriminatory social attitudes.24 Some physicians do not recommend Pap tests for women with intellectual disabilities due to unsuccessful prior examination attempts, the patients' need for sedation, or the patients' lack of insurance.21 Family members may discourage or decline screenings when they are recommended by health professionals,21 and women who live at home with family receive Pap tests at lower rates than other women with intellectual disabilities.10,25
The need for Pap tests in this population has been questioned. Researchers have found lower incidence of cervical cancer but higher incidence of cancer of the corpus uteri and ovaries in women with intellectual disabilities compared with women without intellectual disabilities.26,27 Some researchers and medical professionals argue that screening guidelines may not apply to this group of women because of presumed low rates of sexual intercourse and low incidence of abnormal cervical cytology.28,29 However, women with intellectual disabilities may be unwilling to disclose their sexual histories in the presence of caregivers who accompany them to the examination, leading doctors to erroneously believe these women are not sexually active.19 Taken on balance, the women's lack of knowledge about sexually transmitted diseases,30 their exceptionally high rates of sexual assault victimization,31 and the physicians' lack of knowledge about the women's sexual histories support regular Pap tests for women with intellectual disabilities.
The Surgeon General's Closing the Gap report called for comprehensive measures to increase preventive screenings for adults with intellectual disabilities.32 However, the existing evidence of Pap test rates of women with intellectual disabilities has been based on self-reported or proxy-reported (i.e., caregiver) interview data. Estimates of accurate Pap test recall by women without intellectual disabilities range from 65% to 89%. Overreporting may occur because of social desirability bias.33 In addition, problems with telescoping, or reporting that an exam occurred more recently than it actually did, may also be prevalent.33,34 Women with intellectual disabilities often have limited knowledge or understanding of the exam23 and may be unable to accurately report receipt or may confuse routine care such as a pelvic exam with the Pap test.33,34 Caregiver or proxy reports can also be problematic not only for the recall difficulties outlined previously, but also because the reporter may lack knowledge about the woman's medical care. Therefore, it is important to establish rates of cervical cancer screening receipt from sources other than self- and proxy-reported data.
This study aimed to (1) determine rates of Pap test receipt for women with intellectual disabilities from the women's medical records, which are valid sources of data for receipt of this type of testing;34 and (2) identify the determinants of such screening.
METHODS
We analyzed retrospective medical record data obtained as part of a larger project that included a multisite, randomized controlled trial of an intervention to promote cervical and breast cancer screening among women with intellectual disabilities.35
Site recruitment
Full details of our recruitment and informed consent procedures are available elsewhere.36 Briefly, the study began by identifying potential partner agencies across one Southeastern state in the U.S. The research team contacted community colleges, community rehabilitation programs, and mixed residential and vocational sites that provided services to adults with intellectual disabilities. In the state where this study was conducted, community colleges offer compensatory education programs, which are free educational programs for adults with intellectual disabilities. Sites were asked to help identify women from their program who met study criteria, provide an on-site instructor to deliver the health intervention being tested after receiving training from the research team, and assist the research team in maintaining contact with the participants during the course of the study. Of the 45 programs that were initially contacted, 21 (47%) agreed to participate in the study. These 21 sites were located in 16 counties geographically dispersed across the state and included both rural and urban communities. Women resided in 27 counties across the state.
Participant recruitment
The research team held information sessions at each participating site with women who had intellectual disabilities, site staff, and any interested caregivers or guardians. At these sessions, research team members reviewed the purpose of the study and the consent forms and then presented study information in multiple formats, including a video, group discussion, and consent forms with pictures. The team first obtained consent from each woman and then from her legal guardian, if applicable. In addition, the group reviewed the Health Insurance Portability and Accountability Act (HIPAA) of 1996 together and then the team gathered the signatures required for release of medical information from medical practices.
Enrollment criteria for the randomized controlled trial included female, ≥18 years of age, with an intellectual disability, and able to participate in a brief, in-person interview. Among 269 potential participants, 203 (75%) agreed to participate in the study and release medical records to the research team. Four women withdrew from the study before their medical records were collected. In addition, for the purposes of the study of medical record analysis, we excluded women for whom we did not have medical records and women who were older than 65 years of age (to be consistent with the U.S. Preventive Services Task Force [USPSTF] screening guidelines that were in place at the time data were collected).37 An additional seven women were excluded for missing covariates. These exclusions yielded a final analytic sample of 163 women.
All women participated in interviews with research staff to measure their knowledge of cervical cancer screening, answering questions such as, “What is a Pap test?” and “How often should you receive a Pap test?,” and were paid $15 for each interview.23,35 The research team conducted baseline interviews from September 2009 to December 2010 to measure the women's knowledge and determine the names of their physicians.
Procedures
We requested medical record data from 2006 through 2010 from the health-care providers of all study participants. During their initial interview with research staff, participants provided the names of any doctor or other health-care provider who had provided general care, Pap tests, or breast exams. Many women were uncertain of the name of their doctor or only knew partial information about the doctor. With assistance from staff and caregivers, and with the women's permission, we attempted to identify physicians for all five target years. We experienced greater success (99%) in physician identification for 2010 and less success (e.g., 73% in 2006) for earlier years.
Once we identified the physician or medical practice, we faxed information request packets to each medical practice. The packet included a letter from the project manager, a data abstraction form, and a signed HIPAA consent form. Abstraction forms requested dates of physicals, Pap tests, and mammograms for each year in the study period; health-care providers were to return a value of NR (not received) for any screening not received in that particular year. We asked practices to complete the abstraction form and fax it back to a secure fax machine. After three weeks, the research team called practices that had not responded and faxed the packet again. This procedure was repeated as necessary. Obtaining abstraction forms took multiple attempts, ranging from a single request to 10 contacts from research staff. Details of the abstraction process are available elsewhere.38 Medical record data collection occurred from November 2009 through September 2012.
Various practice staff, including physicians, nurses, and medical record personnel, completed the returned abstraction forms. Among this sample of women 18–65 years of age, Pap test data were obtained for 163 women during the three-year period 2008–2010, yielding a response rate of 82%.
Measures
Dependent variable: receipt of Pap.
We created a binary variable to define Pap test receipt or nonreceipt in each year from 2006 through 2010 for each woman. Point prevalence estimates were determined for each year from 2006 through 2010. We created a second binary variable to define Pap test receipt or nonreceipt at any point from 2008 through 2010, in accordance with USPSTF guidelines current at the outset of the study.37
To identify determinants of receipt of Pap tests during the three-year period, we examined various demographic variables and other factors including residence, living situation, insurance type, history of having children, medical practice type, guardianship status, knowledge of Pap test, and whether or not someone accompanied the woman into the medical examination room. Demographic variables reported by the collaborating sites included the women's guardianship status, race, age, and severity of impairment. We obtained information about the severity of impairment from the women's educational or employment records. The U.S. Census Bureau's39 designation for each woman's home community determined whether she lived in an urban or rural residence. The women reported living situation, history of having a child, and if someone accompanied them into the examination room during medical appointments. We measured knowledge of Pap test during the in-person interview with research staff using a standardized measure.23 The research staff asked each participant to define or describe a Pap test and to state how often women should receive the exam. The staff coded responses as correct or incorrect, depending on whether they accorded with the clinical guidelines. The woman's health insurance type and the medical practice type were obtained from the medical practices.
For data analysis, we used descriptive statistics to report the demographic and other characteristics of the sample and to estimate receipt of cervical cancer screening. We focused on two outcomes: (1) receipt of cervical cancer screening each year from 2006 through 2010 and (2) receipt of cervical cancer screening according to clinical guidelines from 2008 through 2010 (i.e., receipt of cervical cancer screening at any point during the years 2008–2010). Multivariate logistic regression models were estimated to determine the association of various demographic and health-care provider characteristics on the women's likelihood of receiving cervical cancer screening. We performed standard diagnostic tests for collinearity, which was not a concern with these variables. Analyses were conducted using Stata® statistical software version 12.40
RESULTS
Characteristics of the study sample are shown in Table 1. The entire sample was approximately evenly divided between white (55%) and African American (43%) women with a mean age of 40 years. Nearly all women had public health insurance. About half (55%) of the sample received a Pap test in 2008, 2009, or 2010.
Table 1.
Characteristics of a sample of community-dwelling women with intellectual disabilities aged 18–65 years living in North Carolina, 2006–2010 (n=163)
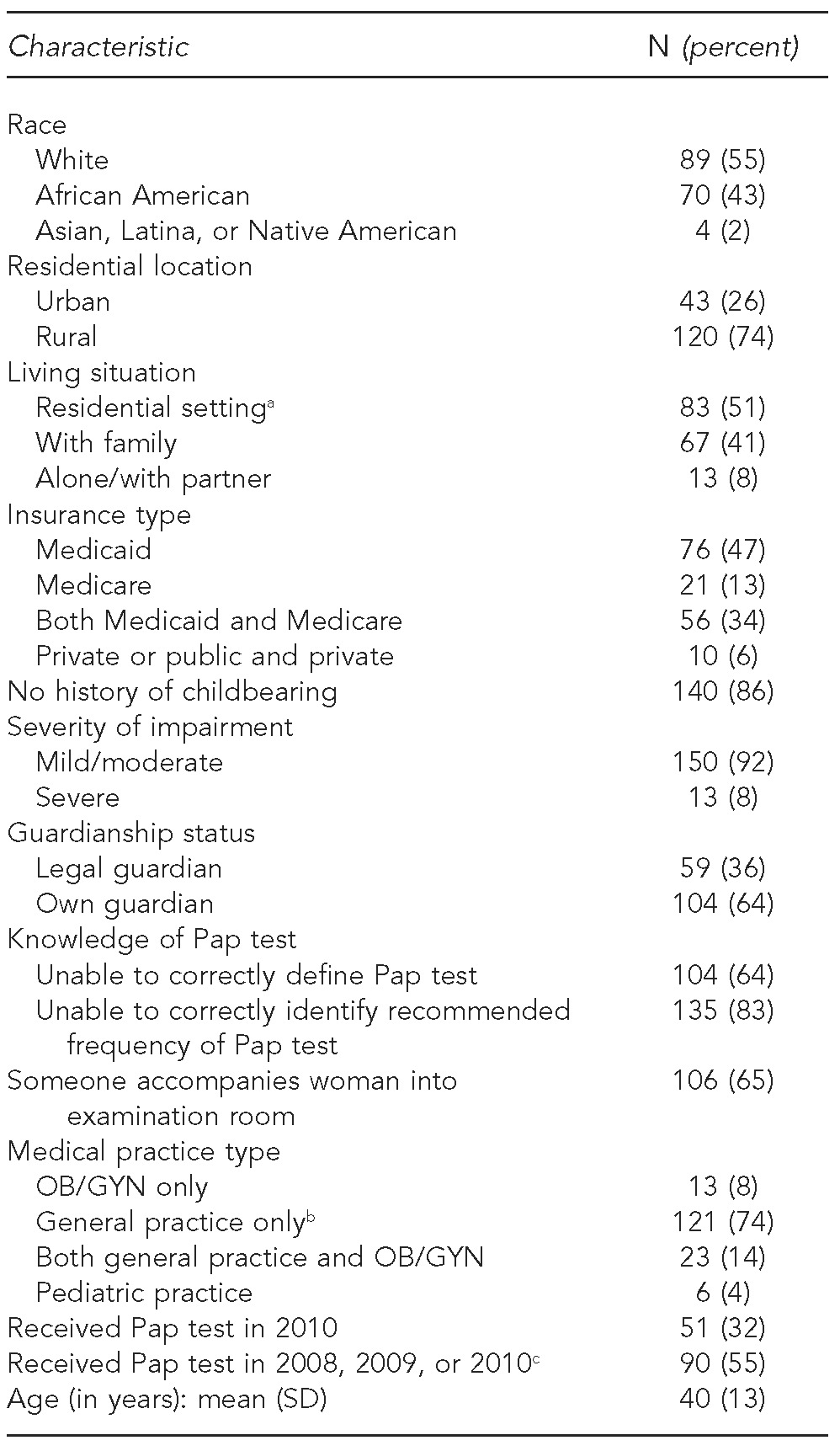
aIncludes group home, supervised apartment, adult foster care, and nursing facility
bIncludes family practice/primary care, internal medicine, residential provider, health department, and rural health clinic
cThe rates of Pap test receipt for 2008–2010 were presented based on the current U.S. Preventive Services Task Force guidelines.
Pap = Papanicolaou
OB/GYN = obstetrician/gynecologist
SD = standard deviation
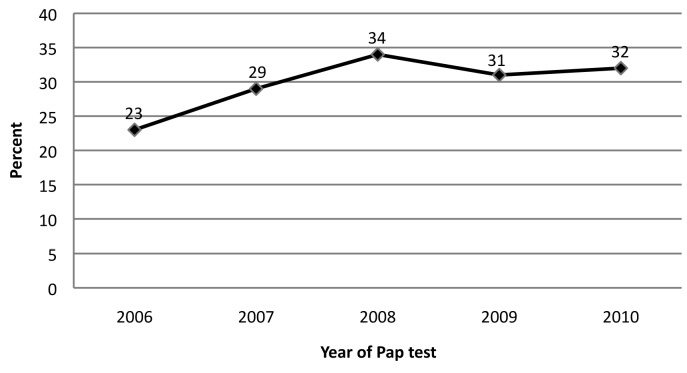
The Figure shows the percentage of the sample that received a Pap test in each year from 2006 through 2010. Rates were relatively stable over time, ranging from 23%–34% of women.
Figure.
Percentage of sample of community-dwelling North Carolina women with intellectual disabilities aged 18–65 years receiving a Pap test: 2006–2010 (n=163)
Pap = Papanicolaou
Results of the multivariate logistic regression model predicting receipt of Pap tests are shown in Table 2. The characteristics associated with receiving Pap tests included living situation, residence location, and medical practice type of women with intellectual disabilities. In other words, women who lived at home with family caregivers were less likely to receive Pap screening (odds ratio [OR] = 0.21, 95% confidence interval [CI] = 0.08, 0.52) than women living in residential settings. Women who lived in a rural setting also had a greater likelihood of receiving Pap tests in any of the three years (OR=3.43, 95% CI 1.40, 8.40) than women who lived in urban settings. Women who had a general practitioner as their physician were less likely to receive the screening (OR=0.13, 95% CI 0.02, 0.81) than women who had an obstetrician/gynecologist (OB/GYN) as their physician. In additional analyses, controlling for all model covariates, there were no statistically significant differences between women who lived alone or with a partner in comparison with women who lived with family caregivers (data not shown).
Table 2.
Multiple logistic regression model predicting receipt of Pap test during a three-year period among a sample of community-dwelling North Carolina women aged 18–65 years with intellectual disabilities (n=163), 2008–2010
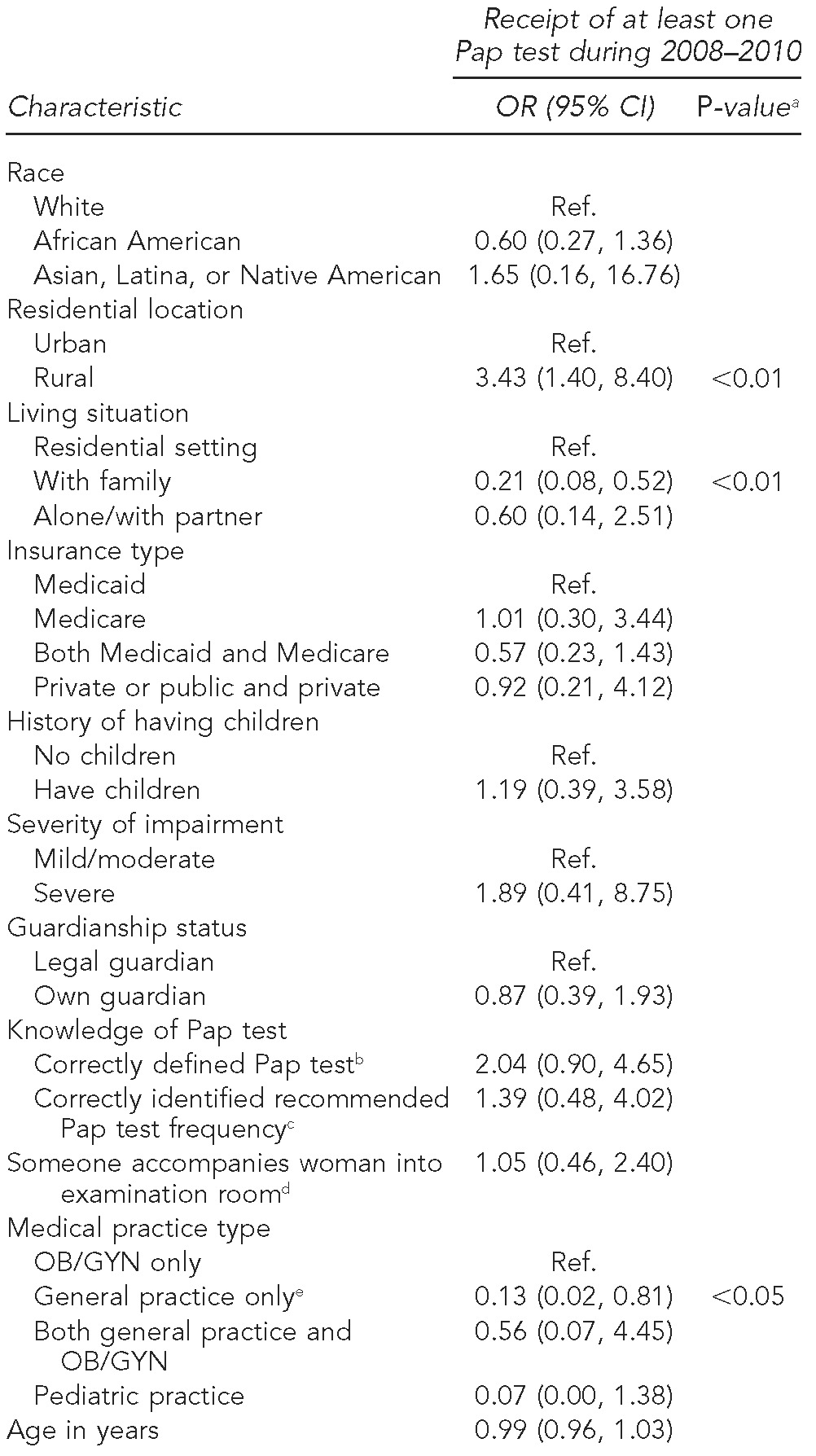
aOnly p-values for statistically significant tests (i.e., p<0.05) are shown.
bThe reference category was women who could not correctly define Pap test.
cThe reference category was women who could not correctly identify the recommended frequency of receiving a Pap test.
dThe reference category was not having anyone accompany the woman into the examination room.
eIncludes family practice/primary care, internal medicine, residential provider, health department, and rural health clinic
Pap = Papanicolaou
OR = odds ratio
CI = confidence interval
Ref. = reference group
OB/GYN = obstetrician/gynecologist
We also conducted sensitivity analyses to explore the relationship between receipt of physical examinations, defined as a general primary care visit, and Pap tests. Sixty-four percent of the sample received a physical exam in 2010 compared with 32% of women who received a Pap test that year. When we estimated new regression models including a covariate for receipt of physical exam, there were no changes in the significance of any other model covariates or in the direction or magnitude of effects (data not shown).
DISCUSSION
This study is the first analysis of determinants of cervical cancer screening for community-based women with intellectual disabilities using data from medical records (as opposed to self-reported or proxy-reported data). We found a three-year Pap test rate of 55%, which is far below both the 93% population target of Healthy People 2020 and the actual three-year national screening rate of 85% in 2008.3 Our rate of screening was, however, somewhat higher than the 39% screening rate reported for a sample from California in 1997.10
The trend in Pap tests was relatively stable during the years 2006–2010, ranging from a low of 23% in 2006 to a high of 34% in 2008. Our findings that women living at home with family caregivers were less likely to receive Pap tests corroborates recent evidence that rates of preventive screenings are generally worse for adults with intellectual disabilities who live at home rather than in residential settings.10,25 However, an unexpected finding was that women who lived in rural communities were more likely to receive screenings than those in urban communities, contrary to previous evidence of better Pap test rates for women without intellectual disabilities living in urban settings,41,42 suggesting that further research is warranted.
These findings suggest that (1) women with intellectual disabilities are not receiving cervical cancer screening at recommended rates or at rates similar to women without intellectual disabilities, (2) interventions to improve Pap test rates for women in the general population have failed to reach women with intellectual disabilities, and (3) there is a need for specialized screening guidelines for women with intellectual disabilities. Such guidelines could effectively include having health-care providers give women with intellectual disabilities adequate time, support, and preparation to understand the procedures.43 New guidelines should recommend screening for women whose sexual histories, including sexual assault victimization, cannot truly be known or are unlikely to be honestly reported in the presence of paid or family caregivers.
While there has been some discussion about if and how often women with disabilities should receive cervical cancer screening,28,29 current estimates of high sexual assault rates31 and limited knowledge of the women's sexual activity indicate that women with intellectual disabilities could benefit from screening with the proper support. In addition, the majority of women in our study reported that someone accompanies them to medical appointments, including into the examination room. While this support may be important in helping the women communicate with their physicians, women may be less likely to disclose sexual relationships, both consensual and coerced, in the presence of a caregiver.
Our finding that women living at home with family are screened at lower rates further emphasizes the need for targeted education of family caregivers about the importance of screenings. Previous research suggests that physicians may not recommend exams and/or family caregivers may refuse them.21 Therefore, educating physicians about the health of women with intellectual disabilities and ways to administer exams in a way that reduces their fear and anxiety is also warranted.
Limitations
This study was subject to several limitations. First, nearly all of the women were insured; as such, this study does not provide evidence about uninsured women with intellectual disabilities. Second, we were unable to collect evidence of why women did or did not receive exams. Third, we were not able to verify the accuracy of the medical record data that the health-care providers and medical practices provided. Fourth, the small sample size and use of a single state limited the study's generalizability. Finally, we could not determine if women had had a hysterectomy.
Strengths
The study also had important strengths. First, we report rates of Pap test receipt among a sample of geographically dispersed women who live in a range of community settings and receive care from a variety of medical practices. This sample closely represents the population of women with intellectual disabilities living in the state in which the sample resides. However, it is more racially diverse than the national population of women with intellectual disabilities.44 Second, our reliance on objective medical records eliminated recall bias, social desirability bias, and other problems associated with self-reported data. A final strength was that the women were not drawn from a single medical practice.
CONCLUSION
Medical record data indicate that women with intellectual disabilities receive cervical cancer screening at rates that are far below Healthy People 2020 targets. Women living in residential facilities, women in rural communities, and women who had OB/GYNs were more likely to be screened but were still largely underserved. Effective interventions are required to enable more women with intellectual disabilities to receive cervical cancer screening.
Footnotes
The protocol was approved by the University of North Carolina at Chapel Hill Institutional Review Board.
REFERENCES
- 1.National Institutes of Health (US) Fact sheet: cervical cancer. [cited 2012 Jan 23]. Available from: URL: http://report.nih.gov/NIHfactsheets/Pdfs/CervicalCancer%28NCI%29.pdf.
- 2.Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Altekruse SF, et al., editors. SEER cancer statistics review, 1975–2008. Bethesda (MD): National Cancer Institute (US); 2011. [cited 2012 Apr 15]. Also available from: URL: http://seer.cancer.gov/csr1975_2008. [Google Scholar]
- 3.Department of Health and Human Services (US), Office of Disease Prevention and Health Promotion. Healthy people 2020. [cited 2012 Jan 25]. Available from: URL: http://healthypeople.gov/2020/topicsobjectives2020/pdfs/HP2020objectives.pdf.
- 4.Ranji U, Salganicoff A. Menlo Park (CA): The Henry J. Kaiser Family Foundation; 2011. Women's health care chartbook: key findings from the Kaiser Women's Health Survey. [Google Scholar]
- 5.Rustgi SD, Doty MM, Collins SR. New York: The Commonwealth Fund; 2009. Women at risk: why many women are forgoing needed health care. [PubMed] [Google Scholar]
- 6.Weisman CS. Baltimore (MD): Johns Hopkins University Press; 1998. Women's health care: activist traditions and institutional change. [Google Scholar]
- 7.Institute of Medicine. Washington: National Academies Press; 2011. Clinical preventive services for women: closing the gaps. [Google Scholar]
- 8.Henderson JT, Weisman CS, Grason H. Are two doctors better than one? Women's physician use and appropriate care. Womens Health Issues. 2002;12:138–49. doi: 10.1016/s1049-3867(02)00134-2. [DOI] [PubMed] [Google Scholar]
- 9.Lewis BG, Halm EA, Marcus SM, Korenstein D, Federman AD. Preventive services use among women seen by gynecologists, general medical physicians, or both. Obstet Gynecol. 2008;111:945–52. doi: 10.1097/AOG.0b013e318169ce3e. [DOI] [PubMed] [Google Scholar]
- 10.Lewis MA, Lewis CE, Leake B, King BH, Lindemann R. The quality of health care for adults with developmental disabilities. Public Health Rep. 2002;117:174–84. doi: 10.1016/S0033-3549(04)50124-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reichard A, Stolzle H, Fox MH. Health disparities among adults with physical disabilities or cognitive limitations compared to individuals with no disabilities in the United States. Disabil Health J. 2011;4:59–67. doi: 10.1016/j.dhjo.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 12.Wisdom JP, McGee MG, Horner-Johnson W, Michael YL, Adams E, Berlin M. Health disparities between women with and without disabilities: a review of the research. Soc Work Public Health. 2010;25:368–86. doi: 10.1080/19371910903240969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Association on Intellectual and Developmental Disabilities. 11th ed. Washington: American Association on Intellectual and Developmental Disabilities; 2010. Intellectual disability: definition, classification, and systems of support. [Google Scholar]
- 14.Krahn GL, Hammond L, Turner A. A cascade of disparities: health and health care access for people with intellectual disabilities. Ment Retard Dev Disabil Res Rev. 2006;12:70–82. doi: 10.1002/mrdd.20098. [DOI] [PubMed] [Google Scholar]
- 15.Ward RL, Nichols AD, Freedman RI. Uncovering health care inequalities among adults with intellectual and developmental disabilities. Health Soc Work. 2010;35:280–90. doi: 10.1093/hsw/35.4.280. [DOI] [PubMed] [Google Scholar]
- 16.Havercamp SM, Scandlin D, Roth M. Health disparities among adults with developmental disabilities, adults with other disabilities, and adults not reporting disability in North Carolina. Public Health Rep. 2004;119:418–26. doi: 10.1016/j.phr.2004.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iacono T, Sutherland G. Health screening and developmental disabilities. J Policy Pract Intellect Disabil. 2006;3:155–63. [Google Scholar]
- 18.Parish SL, Saville AW. Women with cognitive limitations living in the community: evidence of disability-based disparities in health care. Ment Retard. 2006;44:249–59. doi: 10.1352/0047-6765(2006)44[249:WWCLLI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Kopac C, Fritz J, Holt R. Gynecologic and reproductive services for women with developmental disabilities. Clin Excell Nurse Pract. 1998;2:88–95. [PubMed] [Google Scholar]
- 20.Reichard A, Sacco TM, Turnbull H. Access to health care for individuals with developmental disabilities from minority backgrounds. Ment Retard. 2004;42:459–70. doi: 10.1352/0047-6765(2004)42<459:ATHCFI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Tyler CV, Zyzanski SJ, Panaite V, Council L. Nursing perspectives on cancer screening in adults with intellectual and other developmental disabilities. Intellect Dev Disabil. 2010;48:271–7. doi: 10.1352/1934-9556-48.4.271. [DOI] [PubMed] [Google Scholar]
- 22.Parish SL, Moss K, Richman EL. Perspectives on health care of adults with developmental disabilities. Intellect Dev Disabil. 2008;46:411–26. doi: 10.1352/2008.46:411-426. [DOI] [PubMed] [Google Scholar]
- 23.Parish SL, Swaine JG, Luken K, Rose RA, Dababnah S. Cervical and breast cancer-screening knowledge of women with developmental disabilities. Intellect Dev Disabil. 2012;50:79–91. doi: 10.1352/1934-9556-50.2.79. [DOI] [PubMed] [Google Scholar]
- 24.Brown AA, Gill CJ. New voices in women's health: perceptions of women with intellectual and developmental disabilities. Intellect Dev Disabil. 2009;47:337–47. doi: 10.1352/1934-9556-47.5.337. [DOI] [PubMed] [Google Scholar]
- 25.Bershadsky J, Taub S, Engler J, Moseley CR, Lakin KC, Stancliffe RJ, et al. Place of residence and preventive health care for intellectual and developmental disabilities services recipients in 20 states. Public Health Rep. 2012;127:475–85. doi: 10.1177/003335491212700503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patja K, Eero P, Iivanainen M. Cancer incidence among people with intellectual disability. J Intellect Disabil Res. 2001;45:300–7. doi: 10.1046/j.1365-2788.2001.00322.x. [DOI] [PubMed] [Google Scholar]
- 27.Sullivan SG, Hussain R, Threlfall T, Bittles AH. The incidence of cancer in people with intellectual disabilities. Cancer Causes Control. 2004;15:1021–5. doi: 10.1007/s10552-004-1256-0. [DOI] [PubMed] [Google Scholar]
- 28.Wilkinson JE, Cerreto MC. Primary care for women with intellectual disabilities. J Am Board Fam Med. 2008;21:215–22. doi: 10.3122/jabfm.2008.03.070197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilkinson JE, Culpepper L, Cerreto M. Screening tests for adults with intellectual disabilities. J Am Board Fam Med. 2007;20:399–407. doi: 10.3122/jabfm.2007.04.060210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Noonan Walsh P, Heller T, editors. Oxford: Wiley; 2002. Health of women with intellectual disabilities. [Google Scholar]
- 31.Wacker J, Macy R, Barger E, Parish S. Sexual assault prevention for women with intellectual disabilities: a critical review of the evidence. Intellect Dev Disabil. 2009;47:249–62. doi: 10.1352/1934-9556-47.4.249. [DOI] [PubMed] [Google Scholar]
- 32.Office of the Surgeon General (US) Closing the gap: a national blueprint for improving the health of individuals with mental retardation. Report of the Surgeon General's conference on health disparities and mental retardation; Washington: Department of Health and Human Services (US); 2002. [PubMed] [Google Scholar]
- 33.Howard M, Agarwal G, Lytwyn A. Accuracy of self-reports of Pap and mammography screening compared to medical record: a meta-analysis. Cancer Causes Control. 2009;20:1–13. doi: 10.1007/s10552-008-9228-4. [DOI] [PubMed] [Google Scholar]
- 34.Rauscher GH, Johnson TP, Cho YI, Walk JA. Accuracy of self-reported cancer screening histories: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2008;17:748–57. doi: 10.1158/1055-9965.EPI-07-2629. [DOI] [PubMed] [Google Scholar]
- 35.Parish SL, Rose RA, Luken K, Swaine JG, O'Hare L. Cancer screening knowledge changes: results from a randomized control trial of women with developmental disabilities. Res Soc Work Pract. 2012;22:43–53. [Google Scholar]
- 36.Swaine JG, Parish SL, Luken K, Atkins L. Recruitment and consent of women with intellectual disabilities in a randomized control trial of a health promotion intervention. J Intellect Disabil Res. 2011;55:474–83. doi: 10.1111/j.1365-2788.2011.01399.x. [DOI] [PubMed] [Google Scholar]
- 37.Preventive Services Task Force (US) The guide to clinical preventive services: recommendations of the U.S. Preventive Services Task Force. Washington: Agency for Healthcare Research and Quality (US); 2006. [Google Scholar]
- 38.Swaine JG, Parish SL, Ghosh S, Luken K, Wright GA. Obtaining medical records for women with intellectual disabilities in a community-based health promotion intervention. J Policy Pract Intellect Disabil. 2013;10:54–61. [Google Scholar]
- 39.Census Bureau (US) Census 2000 urban and rural classification. [cited 2011 Oct 25]. Available from: URL: http://www.census.gov/geo/www/ua/ua_2k.html.
- 40.StataCorp. Stata®: Version 12. College Station (TX): StataCorp; 2012. [Google Scholar]
- 41.Casey MM, Call KT, Klingner JM. Are rural residents less likely to obtain recommended preventive healthcare services? Am J Prev Med. 2001;21:182–8. doi: 10.1016/s0749-3797(01)00349-x. [DOI] [PubMed] [Google Scholar]
- 42.Coughlin SS, Thompson TD, Hall HI, Logan P, Uhler RJ. Breast and cervical carcinoma screening practices among women in rural and nonrural areas of the United States, 1998–1999. Cancer. 2002;94:2801–12. doi: 10.1002/cncr.10577. [DOI] [PubMed] [Google Scholar]
- 43.Swaine JG, Dababnah S, Parish SL, Luken K. Family caregivers' perspectives on barriers and facilitators of cervical and breast cancer screening for women with intellectual disability. Intellect Dev Disabil. 2013;51:62–73. doi: 10.1352/1934-9556-51.01.062. [DOI] [PubMed] [Google Scholar]
- 44.Human Services Research Institute; National Association of State Directors of Developmental Disabilities Services. National core indicators. [cited 2012 Aug 23]. Available from: URL: http://www.nationalcoreindicators.org.