Abstract
This case report describes the treatment of a 22-year-old girl who had incompetent lips with severe bimaxillary dentoalveolar protrusion. The treatment of choice for such patients is usually extraction of four first premolars and retraction of the anterior teeth. To maintain the extraction space, maximum anchorage is required. Mini-implants were used to provide maximum anchorage for obtaining a good facial profile.
Keywords: Mini-implants, Dentoalveolar, Protrusion, En masse, Anchorage, Spider Screws
1. Introduction
Protrusiveness and proclination of the maxillary and mandibular incisors along with increased procumbency of the lips is a condition known as bimaxillary dentoalveolar protrusion (Proffit et al., 2007). This condition is commonly seen in the Asian (Lamberton et al., 1980; Lew, 1989; Tan, 1996) as well as African–American populations (Fonseca and Klein, 1978; Rosa and Arvystas, 1978; Farrow et al., 1993; Scott and Johnston, 1999). Furthermore, it can be seen in other ethnic groups (Carter and Slattery, 1988; Dandajena and Nanda, 2003). The usual objective of orthodontic treatment of such condition includes the retraction and retroclination of maxillary and mandibular incisors with a resultant decrease in soft tissue procumbency and convexity (Bills et al., 2005). The treatment of choice for these patients is to extract all first bicuspids. In this case, maximum anchorage of the posterior teeth is of great importance for two reasons; to retract the anterior teeth to their greatest extent and increase the chances of correcting the profile.
With the introduction of dental implants (Roberts et al., 1989, 1990), mini-plates (Sugawara et al., 2004; Choi et al., 2005), micro-implants and mini-screws/implants (Park and Kwon, 2004; Park et al., 2001, 2005a,b,c, 2008) as anchorage, it has become possible to achieve absolute anchorage (Kanomi, 1997).
Therefore, this case report demonstrates the efficacy of mini-implants as an anchorage aid in the case of severe bimaxillary dentoalveolar protrusion with incompetent lips.
2. Case report
2.1. Diagnosis
A 22-year-old girl presented with the chief complaint of having lip protrusion. Facially, the patient exhibited a convex profile with incompetent lips. Intraorally, she had Class II canine and molar relationships (2 mm on the right and 1 mm on the left) with minimal maxillary and mandibular crowding. With respect to the facial midline, the upper and lower dental midlines were deviated to the right, 1 mm and 4 mm, respectively (Fig. 1).
Figure 1.

Pre-treatment intra-oral Photographs.
The lateral cephalogram (Fig. 2) and its tracing showed a Class I skeletal pattern with bimaxillary dentoalveolar protrusion (Table 1). As evidenced by the maxillary incisor to NA angle and distance, the maxillary incisor inclination was 34° and was 15 mm ahead of the NA line. With respect to the mandibular incisor, the axial inclination was 34° and 10 mm ahead of the NB line. Furthermore, IMPA was 97°. Upper and lower lips were protruded when compared to the E-line, 4 mm and 6 mm, respectively. Mandibular plane angle was hyperdivergent (NS-GoGn = 36°). The nasolabial angle was acute (83°). Overjet was 8.5 mm and the overbite was 2 mm. There were multiple restored teeth. There were no signs and symptoms of temporomandibular disorders.
Figure 2.

Pre-treatment lateral cephalogram.
Table 1.
Cephalometric measurements.
| Normal | Pre-treatment | Post-treatment | |
|---|---|---|---|
| SNA (°) | 82 ± 2 | 82 | 82 |
| SNB (°) | 80 ± 2 | 80 | 81 |
| ANB (°) | 2 | 2 | 1 |
| SN-GoGn (°) | 32 | 36 | 36 |
| NPog – FH (°) | 89 ± 3.9 | 81 | 82 |
| Upper Incisor to NA (°) | 32 | 34 | 28 |
| Upper Incisor to NA (mm) | 4 | 15 | 9 |
| Lower Incisor to NB (°) | 22 | 34 | 29 |
| Lower Incisor to NB (mm) | 4 | 10 | 6 |
| FMIA (°) | 65 | 46 | 56 |
| FMA (°) | 25 | 38 | 36 |
| IMPA (°) | 90 | 97 | 90 |
| E line: Upper (mm) | −4 | 4 | 0 |
| E line: Lower (mm) | −2 | 6 | 0 |
| Nasiolabial angle (°) | 85–90 | 83 | 94 |
| Overjet (mm) | 2 | 8.6 | 2 |
| Overbite (mm) | 2 | 2 | 1 |
2.2. Treatment objectives
Treatment objectives included the following: (1) align and level the teeth in both arches, (2) achieve Class I canine and molar relationship and ideal overjet and overbite, (3) obtain a balanced facial profile, and (4) improve smile esthetics.
2.3. Treatment plan
The treatment plan was retraction of the maxillary and mandibular anterior teeth. Therefore, all first bicuspids were extracted with maximum anchorage. This option is commonly used to reduce the patient’s lip procumbency (Lew, 1989; Tan, 1996; Kurz, 1997).
2.4. Treatment progress
After the extraction of all first bicuspids, fixed pre-adjusted Bi-Dimensional Edgewise appliances were used (i.e., 0.018 × 0.022 slot in the centrals and laterals, and 0.022 × 0.028 slot canine, bicuspids and molars).
After leveling and alignment, four orthodontic mini-implants (Spider Screw® HDC, Italy) self-drilling type, conical shape with 1.5 mm diameter and 8 mm length were implanted into the buccal alveolar bone between the maxillary and mandibular first molars and second bicuspids (Fig. 3).
Figure 3.
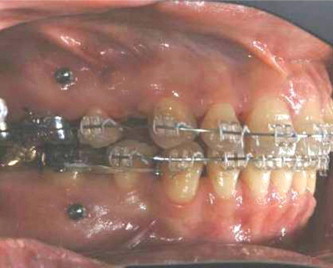
Mini-implants were perpendicularly inserted to the cervical bone. The mini-implants were positioned between the first molars and the second bicuspids.
A 0.018 × 0.022-inch St. St. arch-wire with anterior hooks was placed, Ni–Ti retraction force was applied from the maxillary and mandibular mini-implants and the six anterior teeth were retracted simultaneously.
After en masse movement, the treatment was completed with ideal arch-wires and cusp seating elastics. Lingual bonded retainers on the maxillary and mandibular six anterior teeth and circumferential clear retainers were delivered for both arches. The total treatment time was 20 months.
2.5. Treatment results
A Class I molar and canine relationship was established bilaterally. Ideal overjet (2 mm) and overbite (1 mm) was also achieved. The arches were well coordinated. The maxillary and mandibular dental midlines were coincident with one another as well as with the facial midline. Patients’ bimaxillary dentoalveolar protrusive profile was significantly reduced (Fig. 4).
Figure 4.

Post-treatment intra-oral Photographs.
According to the final superimposition, the maxillary anterior teeth were bodily retracted (6 mm) with intrusion (3 mm). The mandibular anterior teeth were retracted (4 mm) with uprighting (IMPA 90°). There were no significant changes to the position of both maxillary and mandibular first molars. The ANB angle did not change significantly (from 2° to 1°) as shown in Table 1.
All these changes contributed to improving the facial profile as there were significant profile changes in the patient’s lower facial third (Fig. 5). The upper and lower lips had been retracted, 4 mm and 6 mm, respectively in relation to the E-line, and her nasolabial angle had increased (from 83° pre-treatment to 94° post-treatment). No other skeletal or soft tissue changes were noted (Fig. 6).
Figure 5.

Pre- and post- treatment frontal lower third profile comparison.
Figure 6.
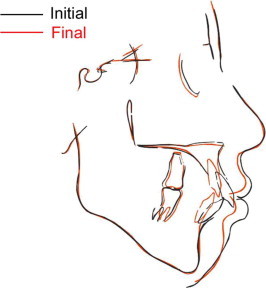
Post treatment cephalogram (a) and Pre- (Black) and post-treatment (Red) Cephalometric superimposition (b).
3. Discussion
Bimaxillary dentoalveolar protrusion, which is characterized by dentoalveolar flaring of both the maxillary and mandibular anterior teeth, with resultant protrusion of the lips and convexity of the face, is commonly seen in Asian populations (Lamberton et al., 1980). Facial esthetics is an important consideration in orthodontic treatment particularly when extractions are considered. It is accepted in orthodontics that extraction of permanent teeth reduces facial convexity (Lew, 1989; Tan, 1996; Kurz, 1997). On the basis of the patient’s chief complaint and the diagnosis of the malocclusion, extracting the maxillary and mandibular first bicuspids is a valid and viable option to decrease lip procumbency.
The advances in the utilizing bone anchorage such as retromolar implant (Roberts et al., 1990), onplants (Block and Hoffman, 1995; Armbruster and Block, 2001), palatal implants (Wehrbein et al., 1996a,b), mini-plates (Umemori et al., 1999), mini-screws (Costa et al., 1998) and mini-implants (Kanomi, 1997) make it possible to overcome previous limitation of orthodontic tooth movement and perform en masse movement in the desired direction. These armamentariums are becoming part of the orthodontic appliance system. As shown in the reported case, the use of mini-implants provided absolute anchorage for the desired tooth movement. Consideration has been made in placing the implant in a higher position to allow for an intrusive force vector during retraction of the incisors.
There have been different methods widely accepted in the literature for comparison of cephalometric headfilms, in other word superimposition. The most accepted one of assessing overall dentofacial change is to superimpose two cephalometric tracings with point registering at sells and the sella nasion (SN) line superimposed. This method is used in this case to show the final changes.
To date, clinical efficacy (Creekmore and Eklund, 1983; Kanomi, 1997; De Pauw et al., 1999; Park et al., 2001; Chae, 2006) and stability (De Pauw et al., 1999; Miyawaki et al., 2003) of temporary orthodontic skeletal anchorage devices have been widely described. With the use of the mini-implants, maximum en masse retraction of the maxillary and mandibular anterior teeth was possible without patient compliance. As can be seen in the current report, the use of mini-implants provided a better system for controlling anchorage and facilitating our mechanics. It avoided the use of conventional anchorage mechanics in the posterior segment and its side effect such as molar slippage or extrusion. This resulted in a favorable outcome. However, total lip competency could not be achieved. This could be due to the fact the discrepancy was very severe as well as the mild deficient chin.
4. Conclusions
-
-
Mini-implants can provide absolute anchorage for en masse retraction of the anterior teeth.
-
-
Mini-implants can simplify the treatment plan significantly in such extraction treatment of Class I bimaxillary dentoalveolar protrusion.
References
- Armbruster P.C., Block M.S. Onplant-supported orthodontic anchorage. Atlas Oral Maxillofac. Surg. Clin. North Am. 2001;9(1):53–74. [PubMed] [Google Scholar]
- Bills D.A., Handelman C.S., BeGole E.A. Bimaxillary dentoalveolar protrusion: traits and orthodontic correction. Angle Orthod. 2005;75(3):333–339. doi: 10.1043/0003-3219(2005)75[333:BDPTAO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Block M.S., Hoffman D.R. A new device for absolute anchorage for orthodontics. Am. J. Orthod. Dentofacial Orthop. 1995;107(3):251–258. doi: 10.1016/s0889-5406(95)70140-0. [DOI] [PubMed] [Google Scholar]
- Carter N.E., Slattery D.A. Bimaxillary proclination in patients of Afro-Caribbean origin. Br. J. Orthod. 1988;15(3):175–184. doi: 10.1179/bjo.15.3.175. [DOI] [PubMed] [Google Scholar]
- Chae J.M. A new protocol of Tweed-Merrifield directional force technology with microimplant anchorage. Am. J. Orthod. Dentofacial Orthop. 2006;130(1):100–109. doi: 10.1016/j.ajodo.2005.10.020. [DOI] [PubMed] [Google Scholar]
- Choi B.H., Zhu S.J., Kim Y.H. A clinical evaluation of titanium miniplates as anchors for orthodontic treatment. Am. J. Orthod. Dentofacial Orthop. 2005;128(3):382–384. doi: 10.1016/j.ajodo.2005.04.016. [DOI] [PubMed] [Google Scholar]
- Costa A., Raffainl M., Melsen B. Miniscrews as orthodontic anchorage: a preliminary report. Int. J. Adult Orthod. Orthognath. Surg. 1998;13(3):201–209. [PubMed] [Google Scholar]
- Creekmore T.D., Eklund M.K. The possibility of skeletal anchorage. J. Clin. Orthod. 1983;17(4):266–269. [PubMed] [Google Scholar]
- Dandajena T.C., Nanda R.S. Bialveolar protrusion in a Zimbabwean sample. Am. J. Orthod. Dentofacial Orthop. 2003;123(2):133–137. doi: 10.1067/mod.2003.83. [DOI] [PubMed] [Google Scholar]
- De Pauw G.A., Dermaut L., De Bruyn H., Johansson C. Stability of implants as anchorage for orthopedic traction. Angle Orthod. 1999;69(5):401–407. doi: 10.1043/0003-3219(1999)069<0401:SOIAAF>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- Farrow A.L., Zarrinnia K., Azizi K. Bimaxillary protrusion in black Americans – an esthetic evaluation and the treatment considerations. Am. J. Orthod. Dentofacial Orthop. 1993;104(3):240–250. doi: 10.1016/S0889-5406(05)81725-1. [DOI] [PubMed] [Google Scholar]
- Fonseca R.J., Klein W.D. A cephalometric evaluation of American Negro women. Am. J. Orthod. 1978;73(2):152–160. doi: 10.1016/0002-9416(78)90185-9. [DOI] [PubMed] [Google Scholar]
- Kanomi R. Mini-implant for orthodontic anchorage. J. Clin. Orthod. 1997;31(11):763–767. [PubMed] [Google Scholar]
- Kurz C. The use of lingual appliances for correction of bimaxillary protrusion (four premolars extraction) Am. J. Orthod. Dentofacial Orthop. 1997;112(4):357–363. doi: 10.1016/s0889-5406(97)70042-8. [DOI] [PubMed] [Google Scholar]
- Lamberton C.M., Reichart P.A., Triratananimit P. Bimaxillary protrusion as a pathologic problem in the Thai. Am. J. Orthod. 1980;77(3):320–329. doi: 10.1016/0002-9416(80)90085-8. [DOI] [PubMed] [Google Scholar]
- Lew K. Profile changes following orthodontic treatment of bimaxillary protrusion in adults with the Begg appliance. Eur. J. Orthod. 1989;11(4):375–381. doi: 10.1093/oxfordjournals.ejo.a036009. [DOI] [PubMed] [Google Scholar]
- Miyawaki S., Koyama I., Inoue M., Mishima K., Sugahara T., Takano-Yamamoto T. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am. J. Orthod. Dentofacial Orthop. 2003;124(4):373–378. doi: 10.1016/s0889-5406(03)00565-1. [DOI] [PubMed] [Google Scholar]
- Park H.S., Kwon T.G. Sliding mechanics with microscrew implant anchorage. Angle Orthod. 2004;74(5):703–710. doi: 10.1043/0003-3219(2004)074<0703:SMWMIA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Park H.S., Bae S.M., Kyung H.M., Sung J.H. Micro-implant anchorage for treatment of skeletal Class I bialveolar protrusion. J. Clin. Orthod. 2001;35(7):417–422. [PubMed] [Google Scholar]
- Park H.S., Kwon O.W., Sung J.H. Microscrew implant anchorage sliding mechanics. World J. Orthod. 2005;6(3):265–274. [PubMed] [Google Scholar]
- Park H.S., Lee S.K., Kwon O.W. Group distal movement of teeth using microscrew implant anchorage. Angle Orthod. 2005;75(4):602–609. doi: 10.1043/0003-3219(2005)75[602:GDMOTU]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Park Y.C., Chu J.H., Choi Y.J., Choi N.C. Extraction space closure with vacuum-formed splints and miniscrew anchorage. J. Clin. Orthod. 2005;39(2):76–79. [PubMed] [Google Scholar]
- Park H.S., Yoon D.Y., Park C.S., Jeoung S.H. Treatment effects and anchorage potential of sliding mechanics with titanium screws compared with the Tweed-Merrifield technique. Am. J. Orthod. Dentofacial Orthop. 2008;133(4):593–600. doi: 10.1016/j.ajodo.2006.02.041. [DOI] [PubMed] [Google Scholar]
- Proffit W.R., Fields H.W., Sarver D.M. fourth ed. Mosby Elsevier; St. Louis, MO: 2007. Contemporary Orthodontics. [Google Scholar]
- Roberts W.E., Helm F.R., Marshall K.J., Gongloff R.K. Rigid endosseous implants for orthodontic and orthopedic anchorage. Angle Orthod. 1989;59(4):247–256. doi: 10.1043/0003-3219(1989)059<0247:REIFOA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Roberts W.E., Marshall K.J., Mozsary P.G. Rigid endosseous implant utilized as anchorage to protract molars and close an atrophic extraction site. Angle Orthod. 1990;60(2):135–152. doi: 10.1043/0003-3219(1990)060<0135:REIUAA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Rosa R.A., Arvystas M.G. An epidemiologic survey of malocclusions among American Negroes and American Hispanics. Am. J. Orthod. 1978;73(3):258–273. doi: 10.1016/0002-9416(78)90133-1. [DOI] [PubMed] [Google Scholar]
- Scott S.H., Johnston L.E., Jr. The perceived impact of extraction and nonextraction treatments on matched samples of African American patients. Am. J. Orthod. Dentofacial Orthop. 1999;116(3):352–360. doi: 10.1016/s0889-5406(99)70249-0. [DOI] [PubMed] [Google Scholar]
- Sugawara J., Daimaruya T., Umemori M. Distal movement of mandibular molars in adult patients with the skeletal anchorage system. Am. J. Orthod. Dentofacial Orthop. 2004;125(2):130–138. doi: 10.1016/j.ajodo.2003.02.003. [DOI] [PubMed] [Google Scholar]
- Tan T.J. Profile changes following orthodontic correction of bimaxillary protrusion with a preadjusted edgewise appliance. Int. J. Adult Orthod. Orthognath. Surg. 1996;11(3):239–251. [PubMed] [Google Scholar]
- Umemori M., Sugawara J., Mitani H., Nagasaka H., Kawamura H. Skeletal anchorage system for open-bite correction. Am. J. Orthod. Dentofacial Orthop. 1999;115(2):166–174. doi: 10.1016/S0889-5406(99)70345-8. [DOI] [PubMed] [Google Scholar]
- Wehrbein H., Glatzmaier J., Mundwiller U., Diedrich P. The Orthosystem – a new implant system for orthodontic anchorage in the palate. J. Orofac. Orthop. 1996;57(3):142–153. doi: 10.1007/BF02191878. [DOI] [PubMed] [Google Scholar]
- Wehrbein H., Merz B.R., Diedrich P., Glatzmaier J. The use of palatal implants for orthodontic anchorage. Design and clinical application of the orthosystem. Clin. Oral Implants Res. 1996;7(4):410–416. doi: 10.1034/j.1600-0501.1996.070416.x. [DOI] [PubMed] [Google Scholar]


