Abstract
The objectives of the current study were to 1) describe fibromyalgia patient-spouse incongruence regarding patient pain, fatigue, and physical function and 2) examine the associations of individual and interpersonal factors with patient-spouse incongruence. Two hundred four fibromyalgia patients and their co-residing partners rated the patient’s symptoms and function. Multilevel modeling revealed that spouses, on average, rated patient fatigue significantly lower than patients. Couple incongruence was not significantly different from zero, on average, for pain severity, interference, or physical function. However, there was significant variability across couples in how they rated the severity of symptoms and function, and how much incongruence existed within couples. Controlling for individual factors, patient and spouse reports of communication problems were significantly associated with levels of couple incongruence regarding patient fatigue and physical function, albeit in opposing directions. Across couples, incongruence was high when patients rated communication problems as high; incongruence was low when spouses rated communication problems as high. An important within-couple interaction was found for pain interference suggesting couples who are similar on level of communication problems experience low incongruence; those with disparate ratings of communication problems experience high incongruence. Findings suggest the important roles of spouse response and the patient’s perception of how well the couple is communicating. Couple-level interventions targeting communication or other interpersonal factors may help to decrease incongruence and lead to better patient outcomes.
Keywords: Chronic Pain, Couples, Multilevel modeling, Symptom incongruence, Communication
1. Introduction
Fibromyalgia (FM) is a debilitating chronic pain syndrome characterized by widespread pain, fatigue, and poor physical function [78] that affects the patient and family unit, in particular the marital relationship [11; 52; 62; 69; 70; 72; 73]. FM has been shown to reduce the ability of the couple to engage in shared activities and intimate behaviors [70; 75]. The unpredictable nature of FM challenges the couple to negotiate household tasks [11; 52; 62; 70; 73], while the invisibility of the illness can compromise the supportive context of the couple [65]. Recently, there has been a movement towards a more dyadic perspective of the chronic illness experience [15; 63; 66]. The developmental-contextual model of couples coping with chronic illness [10] proposes that couples appraise, cope, and adjust to the illness context as a unit. Patients and spouses who share similar appraisals of the illness context and related stressors (e.g., patient’s symptoms) experience more interdependent coping, decision-making, and better dyadic adjustment [1; 10; 22; 24; 73]. Incongruent appraisals have been shown to negatively impact couple well-being and quality of life [22; 24; 51] and are particularly important in a context such as FM, where stigma and fears of invalidation exist [5; 34; 40; 68; 71; 73].
Despite a dearth of knowledge regarding factors associated with incongruence, individual factors, in particular depressive symptoms of patient and spouse play an important role in appraising patient’s symptoms [15; 16; 22; 64]. The level of strain felt by the spouse has also been found to affect appraisal of symptoms with higher levels of strain associated with increased incongruence [13; 41; 55; 77]. However, research suggests a need to move beyond individual factors to capture the interpersonal context of the couple [10; 15]. Communication regarding the illness may reflect the level of interdependent coping and responsiveness within the couple and is associated with greater relationship satisfaction [1; 21; 26; 61; 74] and patient adjustment [10; 23; 36; 45; 57]. Yet, couples with chronic illness often engage in protective buffering and communicate less [23]. Previous research on the role of communication in chronic illness has focused primarily on either the patient or spouse perspective; rarely on both [10].
The majority of incongruence research has involved samples of progressively declining patients [38; 39; 41; 49; 60]. Fewer studies have involved chronic pain samples [15; 22; 64]; only two studies including FM couples were found [12; 33]. In all populations, results are inconsistent. This inconsistency may be due to small samples, heterogeneous populations, and traditional methods that limit what they tell us about incongruence (e.g. Kappa coefficient, difference scores) [43]. A notable exception in the pain literature is the study by Cano and colleagues [15] that used the more comprehensive multilevel modeling (MLM) method to examine incongruence in 84 chronic pain couples.
Applying the developmental-contextual model, this study will use MLM to 1) describe FM patient-spouse incongruence regarding patient pain, fatigue, and physical function and 2) examine associations of individual (depressive symptoms, role overload) and interpersonal (communication problems) factors with patient-spouse incongruence.
2. Method
2.1. Participants
A community-based convenience sample was recruited from a database of approximately 3,000 community-living FM patients at a large academic center in the Pacific Northwest. The sample was augmented by also recruiting through the National Fibromyalgia Association and the Fibromyalgia Network. Patients were mailed or e-mailed an informational letter describing the study and contact information for those interested in hearing more about the study. In total, 3,388 letters were mailed or e-mailed. Of those, 432 were returned as invalid addresses with no additional address available. Therefore, only 2,917 addresses were assumed to be correct. A total of 407 (14%) patients requested further information and 216 couples (53%) were eligible, consented and completed at least part of the study for an overall response rate of 8%. Couples were required to be at least 21 years of age or older, be able to read or speak English, have access to a telephone, and reside together in the home. In addition, patients were required to have a provider-confirmed American College of Rheumatology (ACR) diagnosis of FM. The 1990 ACR criteria base the diagnosis of FM on the subjective report of widespread pain and the semi-objective finding of tender points in specific locations [78]. Patients recruited outside of the FM patient database could fulfill this requirement either by a free examination and diagnosis by coauthors Drs. Jones or Bennett, or by having their primary care provider complete and return a form provided. Patients undergoing litigation regarding injury (but not pension or disability) were excluded. Of the 216 couples consented, 204 completed all parts of the study.
The average age of patients and their spouses was 55 (SD=11.5) and 57.5 (SD=12.5) years respectively. Patients were predominantly women (96%). Couples, on average, had well-established relationships and had lived together, on average for 24.84 (SD=15.31) years. Patients and spouses rated their relationship as good using the Mutuality scale [3], which averages scores across 15 items to obtain a 0–4 scale (patient: 3.10 (SD=0.75); spouse: 3.21 (SD=0.67)). The majority of patients and spouses were Caucasian (86% and 90%, respectively) and had attended at least some college (85% and 80%, respectively). Median annual household income was $50,000–74,999. A third of patients reported being employed (33%), working an average of 20 hours a week (SD=14.7), and 23% of patients reported having children under 18 years of age in the home. Patients reported having FM, on average, 12.70 (SD=8.2) years.
2.2. Measures
2.2.1. Pain
Pain was measured using the 15-item Brief Pain Inventory (BPI) [20]. The BPI has been successfully used with patients with arthritis, back pain and FM, including FM studies reviewed by the FDA [4; 32; 50; 67]. The BPI consists of two subscales – pain severity and pain interference. Pain severity rates the patient’s pain over the last week on a 0 (no pain) to 10 (pain as bad as you can imagine) scale for pain at its worst, least, on average, and right now. Pain interference rates the extent the patient’s pain interferes with 7 activities (i.e., general activity, walking, mood, sleep, work, relations with others, and enjoyment of life) on a 0 (does not interfere) to 10 (interferes completely) scale. Subscale scores are created by averaging items. Higher scores indicate higher levels of pain severity and interference. High Cronbach’s alpha values have been exhibited for both the severity (.75–.97) and interference scales (.78–.91) [4; 30; 32]. Sensitivity, specificity and validity of the scales have also been supported in noncancer pain samples [4; 30; 32]. In the current study, patients and spouses were asked to rate the patient’s pain severity and pain interference over the last week. Both patient and spouse scales demonstrated strong internal consistency: pain severity (patient report: α=.87; spouse report: α=.88) and pain interference (patient report: α=.87; spouse report: α=.91).
2.2.2. Fatigue
Fatigue was measured using the 13-item fatigue scale of the Functional Assessment in Chronic Illness Therapy (FACIT) measure [79]. The measure, developed for use in cancer patients, assesses self-reported tiredness, weakness, and difficulty conducting usual activities due to fatigue. The measure includes such items as “I feel fatigued” and “I have trouble finishing things because I am tired.” Each item is rated on a 0 (not all) to 4 (very much) scale based on fatigue over the past week. All but two items are reverse coded and then all items are summed to create a scale score, with higher scores indicating less fatigue [18]. The scale has demonstrated good construct validity with the Piper fatigue scale (.83) and Profile of Mood States fatigue scale (.77) [80] and good reliability and validity in noncancer samples, including people with arthritis and back pain [19]. In the current study, patients and spouses were asked to rate the patient’s fatigue over the past week. Both patient and spouse scales demonstrated strong internal consistency (patient report: α=.92; spouse report: α=.92).
2.2.3. Physical function
Patient physical function was measured using the 10-item physical function scale of the Fibromyalgia Impact Questionnaire (FIQ) [14]. Items include activities such as shopping, laundry, preparing meals, walking several blocks, climbing stairs, and doing yard work. Each item is rated on a 0 (always able) to 3 (never able) scale based on functional ability over the past week. Scale scores are created by averaging across items and multiplying by 3.33 to create a 0–10 scale with higher scores indicating poor physical function. The instrument has demonstrated good reliability and validity [14]. In the current study, patients and spouses were asked separately to rate the patient’s physical function over the past week. Both patient and spouse scales demonstrated strong internal consistency (patient report: α=.90; spouse report: α=.92).
2.2.4. Depressive symptoms
Depressive symptoms were measured using the 21-item Beck Depression Inventory – second edition (BDI-II) [7]. Each item consists of four statements scored on a 0 to 3 scale based on the patient’s experience during the past two weeks, with higher scores indicating increasing severity. There is extensive evidence for the reliability and validity of the BDI-II in psychiatric and non-psychiatric populations [7]. Scores are summed for a range of 0 to 63, with higher scores indicating greater symptom severity. Scores above 29 are indicative of severe depressive disorder. In the current study, patients and spouses were asked to rate their own depressive symptoms over the past two weeks. Both patient and spouse scales demonstrated strong internal consistency (patient report: α=.93; spouse report: α=.89).
2.2.5. Communication
Illness-related communication was measured using the 15-item Cancer-Related Communication Problem (CRCP) scale [35]. The measure was originally developed to assess the extent of difficulty cancer couples experienced communicating about the patient’s cancer. Both a patient and spouse version were developed to consist of 15 parallel items representing the types of communication problems that can exist between couples during illness, including emotional support, self-protection, protective buffering, and illness/treatment related issues. As the measure has not been previously used with Fibromyalgia, items were modified to refer to the patient’s FM rather than cancer. Some items are identical in the patient and spouse versions (e.g., “When it comes to fibromyalgia, I only tell my spouse what he or she wants to hear”). Other items are modified for the patient or spouse (e.g., patient-version: “I don’t talk with my spouse about how fibromyalgia affects me sexually;” spouse-version: “I don’t talk with my spouse about how him or her having fibromyalgia affects me sexually”). Each item is rated on a 0 (not true) to 2 (often true) scale. Items worded as positive communication are considered problems if rated as 0 (not true) or 1 (sometimes true). Items worded as negative communication are considered problems if rated 1 (sometimes true) or 2 (often true). Higher scores indicate a greater number of communication problems. A study of breast cancer couples found patients reported a median of 6.5 problems (0–15 range) and their spouses reported a median of 5 problems (0–14 range) [35]. Both patient and spouse versions of the measure demonstrated good internal consistency and convergent validity with measures of marital quality and psychological distress for a sample of cancer patients and their partners [35]. In the current study, patient and spouse scales demonstrated good internal consistency (patient report: α=.86; spouse report: α=.78). Fibromyalgia patients reported, on average, 8 problems (SD = 4.18; median = 8; range: 0–15); spouses reported, on average, 6.6 problems (SD = 3.44; median = 7; 0–15 range).
2.2.6. Role overload
Spouse role overload was measured using the 3-item role overload scale [53]. Role overload assesses the extent to which the spouse’s time and energy are exhausted by the demands of caring for the patient. Spouses respond to three items regarding how worn-out and overloaded their care role makes them feel using a Likert scale from 0 (not at all) to 3 (very much). Higher scores indicate high levels of role overload. The scale has exhibited high Cronbach’s alpha values (.71 to .78) in studies of family care [2; 25; 42; 53; 81], and evidence of construct validity with patient physical function and family member depression [2; 53]. In the current study, the scale demonstrated acceptable internal consistency (α=.70).
2.3. Procedure
Participants were recruited through informational letters and recruitment flyers. Potential participants were screened by phone. When couples were deemed eligible and interested, they were mailed separate packets containing surveys and consent forms with instructions to complete the surveys independently. Once both surveys were received, separate phone interviews were scheduled with the patient and spouse to assess patient symptoms and physical function during the past week. Couples were compensated for completion of both mail surveys and phone interviews ($20 for each member of the couple).
2.4. Data analysis plan
Hierarchical Linear Modeling (HLM), used with clustered data, extends multiple regression to the case where the members of the couple are conceived as level-1 units nested within the level-2 unit, the couple. The model can be adapted to represent a cross-sectional model for matched pairs [6] in which the couple replaces the individual as the unit of analysis. The statistical advantage is that it controls for the correlation in the pair of outcome scores associated with each couple (e.g., one for the patient and one for the spouse). This approach allows for a more precise estimation of the between-couple effect by reducing the standard error associated with such tests. An important advantage is that it estimates two latent scores for each couple: an average that represents the level of symptom severity perceived by the couple and an incongruence score that represents the difference in patient-spouse perception of symptom severity.
HLM 7 [59] was used to examine couple incongruence in patient symptoms and function, the heterogeneity of variance in couple incongruence, and variables associated with this incongruence. Similar incongruence models have been used in studies of frail older adult care dyads [41], individuals with chronic pain and their spouses [15], and more recently care dyads where the older adult has mild to moderate dementia [60]. To fit a regression line for each couple, two data points are needed for each member of the couple – patient and spouse. Two parallel scales are created by matching pairs of items on patient measures on their standard deviations and randomly assigning one item from each matched pair to scale A or B. This process is done separately for patients and spouses resulting in parallel scales with similar variance and reliability. This method was first suggested by Raudenbush and colleagues [58] and has also been described by Lyons et al. [41]. The current study will use this method for examining patient fatigue (creating an average fatigue score of 0–4 with higher scores indicating less fatigue). As the fatigue measure has an uneven number of items (i.e., 13), the item least endorsed (“too tired to eat”) was not included in creating parallel scales. Measures of pain severity, pain interference, and physical function do not have adequate numbers of items to ensure parallel scales so the alternative “known variance” option described by Cano et al. [15] was used. This method requires estimating the measurement error for each outcome as ([1 − Reliability] × observed variance), which allows the program to create the precision weight (inverse of the error variance) needed to run the analysis.
The following model will be fit separately to the symptom data for each couple j:
Yij represents the symptom or function score i in couple j (in the case of fatigue i = 1,…4 parallel scales per couple). The level-1 or within-couple model expresses the outcome as a function of a dummy variable that indicates whether the score was reported by the patient or the spouse, plus a residual term r that captures measurement error in the outcome scores. The predictor will be coded −.5 for the patient and +.5 for the spouse. Under this formulation, the model intercept (β0j) represents the expected value of the outcome Y when the predictor INDICATOR is zero, which is the couple average; the model slope (β1j) represents the incongruence or gap between the two members of the couple.
The unconditional level-2 or between-couple model provides estimates of the population averages for couple symptom/function severity (γ00) and couple incongruence (γ10 ) and the variability around those averages (variances of u0j and u1j). A chi-square test can be performed to test whether the variances are significantly different from zero. If they are, significant heterogeneity exists across couples and predictors can be introduced to explain the heterogeneity. The conditional level-2 model will add predictors to explain the heterogeneity across couples in average symptom severity and incongruence in symptom severity, for example:
In this model, the effect of patient and spouse variables on couple symptom/function severity are captured by the coefficients γ02 through γ06, controlling for the effect of years couples have lived together. Similarly, the effect of patient and spouse variables on couple incongruence are captured by the coefficients γ12 through γ16, controlling for the effect of years couples have lived together. Coefficients for each predictor variable are interpreted as unstandardized B coefficients in a simultaneous multiple regression. All predictor variables were mean centered for ease of interpretation. To enable examination of within-dyad versus across dyad effects, we tested models including a term representing the interaction between patient and spouse communication problems. Interaction effects are only reported for symptoms where the effect was found to be significant. Otherwise, main effects models are reported.
Although it may appear that such models should be analyzed using a three-level model due to data at three levels – the couple, the persons within the couple, and observations within persons – this is not considered prudent [37]. An underlying assumption of MLM is there can be variability at each level. However, once the couple member role (e.g., patient vs. spouse) is included in the model by using a dummy indicator variable, the middle level is said to be saturated and no additional variance can be estimated at this level [37]. Thus, a two-level model is considered the appropriate formulation as variability is only expected at two levels – observations within persons, and the couple.
3. Results
3.1. HLM incongruence model of pain severity
Results of the Level 1 model showed that, on average, couples rated the patient’s pain severity as 4.92 (p < .001), indicating a moderate level of severity (1–10 scale). The average incongruence score for patient pain severity was −0.12 (p >.05), indicating that, on average, patients and spouses did not report significantly different scores. However, the random effects indicated significant variability around the average couple patient pain severity score and average incongruence score (Table 1). Couple mean pain severity and incongruence were correlated at .05, suggesting little association between level of pain severity and amount of couple incongruence.
Table 1.
Level 1 and Level 2 hierarchical linear incongruence models: Pain severity
| Fixed effects | Level 1 Model | Level 2 Model | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| B | SE | t | B | SE | t | |
| Couple mean | ||||||
| Intercept | 4.92a | 0.10 | 48.27*** | 4.93 | 0.10 | 51.29*** |
| Years lived together | −0.00 | 0.01 | −0.02 | |||
| PT depressive symptoms | 0.04 | 0.01 | 3.65*** | |||
| PT communication problems | −0.02 | 0.03 | −0.82 | |||
| SP depressive symptoms | 0.03 | 0.02 | 1.65 | |||
| SP communication problems | 0.01 | 0.03 | 0.34 | |||
| SP role overload | 0.05 | 0.05 | 1.01 | |||
| Couple incongruence | ||||||
| Intercept | −0.12b | 0.12 | −1.04 | −0.13 | 0.12 | −1.12 |
| Years lived together | 0.01 | 0.01 | 1.01 | |||
| PT depressive symptoms | −0.01 | 0.01 | −0.67 | |||
| PT communication problems | −0.05 | 0.03 | −1.46 | |||
| SP depressive symptoms | 0.03 | 0.02 | 1.79 | |||
| SP communication problems | 0.03 | 0.04 | 0.76 | |||
| SP role overload | −0.09 | 0.06 | −1.43 | |||
|
| ||||||
| Random effects | Variance Component | χ2 | Variance Component | χ2 | ||
|
| ||||||
| Couple mean | 1.83 | 2182.02*** | 1.60 | 1940.74*** | ||
| Couple incongruence | 1.96 | 728.09*** | 1.83 | 690.76*** | ||
Higher scores indicate greater pain severity.
Negative incongruence scores indicate that the patient is rating patient pain severity as higher than the spouse. Models presented did not differ when duration of disease or spouse’s health (measured by the physical component scale of the SF-36) were included. PT – patient; SP – spouse.
p < .05;
p < .01;
p < .001.
The Level 2 model examined the association of the predictor variables with between-couple variance in pain severity means and incongruence scores. No significant interaction for patient-spouse communication problems was found. Controlling for other predictors in the model (years lived together, patient communication problems, spouse communication problems, spouse depressive symptoms, and spouse role overload), higher levels of patient depressive symptoms were significantly associated with higher couple mean pain severity scores. No variables were significantly associated with incongruence in pain severity. Together, the predictor variables accounted for 12% of the variance in couple mean pain severity and 7% in incongruence. Although the Level 2 model was a significantly better fit over the Level 1 model χ2(12) = 33.82, p <.001, the Level 2 random effects remained significant.
3.2. HLM incongruence model of pain interference
Results of the Level 1 model showed that, on average, couples rated the patient’s pain interference as 5.15 (p < .001), indicating a moderate level of interference (1–10 scale). The average incongruence score for patient pain interference was −0.26 (p >.05), indicating that, on average, patients and spouses did not report significantly different scores. However, the random effects indicated significant variability around the average couple patient pain interference score and average incongruence score (Table 2). Couple mean pain interference and incongruence were correlated at −.01, suggesting little association between level of pain interference and amount of couple incongruence.
Table 2.
Level 1 and Level 2 hierarchical linear incongruence models: Pain interference
| Fixed effects | Level 1 Model | Level 2 Model | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| B | SE | t | B | SE | t | |
| Couple mean | ||||||
| Intercept | 5.15a | 0.15 | 35.54*** | 5.13 | 0.13 | 40.56*** |
| Years lived together | −0.00 | 0.01 | −0.43 | |||
| PT depressive symptoms | 0.09 | 0.01 | 7.30*** | |||
| PT communication problems | −0.04 | 0.03 | −1.32 | |||
| SP depressive symptoms | 0.03 | 0.02 | 1.62 | |||
| SP communication problems | 0.01 | 0.04 | 0.34 | |||
| SP role overload | 0.18 | 0.07 | 2.75** | |||
| PT X SP communication problems | 0.01 | 0.01 | 0.87 | |||
| Couple incongruence | ||||||
| Intercept | −0.26b | 0.17 | −1.58 | −0.16 | 0.16 | −0.99 |
| Years lived together | 0.01 | 0.01 | 0.79 | |||
| PT depressive symptoms | −0.03 | 0.02 | −1.77 | |||
| PT communication problems | −0.13 | 0.04 | −3.05** | |||
| SP depressive symptoms | 0.04 | 0.02 | 1.64 | |||
| SP communication problems | 0.14 | 0.05 | 2.85** | |||
| SP role overload | 0.05 | 0.09 | 0.56 | |||
| PT X SP communication problemsc | −0.02 | 0.01 | −1.98* | |||
|
| ||||||
| Random effects | Variance Component | χ2 | Variance Component | χ2 | ||
|
| ||||||
| Couple mean | 3.70 | 2173.29*** | 2.39 | 1472.31*** | ||
| Couple incongruence | 3.79 | 697.94*** | 3.09 | 604.70*** | ||
Higher scores indicate greater pain interference.
Negative incongruence scores indicate that the patient is rating patient pain interference as higher than the spouse. Models presented did not differ when duration of disease or spouse’s health (measured by the physical component scale of the SF-36) were included. PT – patient; SP – spouse.
p < .05;
p < .01;
p < .001.
The Level 2 model examined the association of the predictor variables with between-couple variance in pain interference means and incongruence scores. Controlling for other predictors in the model, higher patient depressive symptoms and spouse reports of increased role overload were significantly associated with higher couple mean pain interference scores. For incongruence, both patient and spouse reports of communication problems and the communication problem interaction term were significantly associated with incongruence regarding pain interference levels, controlling for other variables in the model. As can be seen in Figure 1 when patients and spouses are similar on the level of communication problems (high or low), there is a low level of incongruence regarding patient pain interference. When couples are dissimilar on the level of communication problems, there is increased incongruence within the couple. Additionally, for those couples where the patient rates problems low and the spouse rates them as high, the direction of incongruence changes with spouses rating patient pain interference higher than patients. Together, the predictor variables accounted for 35% of the variance in couple mean pain interference and 18% in incongruence. Although the Level 2 models was a significantly better fit over the Level 1 model χ2(14) = 103.44, p< .001, the Level 2 random effects remained significant suggesting other variables not included in the model may explain variability across couples.
Figure 1.
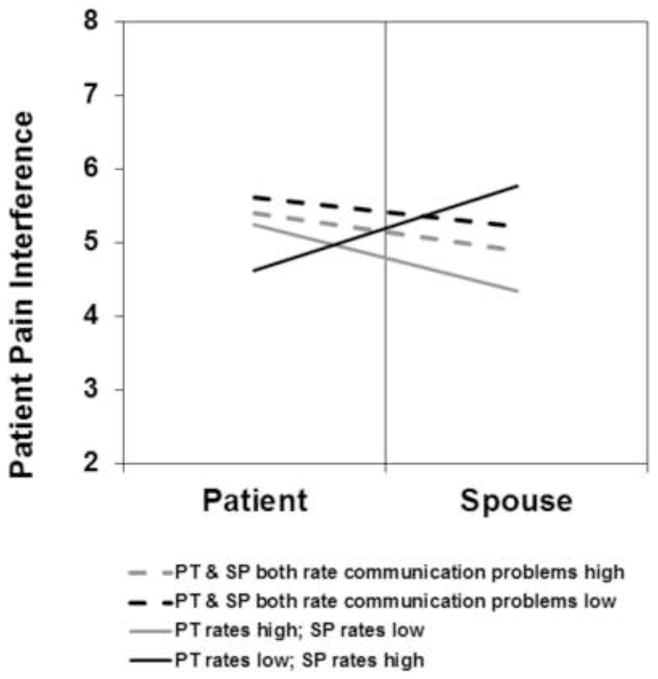
Average couple incongruence on pain interference when patients and spouses similar and dissimilar on level of communication problems. High and low levels of communication problems represent 1 SD above and below the mean, respectively; all other variables held constant.
3.3. HLM incongruence model of fatigue
Results of the Level 1 model showed that, on average, couples rated the patient’s fatigue as 1.65 (p < .001), indicating a moderate level of fatigue (0–4 scale with lower scores indicating more fatigue). The average incongruence score for patient fatigue was 0.16 (p <.01). As patients were coded −.5 and spouses .5, this incongruence score indicates that spouses, on average, rate patient fatigue significantly lower than patients rate their fatigue. The random effects indicated significant variability around the average couple patient fatigue score and average incongruence score (Table 3). Couple mean fatigue and incongruence were correlated at −.07, suggesting little association between level of fatigue and amount of couple incongruence.
Table 3.
Level 1 and Level 2 hierarchical linear incongruence models: Fatigue
| Fixed effects | Level 1 Model | Level 2 Model | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| B | SE | t | B | SE | t | |
| Couple mean | ||||||
| Intercept | 1.65a | 0.05 | 31.94*** | 1.64 | 0.04 | 41.92*** |
| Years lived together | −0.00 | 0.00 | −0.71 | |||
| PT depressive symptoms | −0.04 | 0.00 | −9.82*** | |||
| PT communication problems | 0.02 | 0.01 | 1.68 | |||
| SP depressive symptoms | −0.01 | 0.01 | −0.71 | |||
| SP communication problems | 0.00 | 0.01 | 0.01 | |||
| SP role overload | −0.09 | 0.02 | −3.92*** | |||
| Couple incongruence | ||||||
| Intercept | 0.16b | 0.05 | 3.02** | 0.16 | 0.05 | 3.17** |
| Years lived together | 0.00 | 0.00 | 0.17 | |||
| PT depressive symptoms | 0.01 | 0.01 | 2.15* | |||
| PT communication problems | 0.05 | 0.01 | 3.31*** | |||
| SP depressive symptoms | −0.00 | 0.01 | −0.11 | |||
| SP communication problems | −0.05 | 0.02 | −3.04** | |||
| SP role overload | −0.01 | 0.03 | −0.26 | |||
|
| ||||||
| Random effects | Variance Component | χ2 | Variance Component | χ2 | ||
|
| ||||||
| Couple mean | 0.48 | 3279.81*** | 0.26 | 1879.82*** | ||
| Couple incongruence | 0.44 | 896.63*** | 0.37 | 789.23*** | ||
Higher scores indicate less fatigue.
Positive incongruence scores indicate that the patient is rating patient fatigue as higher than the spouse. Models presented did not differ when duration of disease or spouse’s health (measured by the physical component scale of the SF-36) were included. PT – patient; SP – spouse.
p < .05;
p < .01;
p < .001.
The Level 2 model examined the association of the predictor variables with between-couple variance in fatigue means and incongruence scores. No significant interaction for patient-spouse communication problems was found. Controlling for other predictors in the model, higher patient depressive symptoms and higher spouse role overload were significantly associated with higher couple mean fatigue scores. For incongruence, patient depressive symptoms and both patient and spouse reports of communication problems were significantly associated with incongruence regarding fatigue levels, controlling for other variables in the model. Across couples incongruence regarding patient fatigue was significantly higher when patients reported high levels of depressive symptoms or communication problems but significantly lower when spouses reported high levels of communication problems. However, no significant within-couple effects were found. Together, the predictor variables accounted for 45% of the variance in couple mean fatigue and 15% in incongruence. Although the Level 2 models was a significantly better fit over the Level 1 model χ2(12) = 132.72, p< .001, the Level 2 random effects remained significant suggesting other variables not included in the model may explain variability across couples.
3.4. HLM incongruence model of physical function
Results of the Level 1 model showed that, on average, couples rated the patient’s physical function as 4.52 (p < .001), indicating a moderate level of physical function (0–10 scale). The average incongruence score for patient physical function was −0.23 (p >.05), indicating that, on average, patients and spouses did not report significantly different scores. However, the random effects indicated significant variability around the average couple patient physical function score and average incongruence score (Table 4). Couple mean physical function and incongruence were correlated at .04, suggesting little association between level of physical function and amount of couple incongruence.
Table 4.
Level 1 and Level 2 hierarchical linear incongruence models: Physical Function
| Fixed effects | Level 1 Model | Level 2 Model | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| B | SE | t | B | SE | t | |
| Couple mean | ||||||
| Intercept | 4.52a | 0.16 | 28.09*** | 4.55 | 0.13 | 35.41*** |
| Years lived together | −0.00 | 0.01 | −0.12 | |||
| PT depressive symptoms | 0.09 | 0.01 | 7.08*** | |||
| PT communication problems | −0.05 | 0.03 | −1.55 | |||
| SP depressive symptoms | 0.04 | 0.02 | 2.15* | |||
| SP communication problems | 0.04 | 0.04 | 0.94 | |||
| SP role overload | 0.31 | 0.07 | 4.21*** | |||
| Couple incongruence | ||||||
| Intercept | −0.23 | 0.17 | −1.32 | −0.18 | 0.16 | −1.12 |
| Years lived together | −0.02 | 0.01 | −1.52 | |||
| PT depressive symptoms | −0.01 | 0.02 | −0.71 | |||
| PT communication problems | −0.16 | 0.04 | −3.65*** | |||
| SP depressive symptoms | 0.03 | 0.02 | 1.32 | |||
| SP communication problems | 0.19 | 0.05 | 3.75*** | |||
| SP role overload | −0.02 | 0.09 | −0.25 | |||
|
| ||||||
| Random effects | Variance Component | χ2 | Variance Component | χ2 | ||
|
| ||||||
| Couple mean | 4.60 | 3121.21*** | 2.79 | 1931.46*** | ||
| Couple incongruence | 3.96 | 798.94*** | 3.31 | 693.27*** | ||
Higher scores indicate greater physical impairment.
Negative incongruence scores indicate that the patient is rating patient pain severity as higher than the spouse. Models presented did not differ when duration of disease or spouse’s health (measured by the physical component scale of the SF-36) were included. PT – patient; SP – spouse.
p < .05;
p < .01;
p < .001.
The Level 2 model examined the association of the predictor variables with between-couple variance in physical function means and incongruence scores. No significant interaction for patient-spouse communication problems was found. Controlling for other predictors in the model, higher patient depressive symptoms, higher spouse depressive symptoms, and higher levels of spouse role overload were significantly associated with higher couple mean physical impairment scores.
For incongruence, both patient and spouse reports of communication problems were significantly associated with incongruence regarding physical function levels, controlling for other variables in the model. Again, across couples incongruence regarding patient physical function was significantly higher when patients reported high levels of communication problems but significantly lower when spouses reported high levels of communication problems. No significant within-couple effects were found. Together, the predictor variables accounted for 39% of the variance in couple mean physical function and 16% in incongruence. Although the Level 2 models was a significantly better fit over the Level 1 model χ2(12) = 110.55, p< .001, the Level 2 random effects remained significant suggesting other variables not included in the model may explain variability across couples.
4. Discussion
Little is known about FM couples, in particular, their perceptions of the patient’s symptoms and amount of incongruence within the couple regarding the severity of those symptoms. The current study used MLM to examine FM couple incongruence regarding patient symptoms and physical function and variables associated with incongruence. Several findings are noteworthy. First, couples, on average, reported moderate levels of pain severity, pain interference, fatigue, and physical impairment in the patient. Second, patients and spouses did not differ in their perceptions, on average, except in the case of patient fatigue, where spouses rated significantly less fatigue than patients. However, consistent with previous research with chronic pain couples [15], there was significant variability across couples in how they rated the severity of symptoms and how much incongruence existed within couples. Third, there was no association between the amount of incongruence and how couples rated severity. Fourth, interpersonal factors were significantly associated with patient-spouse incongruence. Finally, a moderate amount of variance in patient-spouse incongruence (15–18%) was explained by a small number of variables, except in the case of pain severity (7%).
Despite the lack of couple incongruence, on average, there was significant variability across couples for all four outcome variables. Controlling for patient and spouse depressive symptoms and spouse role overload, both patient and spouse reports of communication problems were significantly associated with incongruence for fatigue and physical function, albeit in opposing directions. When patients reported high levels of communication problems, couples experienced higher levels of incongruence. Alternatively, when spouses reported high levels of communication problems, couples experienced lower levels of incongruence. The benefit may be in the responsiveness of the spouse, which plays an important role in patient adjustment [16; 29; 44; 46]. When spouses report a high number of communication problems, the lack of incongruence may reflect a relationship in which the patient feels validated. Spouses, who were predominantly male, may be seen as more responsive and supportive if they believe there is “room for improvement,” and are motivated towards better communication and interdependent coping. This is consistent with findings from other chronic pain contexts which have linked greater satisfaction with the relationship to a more supportive spouse [61; 74] and greater feelings of emotional validation [17], allowing the couple to cope more effectively [28; 61]. This may also be a plausible explanation for why couples in the current study where the patient reported high levels of communication problems, had higher levels of incongruence.
The importance of communication between patient and spouse is further underscored by the pain interference finding that couples who are more likely to be similar on the level of communication problems, within the couple, are more likely to experience less symptom incongruence, suggesting an advantage for couples who are more congruent regarding their level of communication about the illness context. Such “emotional” congruence may reflect positive interpersonal interactions, greater relationship satisfaction, and hence spouses better placed to recognize symptoms, even in cases where both members believe there are a large number of areas where they are not communicating well. Couples experiencing disparate ratings of communication problems are not surprisingly more likely to experience increased incongruence regarding pain interference. However, the direction of the incongruence is dependent on which member reports more communication problems. When patients report more communication problems than spouses, spouses tend to rate patient pain interference less severe than patients. When spouses report more communication problems than patients, spouses tend to rate patient pain interference more severe than patients. Due to the cross-sectional nature of the study, it is also possible that incongruence impacts communication within the couple.
Although the primary goal of this study was to understand incongruence in FM couples, consistent with previous literature, patient and spouse depressive symptoms, and spouse feelings of strain were significantly associated with how couples rated levels of symptoms and function [15; 16; 22; 55; 64]. However, the cross-sectional nature of the study again makes it difficult to address causality. It is equally likely that high levels of patient symptoms and physical impairment lead to high levels of patient and spouse depressive symptoms, and greater feelings of spouse role overload.
The current study has several important strengths and implications for practice and future research. First, this is one of the only known studies to use MLM to examine patient-spouse incongruence in FM couples. This innovative methodology allowed us to move beyond average incongruence to understand the variables across, and in the case of pain interference, within couples, that may place couples at risk for incongruence. Second, the study examined both individual and interpersonal risk factors and identified communication problems between patient and spouse as a potential focus for intervention. Couple-level interventions targeting communication and empathy may help to increase symptom recognition thereby decreasing incongruence, leading to better patient outcomes, and bolster the supportive nature of the couple to result in more positive couple adjustment over time [17; 29; 56]. Even in the case of fatigue and function, findings underscore the importance of including the perspective of both members. Several couple-level interventions have shown promising results on both couple and patient outcomes [47; 48; 54], though none have focused on FM couples. As FM patients can often feel stigmatized by family, who question the validity of their illness experience [5; 40; 69; 70; 73], communication-based interventions may be particularly relevant, and a more malleable target than the broader concept of relationship satisfaction.
According to the theoretical framework, focusing on the dyad as the unit of analysis provides a perspective that will allow interventions to maximize outcomes for both members of the couple. If health care providers focus management strategies solely on the patient, they may miss a critical component of the patient’s cumulative disease experience – i.e. the interdependent nature of the couple. Rather, clinicians need to be mindful of the potential interpersonal issues that may exist within FM couples that can hinder optimal outcomes. In particular, it may be beneficial for clinicians to determine both patient and spouse perspectives of the patient’s symptoms and function and assist the couple in discussing FM-related topics about which they are having difficulty communicating. As with many chronic illness contexts, clinicians can also play an important role in identifying spouses who may be experiencing high levels of depressive symptoms and strain. The challenges of chronic pain on the couple increase the need to identify those at greatest risk for poor dyadic adjustment and to provide appropriate interventions at the level of the couple [76]. Health care providers are optimally situated to take a more holistic approach to the couple. It will be important to educate clinicians most likely to see FM patients on the advantages of such an approach.
Despite the strengths of the current study, there are several limitations. First, as noted above, the cross-sectional design limits discussion of directional effects. Future research is needed to examine the temporal order of associations. Second, although the large, community-based sample increases the generalizability of the findings, the focus on co-residing partnered couples means that conclusions regarding other FM dyads (e.g., siblings, parent-adult-child) are not possible. Additionally, due to the low percentage of male patients and non-Caucasian patients, gender and minority effects could not be examined. Future research is needed to understand similarities and differences in incongruence in these additional FM dyads. Third, the study experienced a very low response rate, which may have been partly related to the mode of contact (i.e., cold e-mails and mailed letters), descriptive nature of the study, and eligibility criteria. Nevertheless, the large, community-based convenience sample is typical of the fibromyalgia population in being predominantly white and female, and comparable in age to that found in previous FM research [9; 27; 31; 78]. Additionally, the level of disability of the sample is also representative of the population [8; 27]. It is, however, unknown if the results of the current study can be generalized to those couples who did not select to participate due to factors such as severe depression. Similar to other couple research, couples in the current study rated their relationship, on average, as good and well-established. Again, the generalizability of the findings for couples who rate their relationship as poor is yet unknown and particularly relevant given the findings of the study. Further research on creatively recruiting these under-represented couples is needed. Finally, the large amount of unexplained variance in incongruence (particularly for pain severity) suggests more research is still warranted to identify additional interpersonal factors such as empathy and dyadic coping style.
FM has been found to challenge the supportive nature of the couple [62]. Taking a dyadic approach and moving beyond individual risk factors will broaden our ability to support couples through the process and facilitate adaptive coping and adjustment for both patient and spouse. The current study used MLM to examine risk factors for patient-spouse incongruence that may help us to identify couples in need of intervention, as well as those doing well.
Significant variability was found across couples in how they rated symptom severity and how much incongruence existed within couples. Interpersonal factors were significantly associated with patient-spouse incongruence.
Acknowledgments
This project was supported by NIH grant R21 AR053597 (PI Lyons).
Footnotes
Conflict of interest statement
The authors have no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Acitelli LK, Badr HJ. My illness or our illness? Attending to the relationship when one partner is ill. In: Revenson TA, Kayser K, Bodenmann G, editors. Couples coping with stress: Emerging perspectives on dyadic coping. Washington, DC: American Psychological Association; 2005. pp. 121–136. [Google Scholar]
- 2.Aneshensel CS, Pearlin L, Mullan JT, Zarit SH, Whitlatch CJ. Profiles in caregiving: The unexpected career. San Diego, CA: Academic Press; 1995. [Google Scholar]
- 3.Archbold PG, Stewart BJ, Greenlick MR, Harvath T. Mutuality and preparedness as predictors of caregiver role strain. Research in Nursing & Health. 1990;13:375–384. doi: 10.1002/nur.4770130605. [DOI] [PubMed] [Google Scholar]
- 4.Arnold LM, Lu Y, Crofford LJ, Wolhlreich M, Detke MJ, Iyengar S, et al. A double-blind multicenter trial comparing duloxetine with placebo in the treatment of fibromyalgia patients with or withour major depressive disroder. Arthritis & Rheumatism. 2004;50:2974–2984. doi: 10.1002/art.20485. [DOI] [PubMed] [Google Scholar]
- 5.Asbring P, Narvanen A-L. Women’s experiences of stigma in relation to chronic fatigue syndrome and fibromyalgia. Qualitative Health Research. 2002;12:148–160. doi: 10.1177/104973230201200202. [DOI] [PubMed] [Google Scholar]
- 6.Barnett RC, Marshall NL, Raudenbush SW, Brennan RT. Gender and the relationship between job experiences and psychological distress: A study of dual-earner couples. Journal of Personality & Social Psychology. 1993;64:794–806. doi: 10.1037//0022-3514.64.5.794. [DOI] [PubMed] [Google Scholar]
- 7.Beck AT, Steer RA, Brown GK. Psychological Corporation. 1996. Manual for the Beck Depression Inventory - II. [Google Scholar]
- 8.Bennett RM, Bushmakin AG, Cappelleri JC, Zlateva G, Sadosky AB. Minimal clinically important difference in the Fibromyalgia Impact Questionnaire. The Journal of Rheumatology. 2009;36:1304–1311. doi: 10.3899/jrheum.081090. [DOI] [PubMed] [Google Scholar]
- 9.Bennett RM, Jones J, Turk DC, Russell IJ, Matallana L. An internet survey of 2,596 people with fibromyalgia. BMC Musculoskeletal Disorders. 2007;8(27) doi: 10.1186/1471-2474-8-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berg CA, Upchurch R. A Developmental-Contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin. 2007;133:920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- 11.Bigatti SM, Cronan TA. An examination of the physical health, health care use, and psychological well-being of spouses of people with fibromyalgia syndrome. Health Psychology. 2002;21:157–166. [PubMed] [Google Scholar]
- 12.Bigatti SM, Cronan TA, Frederick H, Kaplan RM. Spouses of women with the fibromyalgia syndrome as proxy raters of health status. Journal of Musculoskeletal Pain. 2007;15(3):9–17. [Google Scholar]
- 13.Broberger E, Tishelman C, von Essen L. Discrepancies and similarities in how patients with lung cancer and their professional and family caregivers assess symptom occurrence and symptom distress. Journal of Pain and Symptom Management. 2005;29:572–583. doi: 10.1016/j.jpainsymman.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 14.Burckhardt CS, Clark SR, Bennett RM. The fibromyalgia impact questionnaire: development and validation. Journal of Rheumatology. 1991;18:728–733. [PubMed] [Google Scholar]
- 15.Cano A, Johansen AB, Franz A. Multilevel analysis of couple congruence on pain, interference, and disability. PAIN®. 2005;118:369–379. doi: 10.1016/j.pain.2005.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cano A, Johansen AB, Geisser M. Spousal congruence on disability, pain, and spouse responses to pain. PAIN®. 2004;109:258–265. doi: 10.1016/j.pain.2004.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cano A, Williams AC. Social interaction in pain: Reinforcing pain behaviors or building intimacy? PAIN®. 2010;149:9–11. doi: 10.1016/j.pain.2009.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cella D, Kallich J, McDermott A, Xu X. The longitudinal relationship of hemoglobin, fatigue and quality of life in anemic cancer patients: Results from five randomized clinical trials. Annual Oncology. 2004;15:979–986. doi: 10.1093/annonc/mdh235. [DOI] [PubMed] [Google Scholar]
- 19.Cella D, Zagari MJ, Vandoros C, Gagnon DD, Hurtz H, Nortier JWR. Epoetin alfa treatment results in clinically significant improvements in quality of life in anemic cancer patients when references to the general population. Journal of Clinical Oncology. 2003;21:366–373. doi: 10.1200/JCO.2003.02.136. [DOI] [PubMed] [Google Scholar]
- 20.Cleeland CS, Ryan KM. Pain assessment: Global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23:129–138. [PubMed] [Google Scholar]
- 21.Coyne JC, Smith DA. Couples coping with a myocardial infarction: A contextual perspective on wives’ distress. Journal of Personality and Social Psychology. 1991;61:404–412. doi: 10.1037//0022-3514.61.3.404. [DOI] [PubMed] [Google Scholar]
- 22.Cremeans-Smith JK, Stephens MAP, Franks MM, Martire LM, Druley JA, Wojno WC. Spouses’ and physicians’ perceptions of pain severity in older women with osteoarthritis: Dyadic agreement and patients’ well-being. PAIN®. 2003;106:27–34. doi: 10.1016/s0304-3959(03)00268-9. [DOI] [PubMed] [Google Scholar]
- 23.Druley JA, Stephens MAP, Coyne JC. Emotional and physical intimacy in coping with Lupus: Women’s dilemmas of disclosure and approach. Health Psychology. 1997;16:506–514. doi: 10.1037//0278-6133.16.6.506. [DOI] [PubMed] [Google Scholar]
- 24.Franks MM, Hong TB, Pierce LS, Ketterer MW. The association of patients’ psychosocial well-being with self and spouse ratings of patient and health. Family Relations. 2002;51:22–27. [Google Scholar]
- 25.Gaugler JE, Zarit SH, Pearlin LI. Caregiving and institutionalization: Perceptions of family conflict and socioemotional support. International Journal of Aging & Human Development. 1999;49(1):1–25. doi: 10.2190/91A8-XCE1-3NGX-X2M7. [DOI] [PubMed] [Google Scholar]
- 26.Hagedoorn M, Kuijer RG, Wobbes T, Sanderman R. Marital satisfaction in patients with cancer: Does support from intimate partners benefit those who need it the most? Health Psychology. 2000;19:274–282. [PubMed] [Google Scholar]
- 27.Hoffman DL, Dukes EM. The health status burden of people with fibromyalgia: a review of studies that assessed health status with the SF-36 or the SF-12. International Journal of Clinical Practice. 2007;62:115–126. doi: 10.1111/j.1742-1241.2007.01638.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holtzman S, DeLongis A. One day at a time: The impact of daily satisfaction with spouse responses on pain, negative affect and catastrophizing among individuals with rheumatoid arthritis. PAIN®. 2007;131:202–213. doi: 10.1016/j.pain.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 29.Issner JB, Cano A, Leonard MT, Williams AM. How do I empathize with you? Let me count the ways: Relations between facets of pain-related empathy. The Journal of Pain. 2012;13:167–175. doi: 10.1016/j.jpain.2011.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jensen MP. The validity and reliability of pain measures in adults with cancer. Journal of Pain. 2003;4:2–21. doi: 10.1054/jpai.2003.1. [DOI] [PubMed] [Google Scholar]
- 31.Jones KD, Bennett RM, Ward RL, Deodhar AA. Description of a half-day interprofessional fibromyalgia clinic with an evaluation of patient satisfaction. American Journal of Physical Medicine & Rehabilitation. 2011;90:825–833. doi: 10.1097/PHM.0b013e31821f6ed3. [DOI] [PubMed] [Google Scholar]
- 32.Keller S, Bann CM, Dodd SL, Schein J, Mendoza TR, Cleeland CS. Validity of the Brief Pain Inventory for use in documenting the outcomes of patients with noncancer pain. Clinical Journal of Pain. 2004;20:309–318. doi: 10.1097/00002508-200409000-00005. [DOI] [PubMed] [Google Scholar]
- 33.Kool MB, van Middendorp H, Bijlsma JWJ, Geenen R. Patient and spouse appraisals of health status in rheumatoid arthritis and fibromyalgia: discrepancies and associations with invalidation. Clinical and Experimental Rheumatology. 2011;29:S63–S69. [PubMed] [Google Scholar]
- 34.Kool MB, van Middendorp H, Boeije HR, Geenen R. Understanding the lack of understanding: Invalidation from the perspective of the patient with fibromyalgia. Arthritis & Rheumatism. 2009;61:1650–1656. doi: 10.1002/art.24922. [DOI] [PubMed] [Google Scholar]
- 35.Kornblith AB, Regan MM, Kim Y, Greer G, Parker B, Bennett S, et al. Cancer-related communication between female patients and male partners scale: A pilot study. Psycho-oncology. 2006;15:780–794. doi: 10.1002/pon.1004. [DOI] [PubMed] [Google Scholar]
- 36.Kuijer RG, Ybema JF, Buunk BP, DeJong GM, Thijs-Boer F, Sanderman R. Active engagement, protective buffering, and overprotection: Three ways of giving support by intimate partners of patients with cancer. Journal of Social and Clinical Psychology. 2000;19:256–275. [Google Scholar]
- 37.Laurenceau J, Bolger N. Using diary methods to study marital and family processes. Journal of Family Psychology. 2005;19:86–97. doi: 10.1037/0893-3200.19.1.86. [DOI] [PubMed] [Google Scholar]
- 38.Lobchuk MM, Kristjanson LJ, Degner LF, Blood P, Sloan J. Perceptions of symptom distress in lung cancer patients: I. Congruence between patients and primary family caregivers. Journal of Pain and Symptom Management. 1997;14:136–146. doi: 10.1016/s0885-3924(97)00022-5. [DOI] [PubMed] [Google Scholar]
- 39.Lobchuk MM, Vorauer JD. Family caregiver perspective-taking and accuracy in estimating cancer patient symptom experiences. Social Science & Medicine. 2003;57:2379–2384. doi: 10.1016/s0277-9536(03)00132-1. [DOI] [PubMed] [Google Scholar]
- 40.Looper KL, Kirmayer LJ. Perceived stigma in functional somatic syndromes and comparable medical conditions. Journal of Psychosomatic Research. 2004;57:373–378. doi: 10.1016/j.jpsychores.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 41.Lyons KS, Zarit SH, Sayer AG, Whitlatch CJ. Caregiving as a dyadic process: Perspectives from caregiver and receiver. Journals of Gerontology: Psychological Sciences. 2002;57B:P195–P204. doi: 10.1093/geronb/57.3.p195. [DOI] [PubMed] [Google Scholar]
- 42.Lyons KS, Zarit SH, Townsend AL. Families and formal service usage: Stability and change in patterns of interface. Aging & Mental Health. 2000;4(3):234–243. [Google Scholar]
- 43.Maguire MC. Treating the dyad as the unit of analysis: A primer on three analytic approaches. Journal of Marriage and the Family. 1999;61:213–223. [Google Scholar]
- 44.Manne S, Ostroff J, Rini C, Fox K, Goldstein L, Grana G. The interpersonal process model of intimacy: The role of self-disclosure, partner disclosure, and partner responsiveness in interactions between breast cancer patients and their partners. Journal of Family Psychology. 2004;18:589–599. doi: 10.1037/0893-3200.18.4.589. [DOI] [PubMed] [Google Scholar]
- 45.Manne S, Ostroff J, Sherman M, Heyman RE, Ross S, Fox K. Couples’ support-related communication, psychological distress, and relationship satisfaction among women with early stage breast cancer. Journal of Consulting and Clinical Psychology. 2004;72:660–670. doi: 10.1037/0022-006X.72.4.660. [DOI] [PubMed] [Google Scholar]
- 46.Manne S, Ostroff J, Winkel G, Grana G, Fox K. Partner unsupportive responses, avoidant coping, and distress among women with early stage breast cancer: Patient and partner perspectives. Health Psychology. 2005;24:635–641. doi: 10.1037/0278-6133.24.6.635. [DOI] [PubMed] [Google Scholar]
- 47.Martire LM, Schulz R, Keefe FJ, Rudy TE, Starz TW. Couple-oriented education and support intervention: Effects on individuals with osteoarthritis and their spouses. Rehabilitation Psychology. 2007;52:121–132. [Google Scholar]
- 48.Martire LM, Schulz R, Keefe FJ, Rudy TE, Starz TW. Couple-oriented education and support intervention for osteoarthritis: Effects on spouses’ support and responses to pain. Families, Systems & Health. 2008;26:185–195. doi: 10.1037/1091-7527.26.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McPherson CJ, Addington-Hall JM. Judging the quality of care at the end of life: can proxies provide reliable information? Social Science & Medicine. 2003;56:95–109. doi: 10.1016/s0277-9536(02)00011-4. [DOI] [PubMed] [Google Scholar]
- 50.Mease PJ, Spaeth M, Clauw DJ, Arnold LM, Bradley LA, Russell IJ, Kajdasz DK, Walker DJ, Chappell AS. Estimation of minimum clinically important difference for pain in fibromyalgia. Arthritis Care Research. 2011;63:821–826. doi: 10.1002/acr.20449. [DOI] [PubMed] [Google Scholar]
- 51.Miaskowski C, Zimmer EF, Barrett KM, Dibble SL, Wallhagen MI. Differences in patients’ and family caregivers’ perceptions of the pain experience influence patient and caregiver outcomes. Pain. 1997;72:217–226. doi: 10.1016/s0304-3959(97)00037-7. [DOI] [PubMed] [Google Scholar]
- 52.Paulson M, Norberg A, Soderberg S. Living in the shadow of fibromyalgic pain: The meaning of female partners’ experiences. Journal of Clinical Nursing. 2003;12:235–243. doi: 10.1046/j.1365-2702.2003.00733.x. [DOI] [PubMed] [Google Scholar]
- 53.Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: An overview of concepts and their measures. Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- 54.Porter LS, Keefe FJ, Baucom DH, Hurwitz H, Moser B, Patterson E, Kim HJ. Partner-assisted emotional disclosure for patients with gastrointestinal cancer. Cancer. 2009;115:4326–4338. doi: 10.1002/cncr.24578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Porter LS, Keefe FJ, McBride CM, Pollak K, Fish L, Garst J. Perceptions of patients’ self-efficacy for managing pain and lung cancer symptoms: correspondence between patients and family caregivers. PAIN®. 2002;98:169–178. doi: 10.1016/s0304-3959(02)00042-8. [DOI] [PubMed] [Google Scholar]
- 56.Porter LS, Keefe FJ, Wellington C, de Williams A. Pain communication in the context of osteoarthritis: patient and partner self-efficacy for pain communication and holding back from discussion of pain and arthristis-related concerns. Clinical Journal of Pain. 2008;24:662–668. doi: 10.1097/AJP.0b013e31816ed964. [DOI] [PubMed] [Google Scholar]
- 57.Rankin-Esquer LA, Deeter A, Taylor CB. Coronary heart disease and couples. In: Schmaling KB, Sher TG, editors. The psychology of couples and illness: Theory, research, & practice. Washington, DC: American Psychological Association; 2000. pp. 43–70. [Google Scholar]
- 58.Raudenbush SW, Brennan RT, Barnett RC. A multivariate hierarchical model for studying psychological change within married couples. Journal of Family Psychology. 1995;9:161–174. [Google Scholar]
- 59.Raudenbush SW, Bryk AS, Congdon R. Hierarchical linear and nonlinear modeling. Lincolnwood, IL: SSI; 2004. [Google Scholar]
- 60.Reamy AM, Kim K, Zarit SH, Whitlatch CJ. Understanding discrepance in perceptions of values: Individuals with mild to moderate dementia and their family caregivers. The Gerontologist. 2011;51:473–483. doi: 10.1093/geront/gnr010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Reese JB, Somers TJ, Keefe FJ, Mosley-Williams A, Lumley MA. Pain and functioning of rheumatoid arthritis patients based on marital status: Is a distressed marriage preferable to no marriage? The Journal of Pain. 2010;11:958–964. doi: 10.1016/j.jpain.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Reich JW, Olmsted ME, van Puymbroeck CM. Illness uncertainty, partner caregiver burden and support, and relationship satisfaction in fibromyalgia and osteoarthritis patients. Arthritis & Rheumatism. 2006;55:86–93. doi: 10.1002/art.21700. [DOI] [PubMed] [Google Scholar]
- 63.Revenson TA, Kayser K, Bodenmann G. Couples coping with stress: Emerging perspectives on dyadic coping. Washington, D.C: American Psychological Association; 2005. [Google Scholar]
- 64.Riemsma RP, Taal E, Rasker JJ. Perceptions about perceived functional disabilities and pain of people with rheumatoid arthritis: Differences between patients and their spouses and correlates with well-being. Arthritis Care & Research. 2000;13:255–261. doi: 10.1002/1529-0131(200010)13:5<255::aid-anr3>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 65.Rodham K, Rance N, Blake D. A qualitative exploration of carers’ and ‘patients’ experiences of fibromyalgia: One illness, different perspectives. Musculoskeletal Care. 2010;8:68–77. doi: 10.1002/msc.167. [DOI] [PubMed] [Google Scholar]
- 66.Schmaling KB, Sher TG. The psychological of couples and illness: Theory, research, and practice. Washington, D.C: American Psychological Association; 2000. [Google Scholar]
- 67.Shillam CR, Jones KD, Miller L. Fibromyalgia symptoms, physical function, and comorbidity in middle-aged and older adults. Nursing Research. 2011;60:309–317. doi: 10.1097/NNR.0b013e31822bbdfa. [DOI] [PubMed] [Google Scholar]
- 68.Smith AA, Friedemann M-L. Perceived family dynamics of persons with chronic pain. Journal of Advanced Nursing. 1999;30:543–551. doi: 10.1046/j.1365-2648.1999.01123.x. [DOI] [PubMed] [Google Scholar]
- 69.Soderberg S, Lundman B, Norberg A. Struggling for dignity: The meaning of women’s experiences of living with fibromyalgia. Qualitative Health Research. 1999;9:575–587. doi: 10.1177/104973299129122090. [DOI] [PubMed] [Google Scholar]
- 70.Soderberg S, Strand M, Haapala M, Lundman B. Living with a woman with fibromyalgia from the persepctive of the husband. Journal of Advanced Nursing. 2003;42:143–150. doi: 10.1046/j.1365-2648.2003.02597.x. [DOI] [PubMed] [Google Scholar]
- 71.Stahl SM. Fibromyalgia: The enigma and the stigma. Journal of Clinical Psychiatry. 2001;62:501–502. doi: 10.4088/jcp.v62n07a00bs. [DOI] [PubMed] [Google Scholar]
- 72.Steiner JL, Bigatti SM, Hernandez AM, Lydon-Lam JR, Johnston EL. Social support mediates the relations between role strains and marital satisfaction in husbands of patients with fibromyalgia syndrome. Families, Systems, & Health. 2010;28:209–223. doi: 10.1037/a0020340. [DOI] [PubMed] [Google Scholar]
- 73.Sylvain H, Talbot LR. Synergy towards health: A nursing intervention model for women living with fibromyalgia, and their spouses. Journal of Advanced Nursing. 2002;38:264–273. doi: 10.1046/j.1365-2648.2002.02176.x. [DOI] [PubMed] [Google Scholar]
- 74.Taylor SS, Davis MC, Zautra AJ. Relationship status and quality moderate daily pain-related changes in physical disability, affect, and cognitions in women with chronic pain. PAIN®. 2013;154:147–153. doi: 10.1016/j.pain.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tikiz C, Muezzinoglu T, Pirildar T, Taskin E, Firat A, Tuzun C. Sexual dysfunction in female subjects with fibromyalgia. Journal of Urology. 2005;174:620–623. doi: 10.1097/01.ju.0000165155.33511.eb. [DOI] [PubMed] [Google Scholar]
- 76.Turk DC, Flor H, Rudy TE. Pain and families. I. Etiology, maintenance, and psychosocial impact. PAIN®. 1987;30:3–27. doi: 10.1016/0304-3959(87)90080-7. [DOI] [PubMed] [Google Scholar]
- 77.Winters-Stone KM, Lyons KS, Bennett JA, Beer TM. Patterns and predictors of symptom incongruence in older couples coping with prostate cancer. Supportive Care in Cancer. doi: 10.1007/s00520-013-2092-0. In Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia: Report of the Multicenter Criteria Committee. Arthritis & Rheumatism. 1990;33:160–172. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 79.Yellen SB, Cella D, Webster K, Blendowski C, Kaplan E. Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. Journal of Pain and Symptom Management. 1997;13:63–74. doi: 10.1016/s0885-3924(96)00274-6. [DOI] [PubMed] [Google Scholar]
- 80.Yellen SB, Cella DF, Webster K, Blendowski C, Kaplan E. Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J Pain Symptom Manage. 1997;13(2):63–74. doi: 10.1016/s0885-3924(96)00274-6. [DOI] [PubMed] [Google Scholar]
- 81.Zarit SH, Zarit JM. Mental disorders in older adults: Fundamentals of assessment and treatment. New York, NY: The Guilford Press; 1998. [Google Scholar]


