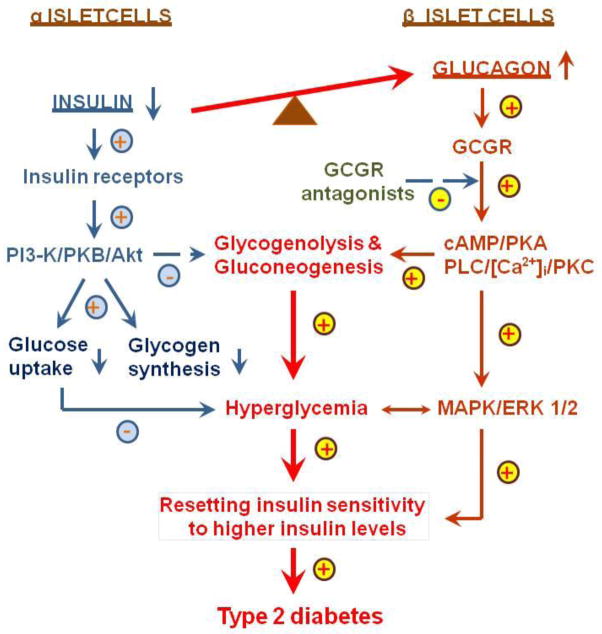
Figure 4.
A hypothesis that proposes a potential role of hyperglucagonemia in the development of hyperglycemic and metabolic phenotypes in type 2 diabetes. In human type 2 diabetes, there is an inappropriate increase in the hyperglycemic glucagon over the hypoglycemic insulin. Imbalance of the actions of insulin and glucagon in favoring the latter leads to increases in glycogenolysis and gluconeogenesis in the liver and other tissues, resulting in hyperglycemia, increased insulin resistance (resetting insulin sensitivity to higher levels of insulin) and impaired glucose tolerance. Moreover, glucagon, via direct activation of GCGR-mediated signaling pathways (cAMP-dependent protein kinase A, PI 3-K/PKB/Akt, PLC/[Ca2+]i/PKC, and MAPK/ERK 1/2), stimulates cellular growth and proliferation, leading to target organ injury. GCGR antagonists are expected to block these metabolic and growth effects of hyperglucagonemia in type 2 diabetes, and reset insulin sensitivity to lower insiulin levels. GCGR, G protein-coupled glucagon receptors; MAPK/ERK 1/2, mitogen-activated protein kinase/extracellular regulated kinases 1 and 2; PKA, protein kinase A; PI3-K, PI3-kinase; PKB/Akt, protein kinase B/AKT; and PLC/]Ca2+]i/PKC, phospholipase C/intracellular calcium/protein kinase C. Modified with permission from Li and Zhuo [38]. Targeting glucagon receptor signaling in treating metabolic syndrome and renal injury in type 2 diabetes: theory versus promise. Clinical Science 2007; 113, 183–193.