Abstract
Background.
The measurement of mobility is essential to both aging research and clinical practice. A newly developed self-report measure of mobility, the mobility assessment tool—short form (MAT-sf), uses video animations to improve measurement accuracy/precision. Using a large baseline data set, we recalibrated the items, evaluated the extent to which older patients’ self-efficacy (i.e., confidence) for walking was related to MAT-sf scores beyond their actual 400-m walk time, and assessed the relationship of the MAT-sf with body mass index and other clinical variables.
Methods.
The analyses employed baseline data from the Lifestyle Interventions and Independence for Elders Study.
Results.
Item recalibration demonstrated that the MAT-sf scoring algorithm was robust. In an analysis with 400-m walk time and self-efficacy regressed on the MAT-sf, both variables shared unique variance with the MAT-sf (p < .001). The MAT-sf was inversely related to several comorbidities, most notably hypertension and arthritis (p < .001), and scores were lowest when body mass index ≥ 35kg/m2. Finally, MAT-sf scores were directly related to Short Physical Performance Battery scores, inversely related to difficulty with activities of daily living (p < .001) and higher for men than for women (p < .001).
Conclusions.
The findings extend the validity and clinical utility of this innovative tool for assessing self-reported mobility in older adults. Longitudinal data on the MAT-sf from the Lifestyle Interventions and Independence for Elders Study will enable us to evaluate the relative contributions of self-report and performance-based measures of mobility on important health outcomes.
Key Words: Mobility, Geriatric assessment, Physical function, MAT-sf
Mobility is central to sustaining independence as people age (1,2), and loss of mobility confers an increased risk of institutionalization and death (3,4). Although objective, performance-based measures of mobility such as the 400-m walk test (5) and the Short Physical Performance Battery (SPPB) (6) have become popular among clinical researchers, self-report measures continue to play a prominent role. Taking advantage of new technology, we recently developed a short-form, 10-item mobility assessment tool (MAT-sf) that uses video animations as opposed to written or interview presented descriptions of tasks as stimuli (7). In the current study, we evaluated the item integrity of the MAT-sf and explored in greater detail the clinical validity of the measure using a large baseline data set from the Lifestyle Interventions and Independence for Elders (LIFE) Study.
There are at least two reasons for continued interest in self-reported measures of mobility. First, performance-based assessment of mobility is not always possible due to constraints with time and space, and single bouts of performance can be influenced by transient patient variables such as physical symptoms and acute illness. Second, although there is obvious overlap between self-report and objective measures of function, older adults’ perceptions often differ from objectively assessed capacities. Also, data have shown that peoples’ perceptions of their abilities are important determinants of what they will do despite objective assessments of the ability in question (8,9).
Historically, the measurement of self-reported mobility has been challenging because respondents are expected to make complex judgments about the meaning of specific tasks presented in written form or by an interviewer. Also, contextual factors that are important in making task-related judgments, such as the availability of a handrail in climbing stairs or the speed of completing a task, are ignored. These concerns prompted us to develop an animated video approach to assessing self-reported mobility, the MAT-sf (7,10).
The LIFE Study provided us with an opportunity to further examine the item calibration used in scoring the MAT-sf. More important, we set out to answer several novel clinically related questions of interest. First, motivated by previous research (8,9), we hypothesized that a measure of self-efficacy specific to the 400-m walk would account for independent variance in MAT-sf scores above and beyond participants’ actual performance on this test. Second, because considerable attention is now being given to body mass index (BMI) and physical disability with aging (11,12), and the relationship appears to be curvilinear, we expected to observe a similar inverted-U-shaped pattern between BMI classifications and MAT-sf scores. Finally, we expected MAT-sf scores to be negatively influenced by chronic health conditions and that, as reported previously (7), men would have higher scores than women, scores would be directly related to SPPB performance, and inversely related to difficulty ratings for activities of daily living (ADL).
Methods
Participants
The LIFE Study eligibility criteria targeted older persons (age 70–89) who were (a) sedentary (spending < 20 min per week in the past month getting regular physical activity and reporting less than 125min/wk of moderate physical activity); (b) at high risk for mobility disability (SPPB score of ≤ 9); (c) able to walk 400 m in ≤15min without sitting, using a walker, or needing the help of another person; and (d) able to safely participate in the intervention. Persons with a SPPB score ≤ 7 were preferentially enrolled to enrich the sample with individuals at high risk for major mobility disability. A total of 1,635 participants were randomized at eight field centers (Supplementary Appendix), although in the current analyses we used data from 1,343 participants due to early problems that several sites had with saving MAT-sf data correctly. The problem was due to a procedure initiated specifically for use in the LIFE Study and was unrelated to the actual MAT-sf software.
Measures
Information regarding participants’ demographic characteristics and comorbidities were based on responses to a structured interview. Weight was assessed in kilograms, with shoes and jackets removed, using a calibrated scale during clinical assessments. Height was measured in centimeters and converted to meters during the analysis phase of the study for the calculation of BMI.
MAT-sf.—
The MAT-sf is a 10-item computer-based assessment of mobility using animated video clips and covers a broad range of functioning. The items were selected based on individual response and information curves derived from item response theory. Each item is accompanied by an animated video clip together with the responses for that question (number of minutes, number of times, yes/no). The test can be done on any laptop, and scores are saved to an exportable file. The MAT-sf has been found to have good test–retest reliability (intraclass correlation coefficient = 0.93) (7) and validity (7,10).
Pepper assessment tool for disability.—
The pepper assessment tool for disability (PAT-D) consists of 19-items that yield three subscales and a total score (13). The three subscales include basic ADL disability, mobility disability, and instrumental activities of daily living (IADL) disability. All factors have acceptable internal consistency reliability (>.70) and test–retest reliability (>.70) coefficients. Fast walkers (gait speed = 1.35 (0.12) m/s) self-report better function on the PAT-D scales than slow walkers (gait speed = 1.00 (0.17) m/s)—effect sizes ranging from moderate to large (0.41–0.95); individuals with cardiovascular disease (CVD) have poorer scores on all scales than those free of CVD (13).
400-m walk test.—
The 400-m walk test is a modified version of a fast-pace mobility walking test originally developed by Newman and her colleagues (4). In the modified version, participants are instructed to walk at their usual walking pace for 400 m (10 laps of a 20-m course defined by two cones). The maximum time allowed for the test is 15min; participants are allowed to stop and stand to rest and may use a cane, but they are neither allowed to lean against any object to support their weight nor allowed to use a walker or to seek help from another person.
SPPB.—
The SPPB is a summary performance measure consisting of three increasingly difficult standing balance tests, usual walking speed over a 4-m distance, and time for five repeated chair stands done as quickly as possible. Each performance measure is assigned a categorical score ranging from 0 (inability to complete the test) to 4 (best performing). A summary score ranging from 0 (worst performers) to 12 (best performers) is calculated by summing the three component scores. Support for the measurement properties of the SPPB has been provided by Guralnik and colleagues (6,14).
Self-efficacy for the 400-m walk.—
A measure of self-efficacy was developed for the 400-m walk based on the methodology described by Bandura (15). After completing the 400-m walk test, participants were asked how much confidence they had in their ability to walk five different distances at the same pace 1 week hence: 5 laps, 10 laps (the same distance as today), 15 laps, 20 laps (twice as far), and 25 laps. Confidence ratings were made for each distance on a scale that ranged from 0 to 10. The verbal anchors No Confidence appeared with a value of 0, Moderate Confidence with a value of 5, and Complete Confidence with a value of 10. In the LIFE-pilot (P) study (16), we found older adults who had more severe mobility problems as defined by SPPB scores less than 7 had significantly lower mean self-efficacy scores (63.9) than those with fewer mobility problems (76.1), p < .001. Also, change in self-efficacy from 0 to 6 months was significantly related to change in satisfaction with physical function from 0 to 12 months, r = .33, p < .0001. The Cronbach alpha for this measure of self-efficacy is 0.90.
Procedures Employed to Recalibrate the MAT-sf
One goal of the present study was to recalibrate the 10 items used in the MAT-sf employing a larger and more representative sample from the study. The original calibration was conducted on a sample of N = 234 (7,10). In the recalibration procedure, we first combined data from the original calibration with baseline data from the LIFE Study. Subsequently, the same item response models were used to calibrate the items and the new item parameters for the 10-item MAT-sf to obtain individual scores for each participant.
Statistical Analyses
The recalibration was conducted using IRTPRO (Scien tific Software International, Inc., Skokie, IL). Category response curves and information curves from the recalibration were compared with those from the first calibration. Both the difference and correlation between the mobility estimates from the two calibrations were examined for assessing the effect of the recalibration. Following the original calibration, a graded response model and a two-parameter logistic model were, respectively, used for recalibrating polytomous and dichotomous responses. We further assessed goodness of fit of the unidimensional model, item fit, differential item functioning, and ceiling and floor effects.
Descriptive statistics (mean, standard deviation, and proportion) were used to characterize the sample. Analyses of the unique relationships of the 400-m walk time and self-efficacy for the 400-m walk with both the MAT-sf and the PAT-D mobility subscale were conducted using general linear models; group comparisons including BMI classifications were made using t-tests or analysis of variance. These analyses were conducted using SAS 9.2 (SAS Institute, Cary, NC).
Results
Descriptive data illustrate that 70.2% were women, 77.3% were whites, and participants had a broad range of education (Table 1). The most common comorbidity was hypertension at 69.8%, followed by diabetes at 25.3%, and cancer at 22.4%. As planned, a mean (SD) SPPB score of 7.4 (1.6) indicates that the sample had evidence of compromised physical functioning.
Table 1.
Participant Characteristics*
| Characteristic | Mean (±SD) or N (%) |
|---|---|
| Age | 78.9 (5.3) |
| Sex | |
| Male | 453 (29.8%) |
| Female | 900 (70.2%) |
| Race | |
| White | 1046 (77.3%) |
| Black | 253 (18.7%) |
| Hispanic | 26 (1.9%) |
| Other | 28 (2.1%) |
| Education | |
| Less than high school | 20 (1.5%) |
| High school (any) | 408 (31.3%) |
| Any postsecondary education (excluding graduate education) | 540 (41.4%) |
| Graduate education (any) | 335 (25.7%) |
| NIH BMI (kg/m2) classifications | |
| <18.5 (underweight) | 4 (0.3%) |
| 18.5–24.9 (normal) | 241 (17.8%) |
| 25–29.9 (overweight) | 490 (36.2%) |
| 30–34.9 (class I obesity) | 347 (25.6%) |
| 35–39.9 (class II obesity) | 167 (12.3%) |
| 40+ (class III obesity) | 104 (7.7%) |
| Comorbidities | |
| Myocardial Infarction | 110 (8.2%) |
| Hypertension | 936 (69.8%) |
| Congestive heart failure | 58 (4.3%) |
| Arthritis | 250 (18.6%) |
| Diabetes | 341 (25.3%) |
| Cancer | 301 (22.4%) |
| Physical health status | |
| MAT-sf | 49.9 (9.3) |
| 400-m walk (s) | 508.7 (113.4) |
| SPPB | 7.4 (1.6) |
| PAT-D mobility | 1.8 (0.7) |
| PAT-D basic ADLs | 1.3 (0.4) |
| PAT-D IADL | 1.1 (0.3) |
Notes: NIH = National Institutes of Health; BMI = body mass index; MAT-sf = mobility assessment tool—short form; SPPB = Short Physical Performance Battery; ADL = activities of daily living; IADL = instrumental activities of daily living.
*These results on the sample of 1,343 participants did not differ from the total sample of 1,635. Percentages for each variable may not equal 100% due to a small number of missing data points.
Item Calibration, Scoring Algorithm, and Other Relevant Metrics for the MAT-sf
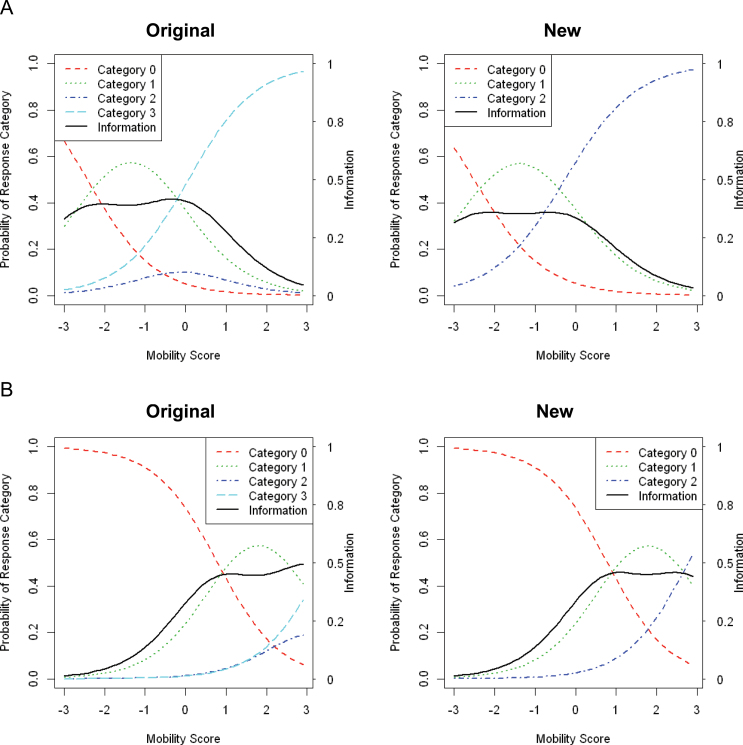
The item parameters for the MAT-sf showed only slight changes in the recalibrated set, with eight items being unaffected (data not shown). For two items, 1 and 2, the response categories had to be collapsed from 4 to 3 because the category characteristic curves showed poor performance as a higher ability category was dominated by a lower ability category. Figure 1 provides the “original” and “new” category response curves for these two items. The term “original” refers to the published calibration procedure with an N = 234; the term “new” refers to calibration from the current study (N = 1343) with combined categories in items #1 and #2. The category response curve is a graphical representation of the probability of answering an item with a given response at a particular level of ability on the construct being measured; here, ability represents mobility. For items that used the four category ordinal scales (0, 1, 2, and 3), each curve represents the likelihood of an individual’s response to each one of the categories of functional ability for that item (Figure 1A and B). A steeper category response curve generally suggests higher discriminating power of the item or item category at the location where the curve has its steepest slope. The information curve, denoted by the solid black line, indicates the amount of information contained in each item. Higher information suggests more accurate estimates of ability for a particular item or category. What is apparent in the recalibrated data for these two items, in which four categories were collapsed to three, is the very minor loss of information at ability level −0.25 for Item 1 (Figure 1A) and ability level 2.8 for Item 2 (Figure 1B). The correlation between scores using the original parameters and the new parameters approached unity (0.99).
Figure 1.
(A) Category response curves and information curve for Item 1 asking “For how many minutes could you walk on level ground at the pace shown?” On the left panel, responses to the four categories are none and 1 (Category 0), 5–15 (Category 1), 20–30 (Category 2), and more than 30 minutes (Category 3). The four dashed lines represent the probability of each response across the range of function and the y-axis is on the left. The solid line represents the information curve, and the y-axis on the right provides the scale. On the right panel, Categories 2 and 3 in the original data are combined to form the new Category 2. Original (n = 234) and new (n = 1343) response curves for Item #1 in MAT-sf. (B) Category response curves and information curve for the Item 2 asking “For how many minutes could you jog on level ground at the pace shown?” On the left panel, responses to the four categories are none and 1 (Category 0), 5–15 (Category 1), 20–30 (Category 2), and more than 30 minutes (Category 3). The four lines represent the probability of each response across the range of function and the y-axis is on the left. The solid line represents the information curve, and the y-axis on the right provides the scale. On the right panel, Categories 2 and 3 in the original data are combined to form the new Category 2. Original (n = 234) and new (n = 1643) response curves for Item #2 in MAT-sf .
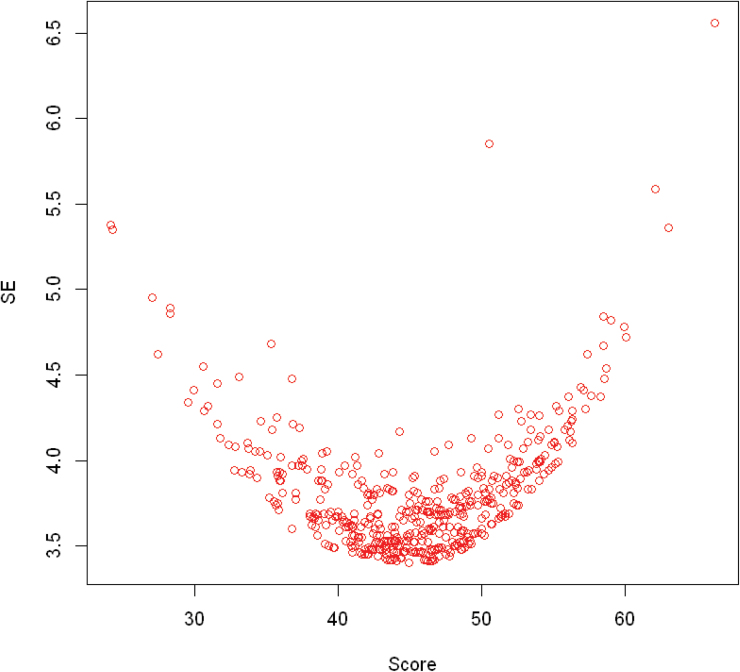
For the recalibration sample, the overall fit of the unidimensional model was satisfactory (comparative fit index = 0.84, Tucker-Lewis index = 0.87, root mean squared error of approximation = 0.15). Individual item fit statistics also suggested that item-level goodness of fit was acceptable. The p values of the chi-square-based marginal fit statistic for the 10 items ranged from 0.73 to 0.99, showing no significant deviation from the respective fitted graded response and a two-parameter logistic model. Differential item functioning analyses were conducted for sex because it is well known that men and women differ in their perceptions of physical functioning. We found neither uniform nor nonuniform differential item functioning for sex. Finally, Figure 2 provides a plot of the MAT-sf scores versus the standard errors for these scores. As expected, this relationship was U shape. Additionally, there was only 0.1% who scored in the lowest category of the MAT-sf and 1.7% scoring in the highest category, illustrating that the measure had neither floor nor ceiling effects.
Figure 2.
Plot of the MAT-sf scores versus the standard error (SE) for these scores.
Clinical Relevance and Validity of the MAT-sf: Primary Analyses
Our first analyses involved linear models that jointly regressed 400-m walk time and self-efficacy on both MAT-sf scores and the PAT-D mobility subscale. Both the 400-m walk time (seconds) and self-efficacy shared unique variance with the MAT-sf and the PAT-D; however, the MAT-sf analysis yielded an R 2 substantially larger than the PAT-D mobility analysis. For the MAT-sf (R 2 = 0.33), the respective betas (se) and t ratios for the 400-m walk and self-efficacy were −0.03 (.002), t = −14.19, p < .001 and 0.14 (.01), t = 13.48, p < .001. For the PAT-D (R 2 = 0.21), the respective betas (se) and t ratios for the 400-m walk and self-efficacy were 0.0015 (.0002), t = 9.0, p < .001 and −0.01 (.0009), t = −11.22, p < .001.
Table 2 provides the means for between-group comparisons on the MAT-sf for BMI classifications and several comorbidities. Given that the BMI categories were found to be related to MAT-sf scores, p < .001, we examined group differences using a Duncan multiple comparison test and ignored the lowest BMI category (<18.5kg/m2) because it had an n = 4. This follow-up test revealed that participants with a BMI from 35 to 39.9 (class II obesity) or 40+ (class III obesity) had lower MAT-sf scores than any other subgroup. Although we could not test for a curvilinear relationship due to the small number with a BMI less than 18.5kg/m2 (underweight), it is interesting to note that these four individual did exhibit compromised function as assessed by the MAT-sf. Also, neither the overweight (BMI = 25–29.9) nor the class I obesity (BMI = 30–34.9) subgroup had lower functioning than normal weight individuals (BMI = >18.5–24.9). Comorbidities that adversely affected MAT-sf scores included hypertension, arthritis, and diabetes (see Table 2).
Table 2.
MAT-sf Scores: BMI Classifications and Comorbidities (Prevalence > 10%)*
| Variable | Category | Mean (SD) | p-Value |
|---|---|---|---|
| BMI (kg/m2) | <.001 | ||
| <18.5 (underweight) | 42.1 (5.99) | ||
| 18.5–24.9 (normal) | 50.7 (9.83) | ||
| 25–29.9 (overweight) | 51.2 (9.11) | ||
| 30–34.9 (class I obesity) | 50.0 (9.16) | ||
| 35–39.9 (class II obesity) | 47.6 (8.56) | ||
| 40+ (class III obesity) | 45.5 (8.48) | ||
| Hypertension | 0.005 | ||
| Yes | 49.4 (9.23) | ||
| No | 51.0 (9.24) | ||
| Arthritis | <.001 | ||
| Yes | 48.3(9.08) | ||
| No | 50.3 (9.31) | ||
| Diabetes | 0.033 | ||
| Yes | 49.0 (9.6) | ||
| No | 50.2 (9.2) | ||
| Cancer | 0.364 | ||
| Yes | 49.5 (9.4) | ||
| No | 50.0 (9.2) | ||
*These results on the sample of 1,343 participants did not differ from the total sample of 1,635. Percentages for each variable may not equal 100% due to a small number of missing data points.
Clinical Relevance and Validity of the MAT-sf: Replication of Initial Validation
Men in the LIFE Study scored higher on the MAT-sf than women, 53.6 ± 8.6 versus 48.0 ± 9.0, p < .001. Examination of relationships of the MAT-sf with 400-m walk time (seconds) and SPPB scores, controlling for gender in each analysis, illustrated that higher scores on the MAT-sf were associated with faster 400-m walk times and higher SPPB scores: beta weight (se) for 400-m walk = −2.24 (0.11), confidence interval (CI) = −2.46, −2.02, R 2 = 0.28, p < .001; SPPB = 2.02 (0.14), CI = 1.99, 2.05, R 2 = 0.20, p < .001. Similar analyses of the MAT-sf with self-reported difficulty in performing mobility related tasks, basic ADLs, and IADLs using the PAT-D were also statistically significant and accounted for substantial common variance: for mobility, beta (se) = −6.62 (0.31), CI = −7.14, −5.92, R 2 = 0.31, p < .001; ADLs = −8.68 (0.60), CI = −9.86, −7.50, R 2 = 0.20, p < .001; IADLs = −7.66 (0.88), CI = −9.39, −5.93, R 2 = 0.13, p < .001. Those with high MAT-sf scores reported less difficulty with mobility, basic ADLs, and IADLs.
Discussion
The LIFE Study is the largest multicenter clinical trial to date to examine whether physical activity can delay major mobility disability among older adults of age 70–89 with compromised lower extremity function. The sample scheme was structured so that 45% of participants had a SPPB score less than or equal to 7, with no one having an SPPB score more than 9. In addition, participants had to be sedentary to qualify, yet able to complete a 400-m walk in less than or equal to 15 minutes. The current investigation used baseline data to recalibrate items in the MAT-sf using item response theory, explored several novel clinical questions related to this measure, and replicated several analyses from the original psychometric paper (7).
Results of the recalibration procedures were highly consistent with previous findings reported on the MAT-sf items (10) and speak to the robustness of the item response theory-derived scoring algorithm used for this measure. There was an almost imperceptible loss in information following recalibration of two items and the correlation between the original and revised scoring approached unity.
One of the most interesting findings of this study were the results from linear models in which the 400-m walk time and self-efficacy related to performing the 400-m walk were regressed on scores of MAT-sf and PAT-D mobility subscale. In both analyses, performance on the 400-m walk and a related measure of self-efficacy shared significant variance with both outcomes; the magnitude of the effects for both variables were comparable. It is important to reemphasize that the self-report of mobility is far more than merely a surrogate for objective measures in that it taps into perceptions that are central in understanding older adults’ willingness to engage in mobility-related activities (9), has been found to mediate improvements in mobility observed in physical activity interventions (17,18), and has been linked to survival in older patients with chronic obstructive pulmonary disease (19). In fact, in a prospective epidemiological study, we found that decline in timed stair climb performance over a 30-month period among older adults with knee pain, who had low leg strength, was dramatically more pronounced among those whose baseline confidence in their ability to climb stairs was low compared with high (20). We also point out that in the statistical models conducted in the current study, 400-m walk time and self-efficacy shared 33% in common with the MAT-sf, whereas this value was 21% for the PAT-D mobility subscale. This differential in explained variance supports the measurement advancement inherent in the MAT-sf.
The relationship observed between BMI categories and MAT-sf scores in this cohort of older adults is consistent with reports suggesting that excessive body weight is a risk factor for decline in mobility (21–24). However, it would appear that there is some protective effect associated with older adults being overweight, whereas the greatest compromise in mobility occurred in older adults who were more than or equal to Class II obesity. In a pilot study that was conducted for the main LIFE trial, Manini and colleagues (25) reported that obesity attenuated the positive effect that the physical activity intervention had on improvement in 400-m walk time. This was an interesting post hoc observation in that clinical trials of overweight and obese older adults, which have compared the relative effectiveness of walking versus walking + weight loss via intentional caloric restriction, consistently find that the combined treatment leads to better mobility-related outcomes than walking alone (12,26,27). Thus, although the current cross-sectional data would seem to support the position that weight loss is not warranted for older adults who are overweight or have class I obesity, such a conclusion seems premature. That is, weight loss in conjunction with increased physical activity is considerably different than weight loss alone and may well be preferable to assuming that being overweight or having class I obesity is health protective. It is also worth noting that 45.6% of the sample would be classified as obese, data that are slightly higher than figures published by the Centers for Disease Control and Prevention (28); needless to say, older adults, even those of age 70–90, have not been spared from the obesity epidemic.
Consistent with past research using self-reported measures of disability, participants in the LIFE Study who had arthritis (29,30), hypertension (31,32), or diabetes (33) had lower scores on the MAT-sf than those without these chronic health conditions, albeit the magnitude of these effects were small. Also, replicating our previous work (7), MAT-sf scores were higher for men than for women and were directly related to performance on the SPPB. MAT-sf scores were most strongly related to the mobility subscale of the PAT-D and had the weakest relationship to the subscale assessing IADLs (13). Of interest is the fact the MAT-sf scores exhibited a relatively normal distribution with only 0.1% scoring in the lowest category and 1.7% scoring in the highest category. By contrast, the distribution for the PAT-D mobility subscale was highly skewed (positive) with 25% reporting that they had no difficulty with mobility-related activities, a result that underscores the added value inherent in the MAT-sf technology.
The strengths of this investigation include a large sample size, advanced statistical methods employed to evaluate the measurement properties of the MAT-sf, and an interesting finding regarding the relationship between self-efficacy for 400-m walk performance and MAT-sf scores after controlling for actual walk time. Limitations include the cross-sectional nature of the study design and the fact that participants were excluded if their SPPB scores exceeded 9. The MAT-sf video technology offers a unique methodological advancement in the assessment of mobility; however, the current version does not include items related to transfer skills such as getting into or out of a bed or chair.
In summary, the MAT-sf scoring algorithm was found to be robust. Whereas the 400-m walk time was related to MAT-sf scores, self-efficacy for performing this test had an equally important relationship with the MAT-sf even after controlling for actual walking performance. Scores on the MAT-sf were lower when BMI was more than or equal to 35, compromised by several comorbidities, and were related to sex and performance on the SPPB in the expected direction. Thus, we conclude that the MAT-sf provides an innovative and valid tool for assessing self-report mobility in older adult populations that have evidence of mild to modest deficits in physical functioning. The longitudinal data in LIFE will enable us to evaluate the relative contributions of self-report and performance-based measures of mobility on important health outcomes.
Supplementary Material
Supplementary material can be found at: http://biomedgerontology.oxfordjournals.org/
Funding
The Lifestyle Interventions and Independence for Elders Study is funded by a National Institutes of Health/National Institute on Aging Cooperative Agreement (UO1 AG22376) and a supplement from the National Heart, Lung and Blood Institute (3U01AG022376-05A2S), and sponsored in part by the Intramural Research Program, National Institute on Aging, NIH.
Conflict of Interest
None of the authors had any financial interest or support for this paper.
References
- 1. Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. the index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919 [DOI] [PubMed] [Google Scholar]
- 2. Rosow I, Breslau N. A Guttman health scale for the aged. J Gerontol. 1966;21:556–559 [DOI] [PubMed] [Google Scholar]
- 3. Branch LG, Jette AM. A prospective study of long-term care institutionalization among the aged. Am J Public Health. 1982;72:1373–1379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Newman AB, Simonsick EM, Naydeck BL, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 2006;295:2018–2026 [DOI] [PubMed] [Google Scholar]
- 5. Furberg CD, Manolio TA, Psaty BM, et al. Major electrocardiographic abnormalities in persons aged 65 years and older (the Cardiovascular Health Study). Cardiovascular Health Study Collaborative Research Group. Am J Cardiol. 1992;69:1329–1335 [DOI] [PubMed] [Google Scholar]
- 6. Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94 [DOI] [PubMed] [Google Scholar]
- 7. Rejeski WJ, Ip EH, Marsh AP, Barnard RT. Development and validation of a video-animated tool for assessing mobility. J Gerontol A Biol Sci Med Sci. 2010;65:664–671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McAuley E. The role of efficacy cognitions in the prediction of exercise behavior in middle-aged adults. J Behav Med. 1992;15:65–88 [DOI] [PubMed] [Google Scholar]
- 9. Rejeski WJ, Craven T, Ettinger WH, Jr, McFarlane M, Shumaker S. Self-efficacy and pain in disability with osteoarthritis of the knee. J Gerontol B Psychol Sci Soc Sci. 1996;51:P24–P29 [DOI] [PubMed] [Google Scholar]
- 10. Marsh AP, Ip EH, Barnard RT, Wong YL, Rejeski WJ. Using video animation to assess mobility in older adults. J Gerontol A Biol Sci Med Sci. 2011;66:217–227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rejeski WJ, Ip EH, Bertoni AG, et al. ; Look AHEAD Research Group Lifestyle change and mobility in obese adults with type 2 diabetes. N Engl J Med. 2012;366:1209–1217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Villareal DT, Chode S, Parimi N, et al. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011;364:1218–1229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rejeski WJ, Ip EH, Marsh AP, Miller ME, Farmer DF. Measuring disability in older adults: the International Classification System of Functioning, Disability and Health (ICF) framework. Geriatr Gerontol Int. 2008;8:48–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Guralnik JM, Seeman TE, Tinetti ME, Nevitt MC, Berkman LF. Validation and use of performance measures of functioning in a non-disabled older population: MacArthur studies of successful aging. Aging (Milano). 1994;6:410–419 [DOI] [PubMed] [Google Scholar]
- 15. Bandura A. Self-efficacy mechanism in physiological activation and health-promoting behavior. In: Madden J, ed. Neurobiology of Learning, Emotion, and Affect. New York: Raven Press; 1991; 229–269 [Google Scholar]
- 16. Rejeski WJ, King AC, Katula JA, et al. Physical activity in prefrail older adults: confidence and satisfaction related to physical function. J Gerontol: Psychol Sci. 2008;63:19–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rejeski WJ, Ettinger WH, Jr, Martin K, Morgan T. Treating disability in knee osteoarthritis with exercise therapy: a central role for self-efficacy and pain. Arthritis Care Res. 1998;11:94–101 [DOI] [PubMed] [Google Scholar]
- 18. Brawley L, Rejeski WJ, Gaukstern JE, Ambrosius WT. Social cognitive changes following weight loss and physical activity interventions in obese, older adults in poor cardiovascular health. Ann Behav Med. 2012;44:353–364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kaplan RM, Ries AL, Prewitt LM, Eakin E. Self-efficacy expectations predict survival for patients with chronic obstructive pulmonary disease. Health Psychol. 1994;13:366–368 [DOI] [PubMed] [Google Scholar]
- 20. Rejeski WJ, Miller ME, Foy C, Messier S, Rapp S. Self-efficacy and the progression of functional limitations and self-reported disability in older adults with knee pain. J Gerontol B Psychol Sci Soc Sci. 2001;56:S261–S265 [DOI] [PubMed] [Google Scholar]
- 21. Ferraro KF, Su YP, Gretebeck RJ, Black DR, Badylak SF. Body mass index and disability in adulthood: a 20-year panel study. Am J Public Health. 2002;92:834–840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mendes de Leon CF, Hansberry MR, Bienias JL, Morris MC, Evans DA. Relative weight and mobility: a longitudinal study in a biracial population of older adults. Ann Epidemiol. 2006;16:770–776 [DOI] [PubMed] [Google Scholar]
- 23. Al Snih S, Ottenbacher KJ, Markides KS, Kuo YF, Eschbach K, Goodwin JS. The effect of obesity on disability vs mortality in older Americans. Arch Intern Med. 2007;167:774–780 [DOI] [PubMed] [Google Scholar]
- 24. Rejeski WJ, Ip EH, Marsh AP, Zhang Q, Miller ME. Obesity influences transitional states of disability in older adults with knee pain. Arch Phys Med Rehabil. 2008;89:2102–2107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Manini TM, Newman AB, Fielding R, et al. ; LIFE Research Group Effects of exercise on mobility in obese and nonobese older adults. Obesity (Silver Spring). 2010;18:1168–1175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Messier SP, Royer TD, Craven TE, O’Toole ML, Burns R, Ettinger WH., Jr Long-term exercise and its effect on balance in older, osteoarthritic adults: results from the Fitness, Arthritis, and Seniors Trial (FAST). J Am Geriatr Soc. 2000;48:131–138 [DOI] [PubMed] [Google Scholar]
- 27. Rejeski WJ, Brubaker PH, Goff DC, Jr, et al. Translating weight loss and physical activity programs into the community to preserve mobility in older, obese adults in poor cardiovascular health. Arch Intern Med. 2011;171:880–886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fakhouri THI, Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity among older adults in the United States, 2007–2010. NCHS Data Brif, No 106 [serial online] 2012 [PubMed]
- 29. Ettinger WH, Jr, Fried LP, Harris T, Shemanski L, Schulz R, Robbins J. Self-reported causes of physical disability in older people: the Cardiovascular Health Study. CHS Collaborative Research Group. J Am Geriatr Soc. 1994;42:1035–1044 [DOI] [PubMed] [Google Scholar]
- 30. Hubert HB, Bloch DA, Fries JF. Risk factors for physical disability in an aging cohort: the NHANES I Epidemiologic Followup Study. J Rheumatol. 1993;20:480–488 [PubMed] [Google Scholar]
- 31. Stuck AE, Walthert JM, Nikolaus T, Büla CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. 1999;48:445–469 [DOI] [PubMed] [Google Scholar]
- 32. Wu Y, Huang H, Wu B, McCrone S, Lai HJ. Age distribution and risk factors for the onset of severe disability among community-dwelling older adults with functional limitations. J Appl Gerontol. 2007;26:258–273 [Google Scholar]
- 33. Gregg EW, Beckles GL, Williamson DF, et al. Diabetes and physical disability among older U.S. adults. Diabetes Care. 2000;23:1272–1277 [DOI] [PubMed] [Google Scholar]