Abstract
Background/Aims
Many migraine patients develop nausea and/or vomiting (N/V) and are referred to gastroenterologists. This can lead to an inappropriate treatment and a delay of the correct diagnosis. We therefore aimed to identify predictors for migraine in patients presenting with N/V as well as headache.
Methods
A total of 407 patients who were first diagnosed with migraine at Samsung Medical Center, Seoul, Korea, in 2009 were analyzed. Among them, 261 patients had N/V (migraine with N/V group) and 146 did not (migraine without N/V group). Each patient was evaluated using a structured questionnaire.
Results
Migraine with N/V group was younger, comprised of more females, had more abnormal body mass index, less alcohol intake, more family history of migraine, higher attack severity, more stress association, more aggravation by physical activity, more abdominal pain, and more photophobia/phonophobia than migraine without N/V group. Multivariate analysis revealed that young age (age < 40 years vs. ≥ 40 years, odds ratio (OR), 2.128; 95% confidence interval (CI), 1.206-3.756; P = 0.009), female (OR, 2.703; 95% CI, 1.492-4.896; P = 0.001), family history of migraine (OR, 2.080; 95% CI, 1.169-3.700; P = 0.013), abdominal pain (OR, 4.452; 95% CI, 1.263-15.693; P = 0.020), and photophobia/phonophobia (OR, 2.296; 95% CI, 1.308-4.030; P = 0.004) were independent predictive factors associated with migraine in patients with N/V.
Conclusions
Because young age, female, family history of migraine, abdominal pain, and photophobia/phonophobia are associated with migraine in patients presenting with N/V as well as headache, physicians should have a high index of suspicion for migraine in N/V patients who belong to these categories.
Keywords: Headache, Migraine disorders, Nausea, Vomiting
Introduction
Migraine is an episodic severe headache generally associated with nausea, and/or photophobia and phonophobia.1,2 Its discriminative features include pulsating, duration of 4-72 hours, unilateral, nausea, and disabling.3 Migraine is a common disease occurring in up to 15% of the population in Western countries.4,5 In South Korea, the 1-year prevalence rate varied from 6.1%6 to 22.3%.7 However, it is frequently underdiagnosed in the general population. This is because many patients do not fully report symptoms, which is a mainstay of diagnosis, and many physicians misinterpret them.8
Migraine and headache are frequently reported by patients with gastrointestinal (GI) symptoms such as nausea, vomiting, retching, abdominal pain, and food intolerance.9-11 Among these symptoms, nausea and vomiting are the most common GI symptoms associated with migraine. Nausea occurs in more than 90% of all migraineurs and vomiting in almost 70% of all migraineurs.8 The most important features of migraine medications are rapid and effective relief of headache pain, decreasing the likelihood of headache recurrence, and not causing nausea. Nevertheless, many migraine patients suffer needlessly from their nausea and vomiting, because some migraine patients with GI symptoms are referred to a gastroenterologist and this leads to an inappropriate treatment and a delay of correct diagnosis.10
We therefore aimed to investigate the characteristics of migraine patients with nausea and/or vomiting (N/V) and to identify predictive factors associated with migraine in patients presenting with N/V as well as headache.
Materials and Methods
Patients
The present study included data from a total of 407 patients who were first diagnosed with migraine at Samsung Medical Center, Seoul, Korea, between January 2009 and December 2009. Among them, 261 patients had N/V (migraine with N/V group) and 146 did not (migraine without N/V group). We included migraine patients with either nausea or vomiting into the migraine with N/V group. The diagnosis of migraine was based on the reporting of headache characteristics and associated symptoms, as detailed in the International Classification of Headache Disorders.1 The patients underwent radiologic evaluations on the brain with computed tomography (CT), magnetic resonance imaging (MRI), and/or transcranial doppler (TCD) by indication. To rule out organic GI problems, an endoscopy was performed in some patients with upper GI symptoms. The study protocol was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board at Samsung Medical Center, Seoul, Korea.
Headache Questionnaire
Each patient was evaluated using a structured questionnaire at the first visit. The questionnaire assessed age, gender, body mass index (BMI), alcohol intake, current smoking, caffeine intake (e.g., coffee, tea and carbonated drink), family history of migraine, and characteristics of migraine. Characteristics of migraine included onset of headache, frequency of headache (per month), location and nature of headache, severity score of headache (according to a numeric score system: 0-10), presence of photophobia and/or phonophobia, concurrent symptom (e.g., nausea, vomiting, abdominal pain and eye pain) and triggers (insomnia, menstruation, physical or psychological problem). BMI was calculated as weight (kg) divided by height (m) squared (kg/m2). Abnormal BMI was defined as BMI < 18.5 kg/m2 (underweight) or ≥ 23.0 kg/m2 (overweight and obese). These categories were created with the consideration of BMI cut-off points recommended by the World Health Organization Working Group for Asian populations.12
Patients diagnosed with migraine previously or treated with medications for migraine were excluded from this study.
Data Collection and Definitions
The following clinical and laboratory information was collected from each patient: age, gender, white blood count (WBC), aspartate aminotransferase, alanine aminotransferase, total bilirubin, prothrombin time, fasting glucose, estimated glomerular filtration rate and serum low-density lipoprotein cholesterol (LDL-C). Radiologic and endoscopic data were collected from the final reports.
Abnormal WBC was defined when WBC count was < 4,000 or > 9,000/µL. Abnormal liver function was defined as serum total bilirubin > 2.0 mg/dL, aspartate aminotransferase and/or alanine aminotransferase > 40 U/L, or prothrombin time > 120%. Abnormal kidney function was defined as an estimated glomerular filtration rate < 60 mL/minutes. Dyslipidemia was defined as serum LDL-C > 130 mg/dL.
Statistical Methods
Statistical analyses were conducted using PASW Statistics 18 for Windows (SPSS, Chicago, IL, USA). The statistical results are presented as mean ± SD or number (percentages). Continuous variables were compared parametrically using Student's t test or non-parametrically using the Mann-Whitney U test. Categorical variables were compared using the χ2-test or Fisher's exact test as appropriate. Multiple logistic regression analysis was performed on variables that showed a distinct difference with statistical significance between the 2 groups, in order to identify variables independently associated with migraine in patients with N/V. A two-sided P-value < 0.05 was taken as statistically significant.
Results
Patients
Baseline characteristics of the two groups are shown in Table 1. Migraine with N/V group was younger (44.7 ± 15.0 years vs. 50.5 ± 13.5 years, P < 0.001) and had more females (70.8% vs. 63.0%, P < 0.001), more abnormal BMI (45.7% vs. 31.7%, P = 0.006), less alcohol intake (23.4% vs. 34.9%, P = 0.012), and more family history of migraine (32.2% vs. 17.8%, P = 0.002) than migraine without N/V group. However, there were no significant differences between the 2 groups regarding current smoking and caffeine intake.
Table 1.
The Baseline Characteristics of Migraine Patients According to the Presence of Nausea and/or Vomiting
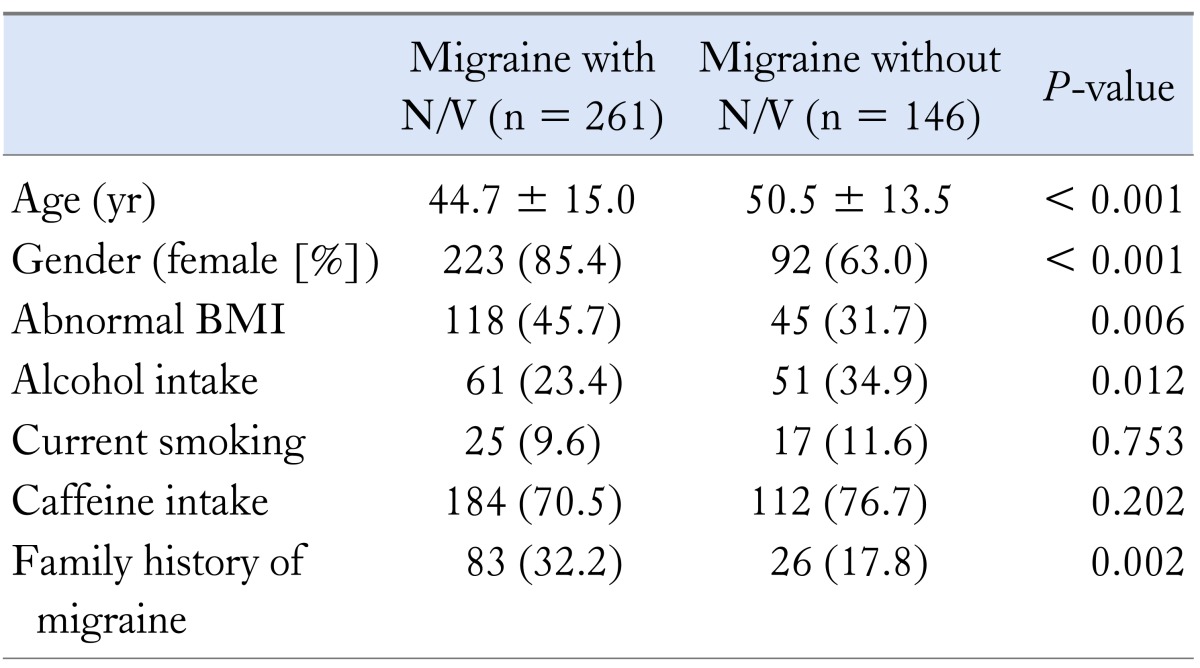
N/V, nausea and/or vomiting; BMI, body mass index.
Data are presented as mean ± SD or number (%).
Headache Characteristics
Headache characteristics of the 2 groups are shown in Table 2. Migraine with N/V group had higher attack severity (score, 7.9 ± 2.0 vs. 7.2 ± 2.2; P = 0.004), more stress association (67.8% vs. 53.2%, P = 0.005), more aggravation by physical activity (45.6% vs. 26.4%, P < 0.001), more abdominal pain (10.8% vs. 2.1%, P = 0.001), and more photophobia and/or phonophobia (41.9% vs. 17.8%, P < 0.001).
Table 2.
The Characteristics of Migraine According to the Presence of Nausea and/or Vomiting
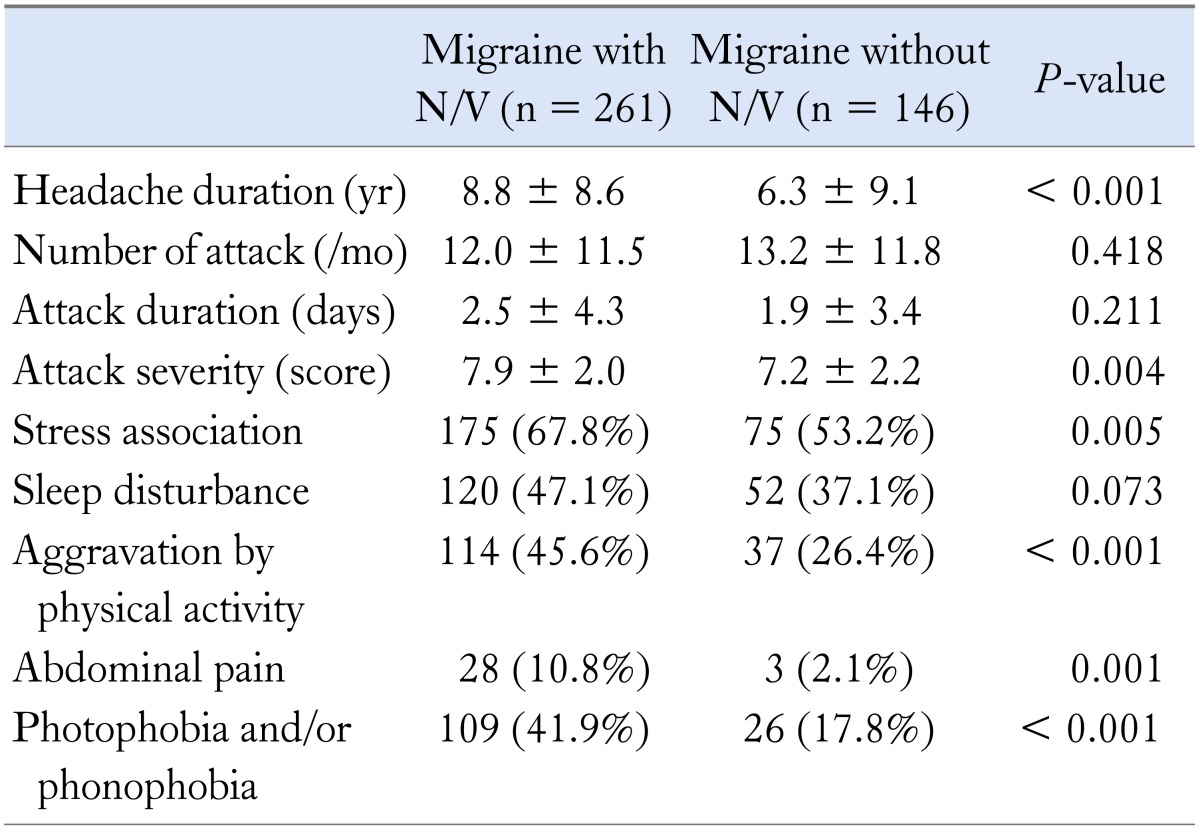
N/V, nausea and/or vomiting.
Data are presented as mean ± SD or number (%).
Laboratory, Brain Imaging and Endoscopic Results
Laboratory and brain imaging results of the 2 groups are shown in Table 3. There were no significant differences between the 2 groups in the laboratory results including WBC, liver function, kidney function, fasting glucose level, and LDL-C.
Table 3.
Comparison of Laboratory and Brain Imaging Results in Migraine Patients According to the Presence of Nausea and/or Vomiting
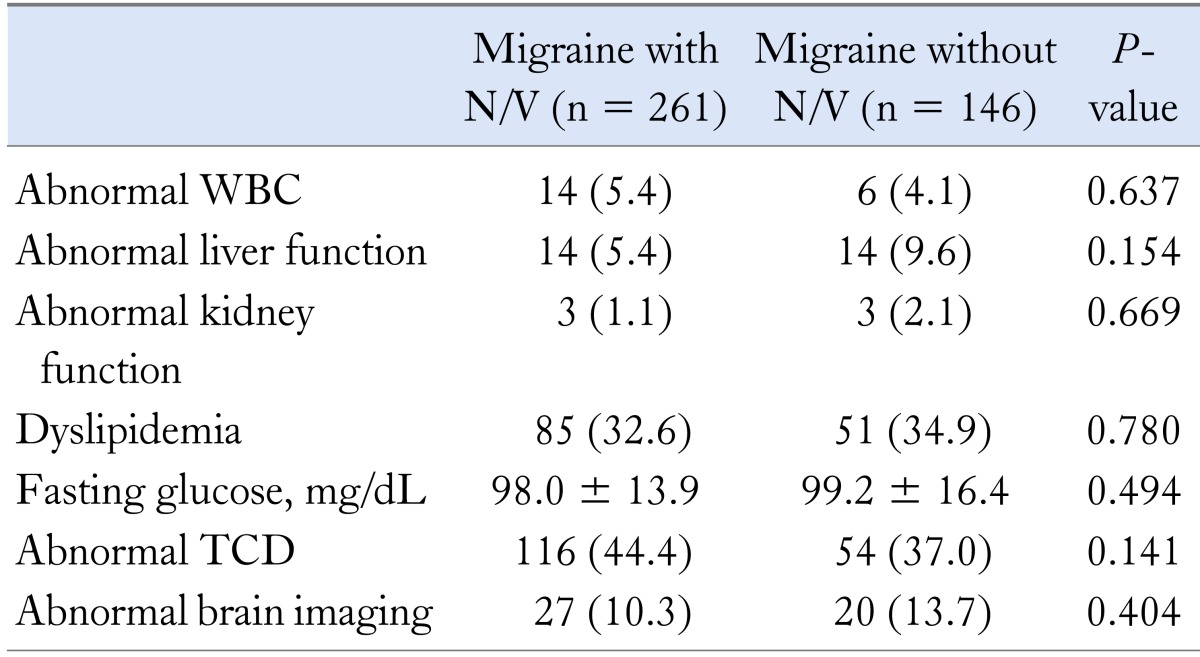
N/V, nausea and/or vomiting; WBC, white blood cell; TCD, transcranial doppler.
Data are presented as mean ± SD or number (%).
Many migraine patients showed abnormal TCD findings such as mild to moderate narrowing or decreased blood flow in the intracranial vessels. In addition, several organic lesions were found on brain CT and MRI (ischemia in 20, small unruptured aneurysm in 7, intracranial vessel stenosis in 7, Arnold-Chiari malformation in 4, small intracranial hemorrhage in 5, Rathke's cleft cyst in 3, maxillary sinusitis in 3, vertebral artery occlusion in 2, suprasellar mass in 1, vestibular schwannoma in 1 and arachnoid cyst in 1). However, there were no significant differences between the 2 groups in TCD and brain imaging.
A total of 71 (27.2%) migraine patients with N/V underwent upper GI endoscopy. Among them, 1 patient (1.4%) had peptic ulcer, 2 (2.8%) had reflux esophagitis and the remaining 68 (95.8%) had no remarkable findings.
Clinical Predictors for Migraine in Patients With Nausea and/or Vomiting
Multivariate analysis revealed that young age (age < 40 years vs. ≥ 40 years, odds ratio [OR], 2.128; 95% confidence interval [CI], 1.206-3.756; P = 0.009), female (OR, 2.703; 95% CI, 1.492-4.896; P = 0.001), family history of migraine (OR, 2.080; 95% CI, 1.169-3.700); P = 0.013), abdominal pain (OR, 4.452; 95% CI, 1.263-15.693; P = 0.020), and photophobia and/or phonophobia (OR, 2.296; 95% CI, 1.308-4.030; P = 0.004) were the independent factors associated with migraine in patients with N/V (Table 4).
Table 4.
Multivariate Analysis for Factors Associated With Migraine in Patients With Nausea and/or Vomiting

Discussion
In the present study, we sought to identify predictive factors associated with migraine in patients presenting with N/V as well as headache. Many migraine patients present with a variety of GI symptoms. Therefore, some migraine patients are referred to gastroenterologist resulting in inappropriate treatment and delay of correct diagnosis. If physicians are well aware of characteristics of migraine patients with N/V, timely diagnosis and appropriate treatment can be provided to migraine patients.
Migraine is a disorder characterized by broad sensory processing dysfunction. It can alter the perception of sensory stimuli, somatosensory, visual, auditory and olfactory sensations, which can lead to various combinations of headache, photophobia, phonophobia, and N/V.2 Autonomic dysfunction in the periaqueductal gray area of the fourth ventricle has been suggested as the cause of nausea and vomiting in patients with migraine.13 However, it is not known specifically which factors trigger N/V in patients with migraine.
In the present study, migraine patients with N/V had more abnormal BMI than migraine patients without N/V. This result is consistent with the findings of other studies that reported that both underweight and obese patients were more likely to experience severe headaches or migraines than patients with normal BMI ranges.14,15
Our results show that migraine patients with N/V have more family history of migraine than migraine patients without N/V. Migraine is well known to have a strong genetic association. Recent studies suggest multifactorial patterns of inheritance including environmental factors in addition to family history.16 The cyclic vomiting syndrome (CVS) is an episodic disorder characterized by nausea and vomiting in children, which is considered as migraine variant.17 CVS and migraine with abdominal symptoms appear to present with similar clinical features. In both CVS and migraine with abdominal symptoms, frequency of headache experienced by patient's mother was noted to be twice that of patient's father, suggesting the possibility of mitochondrial inheritance.18,19
Migraine patients with N/V had longer headache duration prior to diagnosis than migraine without N/V. It is common that patients with unexplained GI symptoms and headaches are consulted to gastroenterologist; this frequently delays a correct diagnosis and often results in an inappropriate treatment. The symptoms discussed might not include headache; they can be incomplete and misinterpreted. Therefore, physicians should include migraine in a differential diagnosis of patients presenting with N/V as well as headache and should inquire specifically about headache.
In the present study population, 47.7% (n = 197) had abnormal TCD and/or brain imaging findings. However, migraine symptoms of enrolled patients were not considered attributable to these abnormal findings. Therefore, they continued to receive migraine treatment even after detection of TCD and/or brain imaging abnormality. Nevertheless we performed additional analysis in subgroup population excluding patients with either abnormal TCD or brain imaging findings (data not shown). The results of subgroup analysis were similar to that of total study population. Young age, female, family history of migraine and photophobia and/or phonophobia were also independent predictive factors associated with migraine in patients with N/V as well as. However, abdominal pain did not show statistical significance in the subgroup analysis (P = 0.087).
In the present study, the incidence rate of N/V among migraine patients was 64.1%, which is lower than that (85.0-87.9%) of the latest report.20 This discrepancy might be due to the possible heterogeneity of the present study population. This retrospective study recruited patients who were diagnosed with migraine. Although the diagnosis of migraine was made according to the criteria of the International Classification of Headache Disorders, there might be some patients who had practically suspicious, but not definite migraine including probable migraine in the present study population. Hence, our results should be interpreted in the context of this limitation and require prospective validation studies.
In conclusion, when encountering N/V patients with headache, careful questioning about family history of migraine, abdominal pain, and photophobia and/or phonophobia is necessary. Because young age, female gender, family history of migraine, abdominal pain, and photophobia and/or phonophobia are associated with migraine, physicians should have a high index of suspicion for migraine in patients who belong to these categories, which might lead to timely diagnosis and appropriate treatment in migraine patients.
Footnotes
Financial support: None.
Conflicts of interest: None.
Author contributions: Yang Won Min and Jin Hee Lee contributed to data analysis and interpretation, and drafted the manuscript. Byung-Hoon Min, Jun Haeng Lee and Jae J Kim performed critical revision of the manuscript. Chin-Sang Chung provided the data and performed critical revision of the manuscript. Poong-Lyul Rhee designed and coordinated the study, contributed to data interpretation, and edited the manuscript.
References
- 1.Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 2.Sprenger T, Goadsby PJ. Migraine pathogenesis and state of pharmacological treatment options. BMC Med. 2009;7:71. doi: 10.1186/1741-7015-7-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Detsky ME, McDonald DR, Baerlocher MO, Tomlinson GA, McCrory DC, Booth CM. Does this patient with headache have a migraine or need neuroimaging? JAMA. 2006;296:1274–1283. doi: 10.1001/jama.296.10.1274. [DOI] [PubMed] [Google Scholar]
- 4.Stovner LJ, Andree C. Prevalence of headache in Europe: a review for the Eurolight project. J Headache Pain. 2010;11:289–299. doi: 10.1007/s10194-010-0217-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sheffield RE. Migraine prevalence: a literature review. Headache. 1998;38:595–601. doi: 10.1046/j.1526-4610.1998.3808595.x. [DOI] [PubMed] [Google Scholar]
- 6.Kim BK, Chu MK, Lee TG, Kim JM, Chung CS, Lee KS. Prevalence and impact of migraine and tension-type headache in Korea. J Clin Neurol. 2012;8:204–211. doi: 10.3988/jcn.2012.8.3.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roh JK, Kim JS, Ahn YO. Epidemiologic and clinical characteristics of migraine and tension-type headache in Korea. Headache. 1998;38:356–365. doi: 10.1046/j.1526-4610.1998.3805356.x. [DOI] [PubMed] [Google Scholar]
- 8.Silberstein SD. Migraine symptoms: results of a survey of self-reported migraineurs. Headache. 1995;35:387–396. doi: 10.1111/j.1526-4610.1995.hed3507387.x. [DOI] [PubMed] [Google Scholar]
- 9.Centonze V, Polito BM, Cassiano MA, et al. The dyspeptic syndrome in migraine: morphofunctional evaluation on 53 patients. Headache. 1996;36:442–445. doi: 10.1046/j.1526-4610.1996.3607442.x. [DOI] [PubMed] [Google Scholar]
- 10.Meucci G, Radaelli F, Prada A, et al. Increased prevalence of migraine in patients with uninvestigated dyspepsia referred for open-access upper gastrointestinal endoscopy. Endoscopy. 2005;37:622–625. doi: 10.1055/s-2005-870251. [DOI] [PubMed] [Google Scholar]
- 11.Kurth T, Holtmann G, Neufang-Huber J, Gerken G, Diener HC. Prevalence of unexplained upper abdominal symptoms in patients with migraine. Cephalalgia. 2006;26:506–510. doi: 10.1111/j.1468-2982.2005.01076.x. [DOI] [PubMed] [Google Scholar]
- 12.Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995;854:1–452. [PubMed] [Google Scholar]
- 13.Welch KM, Nagesh V, Aurora SK, Gelman N. Periaqueductal gray matter dysfunction in migraine: cause or the burden of illness? Headache. 2001;41:629–637. doi: 10.1046/j.1526-4610.2001.041007629.x. [DOI] [PubMed] [Google Scholar]
- 14.Ford ES, Li C, Pearson WS, Zhao G, Strine TW, Mokdad AH. Body mass index and headaches: findings from a national sample of US adults. Cephalalgia. 2008;28:1270–1276. doi: 10.1111/j.1468-2982.2008.01671.x. [DOI] [PubMed] [Google Scholar]
- 15.Winter AC, Berger K, Buring JE, Kurth T. Body mass index, migraine, migraine frequency and migraine features in women. Cephalalgia. 2009;29:269–278. doi: 10.1111/j.1468-2982.2008.01716.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Russell MB. Genetics of migraine without aura, migraine with aura, migrainous disorder, head trauma migraine without aura and tension-type headache. Cephalalgia. 2001;21:778–780. doi: 10.1111/j.1468-2982.2001.00249.x. [DOI] [PubMed] [Google Scholar]
- 17.Stickler GB. Relationship between cyclic vomiting syndrome and migraine. Clin Pediatr (Phila) 2005;44:505–508. doi: 10.1177/000992280504400606. [DOI] [PubMed] [Google Scholar]
- 18.Boles RG, Williams JC. Mitochondrial disease and cyclic vomiting syndrome. Dig Dis Sci. 1999;44:103S–107S. [PubMed] [Google Scholar]
- 19.Symon DN, Russell G. The relationship between cyclic vomiting syndrome and abdominal migraine. J Pediatr Gastroenterol Nutr. 1995;21(suppl 1):S42–S43. doi: 10.1097/00005176-199501001-00012. [DOI] [PubMed] [Google Scholar]
- 20.Kim BK, Chung YK, Kim JM, Lee KS, Chu MK. Prevalence, clinical characteristics and disability of migraine and probable migraine: A nationwide population-based survey in Korea. Cephalalgia. 2013;33:1106–1116. doi: 10.1177/0333102413484990. [DOI] [PubMed] [Google Scholar]


