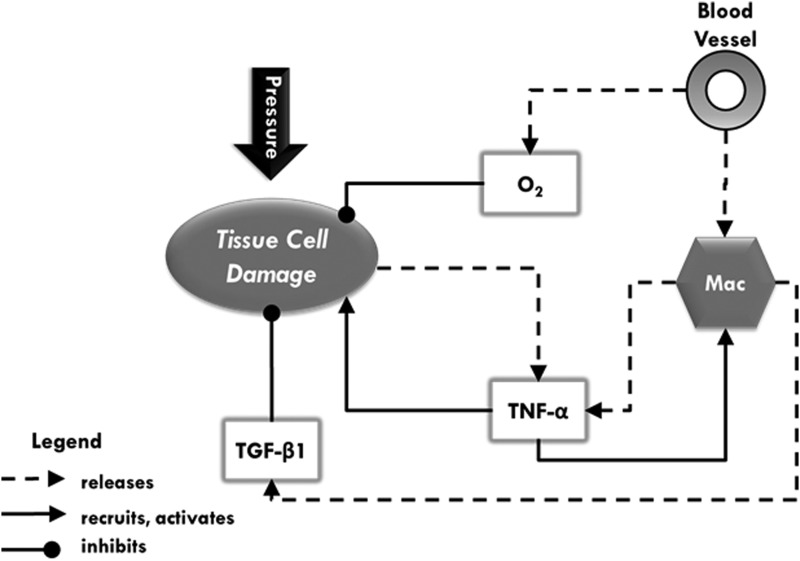
Figure 1.
A schematic of agents, data layers, and their interactions in an agent-based model of pressure ulcer formation. Dotted lines with arrowheads indicate release (e.g., activated macrophages release two types of mediators), while solid lines with arrowheads indicate chemoattraction and/or activation of cells by mediators. Solid lines with circular heads indicate inhibition (e.g., oxygen and transforming growth factor beta-1 [TGF-β1] help prevent tissue cell damage). The types of agents in this model are blood vessels, macrophages (Mac), and tissue cells. Pressure is a status that affects the components of the model. When pressure is applied, tissue cells incur damage (lose health), and blood vessels constrict. This constriction reduces the amount of material that can flow through blood vessels, which, in essence, lowers the amount of oxygen and number of macrophages entering the simulation. Molecular oxygen (O2), represented as a data layer in this model, is necessary for tissue cell health. Therefore, oxygen depletion causes further damage. Damaged tissue cells release tumor necrosis factor alpha (TNF-α), which causes activation of nearby macrophages. Activated macrophages release both TNF-α and TGF-β1, each of which are data layers that represent canonical pro- or anti-inflammatory responses, respectively. Each of these cytokines stands for a group of several pro- and anti-inflammatory mediators that participate in these respective responses. These data layers and oxygen diffuse and decay at each time step (tick). They not only act on agents in their vicinity and in a concentration-dependent manner, but also provide a chemoattractant gradient for some agents. Macrophages in the presence of TNF-α become activated. Both TGF-β1 and oxygen increase the health of nearby tissue cells.