Abstract
OBJECTIVE
New-onset diabetes mellitus (DM) in elderly patients is associated with increased risk of diabetes complications and mortality. It is unknown whether glycemic control in this population influences the mortality risk.
RESEARCH DESIGN AND METHODS
The current study was conducted using the computerized database of the Sharon-Shomron District of Clalit Health Services in Israel. Included in the study were subjects 65 years of age and above with new-onset DM. The primary outcome measures were all-cause mortality and coronary revascularization procedures with either percutaneous coronary intervention or coronary artery bypass grafting.
RESULTS
Participants (n = 2,994) were stratified into four groups according to their mean HbA1c levels during the follow-up period (<6.5% [48 mmol/mol], 6.5–6.99% [48–52 mmol/mol], 7–7.49% [53–57 mmol/mol], and ≥7.5% [58 mmol/mol]). During a mean follow-up of 5.54 ± 2.1 years, 1,173 (39.17%) participants died and 285 (9.51%) underwent coronary revascularization. An HbA1c level >7.5% (58 mmol/mol) was associated with a significantly increased all-cause mortality rate (hazard ratio [HR] 1.74 [95% CI 1.2–1.8], P < 0.0001). This difference remained statistically significant after a multivariate model adjusted for the conventional cardiovascular risk factors and for the use of hypoglycemic agents and statins. Kaplan-Meier survival plots revealed lower survival rates in this group of patients. Coronary revascularization rates were highest among subjects with HbA1c 6.5–6.99% (48–52 mmol/mol) (HR 1.6 [1.01–2.4], P < 0.05) and lowest in patients with HbA1c ≥7.5% (58 mmol/mol).
CONCLUSIONS
An HbA1c level >7.5% (58 mmol/mol) is associated with increased risk for all-cause mortality and with a lower revascularization rate in elderly patients with new-onset DM.
The incidence of diabetes mellitus (DM) increases with age. The high rate of occurrence of DM in the elderly population can be explained by age-related changes in the carbohydrate metabolism (1,2) but mainly by adverse lifestyle factors (3,4).
The natural history and outcome of new-onset DM in the elderly is not clear, due to scarce and conflicting data. A Chinese study suggests that DM diagnosed in older age is milder and associated with less frequent microvascular complications compared with DM diagnosed at younger age (5). Some studies found higher cardiovascular and all-cause mortality rates in the elderly with new-onset DM, compared with nondiabetic elderly subjects (6–9). However, another study found excess of mortality only in elderly females with new-onset DM but not in males (10).
No data exist regarding the influence of glycemic control on the morbidity and mortality of elderly patients with new-onset DM. Previous studies did not consider the influence of other cardiovascular risk factors or the use of hypoglycemic agents on the morbidity and mortality. As a consequence, there are no clinical guidelines specific for this group of patients (11,12).
The aim of this retrospective observational cohort study was to evaluate the association between glycated hemoglobin (HbA1c) levels and all-cause mortality and coronary revascularization procedures in elderly patients with new-onset DM.
RESEARCH DESIGN AND METHODS
Study population
The cohort included residents of the Sharon-Shomron District, Israel, who were medically insured by Clalit Health Services (CHS), the largest health maintenance organization in Israel. CHS insures >50% of the district's population, which is mostly urban and includes both Jews and Arabs. All medical information obtained at the primary care clinics is recorded in the CHS computerized database and can be accessed at the level of the individual patient. Each family physician is responsible for routinely updating the computerized medical records during each patient visit and after any hospital admission. The database includes a list of all diagnoses, demographic data, laboratory values, medications, and medical procedures. This database was the source for our study.
Sample selection
All cases of new-onset DM in elderly patients during 2003 or 2004 were identified. For patients diagnosed in 2003, data were obtained until December 2010. For those diagnosed during 2004, information was collected until December 2011. We included patients who were 65 years of age or older and had at least two blood glucose values of 126 mg/dL and above during the same year. All of the subjects included in the study had available HbA1c levels. We excluded from the analysis those who, in the year preceding the inclusion, had blood glucose values ≥126 mg/dL, had HbA1c ≥6.5% (48 mmol/mol), and/or purchased oral glucose-lowering medications or insulin. Subjects who had died during the inclusion year were excluded from the cohort. Patients were followed for 7 years or until they underwent a coronary revascularization procedure or died.
Study design
We classified the patients into four groups, according to the average HbA1c values during the follow-up period: HbA1c <6.5% (48 mmol/mol), HbA1c 6.5−6.99% (48–52 mmol/mol), HbA1c 7–7.49% (53–57 mmol/mol), and HbA1c ≥7.5% (58 mmol/mol). The average HbA1c was calculated as the mean of all HbA1c values during the follow-up period. For each group, data about sex, smoking status, blood pressure, and BMI was obtained. Information regarding written diagnosis of ischemic heart disease (IHD), peripheral vascular disease (PVD), hypertension (HTN), hyperlipidemia, and chronic renal failure (CRF) at the time of the inclusion was collected. Laboratory data including average glucose, total cholesterol, LDL cholesterol (LDL-c), HDL cholesterol (HDL-c), and triglycerides was collected. The average values were calculated as the mean of the first values in each follow-up year. We obtained data about purchasing oral antihyperglycemic medications, insulin, and statins. Drug compliance was considered consistent if the patient purchased the monthly dose of the drug at least six times per year, during at least 4 of the 7 follow-up years.
Study end points
The outcome measures were all-cause mortality and documentation of percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG) surgery during the follow-up period.
Ethical considerations
The local institutional ethics committee approval was given on December 2011. In accordance with Ministry of Health regulations, the institutional ethics committee did not require written informed consent, because the data were anonymously collected from the computerized medical files, with no participation by the patients.
Statistical analysis
The baseline clinical characteristics of the four patient groups were compared using ANOVA test for continuous variables and χ2 test for nonparametric variables. Cox proportional hazards regression model analysis was used to estimate hazard ratios (HRs) and 95% CIs for all-cause mortality and coronary revascularization (PCI or CABG) according to the four HbA1c groups. This analysis was adjusted for age, sex, BMI, systolic and diastolic blood pressure, previous IHD, previous CRF, current smoking, hypoglycemic medication use, statin use, and LDL-c. Kaplan-Meier survival curve was plotted for all-cause mortality, comparing the four groups according to HbA1c levels. Statistical analysis was performed with the use of SPSS statistical software for windows version 20.0.
RESULTS
Twenty-one thousand eight hundred and fifty-five patients met the inclusion criteria. Fifteen thousand five hundred and fifty were excluded because of blood glucose values >126 mg/dL, HbA1c ≥6.5% (48 mmol/mol), or use of antidiabetic medications before the inclusion. Another 1,141 subjects who died during the inclusion year were excluded. Five thousand one hundred and sixty-four subjects with a mean age of 77.4 ± 7.5 years were available for analysis.
Only 2,994 of them had HbA1c levels measured during the study period. The mean age for subjects with measured HbA1c levels was 75.6 years, compared with 79.8 years for subjects without HbA1c measurement (P < 0.0001). The average glucose value was 131.4 ± 28.5 mg/dL, compared with 122.7 ± 28.9 mg/dL for subjects without HbA1c measurement (P < 0.0001). In the group of subjects with measured HbA1c levels, the all-cause mortality rate during the follow-up years was 40% and revascularization rate 9.5%, compared with 69% mortality and 3.3% revascularization in subjects with no HbA1c measurement (P < 0.0001).
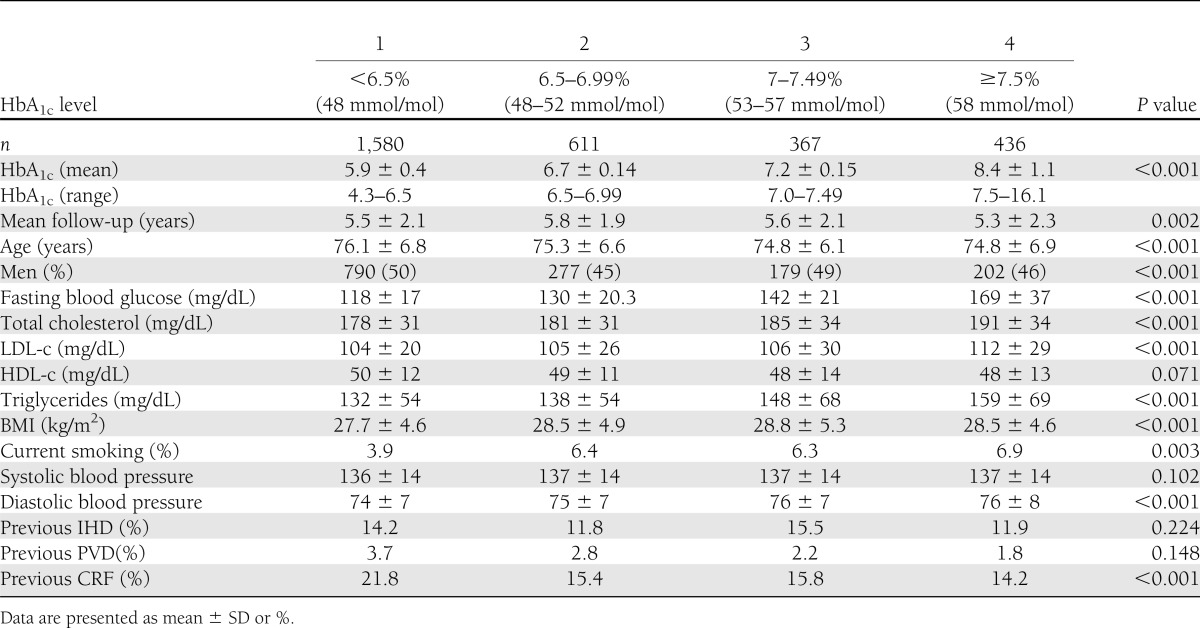
Out of the 2,994 subjects who were available for analysis, 1,448 (48.36%) were males. The subjects were stratified by their mean HbA1c level during the follow-up period. Table 1 shows baseline characteristics of the four groups. HbA1c levels correlated with the fasting blood glucose and triglycerides levels. The LDL-c level was significantly higher in the fourth group. Smoking rates and BMI were significantly lower in the lowest HbA1c group. Other cardiovascular risk factors, including HDL-c levels and systolic blood pressure, were similar between the four groups. Only 11.2% of the patients in the lowest HbA1c group acquired hypoglycemic medications. With higher HbA1c levels, the use of hypoglycemic medications was more prevalent: 29.8, 39.2, and 37.4% in the second, third, and fourth groups, respectively (P < 0.001). The majority of the treated patients used oral hypoglycemic medications (11.1, 29.8, 37.3, and 35.3% respectively; P < 0.001). Only 3% of the patients in the fourth group were treated with insulin alone or in combination with oral hypoglycemic medications. The rate of insulin treatment in the other groups was even lower (0.1, 0.2, and 2.2% in the first, second, and third group, respectively; P < 0.001). Statin use was highest in the second group (51%) and lowest in the fourth group (30%).
Table 1.
Baseline characteristics of the subjects stratified by their HbA1c levels
HbA1c level and mortality
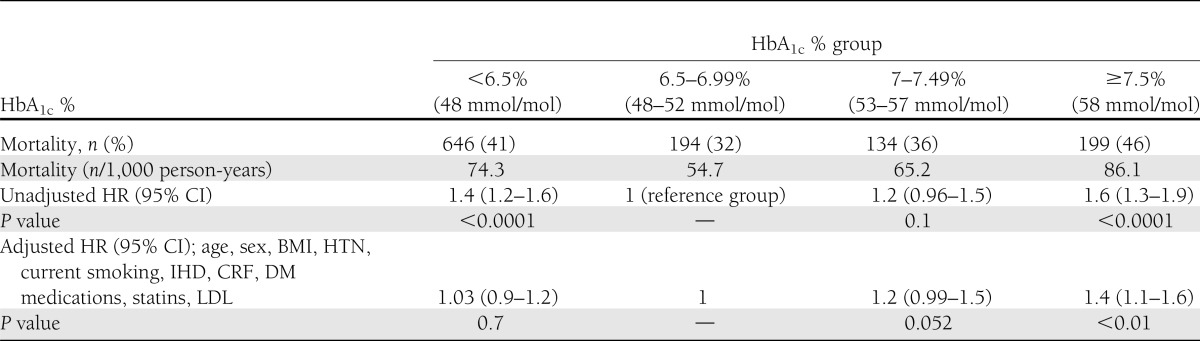
A total of 1,173 subjects died during the follow-up years. All-cause mortality rates were 41, 32, 36, and 46% in the four groups (Table 2). A multivariate model, adjusted for age, sex, previous IHD, previous CRF, use of statin and hypoglycemic medications, current smoking, BMI, systolic and diastolic blood pressure, and LDL-c, was conducted. An HbA1c level >7.5% (58 mmol/mol) was associated with a significantly increased mortality rate, compared with the 6.5–6.99% (48–52 mmol/mol) HbA1c group, which had the lowest mortality rate (adjusted HR 1.4 [95% CI 1.1–1.6], P < 0.01). In subjects with HbA1c 7–7.49% (53–57 mmol/mol), mortality rates were higher, compared with the lowest mortality group (adjusted HR 1.2 [0.99–1.5], P = 0.052), but did not reach statistical significance (Table 2). Because of the broad range of HbA1c in the fourth group, we divided these subjects into two subgroups: HbA1c 7.5–8.5% (58–69 nmol/mol) and HbA1c >8.5% (>69 nmol/mol). There was a higher mortality rate in subjects with HbA1c >8.5% (69 nmol/mol) compared with subjects with HbA1c 7.5–8.5% (58–69 nmol/mol) levels, but this difference was not statistically significant (51.4 vs. 43%, P = 0.098).
Table 2.
HRs for all-cause mortality according to HbA1c levels
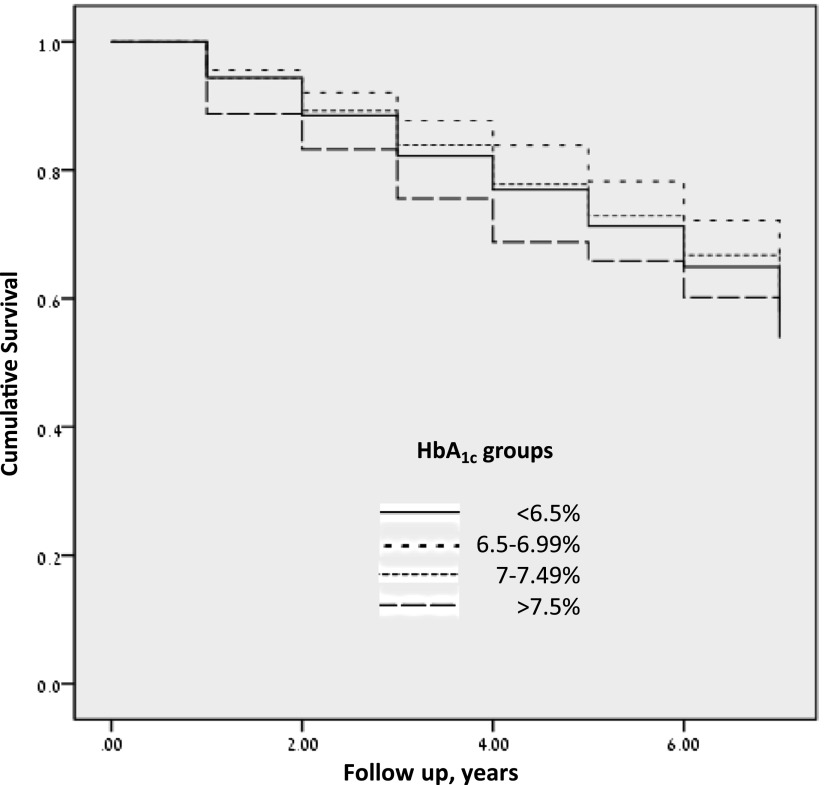
The average survival time was 5.8, 6.1, 5.8, and 5.4 years in the four groups. Figure 1 depicts the Kaplan-Meier survival curves according to HbA1c levels. The lowest survival rates were found in patients with HbA1c >7.5% (58 mmol/mol), and the highest survival rates in patients with HbA1c 6.5–6.99% (48–52 mmol/mol). The lines separated after 1 year of follow-up and remained separated during the entire follow-up period.
Figure 1.
Kaplan-Meier survival plots for all-cause mortality according to HbA1c levels.
HbA1c levels and coronary revascularization
A total of 285 subjects underwent coronary revascularization procedures (PCI or CABG) during the follow-up years. Coronary intervention rates were 9.7, 11, 9.5, and 7% in the four groups (Table 3). A multivariate model, adjusted for age, sex, previous IHD, previous PVD, previous CRF, use of statin and hypoglycemic medications, current smoking, BMI, systolic and diastolic blood pressure, total cholesterol, HDL-c, LDL-c, and triglycerides, was conducted. The revascularization rate was highest in subjects with HbA1c 6.5–6.99% (48–52 mmol/mol) and significantly higher compared with the HbA1c ≥7.5% (58 mmol/mol) group, which had the lowest revascularization rate (adjusted HR 1.6 [95% CI 1.01–2.4], P < 0.05). Because of the broad range of HbA1c in the fourth group, we divided these subjects into two subgroups: HbA1c 7.5–8.5% (58–69 nmol/mol) and HbA1c >8.5% (>69 nmol/mol). There was a lower revascularization rate in subjects with HbA1c >8.5% (69 nmol/mol) compared with subjects with HbA1c 7.5–8.5% (58–69 nmol/mol) levels, but this difference was not statistically significant (5.1 vs. 8.1%, P = 0.26).
Table 3.
HRs for coronary revascularization (PCI and CABG) according to HbA1c levels

CONCLUSIONS
Evidence on the optimal glycemic control for the subgroup of patients with new-onset DM in older age (65 years of age and above) is limited. The few studies that compared elderly subjects with new-onset DM to nondiabetic patients demonstrated short-term elevation in all-cause and cardiovascular mortality (6–10) and long-term elevation of microvascular and macrovascular complications (7). None of these studies checked the association of glycemic control with mortality or diabetes complications. As a consequence, the guidelines of the international diabetic and geriatric associations do not deal with this special population (11,12).
In this large observational cohort study, we have demonstrated that HbA1c level ≥7.5% (58 mmol/mol) during 7 years follow-up in elderly patients with new-onset DM is associated with significantly increased all-cause mortality compared with lower HbA1c levels. Within this group of patients, HBA1c >8.5% (69 nmol/mol) was associated with an even higher mortality rate, although this difference did not reach statistical significance. The lowest mortality rate was found in subjects with HbA1c 6.5–6.99% (48–52 mmol/mol). Data regarding the cause of death and prevalence of hypoglycemia were not available.
It is important to emphasize that the subjects with the highest HbA1c levels had an unfavorable cardiovascular risk factors profile, including higher LDL-c and triglyceride level, lower HDL-c, higher smoking rate, and higher diastolic blood pressure. In addition, the use of statins was lowest in subjects with HbA1c ≥7.5% (58 mmol/mol) and highest in subjects with HbA1c 6.5–6.99%. Nevertheless, the difference in mortality rates remained statistically significant after multivariate analysis. Kaplan-Meier survival plots revealed lower survival rates in this group of patients.
The association between glycemic control, diabetes complications, and mortality has been investigated for many years. A large retrospective cohort study of patients older than 50 years with long-standing type 2 DM and intensive hypoglycemic treatment demonstrated a U-shaped pattern of risk association between HbA1c levels and mortality. HbA1c of ∼7.5% (58 mmol/mol) was associated with the lowest all-cause mortality rate (13). The difference in mortality patterns between our finding and the aforementioned study underscores the need to differentially treat elderly patients with new-onset DM and elderly patients with long-standing disease.
The group with the lowest HbA1c had a higher mortality rate compared with the 6.5–6.99% group. This finding is in accordance with other study findings, which demonstrated higher mortality in elderly patients with very tight glycemic control (13,14). In our study, the same pattern was found in the elderly with new-onset DM. However, the former studies included subjects with long-standing DM who were intensively treated with various hypoglycemic medications, whereas in our cohort, only 11.2% of these subjects used hypoglycemic medications. We assume that the mildly elevated glucose of the subjects in the first group of our cohort may reflect other detrimental disease and is not directly related to DM or its treatment.
The second main finding of our study is that coronary revascularization rates were significantly higher in subjects with HbA1c 6.5–6.99% (48–52 mmol/mol) compared with subjects with HbA1c ≥7.5% (58 mmol/mol), who had the lowest revascularization rate. Within this group of patients, HbA1c >8.5% was associated with an even lower revascularization rate, although this difference was not significant. This inverse relationship between mortality and revascularization rates may reflect a protective effect of revascularization against mortality in elderly patients with new-onset DM. Another possibility is that the poor glycemic control of patients in the fourth group is a marker for suboptimal medical treatment: only 37.4% of them received hypoglycemic medications regularly, the statin use in this group was lowest, the current smoking rate was highest, and they underwent less revascularization procedures. Considerable reasons for undertreatment include poor compliance for medical treatment, lower accessibility to medical services, or poor functional status. Unfortunately, the CHS database does not include information regarding these issues.
Although our study is the first to investigate the association of HbA1c, mortality, and coronary revascularization in elderly patients with new-onset DM, it has several potential limitations that should be considered. First, more than half of the subjects who fulfilled the inclusion criteria were excluded from analysis because they did not have HbA1c measurements. These patients were significantly older, had significantly lower fasting blood glucose, underwent less revascularization procedures, and had a much higher mortality rate. Second, the HbA1c level of the first group ranged from 4.3 to 6.5% (29–48 mmol/mol), which means that probably a portion of this group did not have DM at all. It is important to emphasize that in this group, 21.8% of the subjects had previous CRF. HbA1c values may be falsely elevated or decreased in diabetic subjects with chronic kidney disease; however, in most of the methods used to measure HbA1c, this difference is not clinically significant (clinically significant difference is defined as ≥0.5) (15,16). Nevertheless, in accordance with the low HbA1c, the mean glucose and mean triglyceride values of these subjects were the lowest, as well. This suggests that as a group, we can rely on the HbA1c results. On the other hand, the group of patients with HbA1c ≥7.5% (58 mmol/mol) also had heterogeneous glycemic control (HbA1c 7.5% −16.1% [58–152 mmol/mol]). Subanalysis of this group of patients showed that the mortality rate was higher and revascularization rate lower with HbA1c levels >8.5% (69 nmol/mol). Third, the study was not designed to examine the potential influence of a specific glucose-lowering agent on mortality and revascularization.
Our study is the first in the published literature that focuses on the association between glycemic control, mortality, and revascularization in elderly patients with new-onset DM. In accordance with our findings, an HbA1c target of <7.5% (58 mmol/mol) is associated with a lower mortality rate in elderly patients with new-onset DM. Further research is needed to determine the recommended glycemic control target in this unique population.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
O.T. wrote the manuscript. E.A., A.J., M.G.-C., and P.K. reviewed the manuscript. S.A., E.C., and D.H. researched data. D.H. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Meneilly GS. Pathophysiology of type 2 diabetes in the elderly. Clin Geriatr Med 1999;15:239–253 [PubMed] [Google Scholar]
- 2.Motta M, Bennati E, Capri M, Ferlito L, Malaguarnera M. Diabetes mellitus in the extreme longevity. Exp Gerontol 2008;43:102–105 [DOI] [PubMed] [Google Scholar]
- 3.Mozaffarian D, Kamineni A, Carnethon M, Djoussé L, Mukamal KJ, Siscovick D. Lifestyle risk factors and new-onset diabetes mellitus in older adults: the cardiovascular health study. Arch Intern Med 2009;169:798–807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crandall J, Schade D, Ma Y, et al. Diabetes Prevention Program Research Group The influence of age on the effects of lifestyle modification and metformin in prevention of diabetes. J Gerontol A Biol Sci Med Sci 2006;61:1075–1081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang Y, Qin MZ, Liu Q, Liu Q, Chang ZW. Clinical analysis of elderly patients with elderly-onset type 2 diabetes mellitus in China: assessment of appropriate therapy. J Int Med Res 2010;38:1134–1141 [DOI] [PubMed] [Google Scholar]
- 6.Smith NL, Barzilay JI, Kronmal R, Lumley T, Enquobahrie D, Psaty BM. New-onset diabetes and risk of all-cause and cardiovascular mortality: the Cardiovascular Health Study. Diabetes Care 2006;29:2012–2017 [DOI] [PubMed] [Google Scholar]
- 7.Bethel MA, Sloan FA, Belsky D, Feinglos MN. Longitudinal incidence and prevalence of adverse outcomes of diabetes mellitus in elderly patients. Arch Intern Med 2007;167:921–927 [DOI] [PubMed] [Google Scholar]
- 8.Panzram G, Zabel-Langhennig R. Prognosis of diabetes mellitus in a geographically defined population. Diabetologia 1981;20:587–591 [DOI] [PubMed] [Google Scholar]
- 9.Croxson SC, Price DE, Burden M, Jagger C, Burden AC. The mortality of elderly people with diabetes. Diabet Med 1994;11:250–252 [DOI] [PubMed] [Google Scholar]
- 10.Tan HH, McAlpine RR, James P, et al. DARTS/MEMO collaboration Diagnosis of type 2 diabetes at an older age: effect on mortality in men and women. Diabetes Care 2004;27:2797–2799 [DOI] [PubMed] [Google Scholar]
- 11.American Diabetes Association Standards of medical care in diabetes—2012. Diabetes Care 2012;35(Suppl. 1):S11–S63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sinclair A, Morley JE, Rodriguez-Mañas L, et al. Diabetes mellitus in older people: position statement on behalf of the International Association of Gerontology and Geriatrics (IAGG), the European Diabetes Working Party for Older People (EDWPOP), and the International Task Force of Experts in Diabetes. J Am Med Dir Assoc 2012;13:497–502 [DOI] [PubMed] [Google Scholar]
- 13.Currie CJ, Peters JR, Tynan A, et al. Survival as a function of HbA(1c) in people with type 2 diabetes: a retrospective cohort study. Lancet. 2010;375:481–489 [DOI] [PubMed]
- 14.Gerstein HC, Miller ME, Byington RP, et al. Action to Control Cardiovascular Risk in Diabetes Study Group Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545–2559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Little RR, Rohlfing CL, Tennill AL, et al. Measurement of Hba(1C) in patients with chronic renal failure. Clin Chim Acta 2013;418:73–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Little RR, Tennill AL, Rohlfing C, et al. Can glycohemoglobin be used to assess glycemic control in patients with chronic renal failure? Clin Chem 2002;48:784–786 [PubMed] [Google Scholar]