Abstract
OBJECTIVE
Metabolic memory, in which past hyperglycemia could affect future retinopathy, is a potential issue in studying the relationship between glycemia and retinopathy. We examined retrospectively if mean “metabolic memory-free” glycosylated hemoglobin A1C (HbA1c) values covering total diabetes duration could predict retinopathy in younger-onset type 1 diabetes mellitus (T1DM).
RESEARCH DESIGN AND METHODS
Inclusion criteria were T1DM onset before age 30 years, first visit to our center between 1988 and 1990 soon after onset, continuous HbA1c data for 20 years, and a 20-year follow-up retinopathy examination. Retinopathy predictive capabilities of HbA1c variables were examined.
RESULTS
Of 15 subjects, 5 were retinopathy-positive and 10 were retinopathy-negative at the 20-year follow-up. Mean metabolic memory-free HbA1c values for the 20 years showed a substantial capacity to predict retinopathy at 20 years. The longer the period without HbA1c data following onset in simulation, the less accurate the prediction.
CONCLUSIONS
HbA1c values may predict retinopathy better if metabolic memory-free data are used.
The metabolic memory for glycemia, in which past hyperglycemia could be a risk factor for future retinopathy (1), might affect evaluation of the influence of glycosylated hemoglobin A1C (HbA1c) values on retinopathy if there were periods during the diabetes duration in which HbA1c values were unknown. Observing “metabolic memory-free” type 1 diabetes mellitus (T1DM) patients with continuous HbA1c data just after onset may avoid this effect. We studied if mean HbA1c values could predict retinopathy at 20 years after onset in selected younger T1DM patients minimally affected by hypertension and dyslipidemia.
RESEARCH DESIGN AND METHODS
The Tokyo Women’s Medical University’s Ethics Committee approved this retrospective study. Inclusion criteria were as follows: first visit to the Tokyo Women’s Medical University Diabetes Center between 1988 and 1990; T1DM onset before age 30 years; first visit to the center within 12 months after onset; and follow-up for 20 years after clear onset determined with clear clinical features within a certain month, with continuous HbA1c data, and a 20-year retinopathy examination at the center (8,912, 186, 60, and 15 cases, respectively).
All patients received diagnoses from center specialists, were ketosis-prone, had no history of obesity (BMI >26 kg/m2), and began continuous insulin treatment within 13 months of onset. Retinopathy was examined ophthalmoscopically after mydriasis by center ophthalmologists and was defined as positive by the presence of definite microaneurysm or retinal hemorrhage, or both, in one eye at least once during the 20th year. To maximize standardization, we used HbA1c values measured only at our institute by high-performance liquid chromatography. By our own formulas, we calibrated values between the instruments used (HA8120, HA8121, HA8131, HA8150, HA8160, HA8180; ARKRAY, formerly Kyoto Daiichi Kagaku, Kyoto, Japan). HbA1c values were measured principally once every 1 or 2 months, but sometimes less regularly. A given year’s yearly mean HbA1c value was determined by averaging the monthly values measured that year. If there were no HbA1c measurements during a year, then it was estimated as the average of the previous year's and the next year’s mean values. Patients with more than two such estimated years were excluded.
When the mean of the yearly mean HbA1c values (mA1C) between year N and year 20 after onset was denoted by mA1C(Nth–20th year), the mA1C for the entire 20 years was indicated by mA1C(1st–20th year) and calculated as real data. If each patient had a full 3 years of duration at entry without HbA1c data during that period, then the mA1C for the remaining observation period (4th–20th year) was indicated by mA1C(4th–20th year); with 6 and 9 years of duration, the mA1Cs for the remaining observation period were indicated by mA1C(7th–20th year) and mA1C(10th–20th year), respectively. We calculated those in simulation by masking the HbA1c data during the first 3, 6, and 9 years after onset from the real observed data of 20 years.
We studied whether real mA1C(1st–20th year) data could predict retinopathy at year 20, and whether the capacity diminished with the length of the period without HbA1c data following onset using mA1C(4th–20th year), mA1C(7th–20th year), and mA1C(10th–20th year) in simulation. Furthermore, we examined the difference of the transitions of the yearly mean HbA1c values for the 20-year period between the year-20 retinopathy-positive and retinopathy-negative groups.
The Wilcoxon rank sum test was performed using JMP version 10.0.0 (SAS, Cary, NC). Two-sided P < 0.05 was considered significant.
RESULTS
The mean age of 15 patients (6 males, 9 females) who fulfilled the criteria was 20.3 years (range 5–28; SD ±7.7) at onset. The mean duration at first visit to the center was 2.9 months (range 0–11; SD ±2.8).
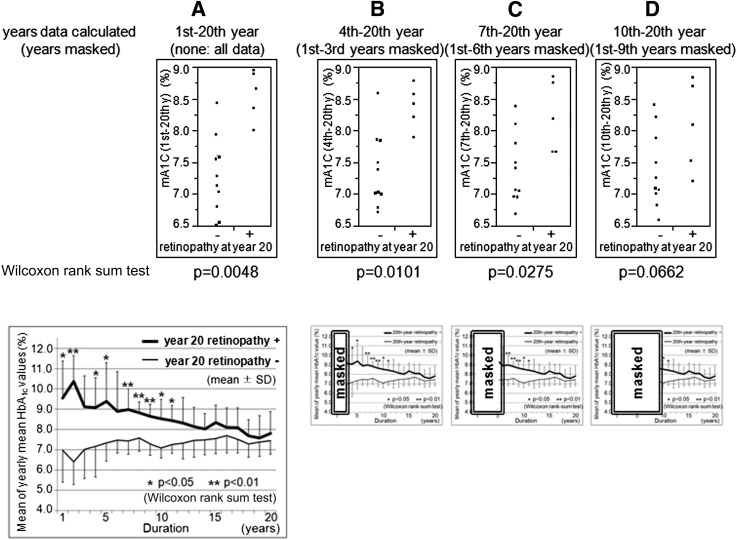
Of these 15 patients, 5 were retinopathy-positive (all showed nonproliferative retinopathy) and 10 were retinopathy-negative at the 20-year follow-up. The values of mA1C(1st–20th year) were well-divided between the two groups (Fig. 1A, top; Wilcoxon rank sum test P = 0.0048). It seemed that mA1C(1st–20th year) substantially predicted retinopathy at year 20 in our patients.
Figure 1.
Differences in the values of HbA1c variables between the retinopathy-positive and retinopathy-negative groups at year 20. A–D: Distributions of the mA1C values by the two groups. Calculated from the total of the real data (A, top) and from the partially masked data in simulation (B–D, top). A (bottom): Difference in the transitions of the yearly mean HbA1c values between the two groups over the course of 20 years. B–D (bottom): Small figures indicate the years masked in simulation. y, year.
In cases of simulated mA1C(4th–20th year), mA1C(7th–20th year), and mA1C(10th–20th year), the differences seemed to lessen gradually between the positive and negative groups at year 20 (Fig. 1B–D, top). There was no significant difference between the two groups in mA1C(10th–20th year), which seemed to have no capacity for predicting year-20 retinopathy (Fig. 1D, top). The longer the period of unknown HbA1c data following onset, the lower the capacity of mA1C to predict 20-year retinopathy seemed to become. This could be explained by the difference of the transitions of the yearly mean HbA1c values between the two groups over the course of 20 years. In the earlier period, these values were higher in the retinopathy-positive group, but they gradually decreased until there was no significant difference between groups (Fig. 1A, bottom).
We obtained nearly complete yearly mean HbA1c values without estimation, except for 2 values out of 300 values in 15 patients for the 20 years. Over the 20 years, we detected no cases of severe anemia. All patients were normotensive (systolic blood pressure <140 mmHg and diastolic blood pressure <90 mmHg) and normolipidemic at their first visit without any drug treatment. At year 20, only one patient was undergoing drug treatment for hypertension or dyslipidemia, or both.
CONCLUSIONS
We demonstrated that mean HbA1c values had a substantial capacity to predict retinopathy at year 20 after onset in our selected younger T1DM patients when we used metabolic memory-free HbA1c data covering the entire duration of diabetes. This suggests that total glycemic exposure in T1DM might have a greater potential for predicting retinopathy than previously reported (2). Furthermore, the longer the period with unknown HbA1c data following onset, the lower the predictive capability of mean HbA1c values for the remaining period seemed to become. This was because of the nonuniform transitions of yearly mean HbA1c values between the year-20 retinopathy-positive and retinopathy-negative groups.
If one began to observe patients who already had long durations of diabetes at a given study entry, the previous unknown higher HbA1c values might cause underestimation of the total glycemic exposure in the retinopathy-positive group, thus providing a less accurate picture of the relationship between glycemic exposure and retinopathy (2). The use of only partial, not whole, post-midcourse HbA1c data of patients with long durations of diabetes might distort evaluation of the true influence of glycemia on diabetes complications.
Because of our low number of subjects, further investigation is needed to confirm the results. However, we scrupulously selected younger T1DM patients with continuous HbA1c data for the entire duration of their diabetes after clear onsets. We also tried to maximize the relative uniformity of conditions in evaluating glycemia and retinopathy among patients, because that was critical for this study. HbA1c values measured by six different instruments might be another limitation, although we used values measured only in our institution with careful calibration between instruments. Retinopathy evaluation by ophthalmoscopy, not photography, could be another limiting factor. Because evaluation was performed only by ophthalmologists in our center in the same manner, a relatively uniform level of accuracy in detection could be expected for all patients, including the retinopathy-positive and retinopathy-negative patients at year 20. Also, the substantially contemporaneous follow-up periods (first visits within a short span of 3 years) used may improve the uniformity of the evaluations of glycemia and retinopathy.
This study could help to promote more accurate investigation of the relationship between hyperglycemia and retinopathy in T1DM, and it demonstrates the importance of using HbA1c data from the total, not partial, diabetes duration to exclude the metabolic memory effect.
Acknowledgments
A.H. designed the study, researched the data, and wrote the manuscript. D.F. contributed to the discussion. N.Y. contributed to the discussion and reviewed the manuscript. S.K. reviewed the manuscript. Y.U. reviewed and edited the manuscript. A.H. and Y.U. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
No potential conflicts of interest relevant to this article were reported.
The authors thank all the patients and colleagues who participated in this study. The authors appreciate Dr. Alan Rosen for his earnest and patient support in English expression, and Dr. Omi Terasaki for his contribution to the discussion.
References
- 1.White NH, Sun W, Cleary PA, et al. Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group Prolonged effect of intensive therapy on the risk of retinopathy complications in patients with type 1 diabetes mellitus: 10 years after the Diabetes Control and Complications Trial. Arch Ophthalmol 2008;126:1707–1715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The Diabetes Control and Complications Trial Research Group The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the diabetes control and complications trial. Diabetes 1995;44:968–983 [PubMed] [Google Scholar]