Abstract
Iodine deficiency disorders (IDD) constitute the single largest cause of preventable brain damage worldwide. Majority of consequences of IDD are invisible and irreversible but at the same time these are preventable. In India, the entire population is prone to IDD due to deficiency of iodine in the soil of the subcontinent and consequently the food derived from it. To combat the risk of IDD, salt is fortified with iodine. However, an estimated 350 million people do not consume adequately iodized salt and, therefore, are at risk for IDD. Of the 325 districts surveyed in India so far, 263 are IDD-endemic. The current household level iodized salt coverage in India is 91 per cent with 71 per cent households consuming adequately iodized salt. The IDD control goal in India was to reduce the prevalence of IDD below 10 per cent in the entire country by 2012. What is required is a “mission approach” with greater coordination amongst all stakeholders of IDD control efforts in India. Mainstreaming of IDD control in policy making, devising State specific action plans to control IDD, strict implementation of Food Safety and Standards (FSS) Act, 2006, addressing inequities in iodized salt coverage (rural-urban, socio-economic), providing iodized salt in Public Distribution System, strengthening monitoring and evaluation of IDD programme and ensuring sustainability of IDD control activities are essential to achieve sustainable elimination of IDD in India.
Keywords: India, iodine deficiency disorders, iodized salt, National Iodine Deficiency Disorders Control Programme, sustainable elimination
Introduction
Food and nutrition security at the individual and population levels is a fundamental right. Nutrition security ensures optimal actualization of human resources and overall progress and development of a society and nation. Malnutrition (both under- and overnutrition) is currently one of the biggest challenges being faced by the modern world. Micronutrient deficiencies, more commonly referred to as “hidden hunger”, form a significant component of burden of malnutrition worldwide, more so in developing countries like India. Deficiencies of iodine, iron, folic acid, vitamin A and zinc are the leading five causes of micronutrient deficiencies which constitute a global public health problem1.
Iodine deficiency disorders (IDD) are linked to iodine deficient soil. Due to glaciations, flooding, rivers changing course and deforestation the iodine present in top soil is constantly leached. This in turn leads to deficiency of iodine in crops grown on iodine deficient soil with consequently low iodine in the diet for livestock and humans. In the past, iodine deficiency was thought to cause only goitre and cretinism. However, over the last quarter of the century, it has become increasingly clear that iodine deficiency leads to a much wider spectrum of disorders commencing with the intrauterine life and extending through childhood into adult life with serious health and social problems. The spectrum of diseases includes goitre, cretinism, hypothyroidism, brain damage, abortion, still birth, mental retardation, psychomotor defects and hearing and speech impairment2. Majority of consequences of IDD are invisible and irreversible but at the same time preventable.
IDD constitute the single largest cause of preventable brain damage worldwide leading to learning disabilities and psychomotor impairment3. Children living in iodine-deficient areas on an average have lower intelligence quotient (IQ), by as much as 13.5 IQ points as compared to children living in iodine-sufficient areas4. IDD have been shown to be associated with at least six of the eight Millennium Development Goals5. IDD are a major challenge to the health of populations the world over particularly among preschool children and pregnant women in low-income countries. Globally two billion people are at risk of iodine deficiency disorders due to insufficient iodine intake6. Nearly 266 million school-aged children worldwide have insufficient iodine intake. Of the 130 countries which reported data for IDD in 2006 (comprising 91.1% of the total global population), IDD was a public health problem in 47 countries6.
The 43rd World Health Assembly held at Geneva, in May 1990 recognized IDD elimination as a major priority7. It adopted Universal Salt Iodization (USI) as the preferred strategy to achieve the goal of IDD elimination by 2000. The United Nations World Summit for Children, 1990 attended by 71 Heads of State and other senior officials of 15 Member States, adopted a plan of action for elimination of IDD by the year 20008. In 2002, in the United Nations General Assembly Special Session (UNGASS) on children, a new goal was adopted for IDD elimination by 20059. Impressive gains have been made in household-level coverage of adequately iodized salt (more than 15 part per million of iodine content) globally. Currently 145 countries worldwide have implemented USI and over 71 per cent of the population worldwide consumes adequately iodized salt10.
Globally, India has the largest number of children born vulnerable to iodine-deficiency11. India, as one of the participants of the UNGASS on children had committed to the goal of IDD elimination by 2005. However, India subsequently revised the IDD control goal in 2006. The IDD control goal in India was to reduce the prevalence of IDD (i.e. total goitre rate) below 10 per cent in the entire country by 201212. This article reviews the efforts done to control IDD in India with a brief outline of the historical evolution of the IDD control programme in India. We look critically at the strengths, weaknesses, opportunities and the threats facing the IDD control activities in India.
Current burden of IDD in India
Surveys conducted by the Central and State Health Directorates, Indian Council of Medical Research (ICMR) and medical institutes since 1950s have clearly demonstrated that IDD is a public health problem in all States and union territories in India. Of the 325 districts surveyed in India so far, 263 districts are IDD-endemic, i.e. the prevalence of IDD is above 10 per cent in the population13. As per the survey conducted by the National Nutrition Monitoring Board (NNMB) in 2000-2001 in rural areas of Kerala, Tamil Nadu, Karnataka, Andhra Pradesh, Maharashtra, Madhya Pradesh, Orissa and West Bengal, the overall prevalence of total goitre rate (TGR) among six to twelve year old children was about 4 per cent14. The prevalence of goitre was highest in Maharashtra (11.9%) and West Bengal (9%).
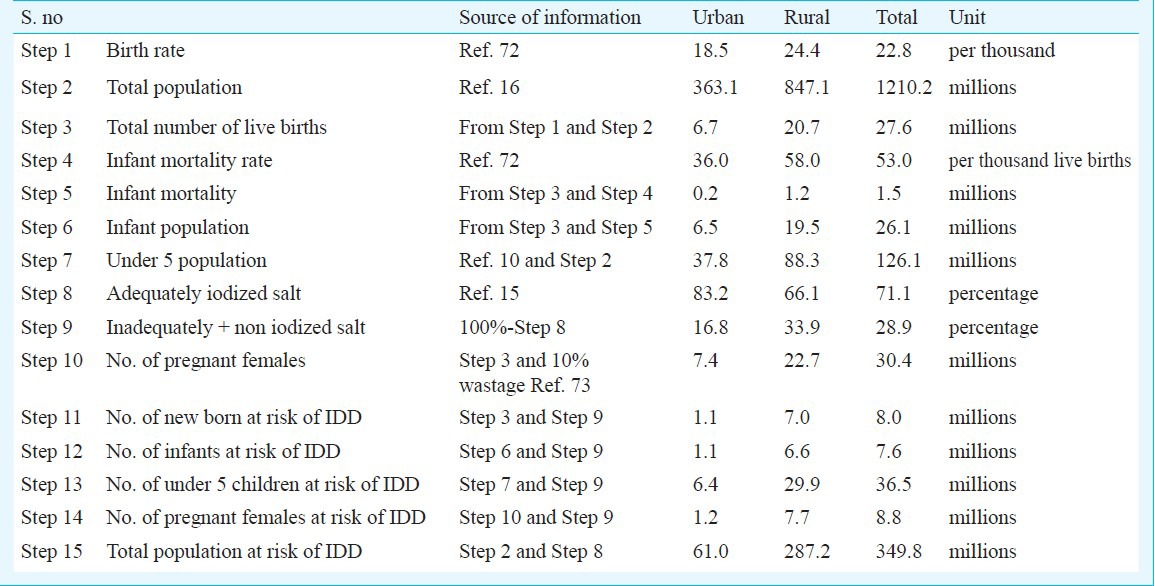
In India the entire population is prone to IDD due to deficiency of iodine in the soil of the subcontinent and consequently the food derived from it. Of these, an estimated 350 million people are at risk of IDD as they consume salt with inadequate iodine (Table I). Every year nine million pregnant women and eight million newborns are at risk of IDD in India. These estimates are based on the household-level coverage of adequately iodized salt as reported in Coverage Evaluation Survey (CES) 2009 and extrapolated to total population estimates from Census 2011 (provisional figures)15,16.
Table I.
Estimated burden of Indian population at risk of IDD
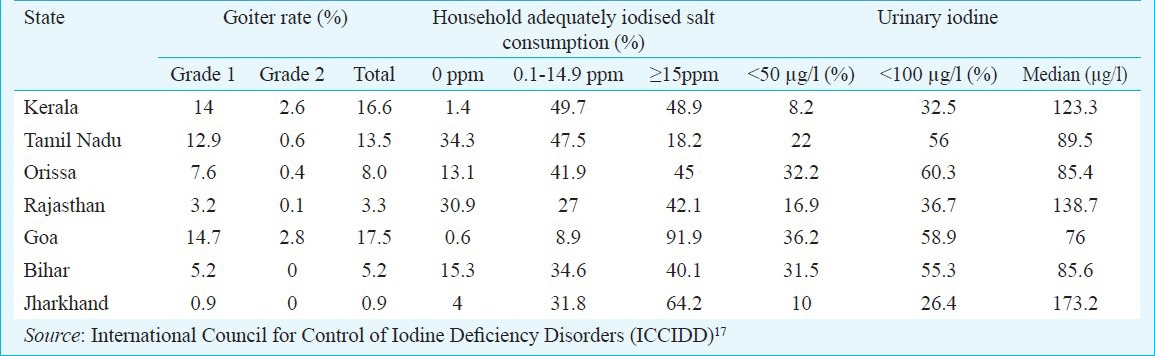
State level IDD surveys were carried out in seven States (Kerala, Tamil Nadu, Orissa, Rajasthan, Bihar, Goa and Jharkhand) from 2000 to 2006 by International Council for Control of Iodine Deficiency Disorders (ICCIDD) in collaboration with State medical colleges, Micronutrient Initiative (MI) and UNICEF17. The surveys were carried as per the recommended guidelines of WHO/UNICEF/ICCIDD and used 30 cluster into 40 children sampling methodology3. Children in the age group of 6-12 yr, women in the household, retail shop keepers and other community stakeholders constituted the study population. All three indicators, viz. total goiter rate (TGR), urinary iodine (UI) concentration and iodine content of salt (household and retail shop) were studied. The household level consumption of adequately iodized salt (≥15 ppm) ranged from 18.2 per cent in Tamil Nadu to 91.9 per cent in Goa (Table II). The median urinary iodine excretion ranged from 76 μg/l in Goa to 173.2 μg/l in Jharkhand. TGR ranged from 0.9 per cent in Jharkhand to 17.5 per cent in Goa. These State level IDD surveys are the only sub-national level IDD surveys in India where all three indicators, viz. iodized salt coverage, urinary iodine and TGR were assessed concurrently.
Table II.
Iodine deficiency disorders (IDD) status of seven States surveyed (2000-2006)
Iodised salt coverage at household level
In India as per the Coverage Evaluation Survey 200915, 91 per cent of households had access to iodized salt, of whom 71 per cent consumed adequately iodized salt. Another 9 per cent consumed salt with no iodine. There are wide rural and urban variations in household coverage of adequately iodized salt (83.2% in urban areas vs. 66.1% in rural areas). Wide variation was also seen across different States/UTs; with Chhattisgarh (31.6%), Karnataka (35.5%) and Jharkhand (41.4%) being the low coverage States and Manipur (98.3%), Meghalaya (98%) and Nagaland (97.1%) being high coverage States.
Historical evolution of the iodine deficiency control programmes in India
Iodine deficiency and its manifestations have been known to mankind from ancient times. IDD was first documented in India in the Himalayan region by McCarrison in 190818. Further studies documenting goitre in India were done by several other researchers including Stott et al (1931)19, and Ramalingaswami (1953)20.
Salt-iodization as an intervention to address goiter, the then well recognized and more visible manifestation of iodine deficiency was first initiated in United States of America (USA) and Switzerland in 1920s21. India was one of the first countries in the world to start a public health programme to address iodine deficiency disorders based on salt iodization. A landmark study in Kangra Valley region, Himachal Pradesh was conducted by Ramalingaswami and his team from 1956 to 197222. This community based intervention study clearly demonstrated the effectiveness of iodized salt in reducing goitre prevalence in Kangra Valley. The study area was divided into three geographically distinct zones, Zone A, Zone B and Zone C. Salt was fortified with either potassium iodate (Zone A) or potassium iodide (Zone C), to deliver 200 micrograms of iodine to each study participants. Zone B was the control area and received non-iodized salt. A progressive and significant decline in prevalence of goiter was observed in Zone A and Zone C populations by 1962. (Fig. 1) Additionally, the pattern of iodine metabolism in this population returned to within normal limits in contrast to the “control” population that did not consume iodized salt. From 1962 onwards, iodized salt was provided to Zone B, the control population also. Subsequent checks in 1968 and 1972 demonstrated a decline in goiter-prevalence in this population as well, which was directly attributable to the introduction of iodized salt in the diet. The results of this study have been supported by evidence from other international community-based intervention programmes as well23,24. These studies from United States and Switzerland clearly showed a causal link between daily consumption of iodized-salt and reduction in prevalence of goiter.
Fig. 1.
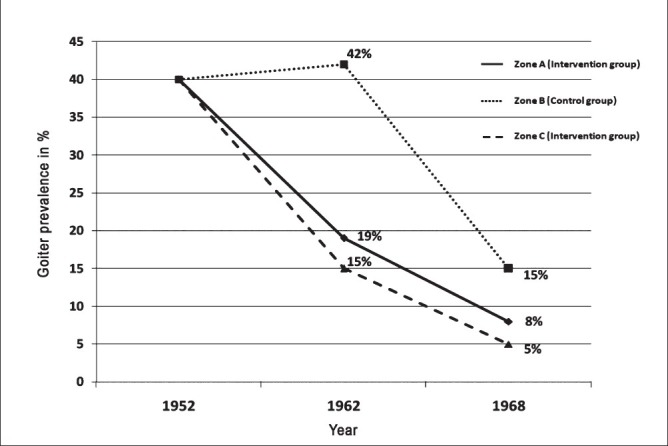
Decrease in goitre prevalence after salt iodization in the Kangra Valley study (1956-72)22. Prevalence of goiter in 1952 was 40 per cent in all the three zones. In zone B (Control group), intervention (iodized salt) was done in 1962.
Based on the success of the Kangra Valley study22, the Government of India established the National Goitre Control Programme (NGCP) in 1962 at the end of the second Five-Year Plan25. The objectives of NGCP were to identify the goiter-endemic regions of the country and supplement the intake of iodine to the entire population in these regions. The NGCP primarily focused on the so called “goitre belt” in the country which comprised the Himalayan and Tarai region in north and north-eastern parts of India.
Subsequently, new evidence emerged that IDD was not limited to a few endemic foci in India and was reported from nearly every geographical region of the country26,27,28. Based on the evidence from district IDD surveys carried out as per the guidelines of NGCP, situation analysis conducted by the Nutrition Foundation of India (NFI) and studies carried out by the Indian Council of Medical Research (ICMR) and the All India Institute of Medical Sciences (AIIMS), New Delhi team, it was decided to expand the activities of NGCP29. In 1983 in the Annual Meeting of Central Council of Health, it was decided that all edible salt in India would be iodized by 199230. The process of iodization salt was started in a phased manner in the country from April, 1986. Iodized salt was brought under the revised Prevention of Food Adulteration (PFA) Act of 198831.
There was a growing realization that iodine deficiency is not limited to goiter alone but could mani-fest in several other ways with far serious consequences. Available scientific evidence both from across the world and from India showed significant impact of iodine deficiency on early brain development, cognition and learning abilities of children4,32,33,34. According to a study by Kochupillai et al27, the incidence of neonatal hypothyroidism in one of the IDD endemic regions of India was one of the highest reported in the world. The incidence of neonatal hypothyroidism varied from 0.1 per cent in an iodine sufficient region of India to 13.3 per cent in iodine-deficient region. In populations with high incidence of neonatal hypothyroidism, increased nerve deafness and low IQ were observed27. These effects of mild brain damage suggested that nutritional iodine deficiency could manifest in ways other than goiter or cretinism.
The World Summit for Children in 1990 endorsed the concept of “IDD as a spectrum of diseases” and set up a target of global elimination IDD by year 2000. India was one of the participants and signatories of this declaration. The Government of India reiterated its commitment to achieve USI by 1995 at the second South Asian Association for Regional Cooperation (SAARC) conference on children in South Asia, held in Colombo, Sri Lanka, in September 199235. Following the SAARC conference, the Government of India introduced an amendment in the National Plan of Action for Children to include universal access to iodized salt by 1995 as a specific goal36.
The nomenclature of the NGCP was changed to National IDD Control Programme (NIDDCP) in 1992 to emphasize the wider implications of iodine deficiency. The identified objectives of the NIDDC programme were to conduct surveys to assess the magnitude of the IDD, supply of iodated salt in place of common salt, resurvey after every five years to assess the extent of IDD and the impact of iodated salt, laboratory monitoring of iodized salt and urinary iodine excretion and health education and advocacy37. The NIDDCP identifies USI as the primary strategy to eliminate IDD as a public health problem in the country.
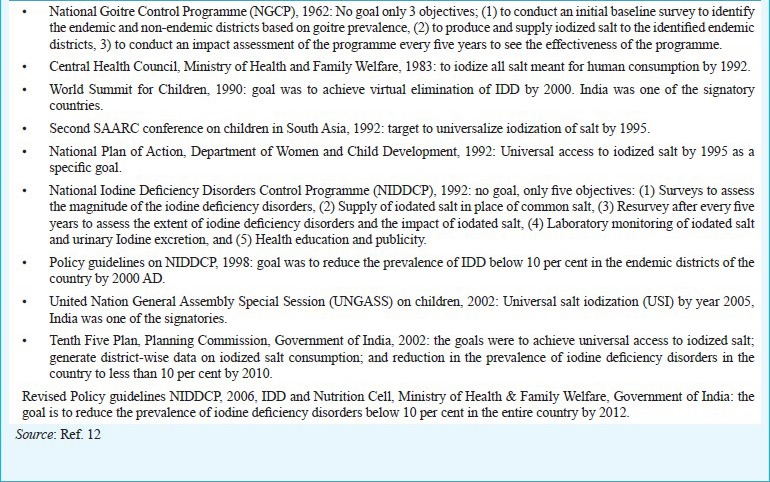
In 1998 after consultation with all stakeholders policy guidelines for NIDDCP were formulated37. The policy guidelines were revised in 2006 and clearly delineated the administrative structure, IDD survey guidelines and financial outlay of the programme12. Concomitant with the evolution of the IDD control programme in India, the IDD control goals also went through various stages of revision and reformulation (Box 1).
Box 1.
Case study of Rajiv Gandhi Mission for Elimination of Iodine Deficiency Disorders, Madhya Pradesh, 1994 to 1996
Progress of IDD control programme in India: A success story
IDD control programme in India is a public health success story. We have come a long way from a district-centric approach of NGCP in 1962 to having a national-level programme today covering the whole country. Nearly 91 per cent of households in the country have access to iodized salt with 71 per cent consuming adequately iodized salt15. Iodized salt production in India was less than two hundred thousand metric tons (MT) per year in 1980s, of which 50 per cent was exported to Nepal. Currently, the total iodized salt production is 5.82 million MT per year, well in excess of the national requirement of 5.2 million MT per year38.
The key factors contributing to this remarkable progress of the IDD control programme in India are effective translation from research to policy, political commitment, involvement of the private sector in production of iodized salt, legislation to ensure iodization of salt and catalytic role played by the troika of academic institutes, civil society and international agencies.
Translation from research to policy: The dynamic evolution of NIDDCP in India demonstrates the successful translation of research to policy to programme. The land mark Kangra Valley study22 (research) was the genesis of IDD control “policy” and subsequent evolution of NGCP (programme) and its implementation39. The researchers used the results of the study effectively to reach a consensus and formulate a policy to combat IDD in India. Further studies carried out in tarai region of India and from other regions led to evolution of NIDDCP from NGCP.
Sustained political commitment: After initial efforts to reach consensus on IDD control, the need to upscale and mainstream the IDD control efforts was felt. Concerted efforts, focusing on both “formal” (Indian Council of Medical Research, Directorate General of Health Services, Health Council, Ministry of Health and Family Welfare, etc.) and “informal” (political leaders, civil society groups, etc.) institutional structure for decision making were adopted. The resultant sustained political commitment to the IDD control policy was borne out by the inclusion of IDD control in the 20-Point Programme of the Government of India in 198340. The commitment of the Government of India (GoI) and senior political leadership to the goal of IDD control was reaffirmed by active participation by India in the World Summit on children in 1990, SAARC Children Summit in 1992 and UNGASS on children, 20028,9,35.
Increased production of iodized salt and involvement of the private sector: The Indian salt industry has made rapid progress over the last three decades with increase in both quantity and quality of iodized salt produced in the country. This increase in iodized salt production is primarily due to the contribution of the private sector. Currently 98 per cent of total iodized salt production in India is from the private sector38. This is a classic example of responsive and responsible participation by the private sector in a major national public health programme.
Institution of legislation to ensure iodization of salt: After sustained advocacy, GoI notified a ban on sale of non-iodized edible salt in 1997 under the Prevention of Food Adulteration Act 195441. The imposition of ban gave a huge impetus to the promotion of adequately iodized salt in the country. However, under pressure from certain segments the ban was withdrawn in 200042. The withdrawal of the ban had adverse effects on household-level coverage of adequately iodized salt. This underscored the need to have a mandatory legislation to ensure USI in India, and the ban was reinstated in 200543.
Catalytic role played by the troika of academic institutes, civil society and international agencies: Government of India and its nodal ministries - Ministry of Health and Family Welfare and Ministry of Industry undoubtedly have the central and primary role in implementation of NIDDCP and USI in India. All India Institute of Medical Sciences, New Delhi, has provided leadership for research policy and advocacy towards IDD control and USI programme in the country. Civil society and international agencies such as Global Alliance for Improved Nutrition (GAIN), International Council for Control of Iodine Deficiency Disorders (ICCIDD), Micronutrient Initiative (MI), UNICEF, World Food Programme (WFP) and WHO have not only acted as important partners for IDD control initiatives in the country, but also as vocal advocates for reinstatement of the ban on the scale of non-iodized salt.
Have we achieved the IDD control goal?
The goal of IDD control programme in India was to reduce the prevalence of IDD (i.e. TGR) below 10 per cent in the country by 2012. The recent Coverage Evaluation Survey (CES) 2009 has reported 91 per cent population coverage of iodized salt in India, of which 71 per cent population is consuming adequately iodized salt and another 20 per cent is consuming salt with some added iodine (<15 ppm)15. The USI target of greater than 90 per cent household coverage of adequately iodized salt is within our reach. The CES results show an increase of nearly 20 per cent from the last national-level iodized salt coverage survey carried out in 2005-2006 (Fig. 2)44.
Fig. 2.
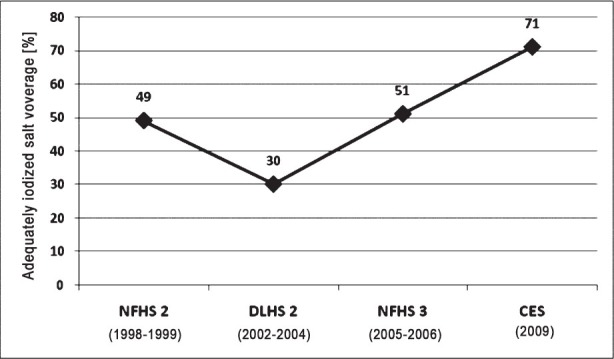
Progress in household level adequately iodized salt coverage in India using salt testing kits (STKs). CES, Coverage Evaluation Surgery 200915; NFHS2, National Family Health Survey50; DLHS2, District Level Household Survey51; NFHS3, National Family Health Survey 249.
There has been remarkable progress in terms of the capacity to produce iodized salt in India. The country currently produces 5.8 million tons of iodized salt (2009-2010) against a total requirement of 5.2 million tons. But due to multitude of factors this increased production of iodized salt has not translated into USI at household level. The major factors for not being able to achieve USI in India are low priority accorded to the NIDDCP programme, meager fund allocation for the programme, lack of communication campaign for sustained and effective behaviour change, lack of monitoring of iodine level of salt from production to consumer end, no mechanism of monitoring iodine content of salt transported by road (leading to easy availability of non-iodized salt in areas where salt is primarily transported by road) and poor implementation of Prevention of Food Adulteration (PFA) Act45,46. Salt iodization especially by small scale producers who contribute to approximately 66 per cent of total iodized salt production in the country is not of optimal quality. There are considerable variations in the levels of iodization, high moisture content of salt and use of improper packaging material leading to sub optimal iodine content of salt at consumer level46. Consumer awareness regarding salt iodization is also inadequate in India. A study done in rural households of eight low-iodized salt coverage (less than national average) States in India, reported that only 58.7 per cent households were aware of iodized salt and only 35.4 per cent respondents knew that iodine deficiency causes “less mental development and diminished intelligence”47. This poor awareness and knowledge of iodized salt and IDD leads to inadequate demand for adequately iodized salt.
As per the criterion of WHO/UNICEF/ICCIDD for tracking progress towards sustainable elimination of IDD we still have a long way to go (Table III). Of the 10 programme indicators listed by WHO/UNICEF/ICCIDD3, India has attained only five, with another four being partially attained (Table IV).
Table III.
Current status of progress towards sustainable elimination of IDD in India
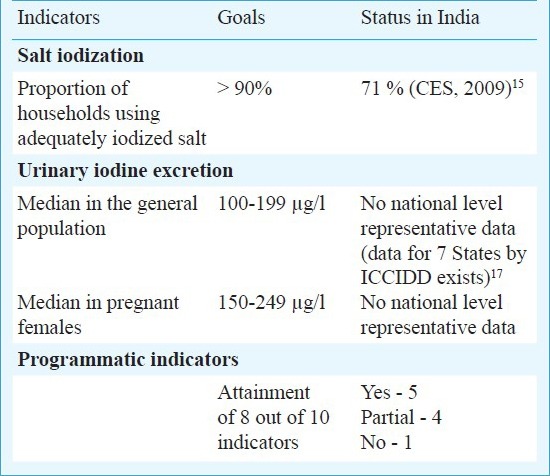
Table IV.
Current status of ten Programme indicators for tracking progress towards sustainable elimination of IDD in India
There is a paucity of representative national-level good quality data for monitoring IDD control activities in India. The national IDD cell/ICMR district-level IDD surveys carried out as part of NIDDCP only report TGR. Even these goitre surveys with different reference periods for different district surveys are carried out infrequently and irregularly making them useless for monitoring State and national level IDD activities. The results available from various State level or district level IDD surveys carried out as a part of research by various academic institutes and international agencies are too sparse and sporadic to be of any use for monitoring programmes.
The current IDD survey guidelines detailed in Revised Policy Guideline on NIDDCP3,12 do not conform to standard guidelines laid down by WHO/UNICEF/ICCIDD for monitoring of IDD control programmes12. The cut-off of TGR used to define a region as IDD endemic is 5 per cent as per the WHO/UNICEF/ICCIDD3 whereas it is 10 per cent as per the revised policy guidelines of NIDDCP12. As per the revised policy guidelines, district level surveys are to be conducted in every district once every five years by rotation in the State using three indicators, viz. TGR, urinary iodine excretion and household level adequately iodized salt consumption. The target population recommended is school aged (6 to 12 yr) children only. It does not include pregnant women as recommended by the standard guidelines of WHO/UNICEF/ICCIDD3. The recommended sample size to be selected using cluster sampling method (30 clusters into 90 children) of 2700 for TGR, 540 for iodized salt and 270 for urinary iodine per district is also not as per the standard guidelines. The current revised policy guidelines lack any epidemiological rationale both in terms of sampling method and sample size. WHO/UNICEF/ICCIDD3 guidelines include urinary iodine in pregnant women and do not include TGR as an indicator. The recommended sample size as per WHO/UNICEF/ICCIDD guidelines is 1200 school aged children and 300 pregnant women for IDD survey. The current allocation of  50,000 to conduct a district level survey is grossly inadequate when one has to collect information of all there indicators viz. TGR, UIE and iodized salt coverage12. District level IDD data cannot be aggregated to obtain State or national IDD estimates as district level surveys are done over different time span. Thus, there is a need to revise the NIDDCP policy guidelines, and bring these in conformation with internationally acceptable IDD control guidelines.
50,000 to conduct a district level survey is grossly inadequate when one has to collect information of all there indicators viz. TGR, UIE and iodized salt coverage12. District level IDD data cannot be aggregated to obtain State or national IDD estimates as district level surveys are done over different time span. Thus, there is a need to revise the NIDDCP policy guidelines, and bring these in conformation with internationally acceptable IDD control guidelines.
The only available indicator in India that can be utilized for monitoring IDD control programme at the State and national level is household level coverage of adequately iodized salt. The most up-to-date and valid source of adequately iodized salt coverage in India is the Coverage Evaluation Survey (CES) 200915. However, CES 2009 used salt testing kits (STKs) to estimate iodine content of salt instead of the recommended gold standard method of iodometric titration. There are methodological issues with using salt testing kits for estimating population level iodized salt coverage because of the low specificity and hence low validity of the method48. But even with these shortcomings, iodized salt coverage (using STKs) is the only useful national level indicator available to track progress towards sustainable elimination of IDD in India. Thus, in spite of the limitations of STKs, the comparison over the years provides useful information on trends in coverage level46,49,50,51.
The way forward
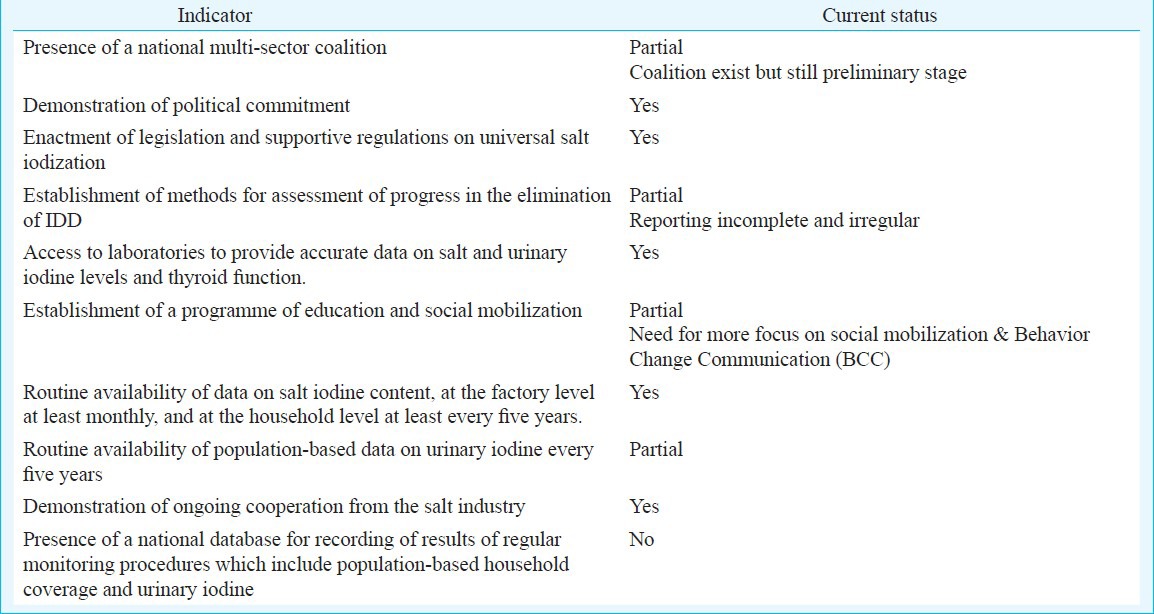
Achieving IDD control goal in India requires a “mission approach” with greater coordination amongst all stakeholders of IDD control. The “mission approach” has to be adopted by the government at the highest political level, and should have clearly defined objectives and strategies. The plan of action has to be executed within a defined time-frame by a committed team. Fast-track procedures and collective action by an inter-sectoral effort are integral components of this approach. Close monitoring and transparent evaluation should be developed in line with the goal, objectives and strategies of the “mission approach”. The potential of “mission approach” in making significant progress towards USI and IDD control has been demonstrated by the successful case study of Madhya Pradesh in India from 1994 to 1995 (Box 2)52. However, it is imperative that “mission approach” is designed concurrent to a “system approach” as sustaining the success achieved during “mission approach” is equally important.
Box 2.
Evolution of goals of IDD control program in India
In 2006, a National Coalition for Sustained Iodine Intake (NCSII) was established53. The National Coalition comprises a wide array of stakeholders involved in iodine deficiency elimination activities in the country. These included Government of India agencies (Ministry of Health and Family Welfare and Salt Commissioners Office), State Government agencies (Ministry of Health and Family Welfare at State level), national institutes/organizations National Institute of Health and Family Welfare (NIHFW), National Cadet Corps (NCC), partner agencies (WHO, UNICEF, WFP, GAIN, MI, ICCIDD), health professionals groups Indian Public Health Association (IPHA), Indian Association of Preventive and Social Medicine (IAPSM), Indian Thyroid Society (ITS), Indian Society of Pediatric and Adolescent (ISPAE), salt manufacturers associations (ISMA), civil society/ consumer advocacy groups and media advocacy groups. The Coalition provides a platform bringing together all partner agencies, government agencies and departments. The Coalition has ensured greater coordination, synergy and experience sharing amongst different stakeholders engaged in IDD control activities in India. There is a need to further strengthen the National Coalition and to establish State level Coalitions on similar lines.
Mainstreaming of IDD control in the policy-making process is imperative. All stakeholders should sensitize policy makers to the criticality of IDD control for human resource development and national progress. It is to be emphasized that even moderate iodine deficiency is associated with cognitive impairment in children54. More focus should also be given to the “rights approach” i.e. it is every child's right to have access to optimal iodine nutrition to ensure optimal brain development.
Health being a State subject as per the constitution of India, it is imperative that due focus be given to State level IDD control activities55. The translation from programme to activities in NIDDCP like all other health programmes occurs at the State level. Currently wide variations in IDD status across different States are observed, making it even more important that we devise State specific action plans to control IDD. State level coalition and alliances of stakeholders would go a long way in taking forward the agenda of IDD in India. There is a need for capacity-building of work force required for IDD control activities in States, institutionalization of IDD research and advocacy in academic institutes at State level.
The time has come for USI in India shifts its focus from “quantity” to “quality”. There is a need to set up a stringent laboratory quality assurance programme from the production end laboratories to the consumer level monitoring laboratories. Capacity-building of private salt manufacturer/refineries and state/district level salt iodization monitoring laboratory personnel is a critical component of ensuring good quality iodized salt.
Despite legislation requiring mandatory salt iodization in India, the primary approach especially with small scale salt producers has been advocacy based i.e. sensitizing, persuading these manufacturers to iodize the salt produced by them for large good of society. The “stick” strategy, i.e. implementation of Prevention of Food Adulteration Act, 1954, and punishing the violators of mandatory salt iodization provision has been only sparingly used. Now the time has come for “zero tolerance” and strict implementation of Food Safety and Standards (FSS) Act, 2006/Prevention of Food Adulteration (PFA) Act, 195431,56. The choice is between 2000 salt producers who must produce quality and adequately iodized salt and millions of newly born children at risk of IDD.
There still exist wide inequities in iodized salt coverage, across States, across the rural-urban divide, across socio-economic strata and amongst marginalized populations57. Pregnant women and newborn children, the most vulnerable to IDD, are still not provided with optimal iodine nutrition58. We have to evolve a mechanism to reach these population sub-groups. Targeted interventions, innovative approaches and concerted efforts are required to ensure that each and every child born in this country is protected from brain damage caused due to inadequate iodine intake.
Pregnant women have increased requirement of iodine and thus it is imperative to monitor their IDD status to ensure optimal brain development of the foetus59. A review of available studies from India shows a significant iodine deficiency in pregnant women58. The recommended iodine intake during pregnancy was increased from 200 to 250 μg/day and median UI concentration cut-off was increased from 100 to 150 μg/l3. This upward revision means that the current level of iodine supplementation in salt (at 15 parts per million level of iodine, daily average salt consumption of 10 g will provide only 150 μg/day of iodine) may not be sufficient to meet the increased requirement during pregnancy. It is imperative that UI monitoring of pregnant women is included as a vital component of NIDDCP in India. There is a need to conduct national level representative surveys to better quantify the iodine nutrition of pregnant women in India. Another important research agenda should be conducting intervention trial for iodine supplementation in pregnant women.
Public Distribution System (PDS) provides an excellent opportunity to reach the unreachable. The key hurdle in achieving USI is ensuring access to quality iodized salt especially for the socio-economically poor strata of the population. This can be overcome by introducing quality iodized salt through PDS. Utilized primarily by the populations below poverty line, providing low-cost quality adequately iodized salt through PDS will ensure that we cover the last one fourth of population which still has limited access to adequately iodized salt. PDS along with Integrated Child Development Services (ICDS) scheme and Mid-day meal (MDM) programme together have huge potential as far as ensuring universal and optimal iodine nutrition to the population is concerned.
Strengthening of National and State IDD cells which are the back bone of the NIDDCP is critical to achieving IDD control goals in India. Increased resources especially financial, infrastructure strengthening and capacity building of human resources of national and State IDD cell should be done at the earliest.
Increasing consumer awareness and demand for adequately iodized salt has been proven to be one of the most effective interventions to promote USI globally. The Behaviour Change Communication (BCC) activities need to be upscaled and intensified. Along with activities targeted towards increasing awareness of consumers, the community needs to be enabled to monitor the quality of iodized salt. Salt testing kits (STKs) are an effective community advocacy tool and if linked to a quality assured laboratory network (with capacity of iodometric titration) can be a highly effective community monitoring mechanism to ensure USI.
Tracking progress of sustainable elimination of IDD at national and State level using defined criteria should be incorporated into the NIDDCP at the earliest3. Monitoring and evaluation is the weakest and most crucial link of IDD control activities in India. There is a need to adopt achievable goals with appropriate resource allocation so that the indicators linked to these goals are measured regularly. State IDD surveys should be carried out regularly every three/five years as per the guidelines.
Sustaining the progress made towards IDD control so far should be the focal point henceforth. Elimination of IDD from a population should always be coupled with a mechanism to ensure the sustainability of the programme. As has been borne out by numerous case studies across the globe, one time elimination of IDD is not the answer60,61. Also, in India slackening of efforts has resulted in re-emergence of IDD as seen in case of Madhya Pradesh62. The task of sustaining iodine deficiency elimination requires constant vigilance. One of the models proposed for sustaining IDD elimination efforts is the Social Process Model (Fig. 3)63. The social process model for health care programmes may be represented by a six-element circular model; (i) assess/reassess the situation epidemiologically, (ii) increase awareness of the situation through communication and dissemination of findings, (iii) develop and achieve political resolve and agreement at all levels (from national to community level), (iv) create and update plans for infrastructure development and plan of action, (v) vigorously implement the programme, and (vi) assess/reassess the programme progress (viz. monitoring and evaluation) to track progress towards sustainable elimination of IDD. Closely linked to the issue of sustaining the progress is the debate surrounding the need for USI, its ethics and allegations regarding promoting monopoly of multinational corporations (MNCs). IDD is a public health problem and thus requires public health intervention. Ensuring equity in iodine nutrition is critical to this approach.
Fig. 3.
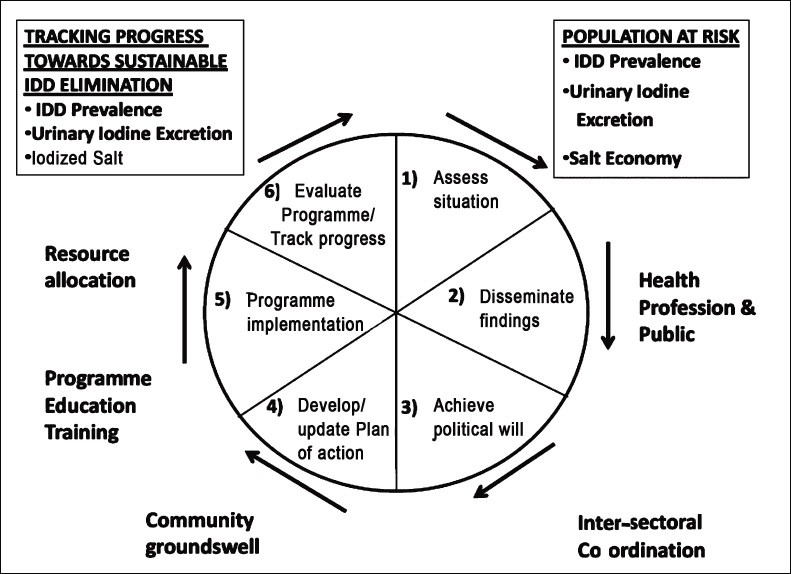
Social process model for a national IDD control programme.
Source: Ref. 74.
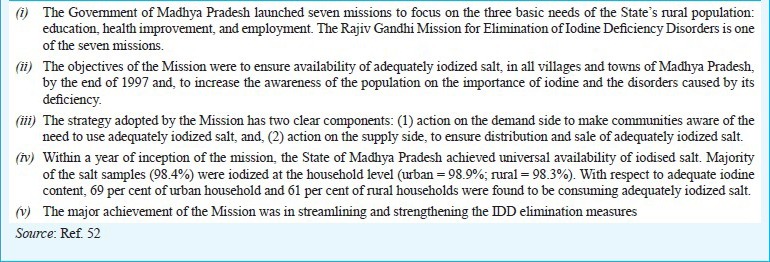
Neonatal hypothyroidism screening programmes to screen and treat newborns with hypothyroidism (including that caused by iodine deficiency), which are adopted by developed countries globally are based on the principle of early detection and treatment. However, due to the high costs involved and other operational difficulties such as low institutional deliveries, this is not suited for developing countries like India. (Fig. 4). Salt iodization has to be universal to reach the most marginalized and individuals at risk. It is extremely difficult and costly to assess iodine deficiency at the individual level. Targeted salt iodization is also administratively not feasible. Thus, health promotion along with USI is ideal strategy to combat IDD in India.
Fig. 4.
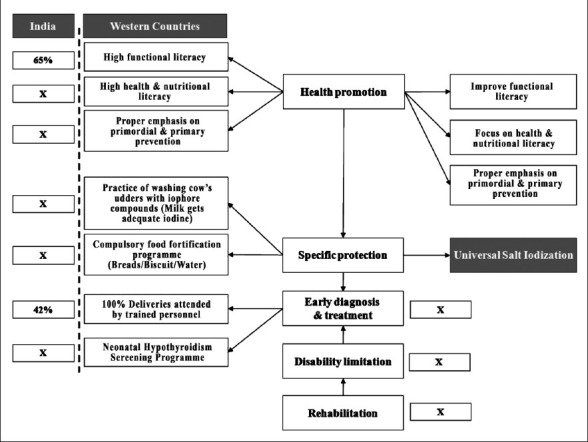
Schematic representation of availability of key components essential for implementation of Neonatal Hypothyroidism Screening Program in India and its comparison with western countries. (“x” denotes absence of the key component).
Source: Ref. 45.
The recommended salt iodine fortification level of 15 ppm provides 150 μg of iodine per day assuming daily salt consumption of 10 g. Iodine fortification at this level meets the recommended daily requirements (RDA) and is also well within the upper safety limit of 1000 μg recommended by WHO3. Iodine intake has been postulated to be an important determinant of the pattern of thyroid diseases, broadly related to three distinct subsets of thyroid disorders; iodine induced hyperthyroidism (IIH) (thyrotoxicosis), autoimmune thyroiditis (AIT), and thyroid carcinoma. The increase in the incidence of IIH subsequent to iodine supplementation is minimal and self limiting. Increase in incidence of IIH has been observed only when iodine is supplemented for a population living in a severely iodine deficient area and more likely to occur only when large doses of iodine are given over a short period of time and is limited to the age groups >40 yr old64. IIH is believed to occur only in subjects with pre-existing autonomous nodular goiter or in patients with latent Graves’ disease, i.e. iodine supplementation merely unmasks the underlying thyroxicosis. Current available evidence linking iodine supplementation with AIT is unequivocal with no study conclusively proving increased incidence of AIT after iodine supplementation65. AIT is a disease of multifactorial aetiology which includes genetic predisposition, environmental factors, and endogenous factors66. Iodine intake may be one of the multiple environmental factors like low birth weight (LBW), viral/bacterial infection, selenium deficiency, radiation, stress, etc. There is no relationship between iodine intake and overall incidence of thyroid cancer67. However, iodine intake leads to an increase in the ratio of papillary (less malignant) to follicular (more malignant) thyroid carcinoma thus having an overall favourable effect. The benefits of iodine supplementation far outweigh the relatively small risks of surplus iodine68,69.
Another critical issue in addressing IDD control in India is devising a strategy to offset the harm caused by the change in IDD control policy and legislations. Serious effects of changes in legislation regulating salt iodization was seen when the Government of India lifted the ban on sale of non-iodized salt in 2000. The iodized salt coverage declined from 49 per cent in 1998-199949 to only 30 per cent in 2002-200351 and subsequently plateauted at 51 per cent in 2005-200650. IDD control programme lost five crucial years due to this change in legislation.
A brief mention also needs to be made about iodine nutrition in light of the recent nuclear radiation accident in Japan70 and mitigating the adverse effects of the same. India is at risk from radiation fallout due to nuclear power plant accidents and threat of nuclear warfare70. The risk from nuclear radiation accidents in India is increased by the region being endemic for iodine deficiency as adverse effects following a nuclear radiation fallout like thyroid cancer are significantly higher in iodine deficient populations71. There is a need to institute disaster preparedness measures to mitigate the damage in case of a nuclear accident.
Conclusions
IDD control programme in India is one of the success stories of public health in the country. The current 91 per cent household level coverage of iodized salt in India, of which 71 per cent is adequately iodized salt, is a big achievement. A mission approach is required with effective and efficient coordination amongst all stakeholders of IDD control efforts in India to achieve and sustain the IDD control goal.
References
- 1.New Delhi: Micronutrient Initiative; 2009. [accessed on July 1, 2011]. Micronutrient Initiative. Investing in the future - a united call to action on vitamin and mineral deficiencies. Global report, 2009. Available from: http://www.unitedcalltoaction.org/documents/Investing_in_the_future.pdf . [Google Scholar]
- 2.Hetzel BS, Delange F, Dunn JT, Ling J, Mannar Venkatesh, Pandav CS, editors. International Council for the Control of Iodine Deficiency Disorders. New Delhi: Oxford University Press; 2004. [accessed on July 1, 2011]. Towards the global elimination of brain damage due to iodine deficiency - a global program for human development with a model applicable to a variety of health, social and environmental problems. Available from: http://www.iccidd.org/cm_data/hetzel-a-frontpage.pdf . [Google Scholar]
- 3.Geneva: World Health Organization; 2007. ICCIDD, UNICEF, WHO. Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers. [Google Scholar]
- 4.Bleichrodt N, Born MP. A meta-analysis of research on iodine and its relationship to cognitive development. In: Stanbury JB, editor. The damaged brain of iodine deficiency - Cognitive behavioral, neuromotor, educative aspects. New York: Cognizant Communication Corporation; 1994. pp. 195–200. [Google Scholar]
- 5.New York: Nutrition Section, Programme Division United Nations Plaza; 2008. UNICEF. Sustainable Elimination of Iodine Deficiency; Progress since the 1990 World Summit for Children. [Google Scholar]
- 6.de Benoist B, McLean E, Andersson M, Rogers L. Iodine deficiency in 2007: global progress since 2003. Food Nutr Bull. 2008;29:195–202. doi: 10.1177/156482650802900305. [DOI] [PubMed] [Google Scholar]
- 7.Geneva: World Health Organization; 1990. World Health Organization. Prevention and Control of Iodine Deficiency Disorders, Report to 43rd World Health Assembly. WHA432. [Google Scholar]
- 8.Bueren GV. World Declaration and Plan of Action on the Survival, Protection and Development of Children. Chapter 72. Martinus WW Nijhoff Publishers; 1998. International documents on children; pp. 414–35. [Google Scholar]
- 9.New York: 2002. May, [accessed on July 1, 2011]. United Nations. United Nations General Assembly Special Session on Children. UNGASS. United Nations Non- Governmental Liaison Service (NGLS) Round up 92. Available from: http://www.un-ngls.org/orf/pdf/ru92kids.pdf . [Google Scholar]
- 10.United Nations Children's Fund. United Nations Plaza, New York: 2011. [accessed on July 1, 2011]. UNICEF. The State of the World's Children 2011. Adolescence; An Age of Opportunity. Available from: http://www.unicef.org/sowc2011/pdfs/SOWC-2011-Main-Report_EN_02092011.pdf . [Google Scholar]
- 11.Iodine Network. Global scorecard 2010. [accessed on July 1, 2011]. Available from: http://www.iodinenetwork.net/documents/scorecard-2010.pdf .
- 12.New Delhi: Directorate General of Health Services Ministry of Health & Family Welfare, Government of India; 2006. [accessed on July 1, 2011]. National Rural Health Mission IDD & Nutrition Cell. Revised Policy Guidelines On National Iodine Deficiency Disorders Control Programme. Available from: http://www.whoindia.org/LinkFiles/Nutrition_Revised_Policy_Guidelines_On_NIDDCP.pdf . [Google Scholar]
- 13.New Delhi: Ministry of Health and Family Welfare, Government of India; 2011. [accessed on July 1, 2011]. Department of Health and Family Welfare. Annual Report 2010-2011. Available from: http://www.mohfw.nic.in/showfile.php?lid=767 . [Google Scholar]
- 14.Prevalence of Micronutrient Deficiencies. Hyderabad: NNMB Technical Report No.22. ICMR, National Institute of Nutrition; 2003. [accessed on July 1, 2011]. National Nutrition Monitoring Bureau. http://www.nnmbindia.org/NNMB%20MND%20REPORT%202004-Web.pdf . [Google Scholar]
- 15.New Delhi: 2010. [accessed on July 1, 2011]. UNICEF. Coverage Evaluation Survey 2009, All India Report. Ministry of Health and Family Welfare, Government of India. Available from: http://www.unicef.org/india/health.html . [Google Scholar]
- 16.New Delhi: Office of Registrar General and Census Commissioner. Ministry of Home affairs, Government of India; 2011. [accessed on July 1, 2011]. Census 2011. Provisional Population Totals Paper 1 of 2011 India Series 1. Available from: http://www.censusindia.gov.in/2011-prov-results/data_files/india/Final%20PPT%202011_chapter3.pdf . [Google Scholar]
- 17.New Delhi: ICCIDD; 2006. [accessed on July 1, 2011]. International Council for Control of Iodine deficiency Disorders (ICCIDD). Tracking Progress Towards Sustaining Elimination of IDD in Seven States 1999-2005. Available from: http://www.iqplusin.org/Reports.htm . [Google Scholar]
- 18.McCarrison R. Observations on Endemic Cretinism in the Chitral and Gilgit Valleys. Proc R Soc Med. 1909;2:1–36. [PMC free article] [PubMed] [Google Scholar]
- 19.Stott H, Bhatia BB, Lal RS, Rai KC. The distribution and cause of endemic goitre in the United Provinces. Indian J Med Res. 1931;18:1059–85. [Google Scholar]
- 20.Ramalingaswami V. The problem of goitre prevention in India. Bull World Health Organ. 1953;9:275–81. [PMC free article] [PubMed] [Google Scholar]
- 21.Kimball OP. History of the prevention of endemic goitre. Bull World Health Organ. 1953;9:241–8. [PMC free article] [PubMed] [Google Scholar]
- 22.Sooch SS, Deo MG, Karmarkar MG, Kochupillai N, Ramachandran K, Ramalingaswami V. Prevention of endemic goitre with iodized salt. Bull World Health Organ. 1973;49:307–12. [PMC free article] [PubMed] [Google Scholar]
- 23.Marine D, Kimball OP. The prevention of simple goiter in man. A survey of the incidence and types of thyroid enlargements in the schoolgirls of Akron (Ohio), from the 5th to the 12th grades, inclusive--the plan of prevention proposed. 1917. J Lab Clin Med. 1990;115:128–36. [PubMed] [Google Scholar]
- 24.Bürgi H, Supersaxo Z, Selz B. Iodine deficiency diseases in Switzerland one hundred years after Theodor Kocher's survey: a historical review with some new goitre prevalence data. Acta Endocrinol. 1990;123:577–90. doi: 10.1530/acta.0.1230577. [DOI] [PubMed] [Google Scholar]
- 25.Pandav CS, Kochupillai N, Karmarkar MG, Nath LM. Iodine deficiency disorders in India: review of control measures. Indian Pediatr. 1986;23:325–9. [PubMed] [Google Scholar]
- 26.Pandav CS, Kochupillai N, Karmarkar MG, Ramachandran K, Gopinath P, Nath LM. Endemic goiter in Delhi. Indian J Med Res. 1980;72:81–8. [Google Scholar]
- 27.Kochupillai N, Pandav CS, Godbole MM, Mehta M, Ahuja MM. Iodine deficiency and neonatal hypothyroidism. Bull World Health Organ. 1986;64:547–51. [PMC free article] [PubMed] [Google Scholar]
- 28.An ICMR Task Force Study. New Delhi: ICMR; 1989. Indian Council of Medical Research (ICMR). Epidemiological survey of endemic goitre and endemic cretinism. [Google Scholar]
- 29.Gopalan C. National Goitre Control Programme - A sad Story. Bulletin of Nutrition Foundation of India. 1981. Jul, [accessed on July 1, 2011]. Available from: http://nutritionfoundationofindia.res.in/pdfs/BulletinArticle/nfi_07_81.pdf .
- 30.Pandav CS, Kochupiliai N, Nath LM. National policy on endemic goiter - harbinger of national policy on nutrition. Indian J Pediatr. 1984;51:277–82. doi: 10.1007/BF02754672. [DOI] [PubMed] [Google Scholar]
- 31.16th ed. Lucknow: Eastern Book Company; 1994. Prevention of Food Adulteration Act: 1954 (along with Rules, Notifications and Commodity index) [Google Scholar]
- 32.Qian M, Wang D, Watkins WE, Gebski V, Yan YQ, Li M, et al. The effects of iodine on intelligence in children: a meta-analysis of studies conducted in China. Asia Pac J Clin Nutr. 2005;14:32–42. [PubMed] [Google Scholar]
- 33.Mehta M, Pandav CS, Kochupillai N. Intellectual assessment of school children from severely iodine deficient villages. Indian Pediatr. 1987;24:467–73. [PubMed] [Google Scholar]
- 34.Upadhyay SK, Agarwal KN, Rani A, Cherian S, Tripathi AM, Agarwal DK. Developmental lag in preschool children of goitrous mothers. Indian Pediatr. 1983;20:259–63. [PubMed] [Google Scholar]
- 35.SAARC Conference on Children. [accessed on July 1, 2011];ICCW News Bull. 1992 40:68–70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/?term=SAARC+Conference+on+Children.+ICCW+News+Bull.+1992 . [PubMed] [Google Scholar]
- 36.New Delhi: Ministry of Human Resources and Development, Government of India, New Delhi; 2005. [accessed on July 1, 2011]. Department of Women and Child Development. National Plan of Action for Children 2005. Available from: http://wcd.nic.in/NAPAug16A.pdf . [Google Scholar]
- 37.New Delhi: DGHS, Ministry of Health & Family Welfare, Government of India; 2003. Directorate General of Health Services (DGHS). Policy guidelines on national iodine deficiency disorders control programme; pp. 1–10. [Google Scholar]
- 38.New Delhi: Salt Department, Ministry of Commerce and Industry, Government of India; 2010. Salt commissioner of India. Annual Report 2009-2010. [Google Scholar]
- 39.Pandav CS, Yadav K, Karmarkar MG. New Delhi: 2010. Sep 1, [accessed on July 2, 2011]. The Success story of Iodine Deficiency in India: Science, Statesman and Society Wisdom in Hindsight. 2nd Britannia Nutrition Foundation Symposium. Available from: http://www.britannia.co.in/bnf/images/session-2/Prof-CSPandav.pdf . [Google Scholar]
- 40.Pandav CS, Yadav K, Moorthy D, Sankar R, Anand K, Karmarkar MG, et al. New Delhi: National Iodine Deficiency Disorders Control Programme; 2010. National Health Programme Series 5. National Institute of Health and Family Welfare. [Google Scholar]
- 41.New Delhi: Ministry of Health and Family Welfare; 1997. Nov 27, Gazette of India. GSR 670(E) 1997. [Google Scholar]
- 42.New Delhi: Ministry of Health and Family Welfare; 2000. Sep 13, Gazette of India. GSR 716(E) 2000. [Google Scholar]
- 43.New Delhi: Ministry of Health and Family Welfare; 2005. Nov 17, Gazette of India. GSR 670(E) 2005. [Google Scholar]
- 44.New Delhi: National Rural Health Mission, Ministry of Health and Family Welfare, Government of India; 2006. [accessed on July 1, 2011]. UNICEF. Coverage Evaluation Survey, All India Report 2006. Available from: http://www.unicef.org/india/Coverage_Evaluation_Survey_2006.pdf . [Google Scholar]
- 45.Pandav CS, Ansari MA, Karmarkar MG. New Delhi: Centre for Community Medicine and NCSII; 2011. [accessed on July 1, 2011]. Salt from Freedom and Iodized salt for freedom from preventable brain damage. Available at URL: http://www.iqplusin.org/downloads/booklet_english.pdf . [Google Scholar]
- 46.Karmarkar MG, Pandav CS, Yadav K, Kumar R. ‘Mission Approach’ to achieve sustainable elimination of iodine deficiency disorders (IDD) in India. World Journal of Endocrine Surgery Jaypee Brother Medical Publishers (P) Ltd. [accessed on July 1, 2011]. Available from: http://www.jaypeejournals.com/eJournals/ShowText.aspx?ID=3226&Type=FREE&TYP=TOP&IN=_eJournals/images/JPLOGO.gif&IID=248&isPDF=YES .
- 47.Micronutrient Initiative, ICCIDD, Nielsen, Office of the Salt commissioner. Iodised salt coverage study 2010: Conducted across eight states in India. Microonutrient Initiative. 2010. [accessed on July 10, 2011]. Available from: http://www.micronutrient.org/CMFiles/indiasalt-coverage-report-2010.pdf .
- 48.Pandav CS, Arora NK, Krishnan A, Sankar R, Pandav S, Karmarkar MG. Validation of spot-testing kits to determine iodine content in salt. Bull World Health Organ. 2000;78:975–80. [PMC free article] [PubMed] [Google Scholar]
- 49.National Family Health Survey (NFHS-2), 1998-99: India. I. Mumbai: IIPS; 1999. International Institute for Population Sciences (IIPS), Macro International. [Google Scholar]
- 50.National Family Health Survey (NFHS-3), 2005-06: India. I. Mumbai: IIPS; International Institute for Population Sciences (IIPS) and Macro International. 2007. [Google Scholar]
- 51.District Level Household Survey (DLHS-2), 2002-04: India. Mumbai: IIPS; 2006. International Institute for Population Sciences (IIPS) [Google Scholar]
- 52.International Council for Control of Iodine Deficiency Disorders. Independent survey evaluation of universal salt iodisation (USI) in Madhya Pradesh. 1996. Jan, [accessed on June 3, 2011]. Available from: http://www.iqplusin.org/downloads/m%5B1%5D.p._report__Executive_Summary__1996.pdf .
- 53.New Delhi: ICCIDD; The Secretariat. Activity report, National Coalition for Sustained Iodine Intake (NCSII), 2009-2010. [Google Scholar]
- 54.Gordon RC, Rose MC, Skeaff SA, Gray AR, Morgan KMD, Ruffman T. Iodine supplementation improves cognition in mildly iodine-deficient children. Am J Clin Nutr. 2009;90:1264–71. doi: 10.3945/ajcn.2009.28145. [DOI] [PubMed] [Google Scholar]
- 55.New Delhi: Ministry of Health and Family Welfare, Government of India; 1947. Department of Health. Act 47. Part IV Directive Principles of State Policy. [Google Scholar]
- 56.New Delhi: Ministry of law and Justice; 2006. Legislative department. The Food Safety and Standards Act, 2006. Act No. 34 of 2006. [Google Scholar]
- 57.Pandav CS, Ansari MA, Sundaresan S, Karmarkar MG. Salt for Freedom and Iodized Salt for Freedom from Preventable Brain Damage. Indian Coalition for control of Iodine deficiency Disorders (ICCIDD) 5th ed. 2008. Sep, [accessed on July 1, 2011]. Available from: http://www.iqplusin.org/Iec.htm .
- 58.Yadav Kapil, Srivastava R, Badhal S, Palanivel C, Pandav CS, Karmarkar MG. Review of iodine nutrition of pregnant women in India: evidence of significant iodine deficiency. Indian J Med Specialties. 2012;3:49–54. [Google Scholar]
- 59.Andersson M, de Benoist B, Delange F, Zupan J. WHO Secretariat, Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the Technical Consultation. Public Health Nutr. 2007;10:1606–11. doi: 10.1017/S1368980007361004. [DOI] [PubMed] [Google Scholar]
- 60.Markou KB, Georgopoulos NA, Makri M, Anastasiou E, Vlasopoulou B, Lazarou N, et al. Iodine deficiency in Azerbaijan after the discontinuation of an iodine prophylaxis program: reassessment of iodine intake and goiter prevalence in school children. Thyroid. 2001;11:1141–6. doi: 10.1089/10507250152740984. [DOI] [PubMed] [Google Scholar]
- 61.Dunn JT. Complacency: the most dangerous enemy in the war against iodine deficiency. Thyroid. 2000;10:681–3. doi: 10.1089/10507250050137752. [DOI] [PubMed] [Google Scholar]
- 62.Pandav CS, Yadav K, Pandav S, Karmakar MG. Bhopal: Background paper presented at Consultation Meet on Nutrition Policy for Madhya Pradesh; 2009. Jun 4, Sustaining Elimination of Iodine Deficiency Disorders in Madhya Pradesh. [Google Scholar]
- 63.Vir SC. Chapter 16. New Delhi: Woodhead Publishing India Pvt Ltd; 2011. Aug, Public health nutrition in developing countries; pp. 432–72. [Google Scholar]
- 64.Stanbury JB, Ermans AE, Bourdoux P, Todd C, Oken E, Tonglet R, et al. Iodine-induced hyperthyroidism: occurrence and epidemiology. Thyroid. 1998;8:83–100. doi: 10.1089/thy.1998.8.83. [DOI] [PubMed] [Google Scholar]
- 65.Zimmermann MB, Moretti D, Chaouki N, Torresani T. Introduction of iodized salt to severely iodine-deficient children does not provoke thyroid autoimmunity: a one-year prospective trial in northern Morocco. Thyroid. 2003;13:199–203. doi: 10.1089/105072503321319512. [DOI] [PubMed] [Google Scholar]
- 66.Prummel MF, Strieder T, Wiersinga WM. The environment and autoimmune thyroid diseases. Eur J Endocrinol. 2004;150:605–18. doi: 10.1530/eje.0.1500605. [DOI] [PubMed] [Google Scholar]
- 67.Burgess JR, Dwyer T, McArdle K, Tucker P, Shugg D. The changing incidence and spectrum of thyroid carcinoma in Tasmania (1978-1998) during a transition from iodine sufficiency to iodine deficiency. J Clin Endocrinol Metab. 2000;85:1513–7. doi: 10.1210/jcem.85.4.6554. [DOI] [PubMed] [Google Scholar]
- 68.Zimmermann MB, Jooste PL, Pandav CS. Iodine-deficiency disorders. Lancet. 2008;372:1251–62. doi: 10.1016/S0140-6736(08)61005-3. [DOI] [PubMed] [Google Scholar]
- 69.Delange F, Lecomte P. Iodine supplementation: benefits outweigh risks. International Council for Control of Iodine Deficiency Disorders, Brussels, Belgium. Drug Saf. 2000;22:89–95. doi: 10.2165/00002018-200022020-00001. [DOI] [PubMed] [Google Scholar]
- 70.Widespread destruction from Japan earthquake, tsunamis - CNN [Internet] [accesses on July 29, 2011]. Available from: http://articles.cnn.com/2011-03-11/world/japan.quake_1_hokkaidotsunami-east-japanrailway?_s=PM:WORLD .
- 71.Cardis E, Howe G, Ron E, Bebeshko V, Bogdanova T, Bouville A, et al. Cancer consequences of the Chernobyl accident: 20 years on. J Radiol Prot. 2006;26:127–40. doi: 10.1088/0952-4746/26/2/001. [DOI] [PubMed] [Google Scholar]
- 72.Registrar General of India. Sample registration System. SRS BulletinVolume 44 No.1. 2009. Oct, [accessed on July 7, 2011]. Available from: http://www.jsk.gov.in/srs-bulletin/SRS-Bulletin-October-2009.pdf .
- 73.New Delhi: NIHFW; 2002. May, National Institute of Health and Family Welfare (NIHFW). Reproductive and Child health - Module for Medical Officer (Primary Health Centre), Integrated Skill Development Training. [Google Scholar]
- 74.Hetzel BS, Pandav C. 2nd ed. New Delhi: Oxford University Press; 1996. SOS for a billion. The conquest of iodine deficiency disorders. [Google Scholar]


