Abstract
Background:
Post-operative pain is often inadequately treated. Optimal utilization of the available resources is essential for improving pain management.
Aims:
The aim of our study was to determine pain management strategies employed after major abdominal surgeries at our institute and their efficacy and safety.
Settings and Design:
Prospective observational study conducted at a tertiary care hospital.
Materials and Methods:
Patients undergoing elective major abdominal surgeries were included. Post-operative analgesic strategy, co-analgesics used, pain and sedation scores, motor block, nausea and vomiting were recorded and patient satisfaction was determined.
Results:
Data was collected on 100 patients. Epidural analgesia was used in 61, patient controlled intravenous analgesia (PCIA) in 25 and opioid infusion in 14 patients. Multimodal analgesia was employed in 98 patients. The level of epidural was between L1-L3 in 31, T10-L1 in 20 and T8-T10 in 10 patients. Pethidine was used in 80% of patients receiving PCIA. Patients with epidurals at T8-T10 had lower pain scores. Fifteen patients had motor block, 73% of which were with epidural at L1-L3. Fourteen patients complained of nausea. Ninety nine out of 100 patients were satisfied with their analgesia.
Conclusion:
Epidural, PCIA and opioid infusions are used for pain relief after major abdominal surgeries at our hospital. Although there is limited drug availability, regular assessments and appropriate dose adjustments by acute pain management service (APMS) and use of multimodal analgesia led to a high level of patient satisfaction. We recommend that feedback to the primary anesthesiologists by APMS is of utmost importance to enable improvement in practice.
Keywords: Abdominal surgery, analgesia, post-operative pain
Introduction
Management of acute post-operative pain has received keen attention in recent years with considerable concurrent advancement in the field.[1,2] Despite this advancement, post-operative pain continues to be a challenge and is often inadequately treated, leading to patient anxiety, stress and dissatisfaction.[2,3,4] Inadequately treated pain can lead to detrimental physiological effects and may also have psychological, economic and social adverse effects.[2,3] It is believed that if sincere efforts are made, it could be possible to significantly improve the treatment of pain in the developed, as well as the developing countries.[5,6] These efforts are of utmost importance as effective pain relief is a powerful technique to modify surgical stress responses,[7] thereby leading to an improved outcome.
Major abdominal surgeries with upper abdominal incisions lead to severe abdominal pain, which if treated inadequately, can cause shallow breathing, atelectasis, retention of secretions and lack of cooperation in physiotherapy. This increases the incidence of post-operative morbidity and leads to delayed recovery. The choice of post-operative analgesic modality employed after major abdominal surgeries at our university hospital is at the discretion of the primary anesthesiologist responsible for managing the patient in the operating room. The choice mainly depends upon the strategy favored by the concerned anesthesiologist and the availability of drugs and equipment. The supply of drugs is erratic and the quantity of equipment might not be sufficient for every patient.
The acute pain management service (APMS) is responsible for the follow-up of these patients, assessment of their pain, management of inadequate pain relief and treatment of any complications. Evaluation of the practice of post-operative pain management by different anesthesiologists and its effectiveness is an essential step toward identifying the better pain management strategies and devising guidelines to improve practice.[3] Such data can increase the weightage of a request made to institutional administration for streamlining the availability of drugs and equipment. With these objectives in mind, we planned a prospective observational study to determine the practice of post-operative analgesia provision by anesthesiologists of our department and the effectiveness and safety of different modalities used. The rationale behind this effort was, as stated by Rawal, the solution to the problem of inadequacy of post-operative pain management does not actually lie in the acquisition of expensive medication or development and use of new techniques, but rather in the optimal utilization of already available drugs, techniques, facilities and establishment of formal pain management services.[8] By reviewing our own practices, our objective is to identify and promote the more effective pain relief strategies within our own resources for the management of moderate to severe post-operative pain.
Materials and Methods
It was a prospective observational study conducted over 4 months. Approval was obtained from the Departmental Research Committee. All patients undergoing elective major abdominal surgical procedures with midline upper abdominal incisions during the study period were included (Whipple's procedure, hemicolectomy, exploratory laparotomy, extended radical cystectomy and nephrectomy, major debulking gynaecological surgery and abdominal aortic aneurysm surgery). Patients undergoing emergency surgery were excluded. The patient's demographics, American Society of Anesthesiologists (ASA) physical status and type of surgery were recorded.
The patient was followed-up at least twice daily by the doctor and nurse of acute pain service as per the routine practice of APMS. In addition, the on-call resident made an evening round of all patients under APMS, also as per routine practice. Principle mode of analgesia and all co-analgesics used were noted. Pain score, sedation score, motor block, nausea, vomiting or any other complication related to pain management was recorded. Pain was assessed by verbal numeric rating scale of 0-10, where 0 is no pain and 10 represents worst pain imaginable (institution-wide pain assessment scale). Observer's assessment of alertness/sedation was used to assess sedation on a scale of 1-5. Modified Bromage Score[9] was used to assess the motor block (0 = no block, 1 = unable to raise straight leg, able to flex knee, 2 = unable to flex knee, able to move ankle and toes, 3 = unable to move the lower limb). Nausea and vomiting was assessed on a scale of 0-3 (0 = none, 1 = mild nausea on inquiry, 2 = moderate nausea/vomiting - treatment required, 3 = vomiting unresponsive to simple antiemetics). Patient satisfaction with the pain relief was determined by the pain nurse at the time of discharge from APMS by asking them to rate their pain management as excellent, good, fair or poor, whether they were satisfied with the pain modality used and would they be willing to have the same modality in the future, if required.
Statistical analysis
As we were observing the pain management practices following major abdominal surgeries for the first time at our institute and did not have previous data on the practice of using different analgesia modalities from our institute or other institutes of the country, a reference or baseline number to calculate the sample size was not available. We were advised by our statistician to collect the sample on the basis of the time period of 3 or 4 months. Thus, we collected data over a period of 4 months. The data was entered, verified and analyzed using SPSS version 16.0 (SPSS Inc. Chicago, IL). Proportions were calculated for all categorical variables and frequencies were generated for the side-effects.
Results
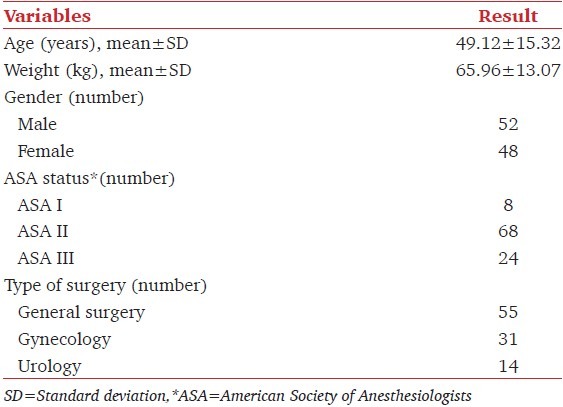
Over a period of 4 months, data was collected on 100 consecutive patients. Demographic features, ASA status and surgical specialty are depicted in Table 1.
Table 1.
Demographic features, ASA status and type of surgery performed
Analgesic modalities for post-operative pain
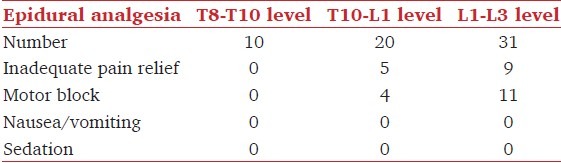
Post-operative analgesia orders were appropriately entered in the patient's files for all patients. Post-operative analgesia was provided with epidural analgesia in 61 patients, whereas patient controlled intravenous analgesia (PCIA) was used in 25 and intravenous (I.V) opioid infusion in 14 patients. Intermittent I.V opioids were not used in any of the 100 patients as the main analgesic strategy. The analgesic modalities employed for different surgical specialties are shown in Figure 1. Multimodal analgesia was employed in 98 patients: I.V paracetamol was used in 90, ketorolac in five and diclofenac suppositories in three patients. In most patients receiving epidural infusion (59/61, 96.7%), the drug used for the infusion included bupivacaine 0.1%, while bupivacaine 0.125% and 0.0625% was used in one patient each. Fentanyl 2 g/ml was added to the epidural infusion in all patients. The rate of infusion was titrated according to the response and kept between 6 and 12 ml/h. The level of epidural insertion was between L1-L3 in 31 patients, T10-L1 in 20 patients and between T8-T10 in 10 patients. Level of epidural, frequency of inadequate pain relief and side effects seen in patients receiving post-operative epidural analgesia are shown in [Table 2]. Epidural infusion was continued for 2 days post-operatively in 47 patients, for 3 days in 13 patients while in one patient epidural infusion was used for 4 days.
Figure 1.
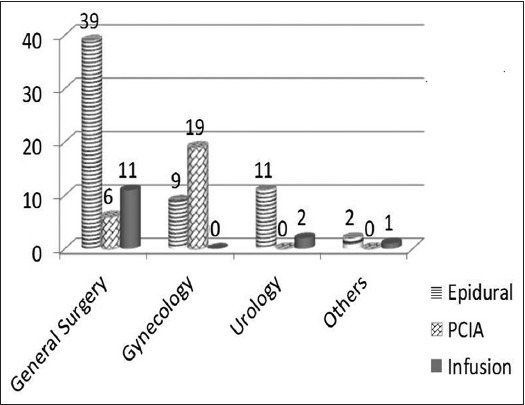
The analgesic modalities used in general surgical, gynecological and urological surgeries
Table 2.
Level of epidural, frequency of inadequate pain relief and side-effects seen in patients receiving post-operative epidural analgesia
Pethidine was used in 20 of the 25 (80%) patients who received PCIA while morphine was used in three and nalbuphine in two patients. All patients with PCIA received a continuous background infusion in addition to the boluses delivered on patient's demand. IV opioid infusion was used as the main analgesic strategies in 14 patients: Pethidine (10-15 mg/h) was used in eight, morphine (1-2 mg/h) in five and nalbuphine (1-3 mg/h) in one patient.
Effectiveness of post-operative analgesia
On the morning of 1st post-operative day, one patient was pain free, 71 patients had mild pain (mean pain score ± standard deviation = 2.53 ± 0.50), 26 had moderate pain (5.46 ± 0.76) and two patients complained of severe pain (7.5 ± 0.70). On the evening visit the same day, pain scores were found to be much improved with ten patients pain free and 87 having mild pain (2.05 ± 0.32), while two had moderate pain (6.5 ± 0.71) and only one patient complained of severe pain (pain score 7). All patients had mild to no pain (1.95 ± 0.68) on the 2nd post-operative day. Actions taken by APMS to relieve moderate to severe pain depended upon the analgesic modality being used for the patient. Patients receiving epidural infusions were given one to two additional 5 ml boluses of the same infusion at half-hourly intervals and if pain relief was still unsatisfactory, I.V bolus of tramadol 50 mg was administered. In patients receiving opioids through PCIA or continuous I.V infusion inadequate pain relief was treated with a bolus of I.V tramadol 50 mg. The originally prescribed analgesic strategy was continued and patients were reassessed after an hour of any intervention made.
When considering the different analgesic modalities, one patient receiving PCIA had no improvement in dynamic pain scores despite adjustments made by APMS. All patients with epidurals inserted at the level of T8-T10 had lower pain scores on the day of surgery and post-operatively and their pain improved further with dose adjustment made by the APMS, whereas 5 (5/20, 25%) and 9 (9/31, 29%) patients with epidural at T10-L1 and L1-L3 levels, respectively continued to feel pain despite adjustments in dose, mainly in the upper part of the incision site Table 2, requiring the administration of co-analgesics and additional boluses, which finally settled the pain.
Side-effects
Nausea occurred in 25 patients in the recovery room. Fourteen patients complained of nausea on the first post-operative day. Nausea was relieved in all patients by simple antiemetics. Patients receiving epidural analgesia did not complain of nausea. Sedation was not seen in any patient. On the first post-operative day 15 (24.5%) of the 61 patients receiving epidural analgesia had unilateral motor block, which was 1/3 on modified Bromage Scale in 14 patients and 2/3 in one patient. The action taken to relieve the motor block was change in position, making the patient lie on the side with the blocked leg up. The number decreased to one patient each with a block of 1/3 and 2/3 on the post-operative day 2 and none on day 3. Around 73% of motor blocks (11/15, 73%) were seen in patients with an epidural level of L1-L3 [Table 2].
Patient's feedback
The quality of post-operative analgesia was rated as excellent by 58 patients and good by 41 patients while one patient did not comment. Ninety five patients stated that they would be willing to have the same analgesic modality in the future, if required while five patients were not sure of their choice. Ninety nine patients stated that they were satisfied with their post-operative analgesic modality.
Discussion
Post-operative analgesia was provided with epidural analgesia in 61 patients, whereas PCIA was used in 25 and I.V opioid infusion in 14 patients. The follow-up and management performed by APMS led to improvement in pain scores and reduction in complications. Pain is one of the most feared factors in the perioperative period. Effective post-operative analgesia is desirable on humanitarian grounds, as well as for its potential to improve post-operative recovery, rehabilitation and outcome.[1,2] In our hospital regular APMS rounds are conducted thrice a day and all post-operative patients receiving epidural infusions, PCIA, continuous I.V opioid infusions or nerve blocks are visited. Patients are assessed for pain and any analgesia related side-effects. Dosages of analgesic agents are adjusted accordingly, additional analgesics are added if required and the side-effects are managed.
During our study, intraoperative analgesia was provided with epidural in 59% patients while 41% received I.V opioids. Adequate intraoperative analgesia, early assessment of pain in the recovery room, prompt delivery of adequate pain medications and continuity of pain relief in the post-operative period through well thought-out strategies are essential for effective pain management. Park et al.[10] in their study, have concluded that intraoperative epidural with general anesthesia followed by continuous epidural infusion improve the overall outcome and shorten the intensive care stay in patients undergoing abdominal aortic operations and other major abdominal surgeries.
PCIA was used in 25 of the 39 patients who received opioid based post-operative analgesia during our study period. This mode of post-operative analgesia has proven to be convenient and safe,[11] allowing patients to adjust their dosages to suit their variable needs, as the demand for analgesics is rarely constant throughout the day. When compared with continuous I.V infusion, PCIA leads to decreased consumption of drugs and a higher patient satisfaction.[12] Patients feel that they have control over their own pain management and this is said to be the main reason for the higher patient satisfaction level.[13] Fourteen patients received opioids by continuous I.V infusion, which has been shown to be superior to the intermittent administration, with a much reduced incidence of break-through pain.[13,14]
A multimodal approach is recommended for post-operative pain management.[2,6,13,15,16] This usually consists of regional analgesic techniques, opioids, non-steroidal anti-inflammatory agents and paracetamol. All anesthesiologists at our hospital used multimodal analgesia for major abdominal surgeries; paracetamol being the most commonly used co-analgesic. The rationale for using multimodal analgesia is the achievement of effective analgesia with the additive or synergistic effects of different classes of analgesic agents with reduced doses of individual drugs and a decreased incidence of side-effects,[16] improved recovery, shorter hospitalization times[17] and better patient satisfaction.
We found considerable variation in the level of epidural insertion among the different anesthesiologists. As all patients included in our study had incisions extending to the xiphisternum, adequate analgesia was more likely to be achieved through a thoracic epidural. However, over 50% of the epidurals were inserted between L1-L3 and only 10 patients had the epidural inserted between T8-T10. None of the latter group had pain on the day of surgery and had only mild dynamic pain on subsequent days, whereas patients with epidurals inserted at lower levels had a higher incidence of inadequate pain relief in the upper part of the incision [Table 2]. Patients with epidural at L1-L3 also had the highest incidence of motor block (35.5%). Chisakuta et al.,[18] in their comparison between lumbar and thoracic epidural for major upper abdominal surgeries, concluded that the thoracic epidural route proved significantly more reliable than the lumbar and provided effective analgesia in all patients. This was not accompanied by significant hypotension or respiratory depression. The incidence of side-effects was significantly higher with lumbar epidural route. They supported the use of thoracic epidural for post-operative pain management after upper abdominal surgery. Königsrainer et al. reported that 52.4% of patients with lumbar epidural catheters developed post-operative lower limb motor weakness, compared with only 4.8% of patients with a thoracic epidural.[19]
In our patients, there was a marked improvement in pain relief between the morning and evening of the first post-operative day. This observation highlights the role of APMS in maximizing pain relief by regular pain assessment and dose adjustments/addition of analgesics accordingly. The importance of formal APMS to improve the post-operative pain management has been recognized for several years and they are now established in most hospitals of Europe, North America and in some major hospitals of the developing countries.[8] These services have the responsibility of improving the quality and safety of post-operative pain management.[13] Cousins et al.[20] have rightly stated that the introduction of APMS has led to an increase in the use of specialized pain relief methods, such as patient-controlled analgesia and epidural infusions of local anesthetic/opioid mixtures, in surgical wards. Implementation of these methods may represent real advances in improving patient well-being and reducing post-operative morbidity. We have observed that APMS has been instrumental in improving the safety profile of these methods in surgical wards. It is essential that APMS team provides regular feedback to the primary anesthesiologists so that they are aware of the limitations in their routine practices and make practice changes accordingly. The authors have presented this data in the departmental research meeting and stressed the importance of changing practices, where indicated, especially regarding the level of epidural insertion for major abdominal surgeries, to help achieve better post-operative pain relief. A cross-sectional survey conducted after 6 months would be useful in assessing the change of practice with respect to epidural insertion level.
The availability of potent opioid drugs is an on-going problem in our country. The choice of opioids is dependent upon the agents available and thus varies from time to time. Potent drugs such as fentanyl and morphine, when available, are usually reserved for high risk patients and for cardiothoracic surgical patients. During our study period, 77% of patients receiving PCIA and 54% of those getting continuous I.V opioid infusion received pethidine as it was the main opioid agent available at the time. There have been times in the past when morphine, pethidine and fentanyl were all running short and we had to make do with less potent agents such as tramadol or nalbuphine even for patients with severe post-operative pain, augmenting the analgesia with a multimodal technique. According to the World Health Organization report of 2003, only about 6% of the morphine stocks are available in developing countries where over 80% of the world's population resides.[21]
We assessed the presence of side-effects as a means of ascertaining the safety and tolerability of the different drugs and strategies employed. Nausea and vomiting was the main side-effect seen with the use of I.V opioids while motor block was the most common side-effect in patients receiving epidural infusions. Nausea and vomiting is a very unpleasant sensation leading to considerable discomfort. Motor block is unpleasant and also delays rehabilitation. The management steps taken by APMS to address these side-effects resulted in a marked decrease in their occurrence and intensity, as ascertained in subsequent rounds. Motor block was seen in a higher number in patients with a lumbar epidural. We have recommended the insertion of lower thoracic epidurals for upper abdominal surgeries rather than lumbar epidurals. This change of practice is expected to decrease the incidence of motor block, as observed by Königsrainer et al.[19] However, an audit will be required in the future to ascertain this change in practice.
We discerned a high level of satisfaction among our patients with post-operative pain management. This is very encouraging for the APMS staff, as the adjustments made by them improved quality of pain relief and reduced side-effects. Prospective collection of data is the strength of our study. However, a limitation of our study is that we did not collect data on the interventions and adjustments in doses made by the APMS team to improve pain relief or manage side-effects. Studies conducted by the APMS to assess the efficacy of the pain management strategies, the occurrence of complications and patient's satisfaction are important to improve practices and enhance the quality of acute pain management. Such studies are especially useful when their results are shared with the practicing anesthesiologists and guidelines developed according to the available resources. In resource limited set-ups, it can be said that it's the mind-set of the anesthesiologist that matters and not the presence of gadgets. Careful selection of the available drugs and techniques is bound to lead to optimal pain relief and patient satisfaction. The authors recommend that acute pain services must conduct on-going data collection on the interventions and treatment alterations made by them to optimize pain relief and treat side-effects and must share this data in an endeavor to achieve practice excellence.
We conclude that APMS rounds and interventions lead to an overall improvement in pain relief and reduction in side-effects. Feedback to the primary anesthesiologists is of utmost importance to enable improvement in practice trends.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Kehlet H. Effect of postoperative pain treatment on outcome-Current status and future strategies. Langenbecks Arch Surg. 2004;389:244–9. doi: 10.1007/s00423-004-0460-4. [DOI] [PubMed] [Google Scholar]
- 2.White PF, Kehlet H. Improving postoperative pain management: What are the unresolved issues? Anesthesiology. 2010;112:220–5. doi: 10.1097/ALN.0b013e3181c6316e. [DOI] [PubMed] [Google Scholar]
- 3.Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: Results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003;97:534–40. doi: 10.1213/01.ANE.0000068822.10113.9E. [DOI] [PubMed] [Google Scholar]
- 4.White PF. Pain management after ambulatory surgery-where is the disconnect? Can J Anaesth. 2008;55:201–7. doi: 10.1007/BF03021503. [DOI] [PubMed] [Google Scholar]
- 5.Brennan F, Carr DB, Cousins M. Pain management: A fundamental human right. Anesth Analg. 2007;105:205–21. doi: 10.1213/01.ane.0000268145.52345.55. [DOI] [PubMed] [Google Scholar]
- 6.Kehlet H, Wilkinson RC, Fischer HB, Camu F Prospect Working Group. PROSPECT: Evidence-based, procedure-specific postoperative pain management. Best Pract Res Clin Anaesthesiol. 2007;21:149–59. doi: 10.1016/j.bpa.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Kehlet H, Holte K. Effect of postoperative analgesia on surgical outcome. Br J Anaesth. 2001;87:62–7. doi: 10.1093/bja/87.1.62. [DOI] [PubMed] [Google Scholar]
- 8.Rawal N. Acute pain services revisited: Good from far, far from good? Reg Anesth Pain Med. 2002;27:117–21. doi: 10.1053/rapm.2002.29110. [DOI] [PubMed] [Google Scholar]
- 9.Bromage PR. A comparison of the hydrochloride and carbon dioxide salts of lidocaine and prilocaine in epidural analgesia. Acta Anaesthesiol Scand Suppl. 1965;16:55–69. doi: 10.1111/j.1399-6576.1965.tb00523.x. [DOI] [PubMed] [Google Scholar]
- 10.Park WY, Thompson JS, Lee KK. Effect of epidural anesthesia and analgesia on perioperative outcome: A randomized, controlled Veterans Affairs cooperative study. Ann Surg. 2001;234:560–9. doi: 10.1097/00000658-200110000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McDonnell NJ, Keating ML, Muchatuta NA, Pavy TJ, Paech MJ. Analgesia after caesarean delivery. Anaesth Intensive Care. 2009;37:539–51. doi: 10.1177/0310057X0903700418. [DOI] [PubMed] [Google Scholar]
- 12.Bertini L. PCA vs. continuous infusion. [Accessed on 2012 Jun 21]. Available from: http://www.anestitunipait/sitosiaarti/3aneortoped/49new.htm .
- 13.Macintyre PE, Schug SA. Acute Pain Management. 3rd ed. Edinburgh: Saunders Elsevier; 2007. [Google Scholar]
- 14.Lubenow TR, Ivankovich AD, Barkin RL. Management of acute postoperative pain. In: Barash PG, Cullen BF, Stoelting RK, editors. Clinical Anesthesia. Philadelphia PA: Lippincott Williams and Wilkins; 2006. pp. 1405–40. [Google Scholar]
- 15.Rawal N. Analgesia for day-case surgery. Br J Anaesth. 2001;87:73–87. doi: 10.1093/bja/87.1.73. [DOI] [PubMed] [Google Scholar]
- 16.Buvanendran A, Kroin JS. Multimodal analgesia for controlling acute postoperative pain. Curr Opin Anaesthesiol. 2009;22:588–93. doi: 10.1097/ACO.0b013e328330373a. [DOI] [PubMed] [Google Scholar]
- 17.White PF, Sacan O, Tufanogullari B, Eng M, Nuangchamnong N, Ogunnaike B. Effect of short-term postoperative celecoxib administration on patient outcome after outpatient laparoscopic surgery. Can J Anaesth. 2007;54:342–8. doi: 10.1007/BF03022655. [DOI] [PubMed] [Google Scholar]
- 18.Chisakuta AM, George KA, Hawthorne CT. Postoperative epidural infusion of a mixture of bupivacaine 02% with fentanyl for upper abdominal surgery. A comparison of thoracic and lumbar routes. Anaesthesia. 1995;50:72–5. doi: 10.1111/j.1365-2044.1995.tb04518.x. [DOI] [PubMed] [Google Scholar]
- 19.Königsrainer I, Bredanger S, Drewel-Frohnmeyer R, Vonthein R, Krueger WA, Königsrainer A, et al. Audit of motor weakness and premature catheter dislodgement after epidural analgesia in major abdominal surgery. Anaesthesia. 2009;64:27–31. doi: 10.1111/j.1365-2044.2008.05655.x. [DOI] [PubMed] [Google Scholar]
- 20.Cousins MJ, Power I, Smith G. 1996 Labat lecture: Pain - A persistent problem. Reg Anesth Pain Med. 2000;25:6–21. doi: 10.1016/s1098-7339(00)80005-x. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization. The World Health Report 2003. Geneva: WHO; 2003. [Accessed on 2012 Jul 19]. Available from: http://www.who.int/whr/2003/en/overview_en.pdf . [Google Scholar]


