Abstract
The quadratus lumborum (QL) block as a postoperative analgesic method following abdominal surgery has been described by Blanco for superficial surgeries but not used for major laparotomy. This ipsilateral QL block had low pain scores and opioid use on day one with sensory block upto T8-L1. The options of various volume used and pros and cons are discussed.
Keywords: Postoperative analgesia, quadratus lumborum, ultrasound
Introduction
Quadratuslumborum (QL) block has been described by Blanco and used as an analgesic for abdominoplasties (unpublished).[1] The radiological study on posterior approach of Transversus Abdominis Plane block (now called QL block) in volunteers has shown the spread of the dye and local anaesthetics from T4-L1.[2] Its efficacy is yet to be determined in a major surgery. To evaluate its efficacy in major laparotomy, it was considered in this case
Case Report
66-year-old gentleman, ASA 3 was scheduled for laparotomy for duodenal tumour excision. His other medical conditions were type 2 diabetes mellitus, cardiomyopathy, chronic smoker, and obstructive sleep apnoea on Continuous Positive Airway Pressure (CPAP) machine. Postoperative analgesia options were discussed with the patient. He was not keen on epidural, but happy to consider other options. He was offered patient controlled analgesia (PCA) fentanyl, QL block, and multimodal analgesia. We had explained the QL block as a novel technique. He preferred to undergo the block while sleeping. After taking informed consent, anesthesia was induced with propofol (Fresofol® fresenius, Sydney, New South Wales, Australia), fentanyl (fentanyl citrate DBL Hospira, Melbourne, Australia), and rocuronium (Esmeron, MSD, Sydney, New South Wales, Australia) for Neuro muscular (NM) paralysis. Maintenance of anesthesia was with 50:50 O2 and air with sevoflurane. The abdomen was opened via right-side large subcostal incision. The procedure lasted 2.5 h and was uneventful. At the end of the procedure, he was positioned in left lateral to obtain appropriate view of QL and TAP extensions of lateral abdominal muscles. Aseptic precautions were taken by wearing sterile gown and sterile drapes. Ultrasound Macro Maxx™ (SonositeInc, Bothell, Washington, USA) was used with linear probe (HFL38_10-5 MHz) covered with sterile plastic sheath SiteRite (Bard Access Systems Inc., Salt lake city, Utah, USA) placed in the anterior axillary line to visualize the typical triple abdominal layers. Then, the probe was placed in the midaxillary line and at this juncture the layers of abdominal layers started to taper. When the probe was placed in the posterior axillary line as per the posterior approach, sonoanatomy showed first the transversus abdominis disappearing then the internal oblique and external oblique forming aponeurosis and appearance of QL noticed [Figure 1]. Figure 1a shows typical muscles layers and the fascia. At the junction of the tapered ends of abdominal muscles and QL, a 21 g 100 mm SonoPlexStimu cannula needle (Pajunk Medizintechnologie Geisingen, Germany0) was inserted in plane [Figure 2] and confirmed its position by injecting saline. Under ultrasound (US) guidance, saline separating the fascia similar to what is seen in the TAP plane was observed. Then in that space 25 mL of 0.5% ropivacaine (Naropin-AstraZeneca, Sydney, North South Wales, Australia) was injected [Figure 3]. Pain scores using the numerator rating scale (NRS) from 0 to 10 were recorded hourly in recovery room and then in the high dependency ward and fentanyl use was monitored for 24 h. He received a fentanyl PCA with bolus dose of 20 mcg with lock out interval of 5 min and multimodal analgesia comprising paracetamol1g every 6 h and parecoxib (Dynastat, Pfizer Pty Ltd, North South Wales Australia) 40 mg daily.
Figure 1.
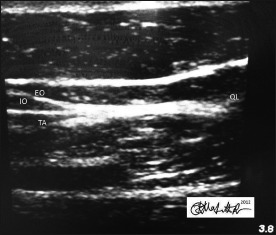
The sonoanatomy of junction between the lateral abdominal layers and the quadrates lumborum. EO = External oblique, IO = Internal oblique, QL = Quadratuslumborum
Figure 1a.
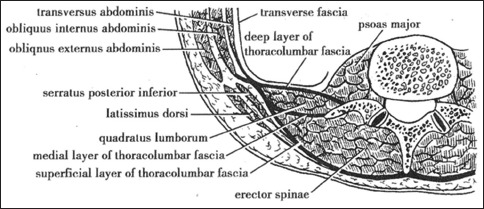
The abdominal muscle layers with thoracolumbar fascia (Source: medicinembbs.blogSpot.com)
Figure 2.
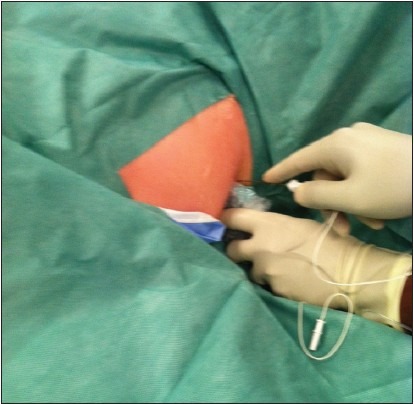
The in plane approach to quadrateslumborum block
Figure 3.
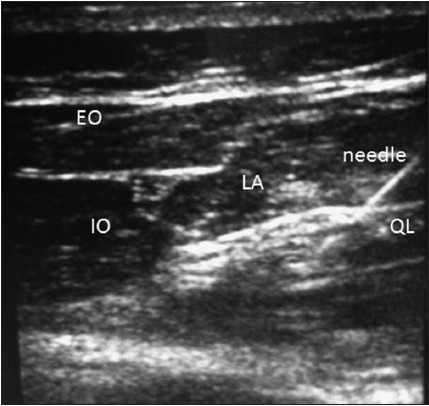
The quadrates lumborum block with local anesthtetic. EO = External oblique, IO = Internal oblique, QL = Quadratuslumborum
Postoperatively in recovery, he did not require any further analgesia. Pain scores were 0/10 and the ipsilateral sensory block was T8-L1. The first analgesic request was about 3 h postoperative. After 15 h, he started experiencing pain requiring more fentanyl PCA amounting to 720 mcg for the remaining day. The average pain scores on day one were 4/10 at rest and 6/10 on coughing and comfortable. The 2nd day, the pain scores were 7/10 and 9/10 requiring 1000 mcg of fentanyl.
Discussion
From this case report, it appears that this novel block has a role in postoperative analgesia in abdominal surgery. Our case had reduced pain scores and opioid requirement in 24 h. With QL block, the opioid use was similar to the day 1TAP block pattern as observed in our previous study.[3] After the success of the single shot technique, we are doing catheter technique. In retrospective, use of continuous catheter infusion would have reduced the 2nd postoperative day pain scores and opioid use. In this patient, it was easy to perform the unilateral QL block in lateral position in the bed. A bilateral block would be needed for midline incisions with more physical support.
Is it different from TAP block? QL is the extension of TAP block toward the dorsal region. The US-guided TAP block has the limitation of requiring two levels of block to cover incisions above and below umbilicus.[4] The QL block in single shot has the advantage of covering all the dermatome segments from caudally L2 to cranially till T4 segments as the drug is expected to travel from the QL to the higher paravertebral spaces.[2] Carney et al., described that the contrast solution placed posteriorly accumulates near the lateral border of the QL and then spreads in a posterior-cranial fashion to the anterior aspect of the QL and psoas major to lie at the paravertebral space. They also saw the contrast enhancement from T4-L2. This was also demonstrated by McDonnell et al.,[5] in the landmark technique, a single bolus dose covering the incisions above and below umbilicus. In our case, the sensory block only covered T8-L1.
This may be due to low volume used. There are no guidelines on the volume of drug to be injected. Based on a radiological study,[2] we administered 0.3 mL/kg of ropivacaine. High doses such as 0.6 mL/kg could cover more dermatomes. In an US-guided contrast study by Barrington et al.,[6] on cadavers demonstrated that multiple injections could involve more nerves. This may amount to use up to at least 30-40 mL to obtain spread to as high as T4 level and expect to last longer. But Carney et al's[2] study in landmark-guided TAP block in volunteers found that 0.6 mL/kg doses had inconsistent distribution of sensory block.2 Toxicity is a concern to use such high volumes. The drug dosage description is beyond the scope of this case report. Considering, the duration was only for a day in our case a catheter infusion may provide longer analgesia. There is a proposal to perform catheter infusion case series in this institute.
In practice, sensory block in volunteers and clinical setting may be different as sensory spread didnot reflect same as in our case. It is difficult to ascertain whether a different pattern exist between blocks performed awake and asleep. It is also not known at this stage whether the extent of spread be sufficient for both anterior and posterior abdominal surgical areas. Theoretically, it should be possible as the block spreads to the paravertebral space to block the nerves as they exit. There may be fewer disadvantages to this block. It may have to be performed in prone position, which is ideal preoperatively, though some of the patients may experience discomfort. If done intraoperative as in this case you may need extrapersonnel to hold the patient and monitor the airway. Extra care may be necessary to avoid trauma to kidney. Further, well-defined studies are needed to confirm the efficacy of QL block, especially for extended incision to loin and long midline incisions.
Conclusion
Our case with QL block highlights its use in postoperative analgesia in major abdominal surgery. More case series for midline incisions and even appropriate randomized trial comparing TAP block are necessary to establish its role in clinical practice.
Acknowledgments
I appreciate Chelsea Hicks for assisting in images and Dr. Venkatesan for going through the manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Blanco R. TAP block under ultrasound guidance: The description of a ‘nonpopstechnique’. Reg Anaesth Pain Med. 2007;32(Suppl 1):130. [Google Scholar]
- 2.Carney J, Finnerty O, Rauf J, Bergin D, Laffey JG, Mc Donnell GJ. Studies on the spread of local anaesthetic solution in transverses abdominis plane blocks. Anaesthesia. 2011;66:1023–30. doi: 10.1111/j.1365-2044.2011.06855.x. [DOI] [PubMed] [Google Scholar]
- 3.Kadam RV, Field JB. Ultrasound-guided continuous transverse abdominis plane block for upper abdominal surgery. J Anaesthesiol Clin Pharmacol. 2011;27:333–6. doi: 10.4103/0970-9185.83676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hebbard PD, Barrington MJ, Vasey C. Ultrasound-guided continuous oblique subcostal transversusabdominis plane blockade: Description of anatomy and clinical technique. Reg Anesth Pain Med. 2010;35:436–41. doi: 10.1097/aap.0b013e3181e66702. [DOI] [PubMed] [Google Scholar]
- 5.McDonnell JG, O’Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transverses abdominis plane block after abdominal surgery: A prospective randomized controlled trial. Anesth Analg. 2007;104:193–7. doi: 10.1213/01.ane.0000250223.49963.0f. [DOI] [PubMed] [Google Scholar]
- 6.Barrington MJ, Ivanusic JJ, Rozen WM, Hebbard P. Spread of injectate after ultrasound-subcostal transverse abdominis plane block: A cadaveric study. Anaesthesia. 2009;64:745–50. doi: 10.1111/j.1365-2044.2009.05933.x. [DOI] [PubMed] [Google Scholar]


