Abstract
Background:
For patients with ST-elevation myocardial infarction (STEMI), guidelines recommend prehospital triage and direct referral to a percutaneous coronary intervention (PCI)-capable centre in order to minimize ischemic time. However, few have studied failed prehospital diagnosis. We assessed the incidence, predictors, and clinical impact of interhospital transfer for primary PCI after initial referral to a non-PCI-capable centre due to a failed prehospital STEMI diagnosis.
Methods:
We studied 846 consecutive STEMI patients undergoing primary PCI between January 2008 and January 2010.
Results:
We found that 609 patients (72%) were directly admitted through prehospital triage and 127 patients (15%) required interhospital transfer after failed prehospital diagnosis. Median first medical contact to treatment time was 88 min in the prehospital diagnosis group and 155 min in the interhospital transfer group (p<0.001). In the interhospital transfer group, the first available electrocardiogram was diagnostic for STEMI in 77% of cases. Predictors of interhospital transfer were female gender, diabetes, prior myocardial infarction, and greater event location to PCI-capable centre distance. Interhospital transfer independently accounted for a 47% increase in ischemic time (95% CI 33 to 63%; p<0.001). One-year mortality was higher in the interhospital transfer group (10 vs. 5.3%; p=0.030).
Conclusions:
Despite an often-diagnostic electrocardiogram, interhospital transfer after failed prehospital diagnosis occurred in 15% of STEMI patients undergoing primary PCI. Interhospital transfer was a major predictor of ischemic time and 1-year mortality was significantly higher. Continuing efforts to optimize prehospital triage are warranted, especially among patients at higher risk of failed prehospital diagnosis.
Keywords: Angioplasty, delay, emergency medical services, ischemic time, myocardial infarction, triage
Introduction
In patients with ST-elevation myocardial infarction (STEMI), rapidly performed primary percutaneous coronary intervention (PCI) by an experienced team has shown to be a superior reperfusion strategy over fibrinolysis,1 even if the patient is initially admitted to a non-PCI-capable centre.2 As a longer time from symptom onset to reperfusion therapy (ischemic time) has been associated with decreased myocardial reperfusion and increased mortality,3,4 many efforts have been made in reducing it. Recently published European Society of Cardiology (ESC) guidelines recommend prehospital diagnosis and direct referral to a PCI-capable centre for primary PCI as the preferred strategy to minimize ischemic time in patients with STEMI.5 Whenever possible, non-PCI-capable centres should be bypassed. In addition, faster system performance is proposed with first medical contact to treatment time (system delay) ≤90 min and door-to-balloon time ≤60 min. Numerous studies document the implementation of regional 12-lead electrocardiogram (ECG)-based prehospital triage systems with subsequent reductions in door-to-balloon time and ischemic time.6–9 However, the proportion of STEMI patients diagnosed by these prehospital triage systems is often unclear. Thus, little is known about the occurrence and clinical impact of a failed prehospital diagnosis in a fully operational prehospital triage system. Our primary purpose was to study the incidence and predictors of interhospital transfer for primary PCI after initial referral to a non-PCI-capable centre due to failure of prehospital STEMI diagnosis and assess its impact on delay to reperfusion and mortality. Furthermore, we studied ECG characteristics of STEMI patients undergoing interhospital transfer due to failed prehospital diagnosis.
Methods
Study design and population
We currently studied the incidence, predictors, and clinical impact of interhospital transfer due to failed prehospital diagnosis. Failed prehospital diagnosis was defined as failure to activate the prehospital triage protocol for STEMI and initial referral of a STEMI patient to a non-PCI-capable centre, despite the regional agreement with emergency medical services (EMS) and referral centres and to directly refer STEMI patients for primary PCI. All consecutive patients with suspected STEMI undergoing acute coronary angiography between 1 January 2008 and 1 January 2010 were considered for this analysis. Among this group, we selected patients with STEMI who had undergone prehospital triage for primary PCI (prehospital diagnosis group) and patients with a failed prehospital diagnosis of STEMI and subsequent interhospital transfer for primary PCI (interhospital transfer group). STEMI was defined as chest pain suggestive of myocardial ischaemia, time from onset of symptoms of less than 12 hours, and an ECG diagnostic for STEMI with new or presumed-new ST-segment elevation in 2 or more contiguous leads of ≥0.2 mV in leads V2–V3 and/or ≥0.1 mV in other leads or left bundle branch block. Primary PCI was the preferred reperfusion strategy for all patients, and fibrinolytics were never administered. Importantly, we excluded all self-referrals, since these patients could not have been diagnosed in the prehospital setting. We also excluded patients on mechanical ventilation, as this may had been a reason for an intermediate admission to the nearest non-PCI-capable centre despite a diagnosis of STEMI. Finally, we excluded patients admitted to our emergency department (ED) and patients with onset of STEMI during hospitalization for other conditions.
Setting
This study was conducted at the University Medical Center Groningen, The Netherlands. With five non-PCI-capable referral hospitals, this centre provides 24/7 emergency care in a region with 750,000 inhabitants. It is the only PCI-capable centre in this region and provides on-site cardiothoracic surgical support. Our EMS consists of ambulances staffed by a driver trained at a paramedic level and a nurse trained at an intensive care level who is experienced in ECG interpretation. In rare occasions, a helicopter staffed by an anaesthesiologist, a nurse, and a pilot is used for complex situations or remote locations. As a national benchmark, EMSs are required to arrive at the scene within 15 min of activation.
Prehospital triage route
In the prehospital setting, EMS staff performed a 12-lead ECG in all patients presenting with symptoms suggestive of acute myocardial infarction. A computerized algorithm aided EMS nursing staff in their assessment of whether the patient was likely to have a STEMI. Subsequent activation of the prehospital triage protocol by contacting the coronary care unit (CCU) of our centre was at the discretion of the EMS nurse. In case of an unclear diagnosis, the EMS nurse was allowed to contact the cardiologist on duty and send the ECG by fax. Once the prehospital triage protocol was activated, near non-PCI-capable centres and the ED of our centre were bypassed. The patient was transported directly to the catheterization laboratory or, less frequently, to the CCU if the catheterization laboratory was not yet available. A bed at the CCU was kept available at all times for emergency procedures. During transportation, the EMS nurse notified the CCU of the oncoming arrival of a STEMI patient and provided the CCU with the patient’s data and estimated time of arrival. Antiplatelet and antithrombin therapy were usually started in the ambulance and consisted of aspirin (500 mg), heparin (5000 IU), and clopidogrel (600 mg), administered by the EMS nurse. During regular hours, the catheterization team was present in our centre and could be activated by the CCU using a pager system. During off-hours, the CCU activated the catheterization team by having the central phone operator call the catheterization team on duty. The catheterization laboratory kept a room ready and equipped during off-hours. The above prehospital triage protocol was the preferred route of admission for patients with STEMI. After its implementation in January 2004, it was followed by all EMS within a range of 90 min of our centre.
Interhospital transfer route
Interhospital transfer for primary PCI was required in case of a failed prehospital diagnosis of STEMI and referral to a non-PCI-capable centre by EMS. Furthermore, EMS staff may refer patients requiring mechanical ventilation to the closest centre for initial stabilization, despite a prehospital diagnosis of STEMI. These patients were transferred for primary PCI after stabilization. All five referral centres were within a range of 60 km and patients were transferred by ambulance. All patients with STEMI were transferred to our centre for primary PCI, and aspirin (500 mg), heparin (5000 IU), and clopidogrel (600 mg) were usually started at the referral centre.
Methods of measurement
Baseline and procedural measures of all patients undergoing primary PCI were documented upon admission and were prospectively collected in a dedicated database. For the interhospital transfer group, the first available ECG was collected by audits to the referring centres and assessed by an experienced cardiologist (BS) blinded to other patient data. EMS time intervals and geographical event location were obtained from EMS registries. Time of first medical contact was defined as EMS arrival at the scene. The time of EMS arrival at the first centre was deemed the ‘door’ time. For patients undergoing interhospital transfer, door-in to door-out time was defined as the interval between arrival and departure at the non-PCI-capable centre. System delay was defined as time of first medical contact to initial intracoronary therapy by means of thrombus aspiration or balloon inflation of the infarct related coronary artery. Ischemic time was defined as time from symptom onset to initial intracoronary therapy. Other time intervals were calculated accordingly. All time-to-reperfusion data were available in >90% of patients except for door-in to door-out time (87%). TIMI flow and myocardial blush grade were scored by the operator during the PCI procedure as previously described and validated.10,11 All-cause mortality was collected using municipal civil registries. These registries provide completeness of follow up regarding mortality in >99% of patients admitted to our department.
Statistical analysis
Continuous variables were summarized as mean±standard deviation or median and interquartile range. Discrete variables were presented as counts and percentages. To compare groups, we used Student’s t-test for normally distributed continuous variables, Mann–Whitney U-test for nonparametric continuous variables, Pearson’s χ2 test for categorical variables, and the linear trend test for ordinal variables. Time-to-treatment intervals and all-cause mortality were analysed and plotted using the Kaplan–Meier method and group differences were tested with the log-rank test. For all analyses, p<0.05 (two-tailed) was considered statistically significant.
A multivariable logistic regression model and a multivariable Cox proportional hazards model were fitted to assess independent predictors of interhospital transfer and 1-year all-cause mortality, respectively. All baseline characteristics listed in Table 1 with p<0.10 in univariable analysis and interhospital transfer were considered for the models. To assess independent predictors of ischemic time, a multivariable linear regression model was fitted. All variables listed in Table 1 with p<0.10 in univariable analysis, interhospital transfer, and total distance travelled by EMS were considered. Ischemic time was first transformed logarithmically, to account for its skewed distribution. Parameter estimates and 95% confidence intervals (CI) were retransformed into meaningful units in the final model. For all multivariable models, a backward stepwise method was used. Predictors remained in the multivariable model if p<0.05. Data was presented as odds ratios (OR) and 95% CI or hazard ratios and 95% CI where appropriate. Statistical analyses were performed with SPSS version 18.0.3 (SPSS, Chicago, Illinois) and Stata version 11.0 (StataCorp, College Station, Texas).
Table 1.
Baseline characteristics.
| Prehospital diagnosis (n=609) | Interhospital transfer (n=127) | p -value | |
|---|---|---|---|
| Age (years) | 65±13 | 66±13 | 0.287 |
| Female | 173/609 (28) | 50/127 (39) | 0.014 |
| Body mass index (kg/m2) | 27±3.9 | 27±4.4 | 0.147 |
| Systolic blood pressure | |||
| mmHg | 128±27 | 129±28 | 0.706 |
| ≤90 mmHg | 48/603 (8.0) | 10/124 (8.1) | 0.969 |
| Heart rate | |||
| bpm | 77±19 | 79±18 | 0.197 |
| >100 bpm | 61/600 (10) | 14/124 (11) | 0.709 |
| Hypertension | 243/599 (41) | 59/123 (48) | 0.130 |
| Diabetes | 55/606 (9.1) | 22/125 (18) | 0.005 |
| Hypercholesterolaemia | 146/540 (27) | 38/110 (35) | 0.111 |
| Current smoking | 300/604 (50) | 53/124 (43) | 0.160 |
| Positive family history | 258/594 (43) | 56/116 (48) | 0.337 |
| Prior MI | 51/606 (8.4) | 26/125 (21) | <0.001 |
| Prior PCI | 48/606 (7.9) | 13/127 (10) | 0.390 |
| Prior CABG | 11/605 (1.8) | 3/127 (2.4) | 0.684 |
| Prior admission to our department | 101/609 (17) | 25/127 (20) | 0.399 |
| Anterior MI | 280/608 (46) | 65/127 (51) | 0.292 |
| Event location to PCI-capable centre distance (km) | 27 (16–38) | 32 (22–44) | 0.004 |
| Helicopter transport | 2 (0.3) | 0 (0) | |
Values are n/N (%), mean±SD, or median (interquartile range).
CABG, coronary artery bypass grafting; MI, myocardial infarction; PCI, percutaneous coronary intervention.
Results
Study population and route of admission
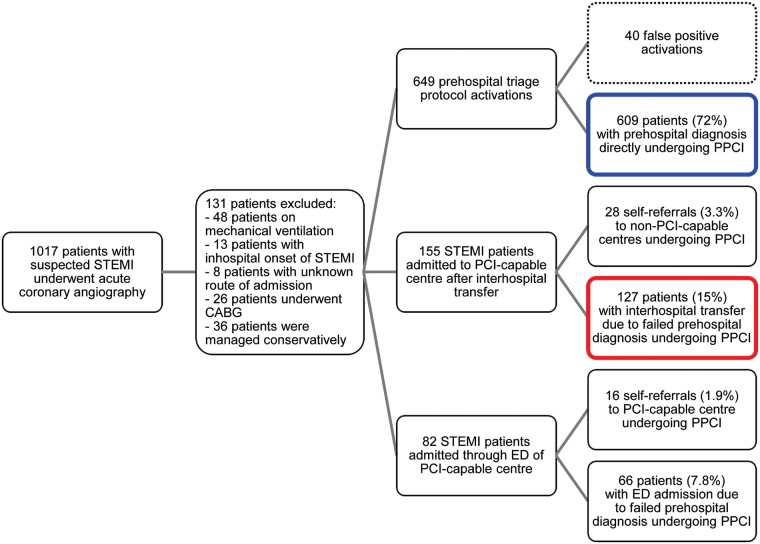
A flowchart for our study population is shown in Figure 1. Between 1 January 2008 and 1 January 2010, prehospital ECGs were performed in 12,555 patients by the EMS, 1017 patients with suspected STEMI underwent acute coronary angiography, and 846 consecutive patients with STEMI underwent primary PCI. Of the latter, 609 patients (72%) were admitted through our prehospital triage protocol (prehospital diagnosis group) and 127 patients (15%) underwent interhospital transfer for primary PCI after failed prehospital diagnosis (interhospital transfer group). Other STEMI patients were emergency department admissions (n=66; 7.8%) and self-referrals (n=44; 5.2%). There were a total of 649 prehospital triage protocol activations of which 40 (6.2%) were false-positive.
Figure 1.
Flowchart for study design and route of admission of patients.
CABG, coronary artery bypass grafting; ED, emergency department; PPCI, primary percutaneous coronary intervention.
Baseline characteristics of patients in the prehospital diagnosis group and interhospital transfer group are shown in Table 1. Patients in the interhospital transfer group were more likely to be female (39 vs. 28%; p=0.014) and have higher rates of diabetes (18 vs. 9.1%; p=0.005) and prior myocardial infarction (21 vs. 8.4%; p<0.001), when compared with patients in the prehospital diagnosis group. Furthermore, patients in the interhospital transfer group were at greater median distance from the PCI-capable centre when they experienced their event (32 vs. 27 km; p=0.004). Remarkably, the number of patients with any prior inpatient or outpatient admission to our department did not differ between the interhospital transfer and prehospital diagnosis groups (20 vs. 17%; p=0.399).
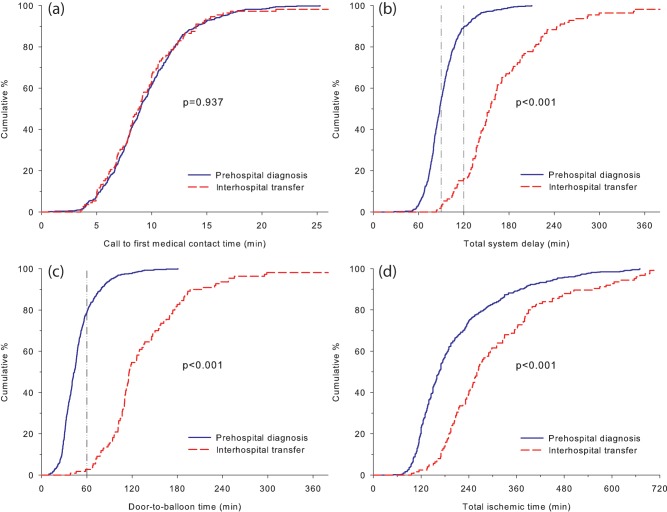
Time-to-treatment intervals and procedural characteristics
Time-to-treatment intervals are shown in Table 2. No differences were seen in call to first medical contact time (Figure 2A), and median first medical contact to first door time was slightly shorter in patients in the interhospital transfer group (34 vs. 44 min; p<0.001). However, patients in the interhospital transfer group experienced additional delays due to door-in to door-out time at the non-PCI-capable centre (median 52 min) and interhospital transportation time (median 29 min). Consequently, substantially longer system delay (median 155 vs. 88 min; p<0.001; Figure 2B) and door-to-balloon time (median 116 vs. 43 min; p<0.001; Figure 2C) were seen in the interhospital transfer group. System delay ≤90 min was achieved in 2.7% of patients in the interhospital transfer group compared with 54% in the prehospital diagnosis group (p<0.001). These rates were 16 and 90% for system delay ≤120 min (p<0.001). Door-to-balloon time ≤60 min was achieved in 2.7 and 79% of patients in the interhospital transfer and prehospital diagnosis group, respectively. Median ischemic time was 263 min for patients in the interhospital transfer group and 165 min for patients in the prehospital diagnosis group (p<0.001; Figure 2D).
Table 2.
Time-to-treatment intervals and procedural characteristics.
| Prehospital diagnosis (n=609) | Interhospital transfer (n=127) | p -value | |
|---|---|---|---|
| Symptom onset to call time (min) | 62 (28–139) | 76 (38–161) | 0.156 |
| Symptom onset to FMC time (min) | 72 (37–150) | 91 (47–171) | 0.151 |
| Call to FMC time (min) | 9 (7–11) | 9 (7–11) | 0.937 |
| FMC to door 1 time (min) | 44 (37–52) | 34 (27–43) | <0.001 |
| Door-in to door-out time (min) | N/A | 52 (31–85) | |
| Interhospital transportation time (min) | N/A | 29 (19–34) | |
| Door-to-balloon time (min) | 43 (32–56) | 116 (102–166) | <0.001 |
| Total system delay (min) | 88 (78–103) | 155 (132–198) | <0.001 |
| Total ischemic time (min) | 165 (125–242) | 263 (202–380) | <0.001 |
| Total distance travelled by EMS (km) | 27 (16–38) | 40 (25–53) | <0.001 |
| Off-hour PCIa | 272/606 (45) | 56/127 (44) | 0.871 |
| Target coronary artery | <0.001 | ||
| Right | 240/608 (40) | 35/127 (28) | |
| Left anterior descending | 276/608 (45) | 59/127 (47) | |
| Circumflex | 85/608 (14) | 25/127 (20) | |
| Left main | 4/608 (0.7) | 6/127 (4.7) | |
| Graft | 3/608 (0.5) | 2/127 (1.6) | |
| Preprocedural TIMI flow | 0.224 | ||
| 0/1 | 360/609 (59) | 69/127 (54) | |
| 2 | 125/609 (21) | 26/127 (21) | |
| 3 | 124/609 (20) | 32/127 (25) | |
| Post-procedural TIMI flow | 0.085 | ||
| 0/1 | 14/607 (2.3) | 2/127 (1.6) | |
| 2 | 46/607 (7.6) | 20/127 (16) | |
| 3 | 547/607 (90) | 105/127 (83) | |
| Post-procedural myocardial blush grade | 0.071 | ||
| 0/1 | 147/583 (25) | 37/115 (32) | |
| 2 | 209/583 (36) | 42/115 (37) | |
| 3 | 227/583 (39) | 36/115 (31) | |
| Glycoprotein IIb/IIIa inhibitor use | 550/607 (91) | 112/127 (88) | 0.404 |
Values are n/N (%) or median (interquartile range).
Before 08:00 hours or after 18:00 hours.
EMS, emergency medical systems; FMC, first medical contact; PCI, percutaneous coronary intervention; TIMI, thrombolysis in myocardial infarction.
Figure 2.
Time-to-treatment intervals: (a) call to first medical contact time; (b) total system delay with 90- and 120-minute reference lines; (c) door-to-balloon time with 60-minute reference line; (d) total ischemic time for patients in the prehospital diagnosis and interhospital transfer groups.
Patients in the interhospital transfer group and prehospital diagnosis group were equally likely to be treated during off-hours (44 vs. 45%; p=0.871; Table 2). The culprit coronary artery was significantly different between both groups (p<0.001). Patients in the interhospital transfer group had higher rates of circumflex artery infarctions (20 vs. 14%) and lower rates of right coronary artery infarctions (28 vs. 40%). The rate of left anterior descending artery infarctions was similar in both groups. Post PCI, epicardial and microvascular myocardial reperfusion as assessed by TIMI flow and myocardial blush grade trended towards poorer results in the interhospital transfer group (p=0.085) and (p=0.071), respectively (Table 2).
ECG characteristics
To gain further insight in the reasons for a failed prehospital diagnosis in the interhospital transfer group, the first available ECG was collected and assessed. ECG characteristics of the patients in the interhospital transfer group are shown in Table 3. Although this group of patients was not directly referred for primary PCI, only 14% of the first available ECGs showed ST-elevation <0.2 mV. The rate of patients with left bundle branch block was 6.9%. Overall, 77% of ECGs were diagnostic for STEMI.
Table 3.
ECG characteristics of interhospital transfer patients.
| Interhospital transfer (n=127) | |
|---|---|
| ECG available | 118 |
| ECG not assessablea | 2 |
| ECG diagnostic for STEMI | 91/118 (77) |
| Symptom onset to ECG time (min) | 135 (72–228) |
| Left bundle branch block | 8/116 (6.9) |
| Right bundle branch block | 5/116 (4.3) |
| ST-segment | |
| Assessable | 108 |
| ST-elevation | |
| <0.2 mV | 15/108 (14) |
| 0.2–0.5 mV | 42/108 (39) |
| 0.6–1.0 mV | 33/108 (31) |
| >1.0 mV | 18/108 (17) |
| ST-deviation | |
| <0.2 mV | 10/108 (9.3) |
| 0.2–0.5 mV | 28/108 (26) |
| 0.6–1.0 mV | 29/108 (27) |
| >1.0 mV | 41/108 (38) |
Values are n/N (%) or median (interquartile range)
Due to arrhythmia.
Predictors of interhospital transfer
In order to identify patient subgroups at higher risk of interhospital transfer, we assessed predictors of failed prehospital diagnosis (Table 4). After multivariable adjustment, female gender (OR 1.58, 95% CI 1.01–2.46; p=0.046), diabetes (OR 1.98, 95% CI 1.11–3.55; p=0.022), prior myocardial infarction (OR 2.86, 95% CI 1.62–5.08; p<0.001), and distance from event location to PCI-capable centre (OR 1.22 per 10 km, 95% CI 1.07–1.39; p=0.002) were independent predictors of interhospital transfer.
Table 4.
Independent predictors of interhospital transfer by logistic regression.
| Odds ratio (95% CI) | p -value | |
|---|---|---|
| Female gender | 1.58 (1.01–2.46) | 0.046 |
| Diabetes | 1.98 (1.11–3.55) | 0.022 |
| Prior MI | 2.86 (1.62–5.08) | <0.001 |
| Event location to PCI-capable centre distance (per 10 km) | 1.22 (1.07−1.39) | 0.002 |
CABG, coronary artery bypass grafting; MI, myocardial infarction.
Predictors of ischemic time
Predictors of total ischemic time in multivariable analysis are shown in Table 5. Age and heart rate were independently associated with longer ischemic time. However, interhospital transfer was the most powerful predictor of ischemic time and was associated with an estimated 47% increase in ischemic time (95% CI 33 to 63%; p<0.001). Notably, the impact of interhospital transfer on ischemic time was adjusted for total distance travelled by EMS (estimate +1.9% per 10 km, 95% CI −0.3 to 4.0%; p=0.088).
Table 5.
Independent predictors of ischemic time by linear regression.
| Estimate (%) | 95% CI | p -value | |
|---|---|---|---|
| Age (per decade) | +7.5 | 4.8 to 10 | <0.001 |
| Heart rate (per 10 bpm) | +3.5 | 1.6 to 5.5 | <0.001 |
| Interhospital transfer | +47 | 33 to 63 | <0.001 |
| Distance travelled by EMS (per 10 km) | +1.9 | −0.3 to 4.0 | 0.088 |
EMS, emergency medical systems.
Clinical outcome
Follow up with regard to mortality at 30 days and 1 year was completed in all patients. Thirty-day mortality was 7.1% in the interhospital transfer group and 3.3% in the prehospital diagnosis group (p=0.043). This pattern was similar at 1-year follow up, with 10% mortality in the interhospital transfer group vs. 5.3% mortality in the prehospital diagnosis group (p=0.030; Figure 3). Independent predictors of mortality at 1-year follow up are shown in Table 6. After multivariable adjustment, an independent association between interhospital transfer and mortality could not be demonstrated (hazard ratio 1.42, 95% CI 0.70–2.88; p=0.335).
Figure 3.
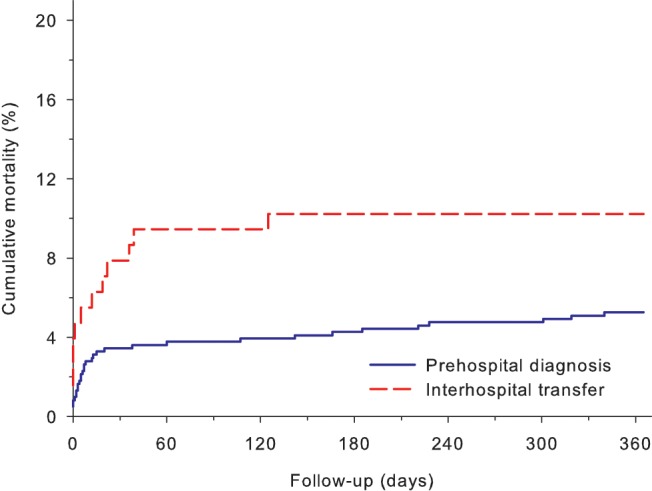
One-year mortality: 10% in the interhospital transfer group and 5.3% in the prehospital diagnosis group (p=0.030).
Table 6.
Independent predictors of mortality at 1-year follow up by Cox regression.
| Hazard ratio (95% CI) | p -value | |
|---|---|---|
| Age (per decade) | 4.35 (2.91–6.51) | <0.001 |
| Systolic blood pressure (per 10 mmHg) | 0.70 (0.63–0.79) | <0.001 |
| Current smoking | 2.14 (1.04–4.40) | 0.038 |
| Prior MI | 2.39 (1.15–4.98) | 0.020 |
| Anterior MI | 2.17 (1.13–4.16) | 0.020 |
| Interhospital transfer | 1.42 (0.70–2.88) | 0.335 |
MI, myocardial infarction.
Discussion
We currently studied a comprehensive fully operational prehospital triage system with a single PCI-capable centre and five non-PCI capable referral centres where the preferred reperfusion strategy for all patients with STEMI was primary PCI and self-referrals were excluded. Principal findings of our study were: (1) among patients with STEMI undergoing primary PCI, the incidence of interhospital transfer due to failed prehospital diagnosis was 15%; (2) in the interhospital transfer group, recommended system delay ≤90 min was seen in only 2.7% of patients, while this rate was 54% for patients in the prehospital diagnosis group; (3) despite a failed prehospital diagnosis, the first available ECG was diagnostic for STEMI in 77% of patients in the interhospital transfer group; (4) patients with onset of STEMI at greater distance from a PCI-capable centre were at higher risk of interhospital transfer, as were women, diabetics, and patients with prior myocardial infarction; (5) interhospital transfer was independently associated with an estimated 47% increase in ischemic time; and (6) mortality was significantly higher in the interhospital transfer group.
Prior studies comparing patients admitted through prehospital triage and interhospital transfer have been performed, but were conducted during the implementation period of the prehospital triage protocol,8 did not use primary PCI as the preferred reperfusion strategy for all patients with STEMI,12 or were limited by inclusion of self-referrals.13,14 Our study design lacked these limitations and allowed us to accurately estimate the rate of failed prehospital diagnosis and identify subgroups with higher risk of interhospital transfer. Moreover, our study includes the newly published ESC system performance measures, demonstrating that substantial improvement in first medical contact to treatment time is necessary for all STEMI patients despite relatively fast treatment times once the patient has arrived at the PCI-capable centre.
The incidence of interhospital transfer due to failed prehospital diagnosis was 15% in our study. This rate is similar to prior studies, reporting rates of 15 and 22%.8,12 Despite its relatively low incidence, interhospital transfer was found to be a major predictor of ischemic time in our study. In a secondary analysis of the HORIZONS-AMI trial, interhospital transfer was also found to be associated with the greatest delay to reperfusion.15 Thus, considerable delay occurs in the group of patients not directly admitted to a PCI-capable centre and guideline recommended first medical contact to treatment time is not met. This finding is supported by most,13,14,16 but not all17 prior studies. Also, the finding that 72% of patients are directly referred for primary PCI after prehospital diagnosis closely resembles the rate of 73% recently reported in a small single-centre study.18 Remarkably, we found that distance travelled by EMS was not predictive of ischemic time in multivariable analysis. This suggests that, within our geographical context, distance travelled by EMS is of minor relevance for total ischemic time. For interhospital transfer patients, most time is lost as door-in to door-out time at the non-PCI-capable centre, rather than interhospital transportation time. The minor impact of EMS transportation distance on total ischemic time was also underlined by a Danish study.8
We found that women and diabetics were at higher risk of interhospital transfer. This may relate to the phenomenon that symptom presentation in these subgroups is often atypical and without chest pain.19–21 Atypical clinical presentation in these subgroups may limit recognition of STEMI by EMS staff and increase the risk of interhospital transfer. Patients with prior myocardial infarction were also at greater risk of interhospital transfer. Although these patients are likely to recognize symptoms of myocardial infarction, ECG interpretation may be harder. Still, the first available ECG in the interhospital transfer group was retrospectively considered diagnostic for STEMI in 77% of cases.
The 1-year mortality we observed in interhospital transfer patients was approximately twice the rate of prehospital diagnosis patients. However, we could not demonstrate an independent association between interhospital transfer and mortality. Part of the excess mortality in the interhospital transfer group may be explained by higher rates of high-risk subgroups, such as patients with prior myocardial infarction and diabetics. However, ischemic time was considerably longer in patients undergoing interhospital transfer and longer ischemic time and system delay have been clearly associated with decreased myocardial reperfusion, greater enzymatic infarct size, poorer left ventricular function, and higher mortality in prior studies, mostly with greater sample size.3,4,22 Therefore, we believe our study was not sufficiently powered to detect an independent association between interhospital transfer and mortality.
ESC guidelines recommend immediate fibrinolysis when expected system delay to primary PCI exceeds 120 min.5 In our study, 84% of patients in the interhospital transfer group and 10% of patients in the prehospital diagnosis group had a system delay >120 min. In some of these patients, fibrinolysis may be an alternative reperfusion strategy. However, we and others23 believe that, in the context of STEMI networks with short transfer distances, further improvements in STEMI care are likely to come from efforts to improve prehospital triage and, if needed, efficient interhospital transfer in order to provide timely primary PCI rather than accepting delays and resorting to fibrinolysis. An important aspect in this process is discussing lessons from analyses as these with all regional STEMI care participants. Now that an increasing number of prehospital triage systems have been successfully implemented, future research should focus on optimization of operational prehospital triage systems by maximizing the percentage of STEMI patients included without an inacceptable rise in false-positive activations. Therefore, it is important to identify patient subgroups at risk of failed prehospital diagnosis and develop interventions aimed at reducing the rate of interhospital transfer in these patients. A greater distance from event location to a PCI-capable centre should not be a reason for an intermediate admission to a non-PCI-capable centre in a haemodynamically stable patient, since substantial delays occur as door-in to door-out time at a non-PCI-capable centre while greater distance travelled by EMS results in minor delays. Furthermore, EMS staff should be aware of the often-atypical symptom presentation in women and diabetics with STEMI. Transportation to a PCI-capable centre should be promptly performed in case of diagnostic uncertainty or difficulties with ECG interpretation in patients with prior myocardial infarction. Finally, physicians should be aware that patients with STEMI initially admitted to a non-PCI-capable centre mostly comprise a group of patients with higher mortality, rather than patients with minor ECG changes and a favourable outcome.
Study limitations
It is important to consider several limitations of our study. First, we studied all patients with suspected STEMI undergoing acute coronary angiography. Therefore, we may have missed patients eligible for primary PCI who died before admission, resulting in an underestimation of mortality. Second, we defined treatment time as time of initial intracoronary therapy (by thrombus aspiration or balloon inflation) which is slightly later than time of wire passage through the culprit lesion, used in the new ESC guidelines. Third, ECGs in patients undergoing interhospital transfer were retrospectively analysed by a single cardiologist. Although ECGs were reviewed independently of other patient data, this may have introduced a bias. Although we put much effort in obtaining the first ECG made by EMS, it is likely that some of the ECGs we assessed were not the first ECG. As studies have shown that an additional 15% of STEMI patients may be diagnosed by performing serial prehospital ECGs,24 the rate of diagnostic ECGs we found in the interhospital transfer group (77%) may be an overestimate. Clearly, it is hard to prevent admission to a non-PCI-capable centre in patients who initially present with a non-diagnostic ECG. Finally, we did not study patients on mechanical ventilation, as this may had been a reason for an intermediate admission to the nearest non-PCI-capable centre despite a prehospital diagnosis of STEMI. Therefore, the results of our study should not be generalized to this complex subgroup of patients.
Conclusions
In a fully operational prehospital triage system, failed prehospital diagnosis and subsequent interhospital transfer occurred in 15% of STEMI patients undergoing primary PCI despite an often-diagnostic ECG. Interhospital transfer was a major predictor of ischemic time and short-term and long-term mortality were higher. Continuing efforts to optimize prehospital triage and direct referral for primary PCI in patients with STEMI are warranted, especially for patients with onset of STEMI at greater distance from a PCI-capable centre, women, diabetics, and patients with prior myocardial infarction.
Acknowledgments
The authors would like to thank all referral centres, regional ambulance facilities, and Pieter CW van der Mijle, MSc for their assistance with data collection.
Footnotes
Conflict of interest: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 2003; 361: 13–20 [DOI] [PubMed] [Google Scholar]
- 2. Dalby M, Bouzamondo A, Lechat P, Montalescot G. Transfer for primary angioplasty versus immediate thrombolysis in acute myocardial infarction: a meta-analysis. Circulation 2003; 108: 1809–1814 [DOI] [PubMed] [Google Scholar]
- 3. Magid DJ, Wang Y, Herrin J, et al. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA 2005; 294: 803–812 [DOI] [PubMed] [Google Scholar]
- 4. Fokkema ML, Wieringa WG, van der Horst IC, et al. Quantitative analysis of the impact of total ischemic time on myocardial perfusion and clinical outcome in patients with ST-elevation myocardial infarction. Am J Cardiol 2011; 108: 1536–1541 [DOI] [PubMed] [Google Scholar]
- 5.Authors/Task Force Members, Steg PG, James SK, et al. ; the Task Force on the Management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC) ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012; 33: 2569–2619 [DOI] [PubMed] [Google Scholar]
- 6. Adams R, Appelman Y, Bronzwaer JG, et al. Implementation of a prehospital triage system for patients with chest pain and logistics for primary percutaneous coronary intervention in the region of Amsterdam, The Netherlands. Am J Cardiol 2010; 106: 931–935 [DOI] [PubMed] [Google Scholar]
- 7. Nestler DM, White RD, Rihal CS, et al. Impact of prehospital electrocardiogram protocol and immediate catheterization team activation for patients with ST-elevation-myocardial infarction. Circ Cardiovasc Qual Outcomes 2011; 4: 640–646 [DOI] [PubMed] [Google Scholar]
- 8. Sorensen JT, Terkelsen CJ, Norgaard BL, et al. Urban and rural implementation of pre-hospital diagnosis and direct referral for primary percutaneous coronary intervention in patients with acute ST-elevation myocardial infarction. Eur Heart J 2011; 32: 430–436 [DOI] [PubMed] [Google Scholar]
- 9. Ortolani P, Marzocchi A, Marrozzini C, et al. Pre-hospital ECG in patients undergoing primary percutaneous interventions within an integrated system of care: reperfusion times and long-term survival benefits. EuroIntervention 2011; 7: 449–457 [DOI] [PubMed] [Google Scholar]
- 10.The thrombolysis in myocardial infarction (TIMI) trial. phase I findings. TIMI study group N Engl J Med 1985; 312: 932–936 [DOI] [PubMed] [Google Scholar]
- 11. Kampinga MA, Nijsten MW, Gu YL, et al. Is the myocardial blush grade scored by the operator during primary percutaneous coronary intervention of prognostic value in patients with ST-elevation myocardial infarction in routine clinical practice? Circ Cardiovasc Interv 2010; 3: 216–223 [DOI] [PubMed] [Google Scholar]
- 12. Dieker HJ, Liem SS, El Aidi H, et al. Pre-hospital triage for primary angioplasty: direct referral to the intervention center versus interhospital transport. JACC Cardiovasc Interv 2010; 3: 705–711 [DOI] [PubMed] [Google Scholar]
- 13. Postma S, Dambrink JH, de Boer MJ, et al. Prehospital triage in the ambulance reduces infarct size and improves clinical outcome. Am Heart J 2011; 161: 276–282 [DOI] [PubMed] [Google Scholar]
- 14. Wang TY, Peterson ED, Ou FS, et al. Door-to-balloon times for patients with ST-segment elevation myocardial infarction requiring interhospital transfer for primary percutaneous coronary intervention: a report from the national cardiovascular data registry. Am Heart J 2011; 161: 76–83.e1 [DOI] [PubMed] [Google Scholar]
- 15. Blankenship JC, Skelding KA, Scott TD, et al. Predictors of reperfusion delay in patients with acute myocardial infarction undergoing primary percutaneous coronary intervention from the HORIZONS-AMI trial. Am J Cardiol 2010; 106: 1527–1533 [DOI] [PubMed] [Google Scholar]
- 16. Miedema MD, Newell MC, Duval S, et al. Causes of delay and associated mortality in patients transferred with ST-segment-elevation myocardial infarction. Circulation 2011; 124: 1636–1644 [DOI] [PubMed] [Google Scholar]
- 17. Blankenship JC, Scott TD, Skelding KA, et al. Door-to-balloon times under 90 min can be routinely achieved for patients transferred for ST-segment elevation myocardial infarction percutaneous coronary intervention in a rural setting. J Am Coll Cardiol 2011; 57: 272–279 [DOI] [PubMed] [Google Scholar]
- 18. Schoos MM, Sejersten M, Hvelplund A, et al. Reperfusion delay in patients treated with primary percutaneous coronary intervention: insight from a real world Danish ST-segment elevation myocardial infarction population in the era of telemedicine. Acute Cardiovasc Care 2012; 1: 200–209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Culic V, Eterovic D, Miric D, et al. Symptom presentation of acute myocardial infarction: influence of sex, age, and risk factors. Am Heart J 2002; 144: 1012–1017 [DOI] [PubMed] [Google Scholar]
- 20. Canto JG, Rogers WJ, Goldberg RJ, et al. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA 2012; 307: 813–822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Radovanovic D, Nallamothu BK, Seifert B, et al. Temporal trends in treatment of ST-elevation myocardial infarction among men and women in Switzerland between 1997 and 2011. Acute Cardiovasc Care 2012; 1: 183–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lonborg J, Schoos MM, Kelbaek H, et al. Impact of system delay on infarct size, myocardial salvage index, and left ventricular function in patients with ST-segment elevation myocardial infarction. Am Heart J 2012; 164: 538–546 [DOI] [PubMed] [Google Scholar]
- 23. von Scheidt W, Thilo C. As time goes by? The fallacy of thrombolysis in STEMI networks. Clin Res Cardiol 2011; 100: 867–877 [DOI] [PubMed] [Google Scholar]
- 24. Verbeek PR, Ryan D, Turner L, et al. Serial prehospital 12-lead electrocardiograms increase identification of ST-segment elevation myocardial infarction. Prehosp Emerg Care 2012; 16: 109–114 [DOI] [PubMed] [Google Scholar]