Abstract
Pulmonary vein thrombosis (PVT) is a rare but life-threatening condition. Although warfarin reduces the risk of atrial fibrillation (AF)-related stroke by 64%, the use of this drug has some limitations. Dabigatran is a relatively novel therapeutic option for patients with AF. The mechanism of action of dabigatran is unclear, and its ability to dissolve pulmonary vein thrombi is uncertain. Scans from a 64-slice multidetector CT (64-MDCT) scanner can evaluate coronary artery stenosis and detect left atrial appendage thrombi and pulmonary vein thrombi. A 73-year-old male patient presented with chest pain, and a 64-MDCT scan was performed to assess coronary artery stenosis. The 64-MDCT scan showed no stenosis but it did reveal a thrombus located in the centre of the left upper pulmonary vein. After 3 months of dabigatran therapy, the thrombus disappeared. This is the first case report of dabigatran dissolving a left upper pulmonary vein thrombus, as assessed by a 64-MDCT scan.
Background
Stroke is the leading cause of long-lasting disability and the third leading cause of death worldwide. Approximately 70% of all strokes are acutely ischaemic in nature and are caused by the embolic or atherosclerotic occlusion of cerebral arteries.
Atrial fibrillation (AF) is a common type of arrhythmia and a major risk factor for stroke. Patients with AF are five times more likely to experience strokes compared with those in sinus rhythm, and AF causes approximately 15% of ischaemic strokes. The most common location of thrombi in patients with AF is the left atrial appendage (LAA), the site of approximately 90% of left atrial thrombi. Currently, transoesophageal echocardiography (TOE) is commonly used to detect LAA thrombi.
Pulmonary vein thrombosis (PVT) may cause a stroke if the thrombus embolises; however, little is known about PVT. PVT has been described in cases of primary or secondary neoplasia of the lung1 and as a rare early complication after lung lobectomy, bilobectomy or lung transplantation. Cases of PVT are commonly diagnosed using pulmonary angiography, TOE, contrast-enhanced chest CT or MRI.
Although warfarin reduces stroke by 64% compared with placebo or reference drugs,2 its use is cumbersome due to its slow onset and offset of action and the need to frequently adjust the dose to maintain an adequate plasma concentration. Warfarin also interacts with foods and other drugs; thus, anticoagulants that are effective, safe and convenient to use are required. In cardioembolic stroke, anticoagulants such as warfarin, dabigatran, rivaroxaban and apixaban effectively prevent secondary ischaemic stroke; therefore, differentiating cardioembolic stroke from non-cardioembolic stroke is important. Rasmussen and coworkers reported that among novel oral anticoagulants (dabigatran 150 mg twice daily, apixaban, rivaroxaban) and warfarin, they found significant reductions in stroke/systemic embolism and stroke (both p<0.001), ischaemic stroke (p=0.043), haemorrhagic stroke and disabling/fatal stroke (both p<0.001), death (p=0.003) and vascular mortality (p=0.003). In addition, for safety, significant reductions in major bleeding (p=0.003) and intracranial bleeding (p<0.001) were found.3 Dabigatran is an oral anticoagulant that directly inhibits thrombin. Dabigatran acts rapidly; its peak plasma concentration is reached 0.5–2 h after administration, and its half-life is 12–17 h. Conservative management of PVT consists of treatment with anticoagulants. If lung infarction is suspected based on a severe clinical status, then embolectomy or lobe resection may be indicated. Currently, there are no published reports of the effectiveness of dabigatran for treating PVT.
A 64-slice multidetector CT (64-MDCT) scan can be used to assess coronary artery stenosis and to estimate the extent of coronary artery plaques. In addition, a 64-MDCT scan can more easily and entirely assess LAA thrombi and pulmonary vein thrombi than TOE. In 2012, we reported two cases of small pulmonary vein thrombi.4 In 2013, we reported a completely occluded pulmonary vein thrombus and a left lower pulmonary vein thrombus that extended into the left atrium (LA), as viewed by transthoracic echocardiography (TTE). Although diagnosing ischaemic stroke subtypes correctly at admission is often difficult, 64-MDCT scan allows researchers to identify cardiac thrombi, such as those in the LA, LAA and pulmonary vein.
Dabigatran is an effective anticoagulant, but its mechanism of action is not fully understood. Furthermore, whether dabigatran can dissolve thrombi in the pulmonary vein remains unclear.
In this report, we present a case of an elderly male patient with left PVT that was treated effectively by administering dabigatran for 3 months.
Case presentation
The patient was a 73-year-old man with dyslipidaemia and asthma. The patient reported chest pain that occurred approximately once per month and lasted several minutes but was not associated with exercise or sleep. A 64-MDCT scan was performed to evaluate the presence of coronary artery stenosis. The patient had no symptoms of tachypnoea, fever, cough, sputum or cerebral infarction. The lung examination did not reveal decreased breath sounds, lung crackles or wheezing. The cardiac examination did not demonstrate a heart murmur or arrhythmia. No previous warfarin treatment had been administered. The ECG showed a normal sinus rhythm and normal axis, and the patient's heart rate was 60 bpm. The chest roentgenogram did not reveal lung cancer. The serum D-dimer level was <0.5 μg/mL (normal <1.0 μg/mL), the protein S activity was 96% (normal 60–150%) and the protein C activity was 131% (normal 64–146%). A 64-MDCT scan did not reveal coronary artery stenosis; however, a thrombus was observed in the left upper pulmonary vein (figures 1–3). This thrombus, which resembled a floating thrombus, was located in the centre of the left upper pulmonary vein and did not touch the wall of the vein, allowing the blood flow around the thrombus to be maintained. After 3 months of dabigatran therapy, the defects on contrast-enhanced CT had disappeared (figures 4–6), suggesting that most of the thrombus had dissolved. Dabigatran has the merits of low risk of stroke and bleeding. Also the patient declined treatment with warfarin due to its narrow therapeutic range, which necessitates frequent monitoring and dosage adjustments to ensure optimal anticoagulation. Therefore, he was treated with dabigatran (150 mg twice daily).
Figure 1.
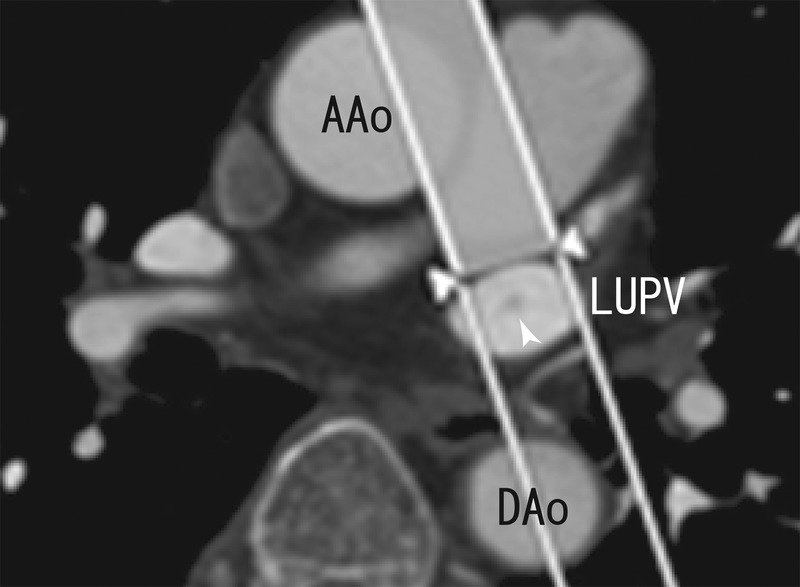
Axial images showing a thrombus in the left upper pulmonary vein (white arrowhead). AAo, ascending aorta; DAo, descending aorta; LUPV, left upper pulmonary vein.
Figure 2.
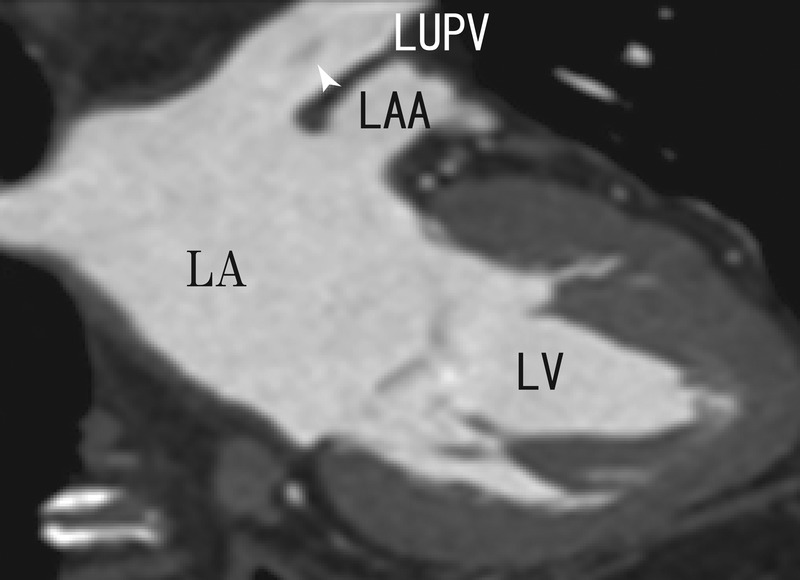
Coronal images showing a thrombus in the left upper pulmonary vein (white arrowhead). LA, left atrium; LAA, left atrial appendage; LUPV, left upper pulmonary vein; LV, left ventricle.
Figure 3.
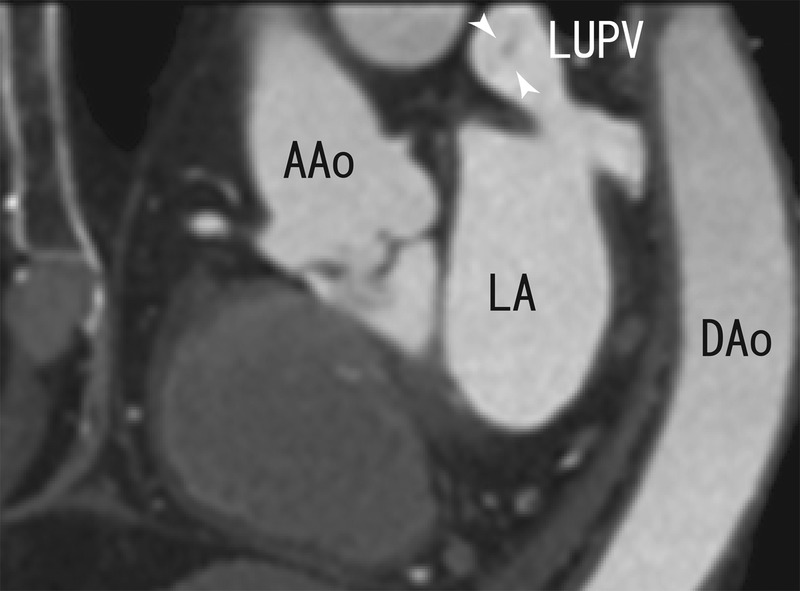
Sagittal images showing a thrombus in the left upper pulmonary vein (white arrowhead). AAo, ascending aorta; DAo, descending aorta; LA, left atrium; LUPV, left upper pulmonary vein.
Figure 4.
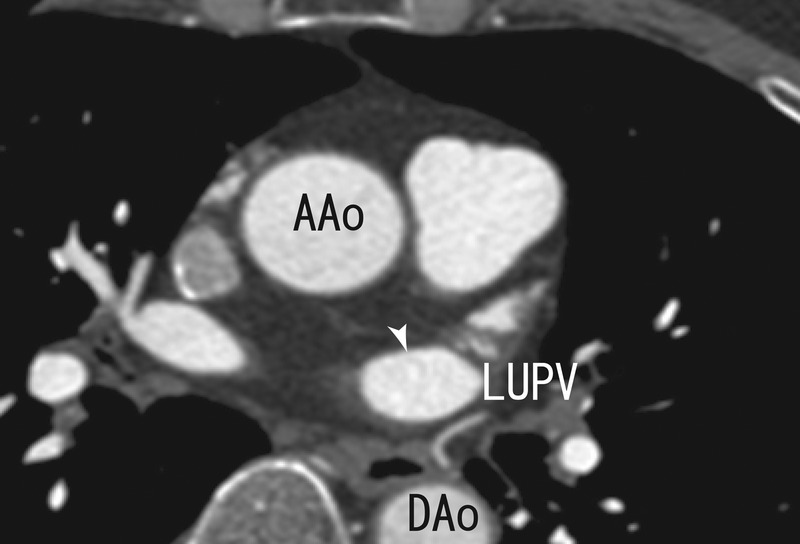
Axial images showing the absence of thrombi in the left upper pulmonary vein (white arrowhead). AAo, ascending aorta; DAo, descending aorta; LUPV, left upper pulmonary vein.
Figure 5.
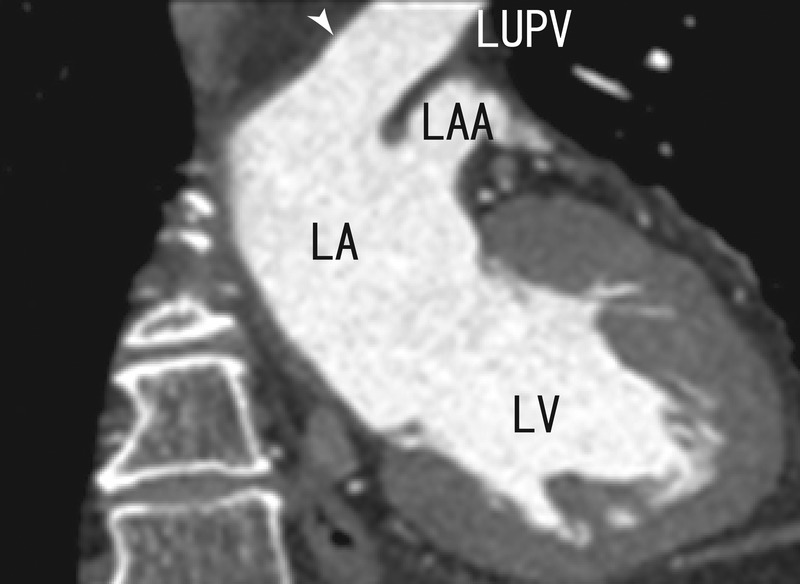
Coronal images showing the absence of thrombi in the left upper pulmonary vein (white arrowhead). LA, left atrium; LAA, left atrial appendage; LUPV, left upper pulmonary vein; LV, left ventricle.
Figure 6.
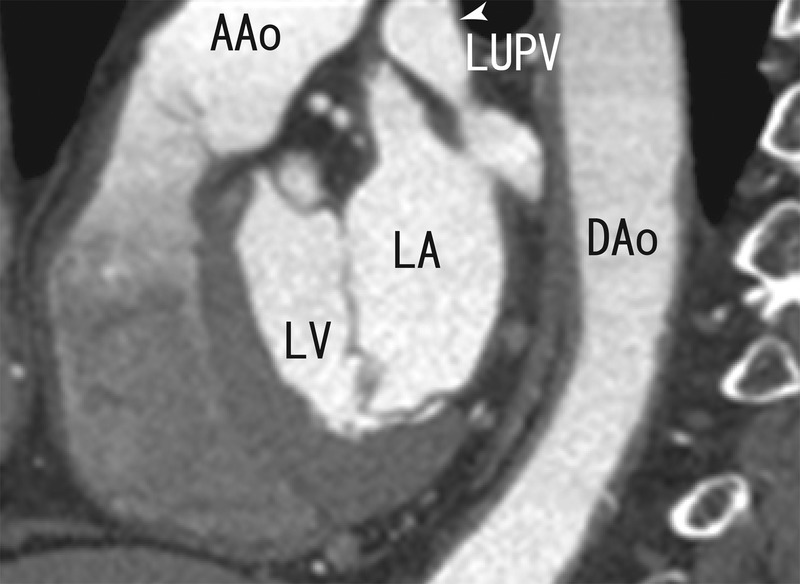
Sagittal images showing the absence of thrombi in the left upper pulmonary vein (white arrowhead). AAo, ascending aorta; DAo, descending aorta; LA, left atrium; LUPV, left upper pulmonary vein; LV, left ventricle.
Treatment
Dabigatran (150 mg twice daily).
Discussion
Although we have produced one case report in which warfarin dissolved a small thrombus in a pulmonary vein,4 there are no published data on the treatment of PVT with dabigatran. PVT is rare and often unrecognised because its clinical symptoms are subtle and atypical (eg, chest pain or dyspnoea); nevertheless, it is a potentially life-threatening condition. PVT is a rare complication following lung surgery or catheter ablation. For more than 50 years, patients with AF have been treated with warfarin. LAA resections or occlusions are optional therapies because LAA thrombi can cause ischaemic stroke. PVT may also cause ischaemic stroke; however, PVT often remains undiagnosed and is not routinely treated to prevent stroke.
Warfarin is a traditional oral thromboprophylactic anticoagulation treatment. It reduced AF-related stroke by 64% in a large meta-analysis2; however, its mechanism of action is not fully understood. Dabigatran is a new oral anticoagulant that acts by specifically and directly blocking the activity of thrombin, the enzyme primarily responsible for thrombus formation. The efficacy of dabigatran has been reported,3 but its mechanism of action is unclear. Whether dabigatran could dissolve a pulmonary vein thrombus was previously unknown.
In the present case, dabigatran successfully dissolved a pulmonary vein thrombus. To the best of our knowledge, this study is the first to show that dabigatran possesses such a capacity. Schmitt and Burg employed CT pulmonary angiography (CTPA) using a 64-MDCT scan to identify PVT in patients without lung cancer, thoracic surgery or catheter ablation; after 10 days, anticoagulant therapy dissolved the thrombi.5 Figure 1 appears to depict a filling defect in the right inferior pulmonary vein (A). However, the report by Schmitt and Burg is not reliable. In their case, the patient had right-sided pulmonary arterial emboli (PE), which appeared to prevent blood flow into the inferior branch. Therefore, the inferior portion of the right lung may have lacked arterial blood and pulmonary vein blood, which may have appeared to be a thrombus in figure 1. The lack of arterial blood and the poor contrast enhancement may have affected the visualisation of the right inferior pulmonary vein, promoting the formation of artefacts. Ten days of anticoagulant treatment improved PE and blood flow restarted in the pulmonary artery and the pulmonary vein, which was observed like dissolution of a thrombus in the right lower pulmonary vein. RLPV and LAA were similar in appearance, and there seemed to be horizontal line in the heart; such a line can be caused by the patient breathing during the examination. Both these images should be considered artifacts, which were created by the lack of artery blood and contrast medium through PE. These defects in the pulmonary vein due to the lack of blood will be observed in patients with PE. Schmitt and coworkers give us the important lesson that we should pay attention to the effects of PE when we assess the defects of contrast-enhancement in the pulmonary vein.
Cardioversion (electric and pharmacological) is associated with an increased risk of thromboembolic events in patients with AF. In cases of inadequate anticoagulation, the risk of thromboembolic events is greater (5–7%). Therapeutic anticoagulation for 48 h for at least 3 weeks before and 4 weeks after cardioversion is recommended for patients with AF; this treatment significantly reduces the risk of thromboembolic events (0.7–0.8%). By combining anticoagulant treatment and diagnostic 64-MDCT scans to prevent thromboembolic events before cardioversion, the risk of thromboembolic events might be greatly reduced. In the present case, the thrombus in the left upper pulmonary vein dissolved. After the complete dissolution of the thrombus, the risk of systemic embolism might have been minimal. Larger studies of AF patients taking dabigatran are needed to determine whether the procedure reduces the risk of cardioembolic events.
In 2013, we reported a completely occluded pulmonary vein thrombus that caused pulmonary vein hypoxia and undernourishment. The effects of pulmonary vein thrombi are unclear but can activate some transcription factors such as hypoxia inducible factor-1 (HIF-1), which is associated with reprogramming cancer cells and embryonic stem cells. These hypoxic changes may drive pulmonary vein myocardium on the pulmonary vein wall, which progresses and maintains AF. But dissolving the thrombus could prevent such changes. We must employ a more systematic approach to analyse the effects on pulmonary vein thrombi of anticoagulants such as dabigatran. Studies should include a prospective design to assess the effects of pulmonary vein thrombi on the pulmonary vein in patients with PVT. Alternatively, a genetic analysis should be conducted to assess how gene regulation in pulmonary vein thrombi affects pulmonary vein myocardium formation.
Learning points.
The main finding of this study was that 3 months of dabigatran treatment dissolved a pulmonary vein thrombus (PVT), as assessed by 64-MDCT imaging performed before and after treatment.
This study is the first to demonstrate that dabigatran may be an effective anticoagulant for treating PVT.
This study suggests that dabigatran may be a good choice for anticoagulant treatment in patients with PVT to prevent thromboembolic events. It also suggests that 64-slice multidetector CT (64-MDCT) scan could be used to diagnose PVT and to assess anticoagulant efficacy.
Large-scale prospective studies are needed to assess the efficacy of dabigatran for treating PVT and preventing thromboembolic events.
Additional studies are also needed to determine the efficacy of a routine 64-MDCT as a diagnostic and assessment tool in patients at high risk of developing PVT and thromboembolic events.
Footnotes
Contributors: This work was performed by HT.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kim NH, Roldan CA, Shively BK. Pulmonary vein thrombosis. Chest 1993;2013:624–6 [DOI] [PubMed] [Google Scholar]
- 2.Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med 2007;2013:857–67 [DOI] [PubMed] [Google Scholar]
- 3.Rasmussen LH, Larsen TB, Graungaard T, et al. Primary and secondary prevention with new oral anticoagulant drugs for stroke prevention in atrial fibrillation: indirect comparison analysis. BMJ 2012;2013:e7097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Takeuchi H. A thrombus of the right upper pulmonary vein: detection by the use of a 64-MDCT. BMJ Case Rep. Published Online: 14 Sept 2012. doi:10.1136/bcr.12.2011.5446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmitt ER, Burg MD. More than just another pulmonary embolism. West J Emerg Med 2012;2013:98–9 [DOI] [PMC free article] [PubMed] [Google Scholar]


