Abstract
Situs inversus totalis is a rare autosomal recessive disorder which can cause diagnostic confusion in a lot of clinical conditions including calculous cholecystitis due to the reversed anatomical positions of abdominal viscera. Laparoscopic cholecystectomy is much more challenging in the presence of this disorder due to loss of usual orientation. We present a case of a 43-year-old woman who was diagnosed at our centre to have calculous cholecystitis in the presence of situs inversus totalis. Laparoscopic cholecystectomy was performed safely after adjustment of the positions of the team inside the operative theatre and of the port sites. The patient tolerated the operation very well and was discharged home after 24h. On follow-up visit the patient was doing very well and completely free of symptoms.
Background
Situs inversus is a rare autosomal recessive disorder which refers to a spectrum of mirror image transpositions of the thoracic viscera, abdominal viscera, or both, and is present in approximately 1 in 5000–20 000 live-births.1
It may be total including abdominal and thoracic viscera, known as situs inversus totalis or it may be partial known as situs inversus partialis. The transposition of the organs may be associated with other congenital anomalies, such as renal dysplasia, biliary atresia, congenital heart disease or pancreatic fibrosis. Situs inversus totalis associated with bronchitis, chronic sinusitis and deficient trachea-bronchial cilia is known as the Kartagener's syndrome.2 3
Situs inversus is not a risk factor for cholelithiasis by itself, but it carries a risk of diagnostic confusion since the symptoms and signs will be misleading as they are arising from abnormally positioned gallbladder especially in patients in whom the diagnosis of situs inversus have not been made yet, and a delay in the diagnosis is expected. In a patient who is already a known case of situs inversus, there will be a high index of suspicion and the diagnosis will be readily made. Laparoscopic cholecystectomy remains the gold standard for symptomatic cholelithiasis even in the presence of situs inversus.
Case presentation
We present a 43-year-old woman, who was diagnosed 5 years ago to have dextrocardia by a chest X-ray performed for an attack of pneumonia. She presented to us with a 3-month history of vague upper abdominal pain and flatulent dyspepsia. The pain was mainly felt in the epigastric region and was radiating to the back, mainly felt after heavy meals. She had no vomiting, fever, jaundice or weight loss. She never had investigations for her condition before. On examination the patient did not have jaundice, abdominal examination was negative apart from tenderness at the epigasric and left upper quadrant. To be mentioned, the apex beat was felt on the right side of the chest.
Investigations
Laboratory investigations including liver function tests were normal. Chest X-ray (figure 1), ECG and echocardiography confirmed the previous diagnosis of dextrocardia. Ultrasonography demonstrated that the liver was located mainly on the left side of the abdomen and the spleen on the right. The gallbladder, filled with multiple gall stones, located on the left side. The bile ducts were normal. CT scan of the abdomen (figures 2 and 3) and chest confirmed the diagnosis of situs inversus totalis.
Figure 1.

Chest X-ray of the patient demonstrating dextrocardia.
Figure 2.

CT scan coronal section demonstrating the liver located in the left side of the abdomen.
Figure 3.
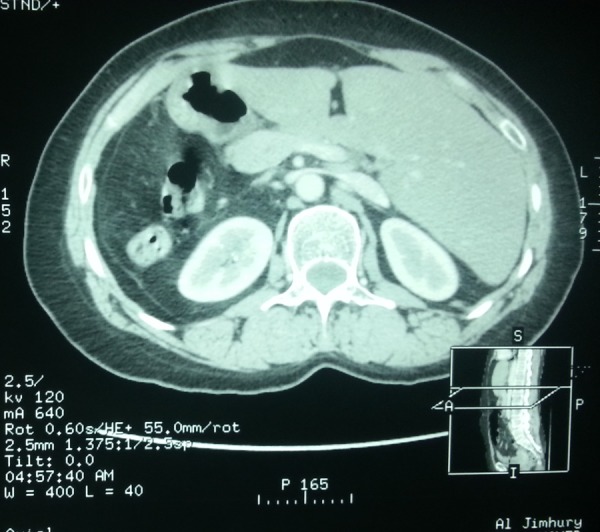
CT scan axial section demonstrating the liver located in the left side of the abdomen.
Treatment
The patient was scheduled for elective laparoscopic cholecystectomy. We adjusted the condition of the theatre and of the team in order to perform this unusual surgery. The monitor was placed near the head of the patient to the left side (figure 4). The surgeon was on the right side of the patient together with the camera assistant and the second assistant stood on the left side. We placed a 10 mm port at the infraumbilical region through which the abdominal cavity was isufflated with carbon dioxide to 14 mm Hg and was used later on for the camera and for extraction of the gallbladder, another 10 mm port was placed on the left side of the abdomen at the midclavicular line below the costal margin, this port was the operating port through which the surgeon used his right hand for dissection. A 5 mm port was placed on the right side of the abdomen at the midclavicular line, almost the same level as the 10 mm port on the left side, this was used by the left hand of the surgeon for retraction of the infundibulum. Another 5 mm port was placed on the left side of the abdomen at the anterior axillary line and was used by the second assistant for caudal traction of the fundus of the gallbladder. The situs inversus was confirmed, the stomach and spleen were on the right side and the liver and gallbladder were on the left side (figure 5 and 6). The dissection was carried out using electrocautery with the right hand of the surgeon while the assistant was applying traction to the fundus. After achieving a clear view of safety of the triangle of Calot, the cystic duct and artery were clipped and the gallbladder dissected away from the liver bed and extracted safely (video 1). The total duration of the procedure was 70 min.
Figure 4.
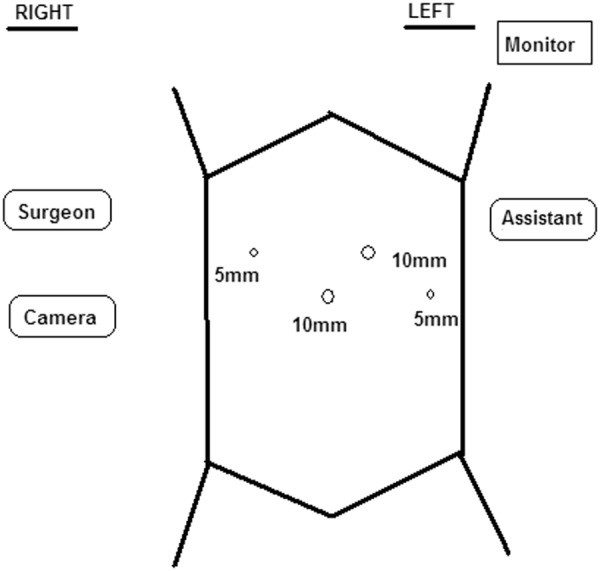
The adjustment of the positions of the team in the theatre and of the port sites.
Figure 5.
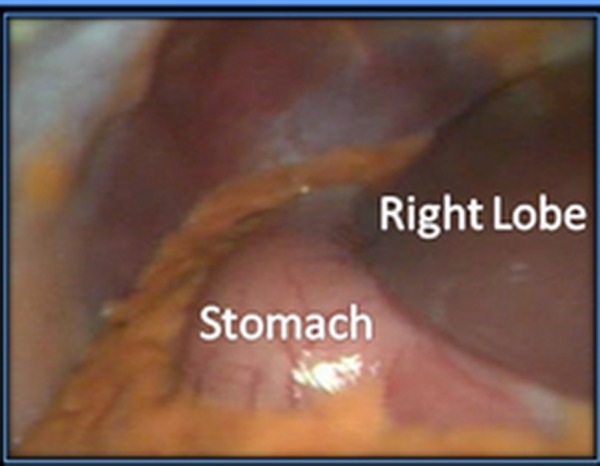
A laparoscopic view showing the stomach in the right side of the peritoneal cavity.
Figure 6.
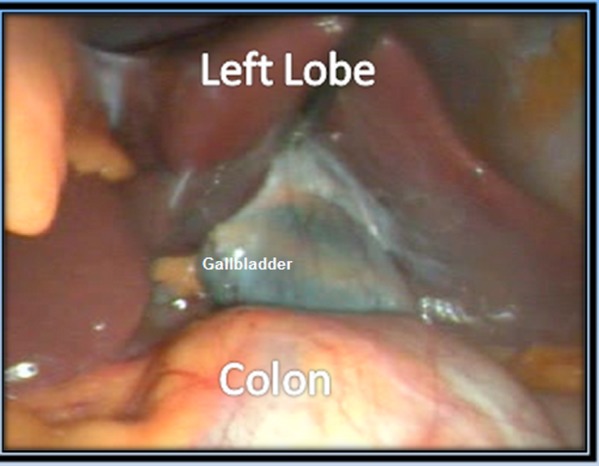
A laparoscopic view showing the gallbladder in the left side of the peritoneal cavity.
Short laparoscopic video demonstrating the heart beating in the right side of the diaphragm, the presence of the spleen and the stomach in the right side of the peritoneal cavity and the gallbladder in the left side.
The patient tolerated the operation very well and was discharged home after 24 h. On follow-up visit the patient was doing very well and completely free of symptoms. Histopathological examination of the specimen revealed chronic calculous cholecystitis.
Discussion
Until now, there is no evidence to suggest that patients with situs inverus totalis are more prone to cholelithiasis . The first reported case of laparoscopic cholecystectomy in a patient with situs inversus totalis was by Campos and Sipes.3
In our search, we found 41 reports about laparoscopic cholecystectomy in patients with situs inversus. All reports documented that situs inversus is not a contraindication for laparoscopy and that the procedure can be performed safely by an experienced laparoscopic surgeon.
Pitiakoudis et al4 on 2005 reviewed 22 reports concerning 25 patients with situs inversus and cholelithiasis, who had laparoscopic cholecystectomy, seven of them were men and 18 women, aging from 20 to 80-year-old. He reported that laparoscopic cholecystectomy, laparoscopic exploration of the common bile duct, intraoperative cholangiography and additional appendectomy were successful in all cases, with none of the patients exhibiting postoperative complications.4
Our patient presented to us with epigastric pain only. According to Rao et al,5 30% of patients reported with situs inversus and cholecystitis presented with epigastric pain only, this was the same finding by McKay and Blake6 and Eisenberg,7 while 10% of patients had right upper quadrant pain also.5 In the rest, the pain was felt mainly in the left upper quadrant or epigastric as well as left side. Due to this unusual pattern of pain, it is fairly understood that patients who have not been diagnosed before to have situs inversus will have delay in the diagnosis of gall stones disease. Our patient was a known case of dextrocardia, that’s why we were highly suspecting the diagnosis of situs inversus totalis. Ultrasonography and CT scan were diagnostic (figures 2 and 3).
It has been documented that laparoscopic cholecystectomy in patients with situs inversus can be performed safely by adjusting ports placement to accommodate for a right-handed surgeon.6 Some authors preferred using the left hand in dissection to perform the operation in a complete mirror image to the conventional laparoscopic technique.3 8–11 In that case ,the umbilical and epigastric 10 mm ports remain the same, but the two 5 mm ports will be on the left side of the abdomen instead of the right side .This of course prefers a left-handed surgeon. We chose to adjust the site of the ports and the standing of the team in order to perform the operation with the right hand (figure 4). The surgeon stood on the right side together with the camera man, while the second assistant stood on the left. This is exactly the reverse of our standard. We put the infraumbilical port in the usual way, after creating the pneumoperitoneum and examining the peritoneal cavity carefully, we put the second 10 mm port on the left side of the abdomen at the mid-clavicular line below the costal margin, this port was the operating port through which the surgeon used his right hand for dissection, that is to say, this replaced the epigastric port in our standard technique. A 5 mm port was placed on the right side of the abdomen at the mid-clavicular line, almost the same level as the 10 mm port on the left side, this was used by the left hand of the surgeon for retraction of the infundibulum. Another 5 mm port was placed on the left side of the abdomen at the anterior axillary line and was used by the second assistant for caudal traction of the fundus of the gallbladder. Our dissection was not difficult, although it was careful and slower than usual because of the mirror image of organs.
The surgeon can use any of the two methods, or any other configuration he or she prefers, the main point is that the principles of dissection of the triangle of Calot should be always followed and the critical view of safety should be always achieved before clipping or cutting any structure.
We were able to perform the procedure safely although it took us 70 min, which is longer than our standard duration (55 min), but we think that the delay in such an unusual case is fairly justified.
One last point deserves attention that the surgeon should always exclude other serious congenital malformations that might be associated with situs inversus totalis especially congenital heart disease, renal problems and of course biliary malformations like atresia before embarking on the surgery for such unusual patients.
Learning points.
Situs inversus totalis is a rare autosomal recessive disorder which can cause diagnostic confusion in a lot of clinical conditions including calculous cholecystitis due to the reversed anatomical positions of abdominal viscera.
Laparoscopic cholecystectomy is much more challenging in the presence of this disorder due to loss of usual orientation.
The surgeon can choose any configuration of the ports he or she prefers, the main point is that the principles of dissection of the triangle of Calot should be always followed and the critical view of safety should be always achieved before clipping or cutting any structure.
The surgeon should always exclude other serious congenital malformations that might be associated with situs inversus totalis before embarking on the surgery for such unusual patients.
Footnotes
Contributors: MSA is the surgeon of the case. SMA is the second surgeon and the author of manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Bohun CM, Potts JE, Casey BM, et al. A population-based study of cardiac malformations and outcomes associated with dextrocardia. Am J Cardiol 2007;2013:305–9 [DOI] [PubMed] [Google Scholar]
- 2.Nursal TZ, Baykal A, Iret D, et al. Laparoscopic cholecystectomy in a patient with situs inversus totalis. J Laparoendosc Adv Surg Tech 2001;2013:239–41 [DOI] [PubMed] [Google Scholar]
- 3.Campos L, Sipes E. Laparoscopic cholecystectomy in a 39-year old female with situs inversus. J Laparoendosc Surg 1991;2013:123–6 [DOI] [PubMed] [Google Scholar]
- 4.Pitiakoudis M, Tsaroucha AK, Katotomichelakis M, et al. Laparoscopic cholecystectomy in a patient with situs inversus using ultrasonically activated coagulating scissors. Report of a case and review of the literature. Acta Chir Belg 2005;2013:114–17 [PubMed] [Google Scholar]
- 5.Rao PG, Katariya RN, Sood S, et al. Situs inversus totalis with calculus cholecystitis and mucinous cystadenomas of ovaries. J Postgrad Med 1977;2013:89–90 [PubMed] [Google Scholar]
- 6.McKay D, Blake G. Laparoscopic cholecystectomy in situs inversus totalis: a case report. BMC Surg 2005;2013:5–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eisenberg D. Cholecystectomy in situs inversus totalis: a laparoscopic approach. Int Med Case Rep J 2009;2013:27–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wood GO, Blalock A. Situs inversus totalis and disease of the billiary tract. Arch Surg 1940;2013:885–96 [Google Scholar]
- 9.Crosher RF, Harnarayan P, Bremner DN. Laparoscopic cholecystectomy in situs inversus totalis. J R Coll Surg Edinb 1996;2013:183–4 [PubMed] [Google Scholar]
- 10.Al-Jumaily M, Achab M, Hoche F. Laparoscopic cholecystectomy in situs inversus totalis: is it safe? J Laparoendosc Adv Surg Tech 2001;2013:229–31 [DOI] [PubMed] [Google Scholar]
- 11.Goh P, Tekant Y, Shang NS, et al. Laparoscopic cholecystectomy in a patient with empyema of the gallbladder and situs inversus. Endoscopy 1992;2013:799–800 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Short laparoscopic video demonstrating the heart beating in the right side of the diaphragm, the presence of the spleen and the stomach in the right side of the peritoneal cavity and the gallbladder in the left side.


