Abstract
The role of a bladder neck sparing (BNS) technique in radical prostatectomy (RP) remains controversial. The potential advantages of improved functional recovery must be weighed against oncological outcomes. We performed a literature review to evaluate the current knowledge regarding oncological and functional outcomes of BNS and bladder neck reconstruction (BNr) in RP. A systematic literature review using on-line medical databases was performed. A total of 33 papers were identified evaluating the use of BNS in open, laparoscopic and robotic-assisted RP. The majority were retrospective case series, with only one prospective, randomised, blinded study identified. The majority of papers reported no significant difference in oncological outcomes using a BNS or BNr technique, regardless of the surgical technique employed. Quoted positive surgical margin rates ranged from 6% to 32%. Early urinary continence (UC) rates were ranged from 36% to 100% at 1 month, with long-term UC rate reported at 84-100% at 12 months if the bladder neck (BN) was spared. BNS has been shown to improve early return of UC and long-term UC without compromising oncological outcomes. Anastomotic stricture rate is also lower when using a BNS technique.
Keywords: Bladder neck reconstruction, bladder neck sparing, lissosphincter, radical prostatectomy, rhabdosphincter
INTRODUCTION
‘The three goals of radical prostatectomy (…) are cancer control, preservation of urinary control, and preservation of sexual function’.[1] As the techniques of RP have evolved, our understanding of the relevant anatomy has improved and better oncological and functional outcomes have been reported. Despite this, there remains no consensus on operative technique and there remain many technical components of the procedure itself where controversy exists. One such contentious area is the role of bladder neck sparing (BNS) versus bladder neck reconstruction (BNr) and the impact of both techniques on oncological and functional outcomes. Those in favour of BNS suggest this technique allows earlier return of continence and a lower incidence of post-operative strictures, without compromising oncological clearance.[2] Surgeons who favour BNr state concerns about compromising surgical margins with no definitive improvement in functional outcome.[3] BNS has been incorporated into open RP (ORP), laparoscopic RP (LRP) and robot-assisted laparoscopic prostatectomy (RALP) techniques. Technical aspects of BNS vary between the surgical approaches because of the technical difficulties this can present and the prolonged learning curve.[4,5,6] Circumferential, anterior and lateral approaches to the have all been described in ORP, LRP and RALP.[7,8,9,10,11,12]
Improved surgical techniques and appreciation of the local anatomy have seen huge modifications to the technique of RP since the first described procedure by Proust in 1901.[13] Preservation of the neurovascular bundle was first reported in 1983 by Walsh et al. and since then, sparing of suspensory mechanism of the urethra[11,14] preservation of urethral length[15,16] posterior rhabdosphincter sparing,[17] BNS[18] and seminal vesicle sparing[19] have all been described as important techniques for optimising functional outcome after RP. BNS has evolved from a better understanding of the anatomy and physiology of mechanisms of UC. New research based on embryological, 3D imaging and urodynamic studies have redefined our understanding of the urinary sphincter mechanism. We now understand the contributions of the BN as an integral part of larger, complex sphincter mechanism that consists of both striated and smooth muscle fibres,[20] rather than an independent external (rhabdo) and internal (lisso) sphincter as previously thought. The rhabdosphincter is horseshoe-shaped and overlies the circular and longitudinal smooth muscle of the urethra. During periods of increased intra-abdominal pressures it contracts and coapts the urethra.[20,21] Due to the relatively low volume of slow twitch muscle fibres compression of the rhabdosphinter cannot be sustained for longer than about 60 s.[21] During the storage phase, the lissosphincter maintains urethral resistance and is the primary mechanism responsible for maintaining resting and baseline continence. Urodynamics studies have demonstrated that an intact lissosphincter maintains continence in the absence of a viable rhabdosphincter.[20,22] BNS technique aims to leave most of the lissosphincter mechanism intact allowing preservation of its function.
We performed a search of the PubMed, Science Direct and Wiley library databases to identify original and review articles in English which addressed BNS and BN reconstruction techniques, oncological and functional outcomes of ORP, LRP and RALP, where BNS technique was used. The search terms used were BN, spare, preservation, reconstruction, urinary incontinence, positive margin, ORP, LRP and RALP. Abstracts and reports from meetings were not included. Relevant articles were reviewed, analyzed and summarized in line with the intentions of this review article. Our initial online database search returned 345 results; 133 via Science Direct, 122 via PubMed and 90 via Wiley library. We further evaluated significant articles found in the citation lists. After narrowing the search down to the relevant papers, current review included 12,806 patients in 31 original studies plus further two review articles directly pertinent to the topic of BNS and BNr. There are 19 studies describing outcomes of BNS in ORP included in the review, six studies on BNS in LRP and five original articles on outcomes of BNS in RALP. The only prospective, randomised study included patients undergoing both RALP and ORP (level of evidence 1b). Remaining studies are non-randomised prospective and retrospective studies with varying population size sample (level of evidence 2-4).
Oncological outcomes
The relationship between BNS and positive surgical margin (PSM) is well-documented in the literature [Table 1]. However, only one study is a prospective, randomised, blinded study with a control group.[18] Gomez et al. in a prospective study did not find any sole PSM at BN in the cohort of 50 men undergoing ORP and BNS, although there were six patients (12%) who had multiple positive margins involving BN.[23] Wood et al. and Lepor et al. performed studies involving intraoperative biopsies of the BN after BNS.[24,25] Wood demonstrated that all nine patients (12%) who had PSM at the BN had multiple PSM's and T3 disease. This was confirmed further by Braslis et al., Soloway and Neulander.[26,27] Braslis et al. reported there was no sole PSM at BN after ORP and 7.5% patients had PSM at the BN, which were multiple PSM's.[26] Soloway and Neulander found only 1% sole PSM at BN. In his study of 676 patients, 4.3% patients had multiple PSM also involving BN.[27] In the series of 365 patients undergoing ORP Shelfo et al. reported total PSM rate at 32%, but only two patients had sole BN PSM.[28] Similarly, Poon et al. in the retrospective cohort study of 220 men concluded no statistical difference between patients undergoing BNS versus the control group.[2] As described by Bianco et al. in the larger prospective studies of 555 men undergoing ORP, total PSM was 32% with 13% PSM at BN and 0.36% sole PSM at BN.[29] More recently Freire et al., in a series of 619 men undergoing RALP, assessed PSM rate at the base of the prostate in the BNS versus control group.[30] Rates were 1.4% and 2.2% respectively. Similarly, Friedlander et al. in a retrospective evaluation of a large cohort of over 1000 men demonstrated identical PSM for BNS and control group, which was 13.8%.[31] In a new prospective, randomised, controlled and blinded study from the Heidelberg group, only 2% of BNS group had a sole PSM at the BN compared with 12.5% PSM rate in the control group.[18] Contrary to the above, Srougi et al. published results of their prospective study, where they ceased recruitment after 70 patients as the PSM rate was 10%, all being at the BN irrespective of the group.[3] In LRP, Katz et al. published results of the series, where overall PSM was 26% and PSM at BN as 9.75%.[32] During the study, they abandoned BNS approach and decreased PSM at BN to zero. Several studies stressed that appropriate patient selection is crucial in order not to compromise the surgical outcome.[12,28,33,34,35]
Table 1.
Oncological outcomes of BNS
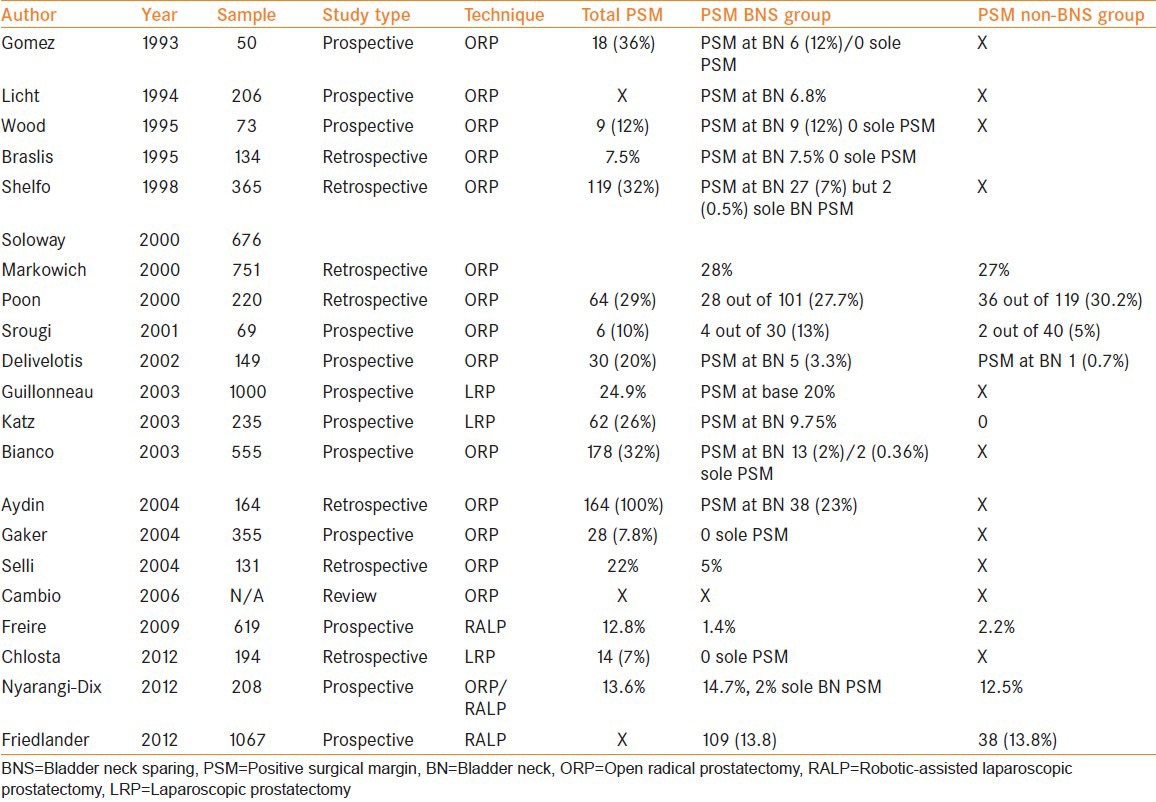
High Gleason score on the prostatic biopsies or suspicion of extra-prostatic extension increases the risk of PSM at the BN.[12,28,35] Aydin et al. described the significance of a sole PSM at the BN.[36] In his retrospective study of 164 men with PSM after ORP, 23% had sole PSM at the BN. Those patients had 69.8% 5-year actuarial risk of biochemical progression compared with 33% who had negative BN margin. The data highlights that the presence of a PSM at the BN has a significant impact on long-term outcomes. Both Marcovich et al. and Aydin et al. have found that a PSM at the BN results in higher rates of biochemical recurrence when compared with single or multiple PSM at other sites.[35,36] However, in 2010, Pierorazio et al. published the results of large review on over 17,000 patients.[37] PSM rate at the BN was only 1.2%. Patients with an isolated PSM at the BN had prostate specific antigen (PSA) free survival rate of 37% and cancer free survival of 92%, which was comparable to prognosis of patients with a seminal vesicle invasion and an extracapsular extension respectively. They concluded that American Joint Committee on Cancer should reconsider BN involvement staging as T4.
Assessing long-term oncological outcomes, we were able to identify only four studies where biochemical recurrence-free survival (BCRFS) in BNS cohorts was compared with non-BNS cohort.[16,29,31,34] Remaining data comes from prospective and retrospective single arm studies. Friedlander et al. assessed PSA, surgical margin status and pathological stage and grade and demonstrated no difference in BCRFS between BNS and control groups with a follow-up period of up to 72 months (hazard ratio 1.20, 95% confidence interval 0.62-2.31, P = 0.596). Similarly, in their prospective, controlled study, Bianco et al. reported that during 7-year of follow-up, BNS did not compromise disease free survival (DFS). Univariable and multivariable analyses of PSM at BNS was not a statistically important factor for DFS. Licht et al. also assessed DFS between BNS and non-BNS groups and showed no statistical difference. Gaker et al. reported that at 5.2-year follow-up, 90% of BNS group had a PSA of less than 0.2 mcg/L and 80% of the non-BNS group had a PSA of less than 0.2 mcg/L at 12.5-year of follow-up.
Functional outcomes
Urinary continence
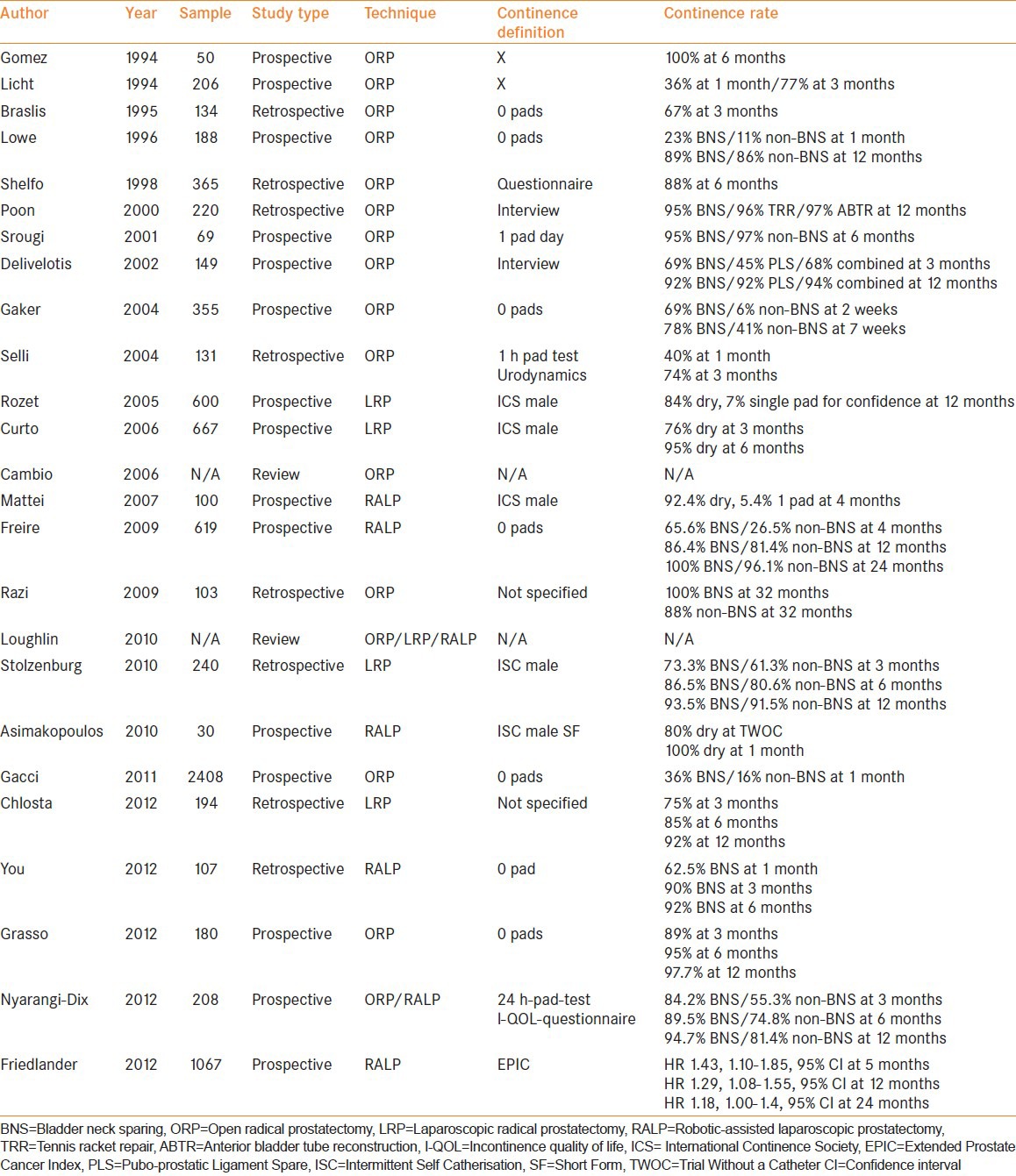
Post-operative return to UC is similar in the reported ORP, LRP and RALP series. Where the BN was preserved UC varies between 36% and 100% at 1 month and 84% to 100% at 12 months follow-up. Table 2 summarises the relevant studies. As with the assessment of oncological outcomes, only one study provides 1b level of evidence. The remaining studies constitute level of evidence 2-4. The method of assessment of UC post-RP has always been controversial and there is no consensus definition.[38] In a prospective study Lowe defined UC as usage of zero pads per day. In his series, UC at 1 month was 23% in the BNS group and 11% in the non-BNS group were continent, which was statistically significant.[39] Long-term UC was similar, 89% and 86% BNS and non-BNS cohorts respectively. Shelfo et al. reported a similar rate of post-operative UC of 88% at 6 months.[28] Connolly et al. studied continence in patients undergoing ORP and bladder BNr (anterior bladder tube reconstruction [ABTR] vs. tennis racket repair [TRR]).[40] Pre-and post-operative urodynamics studies were performed to evaluated continence parameters. All patients were continent post-operatively at 3 months. Differences in maximal urethral closing pressures were the only statistically significant findings between both groups post-operatively. Following analysis, preservation of functional urethral length was significantly longer in patients undergoing ABTR. The authors concluded that preservation of urethral length may promote UC post-ORP. Furthermore, Poon et al. compared outcomes of BNS with ABTR and TRR.[2] At intervals of 1 week, 4 weeks, 3 months, 6 months and 12 months there was no statistical difference in UC among those groups. No significant difference in UC at 6 months was noted by Srougi et al., however, due to the high prevalence of PSM at the BN recruitment to the study was halted pre-maturely.[3] A significant improvement in UC post-BNS was reported by Gaker and Steel, and Deliveliotis et al.[16,41] In both prospective studies, early return of UC in BNS groups was noted compared to control groups, which was statistically important. In 2004 Selli et al. reported similar results from their series.[42] The study of 600 patients undergoing LRP reported a return to UC at 12 months at 84%.[43] Similar results were reported by Bordeaux[10] Leipzig[44] and Warsaw[45] groups. In our institution, we performed a retrospective analysis of 559 LRP. BNS was associated with a statistically insignificant faster recovery of UC at 3 months and statistically significant difference in UC at 12 months between BNS and non-BNS groups, 94.9% and 80.1%, respectively using one pad or less as a definition of continence. More recently, studies aiming at evaluation of BNS technique in RALP have been published. Freire et al. reported significantly better early UC in BNS group versus non-BNS group at 65.6% and 26.5% respectively.[30] At 2-year follow-up, there was no statistical difference between BNS and non-BNS groups and was 100% and 96.1%, respectively. In 2012 Friedlander et al., in a large retrospective cohort of 1067 men showed a significant improvement in early UC between BNS and control groups particularly at 5 and 12 months follow-up.[31] In another study, You et al. compared functional outcomes of RALP with BNS and BNS plus posterior urethral reconstruction (PUR);[46] however, their study was performed retrospectively on a relatively small sample. Nevertheless, it demonstrated a significant improvement in return to UC between a control and PUR groups and control and BNS-PUR groups. There was no significant advantage of BNS plus PUR technique over PUR alone. The authors concluded that PUR and BNS are related with improved UC post-RALP. The only prospective, randomised, controlled, blinded study comes from the Heidelberg group.[18] They demonstrated a significant early return of UC at 4 months follow-up. 84.2% of patients with BNS were continent compared with 55.3% in non-BNS procedure. Similarly at 12 months, the difference in UC was statistically significant and rates were 94.5% and 81.4% for BNS and non-BNS groups. Moreover, in the multiple logistic regression analysis BNS was an independent positive predictor of UC.
Table 2.
Functional outcomes post-BNS
Anastomotic strictures
Gomez et al. were reported that neo vesico-urethral anastomosis stricture rate were lower in BNS group compared with the non-BNS group.[23] Licht et al. confirmed a similar association.[34] Subsequent literature consistently supported these findings and currently there is an agreement that stricture rate post-BNS is relatively lower than in patients not undergoing BNS. Shelfo et al quoted 1% stricture rate in their study.[28] Poon et al. reported BN stricture at 5% for BNS and 11-18% for BNr techniques.[2] Gaker and Steel in 2004 reported that 2.9% of BNS patient had an anastomotic stricture.[16] Other studies present similar findings.[26,41,47] In 2004, Besarani et al. demonstrated that strictures occur mostly within 3 months post-surgery (75%) and are less frequent after 12 months from surgery (5%).[48] Freire et al. reported 1.1% anastomotic strictures in BNS compared with 0.7% in a control group.[30] More recently, the Heidelberg group did not observe the occurrence of any BN strictures post-RP in either BNS and control groups.[18]
Available evidence suggests that BNS technique is likely to be superior to non-BNS for preventing anastomotic strictures. However, most of evidence comes from non-randomised trials hence level of evidence is relatively low.
DISCUSSION
There is a growing body of literature on the role of BNS in RP, although outcome data is still mainly based on non-randomised, prospective and retrospective studies with variable sample size (level 2-4 evidence). Only one randomised, controlled, blinded study has been performed to date (level 1b). In the studies reviewed, PSM rates varied between 6% and 32%. Two series reported on the negative impact of BNS on the PSM. Katz et al. in his prospective series reported that after abandoning the BNS technique the PSM rate dropped by 9.75%, however, total PSM rate was still 26%.[32] Those findings were not confirmed by other studies, which documented that PSM did not negatively correlate with BNS technique. Moreover, newer, larger review postulates that sole PSM at BN is very rare (1.2%) and if present confers 12-year cancer free survival of 92%.[37] Some studies discussed the issue of indications and contra-indications for BNP technique.[12,28,33,34,35] While there is no agreement, it appears that the only absolute contraindication is high risk disease which increases the risk of PSM involving BN. A relative contraindication is a previous pelvic or transurethral prostate surgery as this may increase technical intraoperative difficulties. Some authors postulate additional investigations pre-operatively such as additional bladder base biopsies, pre-operative magnetic resonance imaging, and biopsies of the spared BN. The only randomised, prospective study on the subject concluded that BNS does not negatively impact oncological outcomes.[18] The sole PSM rate at BN was only 2% compared with total PSM rate being 13.6%.
This study also reported objective and subjective assessment of UC and demonstrated that BNS enables early return of UC and long-term UC. In the remaining studies included in our review, varying definitions of UC were used and therefore comparative analysis is not feasible. Two studies in the current review don’t contain information on continence definition applied.[45,47]
Lowe et al. defined UC as zero pads per day[39] while Srougi et al.'s definition was 1 pad/day.[3] Other series used an open interview as a method of assessment of UC without any validated questionnaires. More recently International Continence Society (ICS) male and ICS male short-form were utilised by others. Available data uniformly shows that UC rates post-RP with BNS are at least as good as post non-BNS and it is very likely that BNS expedites early return of UC and improves long-term UC.
CONCLUSION
With changes in surgical technique, BNS has been increasingly incorporated into the RP. Evidence summarised in this review demonstrates that BNS technique leads to early return of UC and long-term UC without compromising oncological outcomes. Anastomotic stricture rate is lower when using BNS technique. BNS is superior to non-BNS techniques and authors of this review postulate application of the method in feasible cases. High risk prostate cancer cases must be considered separately.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Schaeffer EM, Partin AW, Lepor H, Walsh PC. Cambbell-Walsh Urology. Tenth edition. Chapter 102. 2012. Radical retropubic and radical prostatectomy; pp. 2801–2829. [Google Scholar]
- 2.Poon M, Ruckle H, Bamshad BR, Tsai C, Webster R, Lui P. Radical retropubic prostatectomy: Bladder neck preservation versus reconstruction. J Urol. 2000;163:194–8. doi: 10.1016/s0022-5347(05)68003-2. [DOI] [PubMed] [Google Scholar]
- 3.Srougi M, Nesrallah LJ, Kauffmann JR, Nesrallah A, Leite KR. Urinary continence and pathological outcome after bladder neck preservation during radical retropubic prostatectomy: A randomized prospective trial. J Urol. 2001;165:815–8. [PubMed] [Google Scholar]
- 4.Ahlering TE, Skarecky D, Lee D, Clayman RV. Successful transfer of open surgical skills to a laparoscopic environment using a robotic interface: Initial experience with laparoscopic radical prostatectomy. J Urol. 2003;170:1738–41. doi: 10.1097/01.ju.0000092881.24608.5e. [DOI] [PubMed] [Google Scholar]
- 5.Menon M, Tewari A, Peabody JO, Shrivastava A, Kaul S, Bhandari A, et al. Vattikuti institute prostatectomy, a technique of robotic radical prostatectomy for management of localized carcinoma of the prostate: Experience of over 1100 cases. Urol Clin North Am. 2004;31:701–17. doi: 10.1016/j.ucl.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 6.Thiel DD, Francis P, Heckman MG, Winfield HN. Prospective evaluation of factors affecting operating time in a residency/fellowship training program incorporating robot-assisted laparoscopic prostatectomy. J Endourol. 2008;22:1331–8. doi: 10.1089/end.2008.0023. [DOI] [PubMed] [Google Scholar]
- 7.Klein EA. Early continence after radical prostatectomy. J Urol. 1992;148:92–5. doi: 10.1016/s0022-5347(17)36519-9. [DOI] [PubMed] [Google Scholar]
- 8.Latiff A. Preservation of bladder neck fibers in radical prostatectomy. Urology. 1993;41:566–7. doi: 10.1016/0090-4295(93)90106-k. [DOI] [PubMed] [Google Scholar]
- 9.Guillonneau B, Vallancien G. Laparoscopic radical prostatectomy: The montsouris technique. J Urol. 2000;163:1643–9. doi: 10.1016/s0022-5347(05)67512-x. [DOI] [PubMed] [Google Scholar]
- 10.Curto F, Benijts J, Pansadoro A, Barmoshe S, Hoepffner JL, Mugnier C, et al. Nerve sparing laparoscopic radical prostatectomy: Our technique. Eur Urol. 2006;49:344–52. doi: 10.1016/j.eururo.2005.11.029. [DOI] [PubMed] [Google Scholar]
- 11.Tewari AK, Bigelow K, Rao S, Takenaka A, El-Tabi N, Te A, et al. Anatomic restoration technique of continence mechanism and preservation of puboprostatic collar: A novel modification to achieve early urinary continence in men undergoing robotic prostatectomy. Urology. 2007;69:726–31. doi: 10.1016/j.urology.2006.12.028. [DOI] [PubMed] [Google Scholar]
- 12.Asimakopoulos AD, Annino F, D’Orazio A, Pereira CF, Mugnier C, Hoepffner JL, et al. Complete periprostatic anatomy preservation during robot-assisted laparoscopic radical prostatectomy (RALP): The new pubovesical complex-sparing technique. Eur Urol. 2010;58:407–17. doi: 10.1016/j.eururo.2010.04.032. [DOI] [PubMed] [Google Scholar]
- 13.Proust R. Technique de la prostatectomie périnéale. Association Francaise d’Urologie. 1901;5:361. [Google Scholar]
- 14.Stolzenburg JU, Schwalenberg T, Horn LC, Neuhaus J, Constantinides C, Liatsikos EN. Anatomical landmarks of radical prostatecomy. Eur Urol. 2007;51:629–39. doi: 10.1016/j.eururo.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 15.Coakley FV, Eberhardt S, Kattan MW, Wei DC, Scardino PT, Hricak H. Urinary continence after radical retropubic prostatectomy: Relationship with membranous urethral length on preoperative endorectal magnetic resonance imaging. J Urol. 2002;168:1032–5. doi: 10.1016/S0022-5347(05)64568-5. [DOI] [PubMed] [Google Scholar]
- 16.Gaker DL, Steel BL. Radical prostatectomy with preservation of urinary continence: Pathology and long-term results. J Urol. 2004;172:2549–52. doi: 10.1097/01.ju.0000144071.24113.1c. [DOI] [PubMed] [Google Scholar]
- 17.Coelho RF, Chauhan S, Orvieto MA, Sivaraman A, Palmer KJ, Coughlin G, et al. Influence of modified posterior reconstruction of the rhabdosphincter on early recovery of continence and anastomotic leakage rates after robot-assisted radical prostatectomy. Eur Urol. 2011;59:72–80. doi: 10.1016/j.eururo.2010.08.025. [DOI] [PubMed] [Google Scholar]
- 18.Nyarangi-Dix JN, Radtke JP, Hadaschik B, Pahernik S, Hohenfellner M. Impact of complete bladder neck preservation on urinary continence, quality of life and surgical margins after radical prostatectomy: A randomized, controlled, single blind trial. J Urol. 2013;189:891–8. doi: 10.1016/j.juro.2012.09.082. [DOI] [PubMed] [Google Scholar]
- 19.Walz J, Burnett AL, Costello AJ, Eastham JA, Graefen M, Guillonneau B, et al. A critical analysis of the current knowledge of surgical anatomy related to optimization of cancer control and preservation of continence and erection in candidates for radical prostatectomy. Eur Urol. 2010;57:179–92. doi: 10.1016/j.eururo.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 20.Koraitim MM. The male urethral sphincter complex revisited: An anatomical concept and its physiological correlate. J Urol. 2008;179:1683–9. doi: 10.1016/j.juro.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 21.Shafik A. A study of the continence mechanism of the external urethral sphincter with identification of the voluntary urinary inhibition reflex. J Urol. 1999;162:1967–71. doi: 10.1016/S0022-5347(05)68080-9. [DOI] [PubMed] [Google Scholar]
- 22.Gudziak MR, McGuire EJ, Gormley EA. Urodynamic assessment of urethral sphincter function in post-prostatectomy incontinence. J Urol. 1996;156:1131–4. [PubMed] [Google Scholar]
- 23.Gomez CA, Soloway MS, Civantos F, Hachiya T. Bladder neck preservation and its impact on positive surgical margins during radical prostatectomy. Urology. 1993;42:689–93. doi: 10.1016/0090-4295(93)90534-h. [DOI] [PubMed] [Google Scholar]
- 24.Wood DP, Jr, Peretsman SJ, Seay TM. Incidence of benign and malignant prostate tissue in biopsies of the bladder neck after a radical prostatectomy. J Urol. 1995;154:1443–6. [PubMed] [Google Scholar]
- 25.Lepor H, Chan S, Melamed J. The role of bladder neck biopsy in men undergoing radical retropubic prostatectomy with preservation of the bladder neck. J Urol. 1998;160:2435–9. doi: 10.1097/00005392-199812020-00013. [DOI] [PubMed] [Google Scholar]
- 26.Braslis KG, Petsch M, Lim A, Civantos F, Soloway MS. Bladder neck preservation following radical prostatectomy: Continence and margins. Eur Urol. 1995;28:202–8. doi: 10.1159/000475052. [DOI] [PubMed] [Google Scholar]
- 27.Soloway MS, Neulander E. Bladder-neck preservation during radical retropubic prostatectomy. Semin Urol Oncol. 2000;18:51–6. [PubMed] [Google Scholar]
- 28.Shelfo SW, Obek C, Soloway MS. Update on bladder neck preservation during radical retropubic prostatectomy: Impact on pathologic outcome, anastomotic strictures, and continence. Urology. 1998;51:73–8. doi: 10.1016/s0090-4295(97)00463-9. [DOI] [PubMed] [Google Scholar]
- 29.Bianco FJ, Grignon DJ, Sakr WA, Shekarriz B, Upadhyay J, Dornelles E, et al. Radical prostatectomy with bladder neck preservation: Impact of a positive margin. Eur Urol. 2003;43:461–6. doi: 10.1016/s0302-2838(03)00103-9. [DOI] [PubMed] [Google Scholar]
- 30.Freire MP, Weinberg AC, Lei Y, Soukup JR, Lipsitz SR, Prasad SM, et al. Anatomic bladder neck preservation during robotic-assisted laparoscopic radical prostatectomy: Description of technique and outcomes. Eur Urol. 2009;56:972–80. doi: 10.1016/j.eururo.2009.09.017. [DOI] [PubMed] [Google Scholar]
- 31.Friedlander DF, Alemozaffar M, Hevelone ND, Lipsitz SR, Hu JC. Stepwise description and outcomes of bladder neck sparing during robot-assisted laparoscopic radical prostatectomy. J Urol. 2012;188:1754–60. doi: 10.1016/j.juro.2012.07.045. [DOI] [PubMed] [Google Scholar]
- 32.Katz R, Salomon L, Hoznek A, de la Taille A, Antiphon P, Abbou CC. Positive surgical margins in laparoscopic radical prostatectomy: The impact of apical dissection, bladder neck remodeling and nerve preservation. J Urol. 2003;169:2049–52. doi: 10.1097/01.ju.0000065822.15012.b7. [DOI] [PubMed] [Google Scholar]
- 33.Cambio AJ, Evans CP. Minimising postoperative incontinence following radical prostatectomy: Considerations and evidence. Eur Urol. 2006;50:903–13. doi: 10.1016/j.eururo.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 34.Licht MR, Klein EA, Tuason L, Levin H. Impact of bladder neck preservation during radical prostatectomy on continence and cancer control. Urology. 1994;44:883–7. doi: 10.1016/s0090-4295(94)80175-4. [DOI] [PubMed] [Google Scholar]
- 35.Marcovich R, Wojno KJ, Wei JT, Rubin MA, Montie JE, Sanda MG. Bladder neck-sparing modification of radical prostatectomy adversely affects surgical margins in pathologic T3a prostate cancer. Urology. 2000;55:904–8. doi: 10.1016/s0090-4295(00)00451-9. [DOI] [PubMed] [Google Scholar]
- 36.Aydin H, Tsuzuki T, Hernandez D, Walsh PC, Partin AW, Epstein JI. Positive proximal (bladder neck) margin at radical prostatectomy confers greater risk of biochemical progression. Urology. 2004;64:551–5. doi: 10.1016/j.urology.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 37.Pierorazio PM, Epstein JI, Humphreys E, Han M, Walsh PC, Partin AW. The significance of a positive bladder neck margin after radical prostatectomy: The American Joint Committee on cancer pathological stage T4 designation is not warranted. J Urol. 2010;183:151–7. doi: 10.1016/j.juro.2009.08.138. [DOI] [PubMed] [Google Scholar]
- 38.Coelho RF, Chauhan S, Palmer KJ, Rocco B, Patel MB, Patel VR. Robotic-assisted radical prostatectomy: A review of current outcomes. BJU Int. 2009;104:1428–35. doi: 10.1111/j.1464-410X.2009.08895.x. [DOI] [PubMed] [Google Scholar]
- 39.Lowe BA. Comparison of bladder neck preservation to bladder neck resection in maintaining postrostatectomy urinary continence. Urology. 1996;48:889–93. doi: 10.1016/s0090-4295(96)00324-x. [DOI] [PubMed] [Google Scholar]
- 40.Connolly JA, Presti JC, Jr, Carroll PR. Anterior bladder neck tube reconstruction at radical prostatectomy preserves functional urethral length — A comparative urodynamic study. Br J Urol. 1995;75:766–70. doi: 10.1111/j.1464-410x.1995.tb07388.x. [DOI] [PubMed] [Google Scholar]
- 41.Deliveliotis C, Protogerou V, Alargof E, Varkarakis J. Radical prostatectomy: Bladder neck preservation and puboprostatic ligament sparing — Effects on continence and positive margins. Urology. 2002;60:855–8. doi: 10.1016/s0090-4295(02)01956-8. [DOI] [PubMed] [Google Scholar]
- 42.Selli C, De Antoni P, Moro U, Macchiarella A, Giannarini G, Crisci A. Role of bladder neck preservation in urinary continence following radical retropubic prostatectomy. Scand J Urol Nephrol. 2004;38:32–7. doi: 10.1080/00365590310017280. [DOI] [PubMed] [Google Scholar]
- 43.Rozet F, Galiano M, Cathelineau X, Barret E, Cathala N, Vallancien G. Extraperitoneal laparoscopic radical prostatectomy: A prospective evaluation of 600 cases. J Urol. 2005;174:908–11. doi: 10.1097/01.ju.0000169260.42845.c9. [DOI] [PubMed] [Google Scholar]
- 44.Stolzenburg JU, Kallidonis P, Hicks J, Do M, Dietel A, Sakellaropoulos G, et al. Effect of bladder neck preservation during endoscopic extraperitoneal radical prostatectomy on urinary continence. Urol Int. 2010;85:135–8. doi: 10.1159/000314842. [DOI] [PubMed] [Google Scholar]
- 45.Chłosta PL, Drewa T, Jaskulski J, Dobruch J, Varkarakis J, Borówka A. Bladder neck preservation during classic laparoscopic radical prostatectomy-point of technique and preliminary results. Wideochir Inne Tech Malo Inwazyjne. 2012;7:89–95. doi: 10.5114/wiitm.2011.25981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.You YC, Kim TH, Sung GT. Effect of bladder neck preservation and posterior urethral reconstruction during robot-assisted laparoscopic radical prostatectomy for urinary continence. Korean J Urol. 2012;53:29–33. doi: 10.4111/kju.2012.53.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Razi A, Yahyazadeh SR, Sedighi Gilani MA, Kazemeyni SM. Bladder neck preservation during radical retropubic prostatectomy and postoperative urinary continence. Urol J. 2009;6:23–6. [PubMed] [Google Scholar]
- 48.Besarani D, Amoroso P, Kirby R. Bladder neck contracture after radical retropubic prostatectomy. BJU Int. 2004;94:1245–7. doi: 10.1111/j.1464-410X.2004.05151.x. [DOI] [PubMed] [Google Scholar]


