Abstract
Background Recruitment rates of general practitioners (GPs) to do research vary widely. This may be related to the ability of a study to incorporate incentives for GPs and minimise barriers to participation.
Method A convenience sample of 30 GPs, ten each from the Sydney intervention and control groups Ageing in General Practice ‘Detection and Management of Dementia’ project (GP project) and 10 GPs who had refused participation, were recruited to determine incentives and barriers to participating in research. GPs completed the 11-item ‘Meeting the challenges of research in general practice: general practitioner questionnaire’ (GP survey) between months 15 and 24 of the GP project, and received brief qualitative interviews from a research GP to clarify responses where possible.
Results The most important incentives the 30 GPs gave for participating in the project were a desire to update knowledge (endorsed by 70%), to help patients (70%), and altruism (60%). Lack of time (43%) was the main barrier. GPs also commented on excessive paperwork and an inadequate explanation of research.
Conclusions While a desire to update knowledge and help patients as well as altruism were incentives, time burden was the primary barrier and was likely related to extensive paperwork. Future recruitment may be improved by minimising time burden, making studies simpler with online data entry, offering remuneration and using a GP recruiter.
Keywords: general practitioner, recruitment, research
Background
General Practitioners (GPs) are usually the first point of contact in Australia's healthcare system.1 With 79% of people regarding GPs as easily accessible and 81% visiting a GP at least once a year,2,3 the number of medical conditions seen and referrals made by GPs have increased steadily.4 Combined with an ageing population, increased life expectancy and chronic illness, GPs are at the front line of disease management and are a logical research population.4
Professional associations and GPs value and encourage research,1,5–7 which can improve primary care's evidence base, patient care and shape policies.8 Despite this, GP recruitment varies from 0.03–90%,9–16 with heavy workloads, time constraints and stress being identifiable barriers.10,12–13,16–18 This variability seems likely to be partially related to the ability of studies to overcome these obstacles and incorporate incentives.
Several factors do potentially increase GPs' research participation. Demographically, GP research participants have been shown to be younger or more recently qualified and to work in preventative health-focused practices.16,19 This may be caused by relatively younger or more enthusiastic GPs having a greater recognition of the importance of research. Practice nurses helping with administrative research tasks also appear to increase participation,20 as do telephone calls prior to receiving a letter about the study, regular visits to the practice by the study coordinator and update newsletters,7,17 suggesting that GPs prefer to be kept informed.
Other incentives include minimising time burden,10 remuneration,7,9 clinically relevant and interesting research topics and personal or telephone recruitment.10,17,21 Recruitment by a fellow or prominent doctor is another incentive,13,21 and studies utilising steering committees of prominent doctors to select ‘liaison doctors’ to perform general recruitment have principally achieved even higher rates.13–15 Endorsements from professional associations have had mixed results.10,12 Helpful strategies, reported by Williamson et al,22 for the recruitment of GPs included the use of an existing database, minor promotion and a letter of invitation, having an appealing topic, minimising time demands and provision of continuing medical education points. Retention was aided by establishing good relationships with GPs and their staff, minimising tasks for participants, providing clear instruction for participation and, if applicable, clear instructions for the use of software.
The Ageing in General Practice ‘Detection and Management of Dementia’ project (GP project) was a multisite randomised controlled trial (RCT) of Australian GPs using academic detailing to increase skills in dementia detection/management.23 Recruitment incentives were incorporated, including GP/medical recruiters, personal telephone recruitment, endorsements by professional associations and remuneration with continuing medical education (CME) points. Despite this, recruitment of GPs to participate in the study was challenging.
The present study's objective was to survey GPs who agreed and those who declined to participate in the GP study in Sydney to determine reasons for, and barriers against, participation. Additionally, we aimed to provide recommendations for ways to increase future GP participation in research.
Method
The University of New South Wales' Human Research Ethics Advisory Panel gave the study ethical approval. All subjects gave informed consent to participate. Subjects completed a survey and received a brief qualitative interview from a research GP to clarify survey responses where possible.
Participants
In the GP project, GPs and their patients aged 75 years and over were recruited across five Australian sites to an RCT to determine whether academic detailing could increase GPs' dementia detection/management skills and patient and carer quality of life. Assessments were conducted at baseline and at 12, 15 and 24 months. In this study – which was conducted in Newcastle, Sydney, Melbourne, Adelaide and Bendigo in Australia – we assessed whether academic detailing could improve GP diagnosis and management of dementia. We audited GPs' diagnoses of dementia in their patients aged 75 and older before detailing, after detailing and 12 months later. Academic detailing stressed the importance of diagnosis of dementia and educated GPs in techniques for cognitive screening, including the use of the General Practitioner Assessment of Cognition (GPCOG)24 – a brief, efficient method of screening for cognitive impairment – and appropriate investigations and referral pathways. Two in three GPs who accepted entry into the trial were randomised to the intervention group and received the academic detailing; the other third, who were the control group, were mailed a copy of GP guidelines for diagnosis and management of dementia after the 12 month follow-up. There were 40 GPs at the Sydney site (28 in the treatment group, 12 in the control group) participating in the main GP project at the time of recruitment. The GP project's refusal rate was not recorded.
For the present study, a convenience sample of GPs was recruited from the GP project's Sydney control and intervention groups.23 A convenience sample of Sydney GPs who had declined participation in the GP project (refusers) was also recruited.
Survey
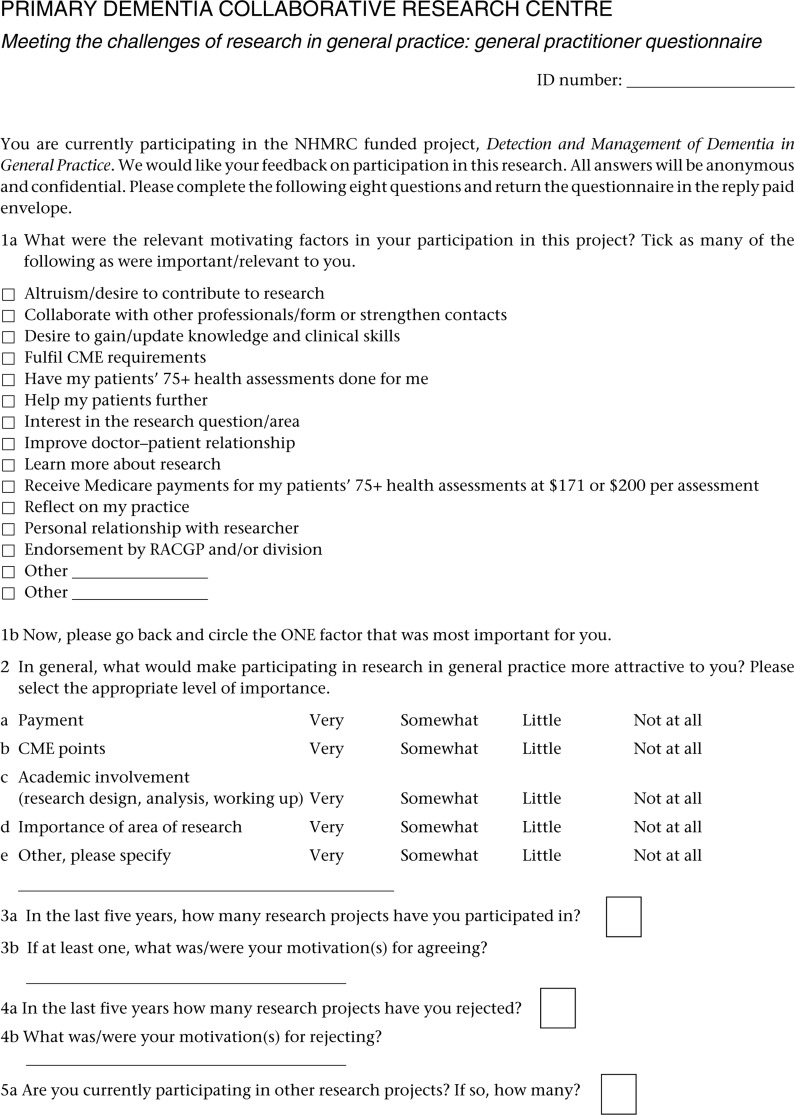
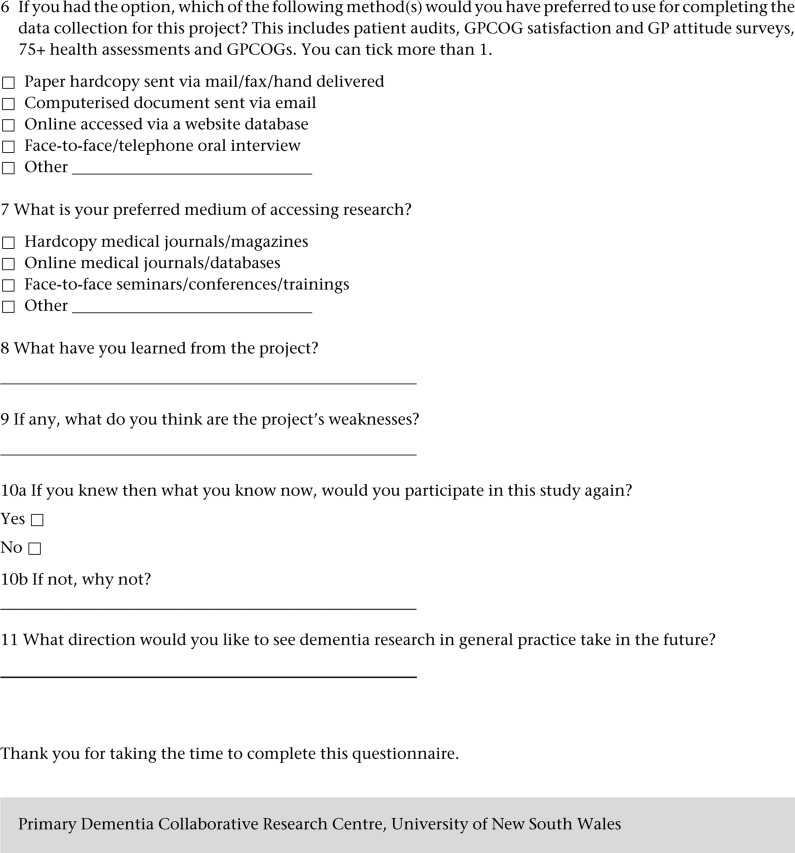
Participants completed the 11-item ‘Meeting the challenges of research in general practice: general practitioner questionnaire’ (GP survey; see Appendix A) between the 15- and 24-month assessments. Developed for this study, it assessed incentives and disincentives for participating in dementia research and ascertained GPs' thoughts regarding the future direction and design of GP research. For example, GPs were asked about motivating factors for research participation, experience with research and incentives to make research participation more attractive. Some questions were not applicable to all groups. Questions concerning their participation in the current study were not applicable to the refuser group (Questions 8, 9 and 10), and questions about motivation for current participation were modified to ask refusers to identify possible motivating factors (Questions 1a and b).
Qualitative interview
Following the survey completion, participants received brief qualitative interviews with a research GP to clarify responses and add any extra information. Answers were recorded on the GPs' surveys and are reported with survey data. General interview observations are reported separately.
Analysis
Survey data were analysed using SPSS version 18. Lack of independent sampling precluded significance testing on questions 1a, 6 and 7, as did the small sample sizes in question 1b. These questions were interpreted using descriptive statistics.
Because of the small sample sizes, Question 2 responses were collapsed into two categories for analysis so that ‘not at all’ and ‘little’ became ‘not important’ and ‘somewhat’ and ‘very’ became ‘important’. Groups were then analysed separately with an exact binomial test (test probability = 0.50 for each response category). Questions 3 and 4 were analysed using a one-way analysis of variance.
Results
Participants
Thirty GPs completed the survey; ten each from the intervention (4 male and 6 female), control (8 male and 2 female) and refuser (8 male and 2 female) groups. Exact ages of respondents were not recorded, but in keeping with the GP project (mean = 50.5 years, SD = 10.6), more than 85% were aged 50 to 65 years. None of the approached GPs for this brief survey declined participation.
Survey results
The three most frequently favoured motivating (or possibly motivating) factors (Table 1, Question 1a) were also endorsed as the most important for Question 1b – update knowledge, help patients and altruism. For Question 2, accrual of CME points and research area importance were rated as important by the treatment (Table 2A) and control (Table 2B) groups. The refuser group only endorsed research area importance (Table 2C).
Table 1.
Question 1a: What were the relevant motivating factors in your participation/possible participation in this project? Tick as many of the following as were important/relevant to you.
| Treatment | Control | Refuser | Total | |
|---|---|---|---|---|
| n = 10 | n = 10 | n = 10 | n = 30 (%) | |
| Altruism | 2 | 8 | 8 | 18 (60) |
| Collaboration | 3 | 2 | 5 | 10 (33) |
| Update knowledge | 8 | 6 | 9 | 23 (77) |
| CME | 5 | 4 | 4 | 13 (43) |
| 75+ health assessments | 3 | 3 | 3 | 9 (30) |
| Help patients | 5 | 8 | 8 | 21 (70) |
| Interest | 3 | 3 | 2 | 8 (27) |
| Improve relationship | 3 | 3 | 3 | 9 (30) |
| Learn | 1 | 1 | 3 | 5 (17) |
| Medicare | 2 | 3 | 1 | 6 (20) |
| Reflect | 5 | 3 | 3 | 11 (37) |
| Researcher | 0 | 0 | 2 | 2 (7) |
| RACGP/division | 2 | 0 | 2 | 4 (13) |
| Other | 2 | 0 | 2 | 4 (13) |
CME = Continuing Medical Education
RACGP = Royal Australasian College of General Practitioners
Table 2.
Question 2: In general, what would make participating in research in general practice more attractive to you? Please select the appropriate level of importance.
| Unanswered | Not important | Important | P(df = 1)† | 95% CI** | |||
|---|---|---|---|---|---|---|---|
| n (%) | Not at all n (%) | Little n (%) | Somewhat n (%) | Very n (%) | |||
| A Treatment Group | |||||||
| Payment | 2 (20) | 1 (10) | 1 (10) | 2 (20) | 4 (40) | 0.29 | 0.03–0.65 |
| CME points | 1 (10) | 0 (0) | 0 (0) | 5 (50) | 4 (40) | 0.004 | 0.66–1.00 |
| Academic involvement | 2 (20) | 1 (10) | 1 (10) | 5 (50) | 1 (10) | 0.29 | 0.03–0.65 |
| Importance of area of research | 3 (30) | 0 (0) | 0 (0) | 2 (20) | 5 (50) | 0.02 | 0.59–1.00 |
| Other | 8 (80) | 0 (0) | 0 (0) | 0 (0) | 2 (20) | 0.50 | 0.16–1.00 |
| B Control Group | |||||||
| Payment | 0 (0) | 1 (10) | 1 (10) | 2 (20) | 6 (60) | 0.11 | 0.03–0.56 |
| CME points | 0 (0) | 0 (0) | 1 (10) | 3 (30) | 6 (60) | 0.02 | 0.003–0.45 |
| Academic involvement | 0 (0) | 1 (10) | 2 (20) | 4 (40) | 3 (30) | 0.344 | 0.07–0.65 |
| Importance of area of research | 0 (0) | 1 (10) | 0 (0) | 5 (50) | 4 (40) | 0.021 | 0.003–0.45 |
| Other | 10 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | N/A* | N/A* |
| C Refuser Group | |||||||
| Payment | 0 (0) | 1 (10) | 2 (20) | 5 (50) | 2 (20) | 0.34 | 0.07–0.65 |
| CME points | 0 (0) | 1 (10) | 3 (30) | 3 (30) | 3 (30) | 0.76 | 0.12–0.74 |
| Academic involvement | 0 (0) | 2 (20) | 2 (20) | 5 (50) | 1 (10) | 0.75 | 0.12–0.74 |
| Importance of area of research | 0 (0) | 0 (0) | 1 (10) | 6 (60) | 3 (30) | 0.02 | 0.003–0.45 |
| Other | 9 (90) | 0 (0) | 0 (0) | 1 (10) | 0 (0) | N/A* | N/A* |
CME = Continuing Medical Education
*Sample size too small to calculate.
**Clopper–Pearson binomial 95% confidence interval.
†Responses collapsed into two categories; ‘Not at all’ and ‘little’ = ‘not important’; ‘somewhat’ and ‘very’ = ‘important’. The P value indicates the difference between the ‘not important’ and ‘important’ categories.
Respondents had participated in and rejected a similar number of research projects in the last five years (Table 3, Questions 3a and 4a). When reporting participation motivators (Question 3b) all groups listed CME point accrual. Interest in the subject area and improved patient outcomes were also favoured, as were practice payment incentives, personal knowledge, an opportunity to collaborate or become involved in research and to provide assistance to GPs' divisions.
Table 3.
Mean number of research projects accepted and rejected
| Participators (treatment and control) mean (n) | Refusers mean (n) | Total mean (n) | F(df) | P | 95%CI | |
|---|---|---|---|---|---|---|
| Question 3: In the last 5 years, how many research projects have you participated in? | 1.44 (18) | 1.10 (10) | 1.32 (28) | 0.36(1,26) | 0.56 | −0.84–1.53 |
| SD = 1.58 | SD = 1.20 | SD = 1.44 | ||||
| Question 4: In the last 5 years, how many research projects have you rejected? | 2.12 (17) | 2.30 (10) | 2.19 (27) | 0.03(1,25) | 0.87 | −2.50–2.14 |
| SD = 2.71 | SD = 3.02 | SD = 2.77 | ||||
Lack of time, the overwhelming reason all groups gave for rejecting past research projects (Question 4b), was mentioned by 13 GPs (43%). Not being approached in person was also mentioned by a control group member. Other responses included lack of interest in the research topic, difficulty executing research in general practice, over-long explanations to give to patients and too much paperwork. Two respondents were currently participating in one other research project (one treatment respondent and one refuser; see Question 5).
Respondents favoured online data collection for the GP project (Table 4, Question 6), matching their preference for online journals (Table 5, Question 7). Other data collection methods/mediums for accessing research were similarly favoured.
Table 4.
Question 6: If you had the option, which of the following method(s) would you have preferred to use for completing the data collection for this project? This includes patient audits, GPCOG satisfaction and GP attitude surveys, 75+ health assessments and GPCOGs. You can tick more than 1
| Treatment | Control | Refused | Total (%)* | ||
|---|---|---|---|---|---|
| Paper/hardcopy | 4 | 4 | 3 | 11 (36) | |
| Computerised | 3 | 2 | 5 | 10 (33) | |
| Online | 7 | 7 | 5 | 19 (63) | |
| Face-to-face | 4 | 3 | 3 | 10 (33) | |
| Other | 0 | 0 | 1 | 1 (3) | |
*Percentage of GP endorsements.
Table 5.
Question 7: What is your preferred medium of accessing research? [Respondents were able to tick more than one]
| Treatment | Control | Refused | Total (%)* | |
|---|---|---|---|---|
| Hardcopy journals | 5 | 4 | 6 | 15 (50) |
| Online journals | 6 | 7 | 8 | 21 (70) |
| Seminars/conferences | 7 | 5 | 4 | 16 (53) |
| Other | 0 | 0 | 0 | 0 (0) |
*Percentage of GP endorsements.
The treatment group frequently cited, as benefits, learning about the GPCOG (Question 8) and general increase in dementia knowledge/types and screening.24 The control group cited fewer benefits other than an overall increase in dementia knowledge, although one GP mentioned being more proactive in prescribing dementia medication. Other responses were increased awareness of memory loss and feeling comfortable discussing it with patients, the need for dementia screening and more accurate assessment. Three control GPs said they had learned nothing, despite receiving copies of the GP Dementia Guidelines in the mail.
Both treatment and control participants commonly listed poor communication about the aims and objectives and insufficient education at the beginning of a project as study weaknesses (Question 9). Other comments concerned the project's length, excessive paperwork, loss of paperwork (mainly by GPs), wanting a more active study role and wanting more GPCOG training.
For Question 10a, 16 of the 20 treatment and control participants (80%) indicated that they would participate in the study again; two said they would not (one treatment; one control) without giving a direct reason (Question 10b) and two did not answer the question.
Screening/diagnosis, management and treatment were common themes regarding future directions of GP dementia research (Question 11), as was a focus on family carer outcomes. Other requests included brainstorming opportunities and education about clinical stages of the dementias, effectiveness of early dementia treatment for Alzheimer's disease, sexual behaviour and disinhibition, frontotemporal dysfunction and medication, how interventions, particularly early intervention will change outcome, prevention strategies and access to services, and how to better organise and structure carer programmes.
Researchers' observations from qualitative interviews
The interviews strongly reflected the answers to the questionnaires. The barriers to research participation – of lack of time and burdensome paperwork – were again cited. GPs preferred simple studies with clear aims and research relevant to their role at the ‘coal face’ of dementia services and they appreciated remuneration but did not rank this highly.
Discussion
Although GPs were already well informed, respondents cited gaining further knowledge about dementia and screening as benefits of research participation. The treatment and control groups agreed they would participate in the GP project again, with altruism the most commonly reported incentive across all groups, desire to gain or update knowledge and clinical skills and a wish to help patients. Interestingly, these were similarly endorsed between groups, suggesting that attitudes towards research did not vary. Rather, it was other aspects of the refuser sample – the GP study itself or the topic – that inhibited the refuser group from participating.
As the relevance of the research area to clinical practice was an identified motivator,10,22 it is possible that while all groups valued research in general, only treatment and control participants considered the GP study topic to be interesting or relevant to their particular practice. Personal recruitment has previously improved participation;21 not being approached in person was mentioned as a reason for rejecting past studies, providing limited evidence that the GP project's personal contact may have been a participation incentive. Recruitment by fellow doctors has shown to yield high recruitment rates.13,21
Although not directly asked, neither desire to collaborate with other fellow GP professionals nor having personal relationships with fellow GP researchers encouraged participation. This may, however, be deceptive as Veitch et al found that having the title ‘doctor’ improved the likelihood of GPs' receptionists connecting telephone calls, suggesting that the impact is on receptionists, not on GPs.21 A GP recruiter may still therefore be a prudent inclusion. Endorsements by professional associations or steering committees may or may not yield extra participation.10,12 The present study did not support an appreciable effect, although the use of ‘liaison doctors’ may be more motivating.13,14
As previously found, although GPs recognised the importance of research, time constraints due to high workload was by far the most commonly reported reason for rejecting studies.10,12,13 In contrast to Salmon et al however,9 the GP survey did not find that remuneration could overcome this barrier. All groups thought CME points were attractive but they were outweighed by lack of time. It is possible that remuneration only adds incremental incentive if time input is minimised or if it is sufficiently commensurate.
All groups favoured online data collection and research access due to simplicity and perceived time savings; this benefits recruitment because of reduced time input and less paperwork.10 Cited weaknesses of the GP project recapitulated attitudes towards research generally. Poor communication about the study's objectives, it's lengthy nature and excessive paperwork all echoed the impression that GPs favour clear, simple studies with minimal time input. Similar to Herber et al,10 GPs preferred future research to focus on issues immediately relevant to them.
The GP survey was limited by several factors. Although some,19,25 but not all,26 previous research has found that younger GPs are more likely to participate in research, the current study could not assess this as fewer than 15% of GPs studied were under the age of 50. Gender bias was present as two-thirds of the sample were male (although this may be an artefact of gender imbalance in the GP project), and it is possible that the convenience sampling introduced further biases. Future surveys should utilise random sampling where possible.
Recruitment is just one component in enhancing research in general practice, which was once considered neglected and ‘one of the most intellectually underdeveloped disciplines in medicine’ and even ‘a lost cause’.27,28 Primary care research lags behind other specialties in output and status.29–31 In Australia, only 3% of Australian GPs engage in research,32 perhaps because of low remuneration,33 pressure to work clinically and a negative attitude toward research.34–36 This situation is improving worldwide with the establishment of practice-based research networks, collaborative targeted research and targeting funds for primary care research.37,38 Participation in research can improve knowledge and skills of clinicians and improve the status of the primary care profession.31
In 2003, the World Organization of Family Doctors (WONCA) made several recommendations in Improving Health Globally: the necessity of family medicine research, which stated that building research capacity and introducing a research culture are essential to realise the potential of family medicine research.31 Action research or participatory research that involves comunities in conducting and owning the research results is an effective method to involve GPs more directly in the research needs of their community.39 It is important to engage practising GPs in generating relevant research questions, facilitating research in their practices and implementing findings.40 This results in GPs who are more analytical about monitoring their own practice, with the potential to improve their practice and so benefit their patients.
Conclusions
Future GP participation in research could be maximised by considering the following recommendations.
Reduce GPs' time burden. The most viable GP research appears to be studies that have minimal time input, regardless of any other factors. Paper-work and other time-consuming activities are deterrents. If unavoidable, they should fall on the research team where possible.
Make it simple and online. Simple instructions and guidelines with information entered into an online database could reduce both real and perceived time burdens.
Offer CME points or other remuneration. Remuneration commensurate with time input, coupled with simple, time-effective protocols, may facilitate recruitment.
Consider the recruiter. Personal recruitment by a GP recruiter seems likely to improve participation. If feasible, the steering committee and ‘liaison doctor’ model, may be even more successful.13,14
Research ‘coal face concerns’. Not all GPs will be interested in all topics. Accept that GPs will choose subject areas clinically relevant to them.
GPs value research and are interested in improving patient outcomes through evidence-based medicine. Careful planning that considers the needs and interests of GPs appears to be the most likely way of improving GP recruitment. By focusing on GPs and following these recommendations, higher rates of participation may be achieved.
ACKNOWLEDGEMENTS
Brodaty and Pond were principal investigators of the project while Brodaty and Waine conceptualised the paper. Shell, Lilian and Waine recruited GPs, collected data and assisted with writing the paper; Gibson and Waine reviewed the literature. All authors were involved in drafting and/or reviewing several versions of the paper. Kim Burns assisted with preparation of the manuscript for submission.
Appendix A
Contributor Information
Henry Brodaty, Scientia Professor of Ageing and Mental Health; Director of Dementia, Collaborative Research Centre, University of New South Wales, Sydney, Australia.
Louisa HR Gibson, Research Assistant, Academic Department in Old Age Psychiatry, Prince of Wales Hospital, Sydney, Australia.
Melissa L Waine, Research Assistant, Faculty of Health, University of Technology, Sydney, Australia.
Allan M Shell, Academic General Practitioner and Honorary Research Fellow.
Ruth Lilian, Administrative Officer, Dementia Collaborative Research Centre, School of Psychiatry, University of New South Wales, Sydney, Australia.
Constance Dimity Pond, Professor of General Practice, Faculty of Health and Medicine, University of Newcastle, Callaghan, Australia.
REFERENCES
- 1.Australian Medical Association Primary Health Care – Position Statement. Australian Medical Association: Canberra, 2010. Available at http://ama.com.au/node/5992 (accessed 14/09/2013). [Google Scholar]
- 2.Wilkinson D, Stave C, Keohane D, et al. The role of general practitioners in the diagnosis and treatment of Alzheimer's disease: a multinational survey. Journal of International Medical Research 2004;32:149–59 [DOI] [PubMed] [Google Scholar]
- 3.Australian Bureau of Statistics 4839.0.55.001 – Health Services: Patient Experiences in Australia, 2009. Australian Bureau of Statistics, 2010. Available at www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4839.0.55.001Main+Features12009 (accessed 27/06/2013). [Google Scholar]
- 4.Britt H, Miller GC, Charles J, et al. General practice activity in Australia 2000–01 to 2009–10: 10 year data tables. General practice series no. 28. Cat. no. GEP 28. AIHW: Canberra, 2010 [Google Scholar]
- 5.Royal Australian College of General Practitioners General practitioner and patient participation in research projects and clinical trials in general practice. Policy endorsed by the 50th RACGP Council, August 2008 [Google Scholar]
- 6.Hummers-Pradier E, Scheidt-Nave C, Martin H, et al. Simply no time? Barriers to GPs' participation in primary health care research. Family Practice 2008;25:105–12 [DOI] [PubMed] [Google Scholar]
- 7.Pearl A, Wright S, Gamble G, et al. Randomised trials in general practice: a New Zealand experience in recruitment. New Zealand Medical Journal 2003;116:1186. [PubMed] [Google Scholar]
- 8.Pirkis JB, Blashki GA, Murphy AW, et al. The contribution of general practice based research to the development of national policy: case studies from Ireland and Australia. Australia and New Zealand Health Policy 2006;3:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salmon P, Peters S, Rogers A, et al. Peering through the barriers in GPs' explanations for declining to participate in research: the role of professional autonomy and the economy of time. Family Practice 2007;24:269–75 [DOI] [PubMed] [Google Scholar]
- 10.Herber OR, Schnepp W, Rieger MA. Recruitment rates and reasons for community physicians' non-participation in an interdisciplinary intervention study on leg ulceration. BioMed Central Medical Research Methodology 2009;9:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosemann T, Szecsenyi J. General practitioners' attitudes towards research in primary care: qualitative results of a cross sectional study. BioMed Central Family Practice 2004;5:31–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levinson W, Dull VT, Roter DL, et al. Recruiting physicians for office-based research. Medical Care 1998;36:934–7 [DOI] [PubMed] [Google Scholar]
- 13.Borgiel AE, Dunn EV, Lamont CT, et al. Recruiting family physicians as participants in research. Family Practice 1989;6:168–72 [DOI] [PubMed] [Google Scholar]
- 14.Kosecoff J, Chassin MR, Fink A, et al. Obtaining clinical data on the appropriateness of medical care in community practice. Journal of the American Medical Association 1987;258:2538–42 [PubMed] [Google Scholar]
- 15.Saver BG, Taylor TR, Treadwell JR, et al. Do physicians do as they say? The case of mammography. Archives Family Medicine 1997;6:543–8 [DOI] [PubMed] [Google Scholar]
- 16.Myerson S. Improving the response rates in primary care research. Some methods used in a survey on stress in general practice since the new contract (1990). Family Practice 1990;10:342–6 [DOI] [PubMed] [Google Scholar]
- 17.Ward J. General practitioners' experience of research. Family Practice 1994;11:418–23 [DOI] [PubMed] [Google Scholar]
- 18.Glynn LG, O'Riordan C, MacFarlane A, et al. Research activity and capacity in primary healthcare: the REACH study: a survey. BioMed Central Family Practice 2009;10:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Askew DA, Clavarino AM, Glasziou PP, et al. General practice research: Attitudes and involvement of Queensland general practitioners. Medical Journal of Australia 2002;177:74–7 [DOI] [PubMed] [Google Scholar]
- 20.Richardson A, Sutherland M, Wells E, et al. Factors affecting general practitioner involvement in a randomised controlled trial in primary care. New Zealand Medical Journal 2002;115:153–5 [PubMed] [Google Scholar]
- 21.Veitch C, Hollins J, Worley P, et al. General practice research. Problems and solutions in participant recruitment and retention. Australian Family Physician 2001;30:399–406 [PubMed] [Google Scholar]
- 22.Williamson MK, Pirkis J, Pfaff JJ, et al. Recruiting and retaining GPs and patients in intervention studies: the DEPS-GP project as a case study. BioMed Central Medical Research Methodology 2007;7:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pond CD, Mate K. Ageing in General Practice team P1–380: The detection and management of dementia in Australian general practice. Alzheimer's Dementia 2008;4(Suppl):T330 [Google Scholar]
- 24.Brodaty H, Pond D, Kemp NM, et al. The GPCOG: a new screening test for dementia designed for general practice. Journal of the American Geriatric Society 2002;50:530–4 [DOI] [PubMed] [Google Scholar]
- 25.Hammersley V, Hippisley-Cox J, Wilson A, et al. A comparison of research general practices and their patients with other practices – a cross-sectional survey in Trent. British Journal of General Practice 2002;52:463–8 [PMC free article] [PubMed] [Google Scholar]
- 26.Down L, Metcalfe C, Avery K, et al. Factors distinguishing general practitioners who more readily participated in a large randomized trial were identified. Journal of Clinical Epidemiology 2009;62:67–73 [DOI] [PubMed] [Google Scholar]
- 27.Horton R. Evidence and primary care. The Lancet 1999;353:609–10 [DOI] [PubMed] [Google Scholar]
- 28.Editorial Is primary-care research a lost cause? The Lancet 2003;361:977. [PubMed] [Google Scholar]
- 29.Farrell E, Magin P, Pirotta P, et al. Training in critical thinking and Research: an audit of delivery by regional training providers in Australia. Australian Family Physician 2013;42:221–4 [PubMed] [Google Scholar]
- 30.Askew DA, Glasziou PP, Del Mar CB. Research output of Australian general practice: a comparison with medicine, surgery and public health. Medical Journal of Australia 2001;175:77–80 [DOI] [PubMed] [Google Scholar]
- 31.van Weel C, Rosser WW. Improving health care globally: a critical review of the necessity of family medicine research and recommendations to build research capacity. Annals of Family Medicine 2 2004;(Suppl 2):S5–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Field D, Ward AM, Lopez DG. Apart from Medicare, what other work do GPs do? Australian Family Physician 2003;32:476–80 [PubMed] [Google Scholar]
- 33.Del Mar C, Askew D. Building family/general practice research capacity. Annals of Family Medicine 2 2004;(Suppl 2):S35–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Parchman M, Katerndahl D, Larme A. Family medicine and research: From here to eternity. Family Medicine 2003;35:291–5 [PubMed] [Google Scholar]
- 35.Katerndahl DA, Parchman M, Larme A. Cultural (R)evolution: developing a research culture in family medicine. Family Medicine 2002;34:616–8 [PubMed] [Google Scholar]
- 36.Neale AV. A national survey of research requirements for family practice residents and faculty. Family Medicine 2002;34:262–7 [PubMed] [Google Scholar]
- 37.Peterson KA, Lipman PD, Lange CJ, et al. Supporting better science in primary care: A description of practice-based research networks (PBRNs) in 2011. The Journal of the American Board of Family Medicine 2012;25:565–71 [DOI] [PubMed] [Google Scholar]
- 38.Brown LJ, McIntyre EL. The contribution of primary health care research, evaluation and development-supported research to primary health care policy and practice. Australian Journal of Primary Health, 2012. Available at http://dx.doi.org/10.1071/PY12058 (accessed 14/09/2013). [DOI] [PubMed] [Google Scholar]
- 39.Mccauly AC, Gibson N, Freeman W, et al. Participatory research maximises community and lay involvement. BMJ 1999;319:774–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Magin P, Pirotta P, Farrell E, et al. General practice research: training and capacity building. Australian Family Physician 32010;9:265–6 [PubMed] [Google Scholar]
ETHICAL APPROVAL
The University of New South Wales' Human Research Ethics Advisory Panel provided ethical approval.
FUNDING
This project was funded by the Dementia Collaborative Research Centre: Assessment and Better Care (Project No. PDCRC-CB40), University of New South Wales, as part of the Australian government's dementia initiative. The views expressed in this work are the views of its author(s) and not necessarily those of the Australian government.
CONFLICTS OF INTEREST
Brodaty, Waine, Shell and Lilian are, or were, employees of the Dementia Collaborative Research Centre, who funded the project. Brodaty, Pond and Gibson and/or their institutions have had financial relationships with GP Training: Valley to Coast, Pfizer, NHMRC, Department of Health and Ageing, Lundbeck, beyondblue, Janssen-Cilag, Merck, Nutricia, Sanofi, Servier, Tau Therapeutics, Novartis, Eisai, Medivation and/or Lilly.