Abstract
Background
Zambian Health Workers Retention Scheme (ZHWRS) commenced in 2003. The schemes' original aim was to retain and recruit Zambian doctors in rural and remote districts. The aim of the ZHWRS subsequently expanded to also include other health workers, in either rural or urban areas. The scheme was formulated to address, in part, the drastic shortage of health workers.
Objectives
To evaluate the effectiveness of the ZHWRS in achieving its aim.
Methods
The data on the number of health workers recruited by the ZHWRS and the spatial distribution of them was reviewed. A survey of health workers was undertaken to elicit their views of their working conditions, their job satisfaction and the effectiveness of retention schemes in retaining or increasing the numbers of and overall satisfaction of health workers.
Results
The ZHWRS has not been successful in recruiting sufficient numbers of health workers to reverse the shortage problem or even to meet the modest targets of the scheme itself. However, these improvements do not decrease the likelihood of Department of Health (DoH) workers leaving their rural based positions.
Conclusions
The ZHWRS has not fully met either its original or revised aims. The drastic shortage of health workers in Zambia continues.
Keywords: Zambia, Health Workers, Retention Scheme
Introduction
In Zambia, the Ministry of Health (MoH) is confronted by a human resource for health (HRH) crisis1. Lack of personnel in key areas of the country's health system is worsened by internal migration (from rural to urban areas). This in turn exacerbates the inequitable spatial distribution of health personnel. Thus, communities in rural areas are most af y the shortage of health workers. This pattern of a dire health worker shortage in total and spatiall ted throughout the countries of sub-Saharan Africa. Internal and external brain drain is severely weakening already stressed public health systems.
In this stud one method by which the Zambian authorities have attempted to address the health worker shortage problem, the Zambian Health Workers Retention Scheme (ZHWRS), is evaluated for its effectiveness. The schemes' initial aim when it was established in 2003 was to retain and recruit indigenous Zambian doctors in rural and remote districts. The ZHWRS subsequently expanded from doctors to assisting other health worker cadres including tutors, nurses and paramedical staff to serve in rural areas.
The method of evaluation of the ZHWRS was twofold. The first was to investigate the spatial distribution of the different health workers by cadre. This indicates the overall shortage of all cadres and the maldistribution of them between urban and rural areas. The second was to survey health worker cadres to find out if they were attracted or could be retained in the Department of Health (DoH) via income and other supplementations such as those available through the ZHWRS. To this end 234 health workers were surveyed and the results from that survey are presented and discussed here. Evidence of the impacts of the ZHWRS on health worker motivation shows marginal success. This outcome is further discussed in the context of the challenges of retention schemes and other potential policy initiatives which could be adopted to address the human resource shortage problem.
The Zambian Health Workforce
Zambia is working with only 50% of the required HRH to deliver basic health services, with even higher vacancy rates in rural areas.1 Staff-to-population ratios nationally are as low as 1 doctor per 14,500 people and 1 nurse per 1,800 people2; this is much lower than the one health worker per 400 people recommended as the minimum threshold necessary to provide coverage of basic health services3. The current shortage of over 28,000 health workers is one of the key impediments to meeting the global commitment to universal access to HIV/AIDS treatment, care and prevention by 2015, as well as to reaching the health-related MDGs4.
In 2005, the MOH initiated a policy reform process to address this critical shortage in the public sector and established targets and strategies to achieve.1 The established employment targets for each health worker cadre were based on recommended World Health Organization (WHO) staff-to-population ratios (2.3 to 1,000) with modifications by the MOH and health facility managers.3 To achieve the targets the health plan is supposed to increase the numbers of trained staff and ensure their equitable distribution, increase productivity and performance of health, ensure effective, ongoing and coordinated approach to human resource planning across the sector and strengthen human resource planning, management and development systems at all levels. It is also supposed to recruit all graduating students, retiring critical cadres, attract Zambian health workers, promote the retention of health workers, through the provision of monetary and non-monetary, strengthen regulatory role of certification and registration of health professionals in order to effectively monitor and control brain drain.1
The health plan is expected to annually produce 100 medical doctors; 500 nurses; 250 midwifes. It aims to annually recruit 100 doctors and 300 nurses from other sources, mainly returning Zambians.1 To address the health worker deficit the health plan had specific cadre targets as shown in table 1.
Table 1.
Public sector staffing levels by Health worker cadre: 2006–2008
| Cadre | 2006 | 2007 | 2008 | Recommended establishment |
Deficit |
| Doctors | 646 | 720 | 861 | 2300 | 1439 |
| Clinical Officer | 1161 | 1213 | 1828 | 4000 | 2172 |
| Registered & Enrolled Midwives | 2273 | 2255 | 2393 | 5600 | 3207 |
| Registered & Enrolled Nurses | 6096 | 6534 | 6345 | 16732 | 10387 |
| Medical Assistants | 2581 | 2334 | 2500 | 3168 | 668 |
| Tutors and lecturers | 157 | 163 | 196 | 200 | 4 |
| Paramedics | 3200 | 3370 | 3090 | 6000 | 2910 |
| Laboratory Technologist | 417 | 427 | 432 | 1560 | 1228 |
Source: Authors' own computation based on Ministry of Health management information system database.
The total recommended establishment for health workers in the MOH is 56,000 however the total existing staff by 2008 was just over 27,000.5 Thus, Zambia is currently operating at 50% of the required HRH and has a deficit of over 28,000 staff.
The Zambian Health Worker retention scheme
In 2003, the Zambian Government in partnership with the Royal Netherlands Government embarked on the ZHWRS. The schemes' aim was to retain and recruit indigenous (i.e. local) doctors in rural and remote districts. This was to ensure a balance in the distribution of key health staff throughout the country. The objectives of the scheme are twofold. One, is to reduce attrition rates of existing, critical health workers from rural and remote areas and two, to attract new health workers to rural areas. The scheme provides various retention incentives, including non-financial incentives such as career development opportunities and housing. The ZHWRS subsequently expanded from covering doctors to also include tutors, nurses and paramedical staff serving in rural and remote districts. Currently, 627 health workers in 41 districts of the country are benefiting from the ZHWRS3.
Prior to the implementation of the ZHWRS there was a policy of compulsory rural posting for doctors of one year after finishing their internship3. However, the implementation of this policy was erratic. This obligatory policy made many doctors quit government posts as they were not ready to serve under indigent conditions. The tactic of some young doctors was to keep on working for some time in tertiary hospitals until they found an attractive post elsewhere, or undertook postgraduate study6. In order to initiate the retention scheme, the extension of the internship in tertiary hospitals from 12 to 18 months was made, and rigorous supervision was offered during that period7. Tertiary hospitals terminated working relations with doctors who had just completed their internships to direct them to the Central Board of Health (CBoH) for rural posting. The CBoH and provincial offices vigorously pursued posting of doctors to rural areas. Between 2003 and end 2004 a total of 68 doctors were contracted under ZHWRS. About 15 doctors were already working in the districts eligible for the ZHWRS, and were integrated into the scheme. Others were taken on from other parts of Zambia8.
The key components of the ZHWRS are that cadres serve a period of three years in rural areas. They are paid a rural hardship allowance per month with cadres in rural and extremely rural districts getting more than those in peri-rural districts. Cadres received education allowances per year per child aged between 5 and 21 years. Deployed district cadres were paid renovation funds to improve their accommodation7. At the expiry of the contract cadres are eligible for assistance for postgraduate study. In addition, cadres are subjected to annual assessment of performance and identification of training needs for capacity building. Several benefits are available to scheme members including hardship allowance, vehicle loans, housing rehabilitation subsidies and facility incentives. They are also to be entitled to a loan of 90% of the three years rural hardships allowance8. Thus, the retention scheme has both monetary and non monetary incentives for health workers.
In 2007 the ZHWRS was expanded to all key cadres to encompass clinical officers, nurses and midwives, laboratory technicians, medical licentiates, paramedics, environmental health technicians, tutors and lectures9. The overall aims of the expanded scheme were to enhance health service delivery, to increase the prospective of achieving the MDGs10. Phase one of the ZHWRS as well as phase two which ran from 2006 up to 2008 cost approximately 10 billion Zambian Kwacha per annum (or US$300,000 at the prevailing exchange rate of ZMK3,500 = US$1) and was funded by the Zambian Government (1%) and donors (99%). The 2009 Action Plan for phase three has a budget of 35 billion Kwacha per annum (or US$700,000 at the prevailing exchange rate of ZMK5,000 = US$1)6.
Methods
Documents and data bases were accessed in the various institutions which included pay rolls, reports, circulars from the MOH in particular the vote on salaries and benefits for health workers by cadre. Additional data collected included housing allowances, medical, risk, communication (travel and telephone), field subsistence allowances (per diems), non-practicing allowances and entertainment.
Self administered/structured questionnaires were used to collect data on salaries and benefits from health workers in three districts that represent extremes in working conditions and, potentially, satisfaction for health workers. Those posted to rural areas considered ‘hardship areas’ - due to relative inaccessibility, harsh weather conditions, sparse population and economic disadvantage - are meant to be advantaged through payment of allowances and professional training opportunities beyond those offered to their urban counterparts. The structured questionnaires were administered to doctors, nurses, midwives, clinical officers, physiotherapists, pharmacists and laboratory technicians/technologists. The survey instrument was closely based upon the Immpact Toolkit titled ‘Health Worker Incentives Survey (HWIS)’ from the University of Aberdeen10. Data collection took place in September, 2008.
A random selection of private and public voluntary health facilities was undertaken from a listing of the facilities in the respective regions. A stratified sampling frame was constituted by region and type in line with policy relevance. A total of 234 health workers were interviewed in three districts namely, Lusaka (urban), Monze and Nyimba (both rural). Monze in southern Zambia is 200km from the capital Lusaka and the town has a population of 30,000. Nyimba in eastern Zambia is 330km from Lusaka and the town has a small population whilst the district comprises 50,000 people. For the purpose of empirical analysis some categories that were thought to be homogeneous were grouped together. Two notable categories were registered and enrolled nurses and registered and enrolled midwives. Based on the above methodology of categorisation, table 2 shows the categories of health workers surveyed.
The majority of the cadres interviewed were registered and enrolled nurses (51%) followed by paramedics (24%). Dental therapist and clinical officers were the smallest category at 2% of total workers.
Statistical analysis of the survey data was undertaken by means of a logit model using E-Views and SPSS.
Results
Staffing Levels
Table 3 shows the beneficiaries of the ZHWRS by cadre type. The staffing levels across all cadres through the ZHWRS mechanism are below the MoH's own (modest) targets. Almost all cadre types are below half of the recommended target that the scheme attempted to achieve.
Table 3.
Beneficiaries of the ZHWRS by Cadre
| Cadre | Targets | Employed | Employed |
| for 2008 | April 2008 | February 2009 | |
| Doctors | 150 | 84 | 94 |
| Medical Licentiate | 150 | 12 | 31 |
| Health Lecturers/Tutors | 200 | 130 | 196 |
| Clinical Officers | 400 | 10 | 31 |
| Nurses and Midwives | 400 | 200 | 204 |
| Paramedics | 250 | 80 | 71 |
| Total | 1,650 | 516 | 627 |
Source: Authors' own computation based on Mwale (2009).
As at 2009 only 627 health workers (or approximately 3% of the total health workforce) were in the MoH workforce as a result of the ZHWRS. Of these 94 were doctors, 27 were medical licentiates, 204 were nurses and midwives and 196 were tutors or lecturers. By retaining 35% of the original batch of doctors and then adding an additional 57, there are now 94 doctors on the ZHWRS who are largely practicing in the rural and remote districts2,11. This represents an increase of only 24% in the number of doctors between 2006 and 2009 which implies that both the attraction and retention capacities of the scheme have been declining over time.
The regional distribution of retention scheme beneficiary findings shows there is a variation of cadres per province across the different provinces. The distribution of health workers is biased towards urban areas with most of the remote areas operating without qualified staff. However, the distribution of doctors in the North western, southern and western provinces which are the most rural areas are higher than in other provinces with 12, 14 and 17 doctors respectively. Luapula and Central province have the lowest with just 5 doctors each. Lusaka, Central and Eastern have the highest provincial total of beneficiaries at 83, 84 and 106 respectively. North Western, Western and Luapula have the lowest at 46, 55 and 59 provincial total respectively. The total regional retention scheme beneficiaries are 627.
The data shows that the percentage gap to target varies across cadres in spite of the retention scheme taking a similar format. For instance, the gap for tutors to target is the lowest at 2% followed by doctors at 37%. Clinical officers' percentage gap to target is the highest at 93% followed by medical licentiates at 79%.
At the national level, the distribution of health workers is still skewed towards urban areas with most of the remote areas operating without qualified staff. For instance, 70% of all doctors employed and 44% of all health workers are based in two urban provinces, namely Lusaka and Copperbelt5. A comparison of doctor population ratios also reveals a higher ratio of 1:6,247 for Lusaka (urban) and 1:65,763 for Northern (remote). In addition, more than half of rural health centres have only one qualified staff member and numerous facilities operate without any professional staff1.
Job Satisfaction and Intentions to Quit
Job satisfaction in the health sector is generally very low. The survey results revealed that approximately 40% of surveyed health workers have either very low or low job satisfaction. This low job satisfaction contributes to the desire to quit and leads to high attrition rates in the health sector.
The survey also revealed that about 48% of the health workers interviewed showed a desire to quit working in their current locations. Of those, 33% indicated that they wanted to join the private health sector, while 26% and 19% wanted to migrate outside Zambia and to local NGO health facilities, respectively. A critical analysis of desire to quit showed that it is primarily affected by factors including age, gender and marital status.
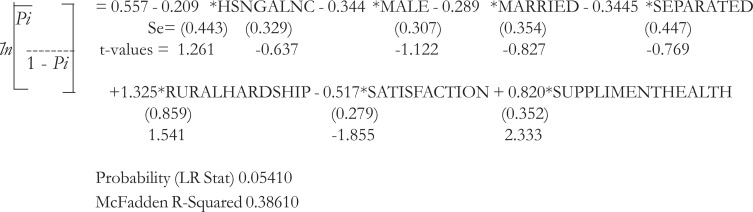
To test the significance of these factors a logit model was estimated with the desire to quit as a dependent variable. The logit model was estimated in E-views and evaluated for model adequacy and is presented in its full function form as indicated in the Logit Model. The regressors include marital status, age, gender, location (urban/rural), level of satisfaction, and whether someone receives housing, rural hardship allowance and whether someone supplements income or not.
The Logit Model
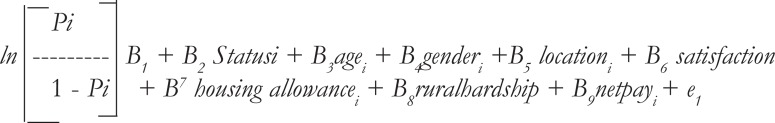
Where Pi is the probability that and individual will report as considering to quit, status is marital status (married, separated or single), gender is the sex where (1 = male and 0 otherwise), satisfaction is the level of satisfaction (1 = satisfied and 0 otherwise) housing allowance indicates whether someone gets housing allowance or not (1 = yes and 0 otherwise), rural hardship is whether someone gets rural hardship allowance (1 = yes and 0 otherwise) while net pay is after tax income. Supplement health is a dummy for individuals who supplement their income with private health work (1= yes and 0 otherwise). Modelling of the above equation suggested that the best fit model is as follows:
The model results reveal a negative relationship between housing allowance and the odds in favour of an individual having the desire to quit. This implies that housing is an important factor in successful retention and attraction of health staff. The results further show a negative relationship between one being male, married and separated and the odds in favour of an individual having the desire to quit. The results indicate the desire to quit is reduced by 35%, 29% and 35% when an individual is male, married and separated, respectively.
The data also shows a positive relationship between rural hardship allowance and the odds in favour of having the desire to quit. The odds in favour of a health worker to quit increases by 3.8 times when someone is on the retention scheme. This could be explained by the fact that actual retention benefits are far less than the cost associated with the harsh conditions in working and living in remote and rural areas. The net result is the desire to relocate and forfeit the rural hardship allowance.
Discussion
In this section a three way discussion of the effectiveness of the ZHWRS is undertaken. First, changes in staffing levels as a result of the ZHWRS and the spatial distribution of health workers is undertaken. Second, the results of a survey of health worker satisfaction and motivation and attitudes towards retention schemes are contextualized. Third, a review of the literature on other financial based retention schemes in health care is undertaken.
Staffing Levels and Location
The data on staffing levels in rural areas shows that some of the initial goals of the ZHWRS have been met. There are now slightly more health care service providers in rural and remote areas where there was no service delivery previously or where the capacity to provide health care services was restricted due to a critical shortage of professional medical staff. The increase in nurse tutors and lecturers, primarily in the cities, should indicate the potential to scale up the number of trained nurses in the coming years.
Further, the findings show that it was very difficult for all health facilities to attract and retain almost all types of health cadres. This was evidenced by the fact that no health facility in Monze and Nyimba (both rural) has ever managed to fulfil their establishments. Reasons for this include the fact that most health cadres shun rural areas due to a host of social and economic factors. Notable factors identified in the survey include lack of accommodation, low salaries, absence of certain allowances (retention, rural hardship), inadequate allowances and social amenities. These factors, including bureaucratic failure, compound each other to worsen the human resource situation in remote and rural areas. The facility managers interviewed also pointed out that the retention scheme should be rolled out to include all cadres serving in rural areas rather than just focussing on doctors. This has now been done. It is particularly hard to recruit health cadres such as doctors, medical assistants, clinic officers and nurses for rural areas. This is despite these cadres being eligible for the ZHWRS. These factors pose a serious challenge to health facility managers in ensuring quality and equity in health care delivery in that they can not achieve staff levels anywhere near the allocated establishment.
Job Satisfaction and Motivation
The ZHWRS lacks practical and effective strategies to address factors affecting the motivation of health cadres in remote and rural areas. The “one size fits all” approach to recruitment of HRH in the ZHWRS is a severe limitation in that health cadres' unique characteristics and needs are neglected in the process, as the lifestyle needs of a newly qualified, urban, single, young doctor are very different to that of a more mature, rural, nurse with a family, for example. Therefore, the context in which a policy is designed and implemented should vary from person to person which should deal effectively with context-specific issues which motivate HRH11.
The survey results also found that the ZHWRS lacks a comprehensive multi-sectoral rural implementation plan and policy which health workers regarded as the greatest negative factor to improving their working conditions in rural and remote areas. Worse still, the human resource management system is weak and convoluted with bureaucratic structures that are negatively affecting the performance of health worker retention programmes. For instance, delays in payments and placement on payroll are common8. Also, the Government has been rigid in facilitating the decentralisation process of administrative procedures so that more decision making power can be allotted to lower levels of the management. Yet, these lower levels lack the management skills to ensure efficient outcomes are achieved. The simplification and harmonisation of incentives with government loan procedures is also critical but neglected2.
To address the difficulties arising with the ZHWRS, non-financial incentives should include career paths, stimulating training and encouraging deployment through investment in services, providing better housing loans and greater reward of work performances.
While MOH recruits and posts health workers to poorer areas of the country, inferior conditions and out-migration leads to a paradoxical situation of staffing gaps. This pushes health workers to seek employment in the international market. Push and pull factors for migration include poor remuneration12, poor working conditions with limited supplies and no supervision, heavier workloads in rural public facilities13, limited career and educational opportunities for workers and their families, and poor communication14.
Other Financial Incentive Schemes for Health workers
The literature on other health worker retention schemes reports mixed success in achieving programme aims. National schemes that commit students to service requiring scholarships and educational loans with service requirements have significantly lower recruitment sizes than national schemes that commit health workers after their training by offering direct financial incentives and loan15. Elsewhere, it has been shown that students who find careers in primary care appealing at admission into medical school develop a strong interest in highly specialized health care during their training which depends on technology that is usually not available to underserved areas16. Additionally, evidence indicates that participants in financial incentive schemes significantly prefer to leave their first placed sites after completion of their obligation, compared to similar non obligated health workers. However, retention scheme participants are more likely to practice in some underserviced areas or to work with an underserved population than their peers16.
Other studies show considerable difference in the level of satisfaction with participants more satisfied than non-participants with their work and personal life in underserviced areas16. Lack of satisfaction with work and personal life in underserviced areas affect the likelihood of sharing experiences with colleagues and health care delivery17. Elsewhere it was found that lack of interaction with participants during different stages of programme enrollment, during selection, preparation of the participants and their families before the start of the obligated service affect scheme adversely affect uptake18–19. Another difficulty arising with retention schemes is a lack of career guidance, mentoring, monitoring of problems, and on going support during the obligatory period of rural service. Another study found that participating health workers deter non-participants from practice in underserviced communities because the participants compete with non-participants for patients and practice personnel16. Another study concludes that many incentive programmes have achieved their primary goal of short term recruitment but have had less success with long term retention15.
Conclusions
The MoH in Zambia is severely affected by a drastic human resource for health shortage. In spite of some minor success registered by the ZHWRS, the crisis of the shortage of human resources for health is an ongoing and massive challenge to the MoH. It needs to develop pragmatic policies that will address and solve the problem. Both rural and urban areas are understaffed. The main aim of retention schemes like the ZHWRS is to decrease attrition rates and increase recruitment of critical health care service providers, especially in rural and remote areas. The current scheme is not yet achieving even the modest aims that government has set it.
Table 2.
Health worker cadres surveyed (n=234)
| Registered | Paramedics | Registered & | Medical | Doctors | Clinical |
| & Enrolled | Enrolled Nurses | Assistants | Officers | ||
| Midwives | |||||
| 33 | 56 | 116 | 14 | 7 | 8 |
| 14% | 24% | 51% | 5% | 3% | 3% |
Acknowledgements
This research was funded by the agreement that HEARD had in the years (2006–2010) through the Joint Financing Agreement (JFA) with the following donors: Norwegian Ministry of Foreign Affairs, Sida, Irish Aid, DFID, UNAIDS and Koninkrijk der Nederlanden
References
- 1.Ministry of Health, author. Human Resources for Health Strategic Plan: 2006 – 2010. Lusaka: Ministry of Health; 2005. [Google Scholar]
- 2.Mwale H. Human Resources for Health Innovations in Zambia: A Case Study of the Zambia Health Workers Retention Scheme. Geneva: World Health Organization; 2009. [Google Scholar]
- 3.Ministry of Health, author. Scale Up Plan for the Human Resources Retention Scheme. Lusaka: Ministry of Health; 2007. [Google Scholar]
- 4.World Health Organization, author. The World Health Report 2006: Working Together for Health. Geneva: World Health Organization; 2006. [Google Scholar]
- 5.Ministry of Health, author. 2008 Annual Health Statistical Bulletin. Lusaka, Zambia: Ministry of Health; 2009. [Google Scholar]
- 6.Tjoa A, Kapihya M, Libetwa M, Schroder K, Scott K, Lee J, McCarthy E. Meeting Human Resources for Health Staffing Goals by 2018: A Quantitative Analysis of Policy Options in Zambia. Human Resources for Health. 2010;8:15. doi: 10.1186/1478-4491-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ministry of Health, author. Mid-Term Review of the Zambia National Health Strategic Plan NHSP IV, 2006–2010. Lusaka, Zambia: Ministry of Health; 2008. [Google Scholar]
- 8.Koot J, Martineau T. Mid Term Review of Zambian Health Workers Retention a. Scheme (ZHWRS) 2003–2004. Lusaka, Zambia: Ministry of Health; 2005. [Google Scholar]
- 9.Mwale H, Smith S. Human Resources Retention Scheme: Qualitative and Quantitative Experience from Zambia. Lusaka: World Health Organisation (WHO); 2008. [Google Scholar]
- 10.University of Aberdeen, author. Health Worker Incentives Survey (HWIS) Aberdeen: University of Aberdeen; 2007. [10 June 2010]. www.immpactinternational.org/toolkit/ [Google Scholar]
- 11.Campbell D, Caffrey C. Zambia: Taking Forward Action on Human Resource for Health with DFID/OGAC and Other Partners. Chapel Hill, NC: Capacity Project; 2009. [Google Scholar]
- 12.Awases M, Gbary A, Nyoni J, Chatora R. Migration of Health Professionals in Six Countries: A Synthesis Report. Brazzaville, Democratic Republic of Congo: World Health Organisation (WHO) Regional Office for Africa; 2004. [Google Scholar]
- 13.Hagopian A, Thompson M, Fordyce M, Johnson K, Hart L. The Migration of Physicians from sub-Saharan Africa to the United States of America: Measures of the African Brain Drain. Human Resources for Health. 2004;2:17. doi: 10.1186/1478-4491-2-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iipinge S, Dambisya M, Loewenson R, Chimbari M, Ndetei D, Munga M, Sibandze S, Lugina H. Policies and incentives for health worker retention in east and southern Africa: Learning from country research. Harare, Zimbabwe: University of Namibia, Training and Research Support Centre, University of Limpopo, EQUINET, ECSA-HC, EQUINET Discussion Paper 78 EQUINET; 2009. [Google Scholar]
- 15.Pathman D, Fryer E, Phillips L, Smucny J, Miyoshi T, Green L. National Health Service Corps staffing and the growth of the local rural non-NHSC primary care physician workforce. Rural Health. 2006;22(4):285–293. doi: 10.1111/j.1748-0361.2006.00048.x. [DOI] [PubMed] [Google Scholar]
- 16.Barnighausen T, Bloom D. Financial incentives for return of service in underserved areas: a systematic review. BMC Health Services Research. 2009;9:86. doi: 10.1186/1472-6963-9-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ndetei M, Khasakhala L, Omolo J. Incentives for health worker retention in Kenya: An assessment of current practice. EQUINET Discussion Paper 62. Harare, Zimbabwe: AMHF, EQUINET, ECSA-HC; 2008. [Google Scholar]
- 18.Lehmann U, Dieleman M, Martineau T. Staffing remote rural areas in middle- and low-income countries: A literature review of attraction and retention. BMC Health Services Research. 2008;8:19. doi: 10.1186/1472-6963-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dieleman M, Cuong V, Anh V, Martineau T. Identifying factors for job motivation of rural health workers in North Viet Nam. Human Resources for Health. 2003;1:10. doi: 10.1186/1478-4491-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mangham L, Hanson K. Employment preferences of public sector nurses in Malawi: results from a discrete choice experiment. Tropical Medicine and International Health. 2009;13(12):1433–1441. doi: 10.1111/j.1365-3156.2008.02167.x. [DOI] [PubMed] [Google Scholar]