Abstract
Over the last two centuries, treatment of hip pathology has evolved from joint excision and osteotomies to modern total hip arthroplasty (THA), which is considered one of the most successful surgical interventions ever developed. We here review the history of hip procedures that preceded Themistocles Glück. This evaluation reminds us of the ephemeral nature of human industriousness and how medical research and procedures are not isolated developments but correlate to the social, economical, and cultural framework of their time.
John Rhea Barton (1794–1871) in Philadelphia, PA, USA, is credited with performing the first osteotomy on an ankylosed hip in 1826 [1–3]. He performed an intertrochanteric osteotomy without anesthesia in only seven minutes. After 20 days, he manipulated the extremity to provoke a fibrous reaction at the ends of the severed bone, and thus created a pseudarthrosis. The patient, John Coyle, and was a sailor.
Portrait of John Rhea Barton
Joint excision was first practiced for many types of joint diseases. The enthusiasm shown at that time for joint excision was, as with all surgical innovations, the result of special circumstances. It was a reaction to the appalling frequency with which amputation was being practiced in Europe and America. Liverpool, in the UK, had gained notoriety for its skilled surgeons: Henry Park (1744–1831) worked at The Royal Infirmary [10]. Liverpool was a large commercial port, and sailors arrived with wounded limbs, in many instances injured months earlier. These types of injuries required radical treatment, which in the late 1700s meant amputation. Amputation of the extremity in these cases often offered a simple but, as Park thought, unnecessary solution to the problem. In a letter to his teacher, Percival Pott (1717–1788), Park described his principles of treatment: “The resource I mean is the total extirpation of the articulation, or the entire removal of the extremities of all the bones which form the joints, with the whole, or as much as possible of the Capsular Ligament; thereby obtaining a cure by means of Callus.”
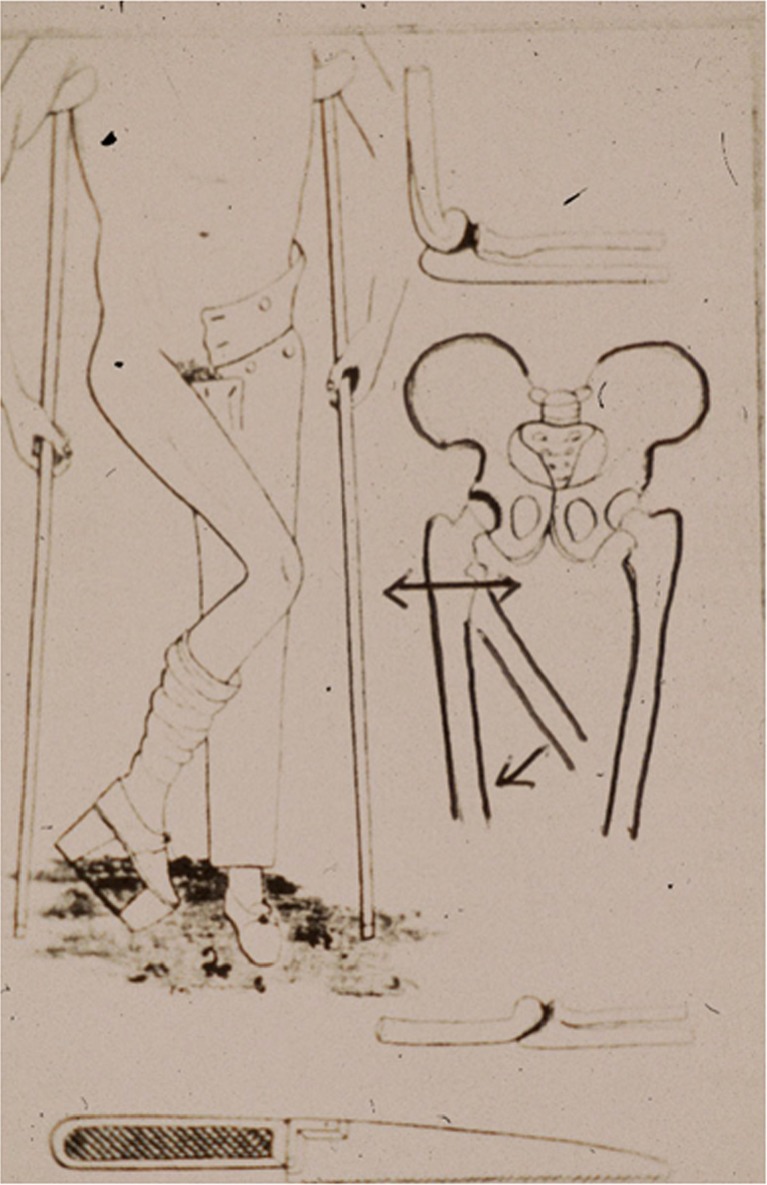
Osteotomy performed on John Coyle (drawing by John Rhea Barton)
Anthony White (1782–1849) of the Westminster Hospital in London is credited [11] with the first excision arthroplasty in 1821 though he did not make a personal report. This procedure ameliorated pain and preserved mobility but at the expense of stability. It was this technique that gained him recognition in the medical community, as described in his obituary that appeared in the Lancet.
John Rhea Barton residence, northwest corner of Broad and South Streets; watercolor drawing, watercolor and India ink, original paper signed Frank H. Taylor
John Rhea Barton was born in Lancaster, PA, USA, in 1796 and was of a distinguished ancestry. His grandfather was the Reverend Thomas Barton; his father was William Barton, named one of the judges for the Western Territory by General George Washington. He moved to Philadelphia, PA, and became secretary for the American Philosophical Society. The Barton name was synonymous with the sciences: “From Benjamin Barton, nephew of Rittenhouse born in 1766, down through John Rhea Barton, who died in 1871; the Bartons were the hereditary Old Philadelphia scientific family.” John Rhea Barton studied at the Pennsylvania Hospital, graduating in 1818. Shortly thereafter, he began teaching at the Pennsylvania Hospital and became surgeon at the Philadelphia Almshouse, established in 1729 as the first institution in the American Colonies to provide hospitalised care for the poor. He worked for Philip Syng Physick (1768–1837), the father of American Surgery, who had been a student of John Hunter (1728–1793) in London, UK. It was said that Barton was ambidextrous and that once he had positioned himself for an operation, he did not move about. From 1823 he was a surgeon at the Pennsylvania Hospital. The daring and skill with which Barton executed his surgical operations aroused the envy and admiration of his colleagues and was the theme of many anecdotes. The high point of his fame came in 1826, when executed an osteotomy for ankylosis in the hip in seven minutes. The patient, John Coyle and was a sailor. Barton first excised the femoral head, neck and trochanters, and the patient survived the operation for 12 years. Barton also examined the possibilities of connecting the broken pieces through etching mediums in cases of unhealed fractures. Barton is best known as the originator of the corrective osteotomy for joint ankylosis. He performed a femoral osteotomy between the greater and lesser trochanters to secure motion in an ankylosed hip. This has been called the first successful arthroplasty. Barton’s surgery was reported in the North American Medical and Surgical Journal: “He divided the bone through the great trochanter and part of the neck of the bone, extended the adducted limb and dress the wound. After the irritation from the operation shall have passed away, to prevent, if possible by gentle and daily movement of the limb, the formation of bony union, and to establish an attachment by ligament only, as in cases of ununited (sic) fractures, or artificial joints as they are called”. Three months after the operation, the patient walked reasonably well with a cane, but six years later all motion had been lost. Barton provided the first evidence that motion prevented bone fusion. However, his surgery popularised hip osteotomy as a rational plan for overcoming bony ankylosis, a hitherto untreatable lesion. Although there were some spectacular successes, outcomes were generally disconcertingly unpredictable. Most joints eventually became ankylosed, a disappointing outcome for the perilous procedure that had a mortality rate of approximately 50 %, high even by the standards of the day.
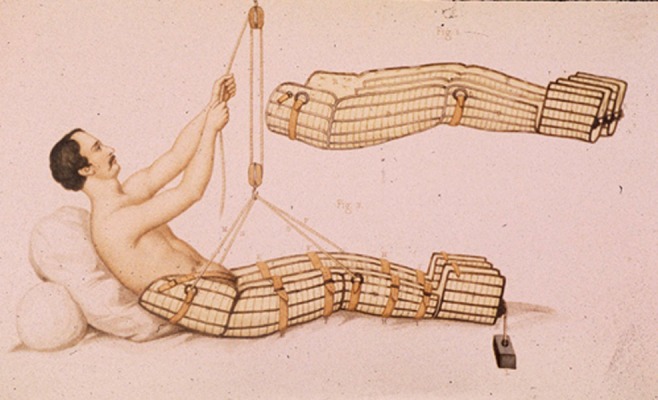
Rehabilitation performed at this period
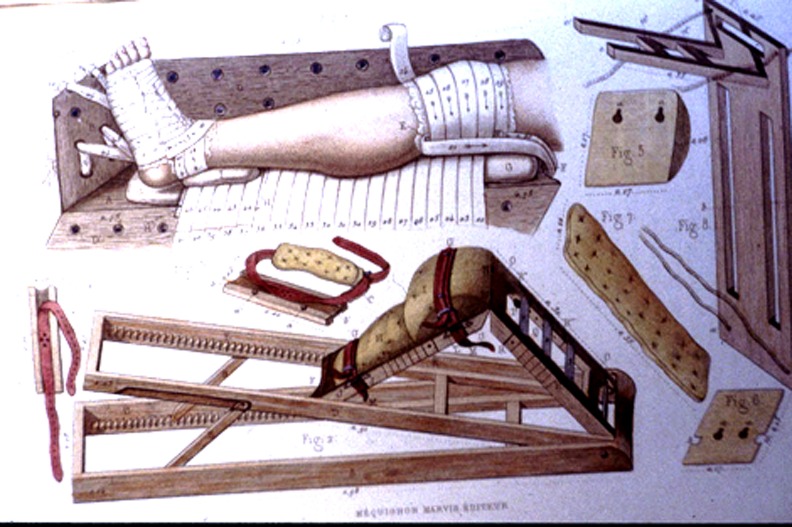
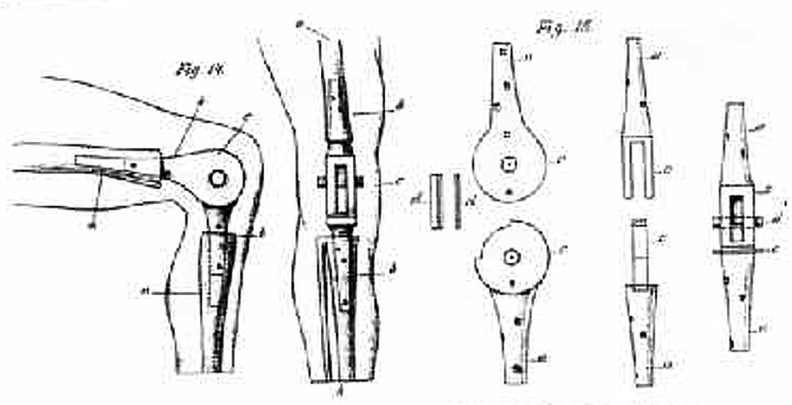
Devices for rehabilitation at this period
Portrait of Auguste Stanislas Verneuil (1823–1895)
Carnochan (1840) of New York, NY, USA, was the first surgeon who thought that the hip joint could also be replaced. He inserted a wooden block between the damaged ends of a hip joint and later, several other biological and foreign materials were used. These included skin, fascia, muscle, pig bladder, and gold foil, all of which were painful failures. Auguste Stanislas Verneuil (1823–95), of Paris, France, performed soft-tissue hip interpositions in 1860. Aristide Auguste Stanislas Verneuil (1823–1895), French physician and surgeon, studied medicine in Paris under Jacques Lisfranc de St. Martin (1790–1847), Pierre-Antoine-Ernest Bazin (1807–1878), Charles-Pierre Denonvilliers (1808–1872) and Joseph-François Malgaigne (1806–1865). Léopold Ollier (1830–1900) [9] worked at the Hôtel-Dieu hospital in Lyon, France, generating tremendous interest in the concept of interpositional arthroplasty. In 1885, he described the interposition of adipose tissue in uninfected joints. However, he did not fix the interposed material to the subjacent bone, and his procedures were generally ineffective. Subsequently, Czech surgeon Vitezlav Chlumsky (1867–1943), working in Breslau, Germany (now Wroclaw, Poland), systematically experimented with many interpositional materials [5]. Among the wide variety were muscle, celluloid, silver plate, rubber struts, magnesium (which fomented exactly the opposite effect of what was expected—this being consolidation of bone osteotomies or fractures), zinc, glass, pyres, decalcified bones, wax and celluloid. His earliest implantations of artificial joints are variously reported as the mid-1880s to 1890. During this period, it became obvious that simple joint resection barely improved the patient’s life. The resected joint, or rather what remained of it after the resection, was painful, unstable and in need of sturdy braces.
Portrait of Murphy
Around the turn of the century, another approach (perhaps more reasonable at this period) was advocated by John Benjamin Murphy (1857–1916) from Chicago, IL, USA, for localised osteoarthritis of the hip joint. He described neither implant surgery nor resection but simply removal of overhanging bone osteophytes from the base of the head of the femur and the rim of the acetabulum, a procedure described as hip cheilotomy [7, 8].
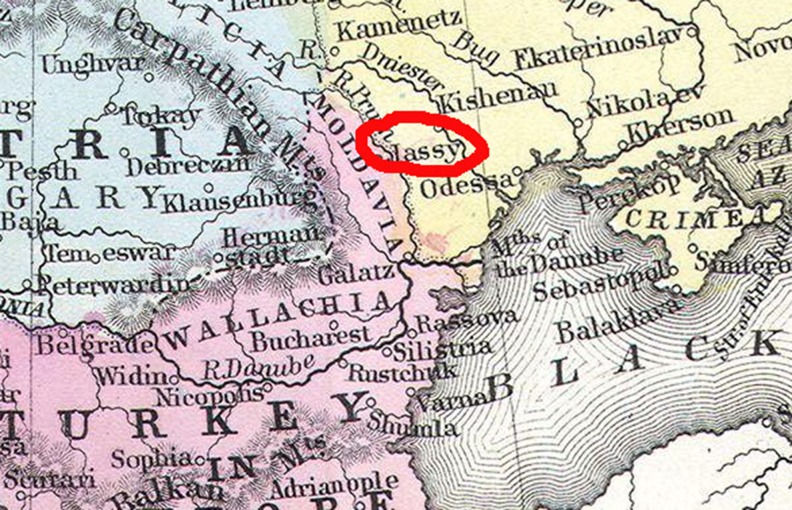
Themistocles Glück (1853–1942) led the way in the development of hip implant fixation [4]. After the death of two of their children in Germany, his parents started a new life in Iasi, Moldovia (now Romania). Iasi (German Jassy) is a university town in northeastern Romania, in the region of Moldova and the capital of the district of the same and was the most important city of the Principality of Moldavia . Glück was born in Iasi, where his father, a doctor, later became physician to the Romanian King Charles I. In 1864, the Glücks sent their son to a German school—Mary Magdalene School—in Wroclaw. After high school, in 1873, he studied medicine in Leipzig and after 1875 in Berlin. Rudolf Virchow, Bernhard von Langenbeck and Ernst von Bergmann were his teachers. After taking the state examination in 1876, he became a military physician during the Russian–Ottoman war. From 1878 to 1884, he was assistant to Langenbeck in Berlin. Glück was an excellent student and won a prize for research on nerve regeneration, which he conducted under the supervision of Virchow. His interest in bone defects was almost certainly encouraged by his work as a wartime surgeon in the Balkans in 1877 and 1885. During the Serbian–Bulgarian war (1885–1886) Glück fixed the ends of a fractured femur with two steel plates secured to the bone with screws. He was amazed at how early the injured limb could resume movement. Around this time, he replaced a portion of a mandible resected for cancer with a steel plate fixed to the bone with screws, with an excellent result. He was unable to continue a university career because von Langenbeck retired and his replacement, von Bergmann, found no position for him. He returned to his homeland and worked for a short time in Bucharest, then practiced industrial medicine in Berlin until 1890, when he was appointed head of surgery at the Emperor and Empress Friederich Paediatric Hospital. In 1890, he was named surgical chief physician to the new Emperor and Empress Frederick Hospital in Berlin-Wedding.
Professor Themistocles Glück (1853–1942)
Map of Moldavia in 1860
Map of Europe in 1860
Several surgeons already had the insight that the free space left after removal and resection of the diseased joint might be filled with an artificial joint. One such surgeon was the Russian N.I. Pirogow, who in 1830 proposed the replacement of a tuberculous knee with an artificial joint made of ivory. However, Glück was thhe first surgeon to replace not one but many tuberculous joints using artificial joints made from ivory. Remarkably, he designed and implanted artificial wrists, elbows, shoulders, hips, knees and ankles. In 1991, German orthopaedic surgeon Wessinghage traced 14 total joint replacements carried out by Glück during the 1880s that were described in Glück’s publications [6]; five were still functioning in 1891: three total knee replacements, one elbow and one total wrist replacement. All total joint replacements were made from ivory. For fixation inside the marrow cavity, Glück often used a special form of very hot “bone cement” that hardened within one minute. In 1890, he was due to present his arthroplasty work to the tenth international surgical congress in Berlin. He believed that people needed to visualise ideas before they could be convinced of their value. He therefore had a complete skeleton fitted with his various arthroplasties, which by now included the wrist, elbow, shoulder, ankle, hip and knee. This became famous as the “skeleton of Paris” and was exhibited until the World War II, when it disappeared into Russia along with the famous Berlin Medical Collection.
After Glück’s lecture in 1890, there came a severe clash with his chief, Professor von Bergman, new head of the Berlin surgical clinic. Behind it was von Bergman’s disappointment with the failure of treatment of his own patients with Koch’s disease and his disillusionment with all things that may mean progress of surgery. Von Bergman forced Glück to publish a repentant declaration, in which Glück retracted his results with total joint replacement, his recommendations for the method and his ideas for further development of total joint replacement. Although Glück’s joint replacements were spectacularly successful in the short term, they all ultimately failed because of chronic infection. A report of five cases was published, all tuberculous joints. Three prostheses were subsequently removed, but one knee and one wrist replacement were left in situ despite fistula formation. Glück, a rigid follower of asepsis, later realised that prior joint infection was a contraindication to joint replacement. Due to the opposition of his colleagues, Glück stopped this work altogether and abandoned his presentation to the international congress. He wrote in his open retracting letter that replacing joints affected by active tuberculosis was erroneous because the infection recurred. He took full responsibility for this mistakes. He then sank into oblivion. Where Glück failed was in the choice of materials and in the choice of patients. However, these failures were also due to the period in which he lived and worked. His total joint replacement operations were a splendid idea done on the wrong patients and at the wrong time. Even in modern times, with the availability of antibiotics to treat the tuberculis joint, total replacement of joints damaged by tuberculosis infection is very difficult. Modern materials, such as stainless steel, cobalt chrome and titanium alloys lay in the distant future. Nevertheless, Glück was the first to develop the idea of biocompatibility—foreign materials for total joint replacement must be well tolerated by the patient’s body.
Total knee joint by Glück: a modular hinge made from ivory
The dismissal of Glück’s work on joint replacement did not diminish his enthusiasm for research in other areas of medicine. He described several surgical operations, including laryngectomy, preventive resection of the trachea, lung resection and use of a plate for the repair of inguinal hernias. He also wrote on the treatment of thrombophlebitis and peritonitis, investigation of kidney function, chemotherapy and functional orthopaedics. He recognised that experimental surgery on various animal species was the only way to achieve decisive progress. Only after extensive and successful animal trials were total joint replacements carried out in human patients. In his later years, Glück was honoured for his work. In 1922 he was made an “extraordinary professor” and, in 1930, at the age of 77, he was invited to join the honour roll of the German Surgical Society. On his 80th birthday, a special biography was published by the German orthopaedic surgeon Fritz Lange. Glück died aged nearly 90 on 25 April 1942 in Berlin. For his work on nerve suture and regeneration, he received the first State Prize of the Berlin University. French surgeons Louis Léopold Ollier and Jules Péan had already recognised Glück’s importance in the 1890s. With his throat surgery, he gained an international reputation. However, it was only in 1922, at age 70, that he was appointed associate professor, and he was even nominated for the Nobel Prize. The German Surgical Society awarded him an honorary membership, and since 2000, the German Society for Orthopaedics and Orthopaedic Surgery annually present the Themistocles Glück Award for Arthroplasty.
References
- 1.Barton JR. On the treatment of anchylosis, by the formation of artificial joints. North Amer Med and Surg Jour. 1827;3(279):400. [PMC free article] [PubMed] [Google Scholar]
- 2.Barton JR. Am J Med Sci. 1837;21:336–339. [Google Scholar]
- 3.Barton JR. On the treatment of ankylosis by the formation of artificial joints. 1827. Clin Orthop Relat Res. 2007;456:9–14. doi: 10.1097/BLO.0b013e31803254fd. [DOI] [PubMed] [Google Scholar]
- 4.Brand R, Mont M, Manring M. Themistocles Glück 1853–1942. Clin Orthop Relat Res. 2011;469:1525–1527. doi: 10.1007/s11999-011-1836-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chlumsky V (1896) Zentralblatt für or thopaedische Chirurgie (Continued Centralblatt für orthopaedische Chirurgie un mechanik from 1887–1890)
- 6.Glück T. Referat uber die durch das moderne chirurgische Experiment gewonnenen positiven Resultate, betreffend die Naht und den Ersatz von Defecten ho¨herer Gewebe, sowie u¨ber die Verwethung resorbirbarer und lebendiger Tampons in der Chirurgie. Arch klin chir. 1891;41:187–239. [Google Scholar]
- 7.Murphy JB. Trans Amer Surg Ass. 1904;22:213. [Google Scholar]
- 8.Murphy JB (1915) Cheilotomy. Surgical Clinics of Jhon B. Murphy. Vol IV. Philadelphia: Sanders
- 9.Ollier L (1885) Traité des Résections et des opérations conservatives qu’ont peut practiquere sur le systême osseux. Paris
- 10.Park H (1782) An account of a new method of treating diseases of the joints of the knee and elbow. In: Pott MP (ed) London [PMC free article] [PubMed]
- 11.Anthony W. Obituary. Lancet. 1849;1:324. [Google Scholar]