Abstract
Background
High tibial osteotomy and unicompartmental knee arthroplasty are surgical treatment options for unicompartmental knee arthritis; these procedures are indicated for patients who do not have severe arthritis in the lateral compartment. Valgus stress radiographs sometimes are used to make this evaluation, but this test has not been critically evaluated.
Questions/purposes
We sought to determine (1) whether valgus stress radiographs help to evaluate the integrity of the cartilage in the lateral compartment in patients undergoing TKA for noninflammatory arthritis, and (2) whether valgus stress radiographs can identify patients whose varus deformity is correctable.
Methods
We reviewed preoperative hip-to-ankle standing radiographs, AP standing radiographs, and valgus stress radiographs of 84 patients (91 knees) who underwent TKA for varus knee arthritis between July 2010 and January 2012. Valgus stress radiographs were obtained with the patient supine with the knee 20° flexed and a firm manual valgus force was applied through the knee. On valgus stress radiographs, the lateral compartment joint space width and the corrected mechanical alignment were measured. Intraoperative cartilage assessment (Outerbridge grade) was compared with lateral compartment joint space width. Knees with mechanical leg alignment of 3° varus to 3° valgus on valgus stress radiographs were considered correctable deformities.
Results
The lateral compartment joint space width on valgus stress radiographs did not correlate with the intraoperative Outerbridge grading of the lateral compartment cartilage (rs = −0.154; p = 0.146). The majority of knees (93%; 55 of 59) with 10° or less mechanical varus on hip-to-ankle standing radiographs were correctable within the range of 3° varus to 3° valgus.
Conclusions
Valgus stress radiographs provided no added benefit to the radiographic assessment of the lateral compartment cartilage and regarding the correctability of the varus deformity.
Level of Evidence
Level III, diagnostic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
Arthritis is a common and severe musculoskeletal disease causing a high economic burden on society. It has been suggested that by 2020 approximately 59 million people in the United States will be affected by degenerative joint disease [7].
High tibial osteotomy and unicompartmental knee arthroplasty (UKA) are surgical treatment options for unicompartmental knee arthritis [25]. For high tibial osteotomy and UKA, intact cartilage of the lateral compartment is important [12]. The radiographic assessment of lateral compartment cartilage in medial knee arthritis is difficult. Previous studies have described poor sensitivity of the Kellgren-Lawrence grading scale [14] on AP standing radiographs [3, 29]. To improve the accuracy, valgus stress radiographs have been used to identify patients with arthritis in the lateral compartment [11, 12].
In UKA, the angular deformity should be passively correctable and soft tissue releases bear the risk of overcorrection and therefore should be avoided [8, 12, 13, 18]. Valgus stress radiographs have been described as an option to preoperatively assess the ability to correct varus deformities in medial knee arthritis [2, 12]. Despite these potential benefits in addition to AP standing radiographs, valgus stress radiographs are not routinely obtained in clinical practice [9, 26].
To the best of our knowledge, the clinical value of the valgus stress test in the preoperative radiographic assessment for UKA and high tibial osteotomy has not been described in the literature. This is the first study to assess valgus stress radiographs in a large number of patients. We sought to determine (1) whether valgus stress radiographs help to evaluate the integrity of the cartilage in the lateral compartment in patients undergoing TKA for noninflammatory arthritis, and (2) whether valgus stress radiographs can identify patients whose varus deformity is correctable.
Patients and Methods
We prospectively studied a series of all 97 knees in 84 patients who underwent primary TKA for varus noninflammatory arthritis of the knee between July 2010 and January 2012. Each patient received a preoperative standardized AP hip-to-ankle standing radiograph, an AP standing knee radiograph, and a valgus stress radiograph. All images were stored in a generic DICOM format.
The exclusion criteria were defined as secondary OA and neutral or valgus alignment observed on hip-to-ankle standing radiographs. Patients were prospectively enrolled in this study. Six patients were retrospectively excluded because not all radiographs were on file, leaving 78 patients (91 knees; 45 right knees and 46 left knees). There were 34 men and 44 women, who underwent 65 unilateral, 10 bilateral, and three staged bilateral procedures. The mean age of the patients was 69 years (range, 50–89 years), and their mean BMI was 25.7 kg/m2 (range, 17–45 kg/m2). The study was approved by the institutional review board and all patients consented to participate in the study before surgery.
All radiographs were obtained after standardized institutional protocols. Hip-to-ankle standing radiographs and AP standing radiographs were corrected for effects of magnification through a scale and a 25-mm metal calibration sphere, respectively. Valgus stress radiographs were obtained in the radiology department of the authors’ institution on conscious patients, without anesthesia, who were in the supine position with a wedge under the knee to achieve an approximate flexion of 20° and to relax the posterior capsule [22]. The senior author (FB) manually applied a firm valgus force through the affected knee, paying special attention to neutral rotation and keeping the tibia plateau parallel to the x-ray beam. For valgus stress radiographs, calibration was achieved by measuring the width of the tibia on corresponding AP standing and valgus stress radiographs and mathematical correction of joint space width.
The grading and all measurements were performed on a picture archiving and communication system (PACS) with commercial planning software (Sectra IDS7; Sectra, Linköping, Sweden).
The grading according to the Kellgren-Lawrence grading scale [14] for the lateral compartment was performed on AP standing radiographs.
On hip-to-ankle standing radiographs, the hip-knee-ankle angle was defined as the angle between the femoral mechanical axis (center of hip to center of knee) and the tibial mechanical axis (center of knee to center of ankle) [19–21]. In the current study, the mean hip-knee-ankle angle was 8.3° (95% CI, 7.4°–9.1°) varus. The distal lateral femur angle was defined as the angle between the femoral mechanical axis and the line connecting the most distal points of the medial and lateral femur condyles [4]. The proximal medial tibia angle was defined as the angle between the tibial mechanical axis and the best-fit line along the surface of the tibial plateau [24].
On valgus stress radiographs, medial and lateral joint space width was measured parallel to the tibial shaft axis from the midpoint of the medial and lateral femoral condyles to the tibial plateau [6] (Fig. 1). In the current study, valgus forces compressed the mean lateral joint space width by 1.5 mm (95% CI, 1.1–1.8 mm) to a mean lateral joint space width of 5.1 mm (95% CI, 4.8–5.5 mm). The mean medial joint space width increased by 4.4 mm (95% CI, 4.0–4.8 mm) to 6.0 mm (95% CI, 5.7–6.3 mm). The applied manual force compressed the lateral joint space width by 23% and increased the medial joint space width by 73% which compares favorably with a previously described standardized method of applying 15 kilopond (approximately 140 N) of force through a device [28].
Fig. 1A–B.
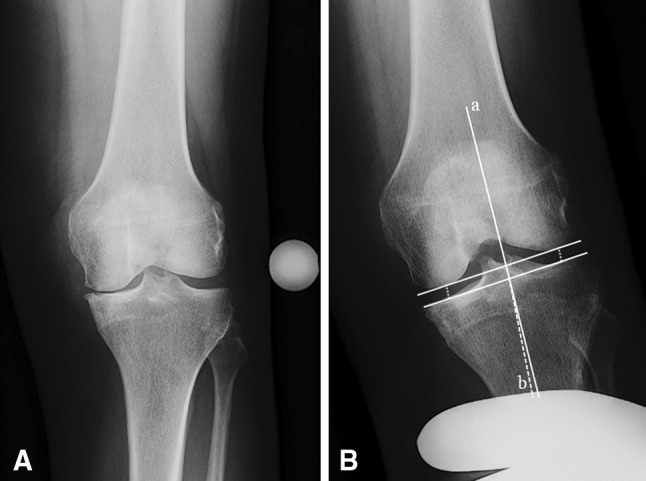
(A) A standardized left AP standing radiograph shows the knee of a 79-year-old woman with Kellgren-Lawrence Grade 3 osteoarthritis in the medial compartment and Grade 1 in the lateral compartment, respectively. (B) The corresponding valgus stress radiograph shows the measurements of the medial (5.7 mm) and lateral (5.4 mm) joint space width and the correctability of the varus deformity as an angle between axis a and b, respectively. Manual valgus force corrected the deformity to 1° varus.
Knees which corrected to a mechanical leg alignment within the range of 3° varus to 3° valgus on stress films were defined as correctable. Varus knees in which valgus force resulted in greater than 3° valgus were considered overcorrected and varus knees corrected to less than 3° varus were considered undercorrected, respectively.
To measure the degree of correction on the valgus stress test we identified the most distal points of the medial and lateral femur condyles [4] and reconstructed the mechanical axis of the femur based on the lateral distal femur angle (hip-to-ankle standing film). In a similar technique, the mechanical axis of the tibia was determined based on a line along the surface of the tibial plateau [24] and the proximal medial tibia angle retrieved from the hip-to-ankle standing film. This method allowed determining the femoral mechanical axis and the tibial mechanical axis on valgus stress radiographs. The degree of correctability was defined as the angle between these two axes (Fig. 1).
The Outerbridge grading scale [23] was used for direct intraoperative cartilage assessment of the lateral compartment. The senior author (FB) evaluated the cartilage condition of the central 75% weightbearing portion of the lateral tibia and femur which was confirmed by intraoperative photo imagery.
Intraobserver and interobserver reliabilities for measurements were assessed by two independent blinded observers (WW, JBM) for 20 randomly selected corresponding sets of radiographs. Intraobserver and interobserver reliabilities for the grading scores also were evaluated by two independent blinded observers (WW, FB) for all radiographs. For intraobserver reliabilities, grading and measurements were performed at two occasions separated by a minimum of 4 weeks. Single measures are given for intraobserver calculations and average measures for the interobserver calculations. Excellent intraobserver and interobserver intraclass correlation coefficients (ICCs) were observed for all parameters analyzed (Table 1).
Table 1.
Interobserver and intraobserver ICC for analyzed parameters
| Parameter | Interobserver ICC | Intraobserver ICC |
|---|---|---|
| Kellgen-Lawrence lateral (n = 91) | 0.873 | 0.905 |
| Hip-knee-ankle angle on hip-to-ankle radiographs (n = 20) | 0.999 | 0.994 |
| Correctability (n = 20) | 0.924 | 0.911 |
| Lateral joint space width on valgus stress radiographs (n = 20) | 0.994 | 0.871 |
| Medial joint space width on valgus stress radiographs (n = 20) | 0.984 | 0.942 |
ICC = intraclass correlation coefficient; Kellgren-Lawrence lateral = grading according to the Kellgren-Lawrence grading scale for the lateral compartment performed on AP standing radiographs; correctability = mechanical leg alignment on valgus stress radiographs.
The distributions of variables were tested in exploratory data analysis. A Kolmogorov-Smirnov test was used to identify normal distribution of the variables. Only hip-knee-ankle angle and medial joint space width on valgus stress radiographs were normally distributed (p = 0.138 to 0.2). For descriptive analysis, absolute mean values and differences of joint space width were expressed in millimeters with 95% CIs. Hip-knee-ankle angle was expressed in degrees with 95% CIs. Distributions of joint space width values were compared using the Mann-Whitney U test. A p value less than 0.05 was considered significant, and a p value less than 0.001 was considered highly significant. Correlation was classified as poor (0.00–0.20), fair (0.21–0.40), moderate (0.41–0.60), good (0.61–0.80), or excellent (0.81–1.00) [1]. Spearman rank correlation (rs) was used for nonparametric correlations. Outerbridge grades of the tibia and femur were combined to an Outerbridge grade of the lateral compartment. The higher grade on either the tibia or the femur determined the Outerbridge grade of the compartment. A two-way mixed model with 95% CIs was used for calculation of ICCs.
Statistical tests were performed using SPSS® 16.0 software for Windows® (SPSS Inc, Chicago, IL, USA).
Results
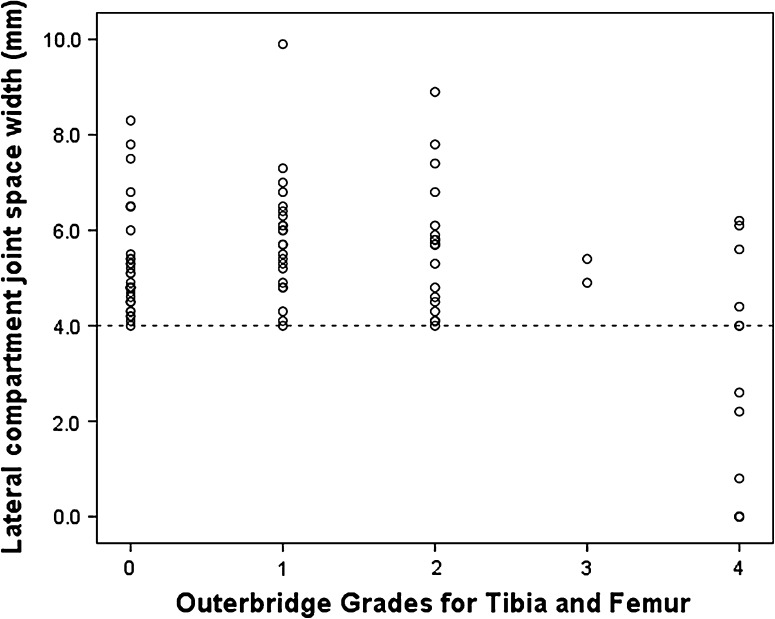
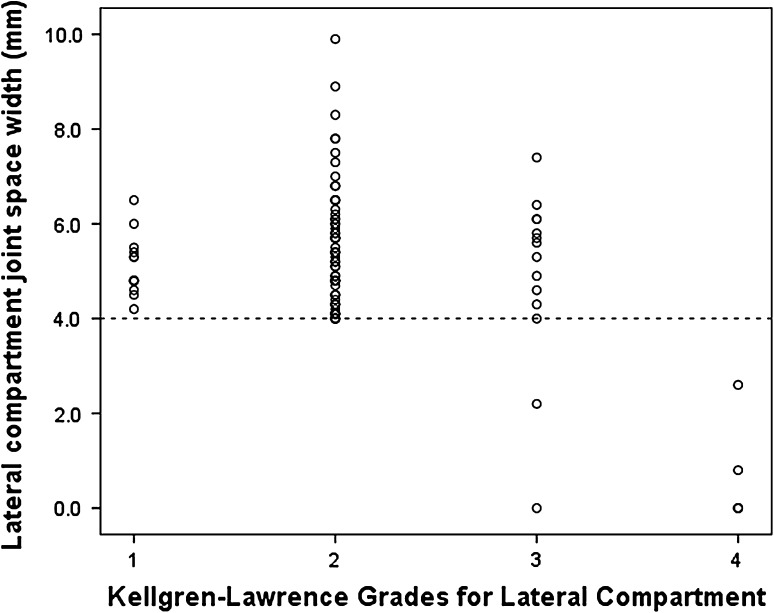
Arthritis severity in the lateral compartment as assessed on valgus stress radiographs did not correlate well with the appearance of the lateral compartment cartilage at surgery. There was a poor correlation (rs= −0.154; p = 0.146) between lateral joint space width and Outerbridge grades. All knees with an Outerbridge Grade of 0, 1, 2, or 3 maintained a joint space width of 4 mm or more. In seven knees (8%), the lateral joint space width measured less than 4 mm, but all these knees showed an Outerbridge Grade 4 in the lateral compartment. Even in knees with Outerbridge Grade 4, 46% showed a lateral joint space width of 4 mm or more (Fig. 2). On valgus stress radiographs, lateral joint space width was significantly (p = 0.005) higher in males than females and there was a weak but significant (rs= −0.208; p = 0.048) correlation between age and lateral joint space width. In the assessment of lateral compartment cartilage, valgus stress radiographs provided no benefit in addition to AP standing radiographs. All knees with a lateral Kellgren-Lawrence Grade 1 or 2 maintained a lateral joint space width of 4 mm or more on valgus stress radiographs. All knees with a lateral Kellgren-Lawrence Grade 4 had a lateral joint space width less than 4 mm (Fig. 3). There was a significant correlation (rs= 0.553; p < 0.001) between true cartilage damage as assessed at surgery and lateral Kellgren-Lawrence grades as assessed on AP standing radiographs.
Fig. 2.
A scatterplot illustrates the relationship between lateral compartment joint space width on valgus stress radiographs and intraoperative cartilage assessment (Outerbridge grading scale) of the lateral compartment for the entire cohort (n = 91). All knees with an Outerbridge Grade of 0, 1, 2, or 3 maintained a joint space width of 4 mm or more.
Fig. 3.
A scatterplot illustrates the relationship between the lateral compartment joint space width on valgus stress radiographs and Kellgren-Lawrence grades of the lateral compartment assessed on standing AP radiographs for the entire cohort (n = 91). All knees with a lateral Kellgren-Lawrence Grade 1 or 2 maintained a lateral joint space width of 4 mm or more on valgus stress radiographs. All knees with a lateral Kellgren-Lawrence Grade 4 had a lateral joint space width less than 4 mm.
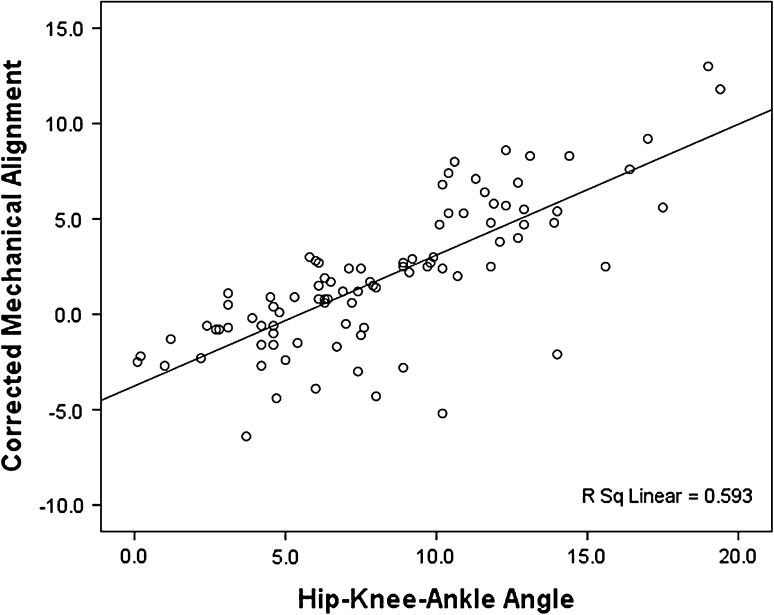
In knees with 10° or less mechanical varus on hip-to-ankle standing radiographs, the varus deformity was corrected to a mean of 0.1° (95% CI, −0.6 to 0.5) valgus on valgus stress radiographs. In knees with greater than 10° mechanical varus on hip-to-ankle standing radiographs, valgus force corrected the varus deformity to a mean of 5.5° (95% CI, 4.3–6.8) varus. The majority of knees (93%; 55 of 59) with 10° or less mechanical varus on hip-to-ankle standing radiographs corrected within the range of 3° varus to 3° valgus. Four knees overcorrected between 3.9° and 6.4° valgus and of these, one knee had a lateral Kellgren-Lawrence Grade 4 (6.4° valgus) and one knee had an Outerbridge Grade 4 (4.4° valgus), respectively. Of all knees with greater than 10° varus on hip-to-ankle standing radiographs, most (91%; 29 of 32) undercorrected between 3.8° varus and 13.0° varus and only one knee with advanced arthritis (lateral Kellgren-Lawrence Grade 4) overcorrected to 5.2° valgus. For the entire cohort, there was a significant correlation (rs = 0.761; p < 0.001) between the degree of correctability on the valgus stress film and the mechanical alignment on the hip-to-ankle radiograph (Fig. 4).
Fig. 4.
A scatterplot illustrates the relationship between the corrected mechanical alignment on valgus stress radiographs and the mechanical varus alignment (hip-knee-ankle angle) on hip-to-ankle radiographs for the entire cohort (n = 91). There is a significant correlation between the degree of correctability on the valgus stress radiograph and the mechanical alignment on the hip-to-ankle radiograph.
Discussion
Successful outcomes with UKA and high tibial osteotomy require strict observation of indications [5]. One of the most important factors influencing long-term survival is the condition of cartilage in the opposite femorotibial compartment [27]. To the best of our knowledge, the clinical value of the valgus stress test in the preoperative radiographic assessment for UKA and high tibial osteotomy has not been described in the literature. We therefore evaluated the clinical value of the valgus stress radiographs in patients with medial compartment arthritis by answering the following research questions: (1) Does the valgus stress test identify patients with lateral compartment arthritis? (2) Is the valgus stress test helpful in assessing the correctability of the deformity?
We acknowledge the following limitation: valgus stress radiographs were obtained through manual force and not through a more reproducible force applied via a device [9]. This method can lead to increased variability of valgus force, which consequently might impair accurate measurements. However, the valgus stress test is a common clinical test for evaluation of the medial collateral ligaments and most surgeons use the current technique in the physical examination of the knee in the preoperative assessment for UKA and high tibial osteotomy [12].
In our study, valgus stress radiographs provided no added benefit to AP standing radiographs in the preoperative assessment of lateral compartment cartilage damage in varus knees. The comparison of our results with those in the literature is limited because only two studies assessed the lateral joint space width in varus knees. Gibson and Goodfellow [11] were the first to decribe stress radiography in the preoperative assessment of UKA. Their study included 24 varus knees and they showed that knees with a lateral joint space width between 5 mm to 11 mm had intact cartilage at the time of surgery. They reported a mean joint space width of 8 mm, which is distinctly higher than the results in our study, but considering the low sample size and wide range of values there might have been a skew toward a higher mean joint space width. Tallroth and Lindholm [28] reported a mean lateral joint space width of 5.1 mm in a study of 30 knees with osteoarthritis predominantly in the medial compartment. They compared different modes of imaging but did not include a direct cartilage assessment, and concluded that valgus force compressed the lateral joint space width by 23% compared with AP standing radiographs.
Our study furthermore suggests that lateral joint space width as measured on valgus stress radiographs is a poor predictor of cartilage degeneration. This finding is in line with that of Fife et at. [10] who reported that 33% of patients whose radiographs showed tibiofemoral joint space narrowing on AP standing films had normal articular cartilage at arthroscopy. In addition to the influence of arthritis on joint space width, sex and age have to be considered. Higher joint space widths have been reported for men compared with women [16, 17], which was confirmed in our study. We also observed that the joint space width decreases with increasing age as previously reported [16]. Considering the results of our study and those from the literature, the previously suggested cutoff of 5 mm joint space width [11] on stress radiographs does not appear to be an accurate parameter to predict intact cartilage.
Valgus stress radiographs can assess the correctability of varus deformities. Our study is the first to assess the correctability of the mechanical alignment on valgus stress radiographs. We observed a strong correlation between the mechanical varus alignment on hip-to-ankle standing radiographs and the degree of correctability on valgus stress radiographs. With increasing severity of the varus deformity, the medial collateral ligament shortens and it becomes impossible to correct the deformity on valgus stress radiographs. However, in knees with less than 10° mechanical varus on hip-to-ankle standing radiographs, the majority of knees (93%) were corrected between 3° varus to 3° valgus. This finding supports the concept of considering only knees with less than 10° varus deformity for medial UKA [15]. Knees with minor varus deformity are more likely to be overcorrected on stress films and therefore attention has to be paid when using a spacer for intraoperative soft tissue balancing because of the risk of leaving these knees in valgus. However, because there were only two knees that corrected to more than 3° valgus, the valgus stress test provided little added information for UKA.
In knees that were correctable only to 3° varus on valgus stress radiographs, the technique of filling the medial femorotibial space with a spatula to reconstruct the native mechanical alignment may result in as much as 5° postoperative varus, assuming that removal of the spatula adds 2° varus to the mechanical leg alignment. When aiming for perfect postoperative mechanical alignment of neutral to 2° varus in UKA, the valgus stress test may be a helpful test to preoperatively assess the correctability and to adjust the operative technique accordingly. Alternatively, computer navigation and robotic surgery are procedures to achieve reproducible mechanical alignment.
We found that valgus stress radiographs provided no added benefit in the preoperative radiographic assessment of the lateral compartment in varus knees. Our approach involved use of a previously described method [6] in a large number of knees. In addition, the measurement method we used was reliable with excellent interobserver and intraobserver agreement. Valgus stress radiographs identified only advanced lateral compartment arthritis and offered no added benefit over AP standing radiographs and hip-to-ankle standing radiographs in the preoperative assessment for UKA and high tibial osteotomy.
Acknowledgments
We thank Michelle Perna BS and Danielle Perkins PA-C for assistance with the data collection.
Footnotes
The institution of the authors has received, during the study period, funding from Smith & Nephew, Inc (Memphis, TN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Altman DG. Practical Statistics for Medical Research. London, UK: Chapman & Hall; 1991. [Google Scholar]
- 2.Argenson JN, Chevrol-Benkeddache Y, Aubaniac JM. Modern unicompartmental knee arthroplasty with cement: a three to ten-year follow-up study. J Bone Joint Surg Am. 2002;84:2235–2239. [PubMed] [Google Scholar]
- 3.Brandt KD, Fife RS, Braunstein EM, Katz B. Radiographic grading of the severity of knee osteoarthritis: relation of the Kellgren and Lawrence grade to a grade based on joint space narrowing, and correlation with arthroscopic evidence of articular cartilage degeneration. Arthritis Rheum. 1991;34:1381–1386. doi: 10.1002/art.1780341106. [DOI] [PubMed] [Google Scholar]
- 4.Cooke TD, Scudamore RA, Bryant JT, Sorbie C, Siu D, Fisher B. A quantitative approach to radiography of the lower limb: principles and applications. J Bone Joint Surg Br. 1991;73:715–720. doi: 10.1302/0301-620X.73B5.1894656. [DOI] [PubMed] [Google Scholar]
- 5.Deschamps G, Chol C. Fixed-bearing unicompartmental knee arthroplasty: patients’ selection and operative technique. Orthop Traumatol Surg Res. 2011;97:648–661. doi: 10.1016/j.otsr.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 6.Down C, Xu Y, Osagie LE, Bostrom MP. The lack of correlation between radiographic findings and cartilage integrity. J Arthroplasty. 2011;26:949–954. doi: 10.1016/j.arth.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Elders MJ. The increasing impact of arthritis on public health. J Rheumatol Suppl. 2000;60:6–8. [PubMed] [Google Scholar]
- 8.Emerson RH, Jr, Head WC, Peters PC., Jr Soft-tissue balance and alignment in medial unicompartmental knee arthroplasty. J Bone Joint Surg Br. 1992;74:807–810. doi: 10.1302/0301-620X.74B6.1447238. [DOI] [PubMed] [Google Scholar]
- 9.Eriksson K, Sadr-Azodi O, Singh C, Osti L, Bartlett J. Stress radiography for osteoarthritis of the knee: a new technique. Knee Surg Sports Traumatol Arthrosc. 2010;18:1356–1359. doi: 10.1007/s00167-010-1169-2. [DOI] [PubMed] [Google Scholar]
- 10.Fife RS, Brandt KD, Braunstein EM, Katz BP, Shelbourne KD, Kalasinski LA, Ryan S. Relationship between arthroscopic evidence of cartilage damage and radiographic evidence of joint space narrowing in early osteoarthritis of the knee. Arthritis Rheum. 1991;34:377–382. doi: 10.1002/art.1780340402. [DOI] [PubMed] [Google Scholar]
- 11.Gibson PH, Goodfellow JW. Stress radiography in degenerative arthritis of the knee. J Bone Joint Surg Br. 1986;68:608–609. doi: 10.1302/0301-620X.68B4.3733839. [DOI] [PubMed] [Google Scholar]
- 12.Goodfellow J, O’Connor J, Dodd C, Murray D. Unicompartmental Arthroplasty with the Oxford Knee. Oxford, UK: Oxford University Press; 2006. [Google Scholar]
- 13.Insall J, Walker P. Unicondylar knee replacement. Clin Orthop Relat Res. 1976;120:83–85. [PubMed] [Google Scholar]
- 14.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am. 1989;71:145–150. [PubMed] [Google Scholar]
- 16.Lanyon P, Muir K, Doherty S, Doherty M. Age and sex differences in hip joint space among asymptomatic subjects without structural change: implications for epidemiologic studies. Arthritis Rheum. 2003;48:1041–1046. doi: 10.1002/art.10886. [DOI] [PubMed] [Google Scholar]
- 17.Lanyon P, O’Reilly S, Jones A, Doherty M. Radiographic assessment of symptomatic knee osteoarthritis in the community: definitions and normal joint space. Ann Rheum Dis. 1998;57:595–601. doi: 10.1136/ard.57.10.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Laskin RS. Unicompartmental tibiofemoral resurfacing arthroplasty. J Bone Joint Surg Am. 1978;60:182–185. [PubMed] [Google Scholar]
- 19.Marx RG, Grimm P, Lillemoe KA, Robertson CM, Ayeni OR, Lyman S, Bogner EA, Pavlov H. Reliability of lower extremity alignment measurement using radiographs and PACS. Knee Surg Sports Traumatol Arthrosc. 2011;19:1693–1698. doi: 10.1007/s00167-011-1467-3. [DOI] [PubMed] [Google Scholar]
- 20.Merle C, Waldstein W, Pegg E, Streit MR, Gotterbarm T, Aldinger PR, Murray DW, Gill HS. Femoral offset is underestimated on anteroposterior radiographs of the pelvis but accurately assessed on anteroposterior radiographs of the hip. J Bone Joint Surg Br. 2012;94:477–482. doi: 10.1302/0301-620X.94B4.28067. [DOI] [PubMed] [Google Scholar]
- 21.Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69:745–749. [PubMed] [Google Scholar]
- 22.Mukherjee K, Pandit H, Dodd CA, Ostlere S, Murray DW. The Oxford unicompartmental knee arthroplasty: a radiological perspective. Clin Radiol. 2008;63:1169–1176. doi: 10.1016/j.crad.2007.12.017. [DOI] [PubMed] [Google Scholar]
- 23.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43:752–757. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 24.Paley D. Principles of Deformity Correction. Berlin, Germany: Springer; 2003. [Google Scholar]
- 25.Richmond JC. Surgery for osteoarthritis of the knee. Rheum Dis Clin North Am. 2013;39:203–211. doi: 10.1016/j.rdc.2012.10.008. [DOI] [PubMed] [Google Scholar]
- 26.Schindler OS, Scott WN, Scuderi GR. The practice of unicompartmental knee arthroplasty in the United Kingdom. J Orthop Surg (Hong Kong). 2010;18:312–319. doi: 10.1177/230949901001800311. [DOI] [PubMed] [Google Scholar]
- 27.Swienckowski JJ, Pennington DW. Unicompartmental knee arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am. 2004;86(suppl 1):131–142. doi: 10.2106/00004623-200409001-00004. [DOI] [PubMed] [Google Scholar]
- 28.Tallroth K, Lindholm TS. Stress radiographs in the evaluation of degenerative femorotibial joint disease. Skeletal Radiol. 1987;16:617–620. doi: 10.1007/BF00357109. [DOI] [PubMed] [Google Scholar]
- 29.Wada M, Baba H, Imura S, Morita A, Kusaka Y. Relationship between radiographic classification and arthroscopic findings of articular cartilage lesions in osteoarthritis of the knee. Clin Exp Rheumatol. 1998;16:15–20. [PubMed] [Google Scholar]