Abstract
Background
High readmission rates are viewed by the Centers for Medicare & Medicaid Services as a quality of care determinant but it is unclear whether readmission rates per se reflect quality and the drivers of readmissions after hip arthroplasty remain unclear.
Question/purposes
We therefore describe the effects of (1) insurance, discharge disposition, and mental health status as they relate to rates; (2) rehospitalization charges; and (3) reasons for readmissions.
Methods
We studied a cohort of all 27,019 patients who initially underwent hip arthroplasty in Florida (April 2009 to March 2010). Participants were identified using the All Patient-Refined Diagnosis-Related Group 301. Data were provided by the Agency for Health Care Administration and the Florida Hospital Association who with the Florida Orthopedic Society studied readmissions within 15 days. We extracted readmission rates and their reasons; original payers, discharge disposition, mental health status; and readmission charges.
Results
The readmission rate in the first 15 days was 5%. Rates varied by type of insurance: self-pay/underinsured, Medicaid, and Medicare patients (6%) had higher rates than individuals with commercial insurance, HMO, or PPO (3%). Patients discharged to skilled nursing facilities (SNFs) had higher rates (7%) than patients discharged home with/without health care (both 3%). Patients with a mental health issue (10%) were readmitted more frequently than patients without it (5%). Medicare readmissions comprised 81% (USD 59,222,829) of the total readmission charges in this cohort. The most common reasons were infections (all 27%), hip arthroplasty (11%), and cardiovascular problems (9%).
Conclusions
Patients were more frequently readmitted if their payer was the government, they were discharged to a SNF, or they had a mental health disorder. Infections were the most common reasons for readmission. Our data suggest readmission rates alone do not necessarily reflect quality of care.
Introduction
Value purchasing has become a central strategy in the efforts to improve health care [14]. The reduction of rehospitalizations is currently seen by policymakers as a way to partially achieve this goal and reduce costs. The Patient Protection and Affordable Care Act of 2010 included various cost-control elements such as a new hospital readmission policy that will impose financial penalties to hospitals with high risk-adjusted readmission rates for selected high-volume and high-cost conditions [10]. In June 2012 after substantial debate, the National Quality Forum Board of Directors voted to uphold its initial decision [11], already challenged by seven hospital systems, to endorse an all-cause hospital wide readmissions measure developed by Yale University and the Centers for Medicare & Medicaid Services (CMS). Beginning October 2012, more than 2000 hospitals will be penalized because of their high standardized readmission rates on acute myocardial infarction, heart failure (HF), and pneumonia.
Although hip arthroplasty was not included in the initial set of diagnoses, it will be part of the second-tier diagnoses that will be included in Phase II beginning in 2015 [19]. An analysis of those penalties shows 76% of hospitals with a case mix that includes low-income patients will lose Medicare funds in the 2013 fiscal year, whereas only 55% of hospitals treating few low-income patients will be penalized [23]. Starting in 2015, a 30-day risk-standardized readmission rate measure after THA/TKA will be implemented [19]. Currently, policymakers consider readmission rates as a quality measure and high rates as a sign of poor quality of care.
However, to ascertain whether they truly reflect the quality of care, such measures must be strongly supported by scientific evidence. Quality improvement efforts tend to be iterative and lack most methods used in clinical research studies such as well-defined research protocols, explicit data collection tools, well-designed databases, clear quality-control plans, and detailed analytic plans designed to reduce bias. Most quality measurement efforts struggle to find a balance between measures that are scientifically sound yet feasible to implement. Sadly, feasibility generally trumps sound science and pandering to the media has become commonplace in the quality arena. There is no standard framework to evaluate the strength and amount of evidence required before a measure is suitable for public reporting or pay-for-performance programs [20]. Invalid quality-of-care measures pose major risks to patients, payers, clinicians, and maybe even the public trust in the medical profession [21]. Particularly vulnerable in this arrangement are the minority and the poor. There are major concerns that closer adherence to quality indicators could lead to restriction of care [17]. In addition, factors that could influence readmissions such as mortality [6, 7, 9], length of stay [6, 7], and even racial, ethnic, and socioeconomic patient characteristics [15] must be recognized and the readmission rate adjusted accordingly. The current approach omits consideration of important variables that determine readmissions and a deeper understanding of the complexity surrounding them is warranted. In addition, if those measures are to be publicly reported, they should have the same reporting standards as pharmaceutical and financial entities. Currently, investors are generally confident that figures in financial reports are correct. The Securities and Exchange Commission designated and authorized the Financial Accounting Standards Board (an independent body) to establish and improve standards for financial accounting and reporting. In the same line, pharmaceutical companies must adhere to the Code of Federal Regulations when making statements to consumers about drug products. Promotional claims by companies must be supported by evidence or clinical experience. Oversight of these communications comes predominantly from the US Food and Drug Administration’s Division of Drug Marketing, Advertising, and Communications and failure of companies to follow these guidelines can result in enforcement actions [21].
Currently, the real drivers and complexities associated with readmissions after hip arthroplasty remain unclear. The readmission rates policy omits consideration of important variables that affect them. Before implementation, quality measures need to be well understood and proven scientifically sound. We performed this investigation to achieve better recognition and understanding of the drivers and complexities associated with readmissions after hip arthroplasty. This investigation is purely descriptive in nature.
The purposes of this retrospective study were to describe (1) readmission rates within 15 days and how they related to insurance type, discharge disposition, and mental health status; (2) costs of rehospitalizations; and (3) reasons for readmissions.
Patients and Methods
We used data from the Agency for Health Care Administration who collects discharge information on all licensed acute care hospitals, comprehensive rehabilitation hospitals, ambulatory surgical centers, and emergency departments in the state of Florida quarterly. The Florida Hospital Association (FHA) teamed with the Florida Orthopedic Society to study readmissions within 15 days after hip arthroplasty in the state of Florida. All information was collated by the FHA. Patients were identified using the All Patient-Refined Diagnosis-Related Group (APR-DRG) 301 (hip arthroplasty) for the 12-month period from April 2009 to March 2010. APR-DRG is a software algorithm that takes into account severity of illness and likelihood of dying. In 2006, the CMS recommended using APR-DRGs as the primary predictor of resource use without accounting for procedure characteristics such as surgical complexity [5]. We identified a total of 27,019 patients during the study period; they comprise the observational cohort under analysis.
The overall readmission rate and the proportion of patients that was rehospitalized in institutions different from the ones of the original procedure were determined. We examined whether readmission rates related to the following factors: (1) payer (Medicaid, Medicare, commercial preferred provider organization [PPO], commercial insurance, commercial health maintenance organization [HMO], self-pay/underinsured, and all others); (2) original discharge disposition (home, home health/home infusion, skilled nursing facility [SNF], and others); and (3) the presence or absence of a mental health issue among patients. We determined the charges of rehospitalizations according to payers. Outcomes of interest also included the reasons for readmissions and their occurrence according to the location to which patients were discharged originally after the index surgery.
We conducted descriptive statistical analyses. Data were reported as numbers, means, and proportions. We used proportions for nominal data. The measure of central tendency used was the arithmetic mean.
Results
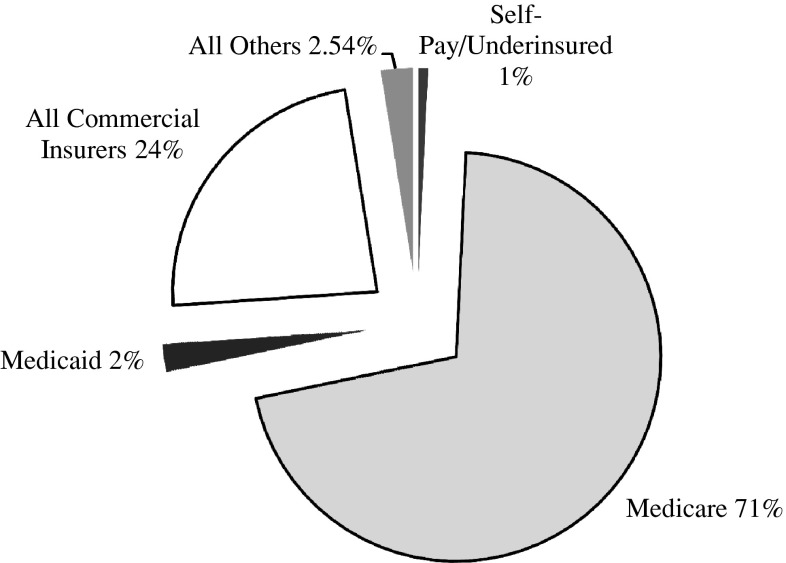
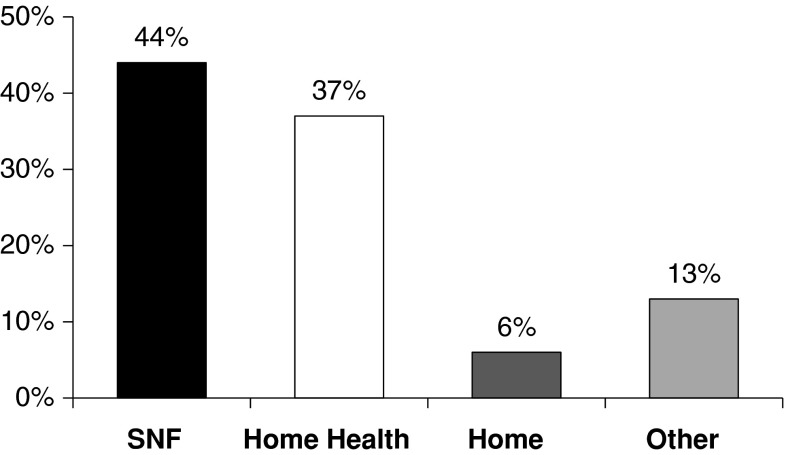
There were 27,019 patients admitted during the study period; 1356 patients were rehospitalized within 15 days for an overall readmission rate of 5.0%. Twenty-one percent of readmitted patients had their rehospitalizations in institutions different from the ones of the original procedure. Medicare was the most frequent payer (71%) followed by commercial insurers (24%) (Fig. 1). Readmission rates varied by type of insurance because patients with Medicaid (5.9%), self-pay/underinsured (5.8%), and Medicare (5.8%) had higher readmission rates than individuals with commercial insurance (2.6%), commercial HMO (2.7%), or commercial PPO (2.5%). Overall, 20% of patients were readmitted to hospitals different from the ones of the original procedures. Medicare was the payer in more than 70% of the original cases (Table 1). After the index surgery, most of the patients were discharged to either a SNF (44%) or to home with home health care (37%) (Table 2; Fig. 2). Patients who were originally discharged to SNFs had higher readmission rates (7.0%) than patients discharged directly to home without home health care (3.2%) or with it (2.7%) (Table 2). From the 27,019 patients identified during the study period, 4.3% (n = 1165) were diagnosed with a mental health issue. Patients with a mental health condition (8.7%) were readmitted more frequently than patients without it (4.9%).
Fig. 1.
The pie chart shows the proportions of patients admitted in Florida (APR-DRG 301) from April 2009 to March 2010 according to insurance type.
Table 1.
Readmission rates within 15 days after hip arthroplasty according to payers including proportion of patients readmitted to hospitals different from the ones of the original procedures
| Payer | Patients admitted (number) | Patients readmitted (number) | Readmitted to another hospital (%) | Readmission rate (%) |
|---|---|---|---|---|
| Medicare | 19,273 | 1121 | 21.3 | 5.8 |
| Medicaid | 596 | 35 | 28.6 | 5.9 |
| Commercial PPO | 2254 | 57 | 5.3 | 2.5 |
| Commercial insurance | 2054 | 53 | 17.0 | 2.6 |
| Commercial HMO | 1946 | 53 | 26.4 | 2.7 |
| Self-pay/underinsured | 208 | 12 | 33.3 | 5.8 |
| All others | 688 | 25 | 8.0 | 3.6 |
| Total | 27,019 | 1356 | 20.7 | 5.0 |
PPO = preferred provider organization; HMO = health maintenance organization.
Table 2.
Readmission rates within 15 days after hip arthroplasty by location to which patients were discharged originally
| Discharge disposition | Patients admitted (number) | Patients admitted (%) | Patients readmitted (number) | Readmission rate (%) |
|---|---|---|---|---|
| Home | 1678 | 6 | 54 | 3.2 |
| Home health/infusion | 10,029 | 37 | 269 | 2.7 |
| Skilled nursing facility | 11,897 | 44 | 835 | 7.0 |
| Others | 3415 | 13 | 198 | 5.8 |
Fig. 2.
The discharge disposition of patients admitted in Florida (APR-DRG 301) from April 2009 to March 2010 shows most patients were discharged to either a SNF (44%) or to home with home health care (37%).
Overall, readmissions cost for this DRG totaled USD 73,259,090. Medicare readmission charges amounted to USD 59,222,829 representing 80.8% of the total (Table 3). However, when costs were analyzed as charges per readmission, the group that comprises all other payers had the highest mean charge (USD 80,679).
Table 3.
Readmission charges according to payers
| Payer | Patients readmitted (number) | Total charges (US dollars) | Charges per readmission (mean US dollars) |
|---|---|---|---|
| Medicare | 1121 | 59,222,829 | 52,830 |
| Medicaid | 35 | 2,581,606 | 73,760 |
| Commercial PPO | 57 | 2,722,851 | 47,769 |
| Commercial Insurance | 53 | 3,147,536 | 59,387 |
| Commercial HMO | 53 | 3,184,721 | 60,089 |
| Self-pay/underinsured | 12 | 382,577 | 31,881 |
| All others | 25 | 2,016,970 | 80,679 |
| Total | 1356 | 73,259,090 | 54,026 |
PPO = preferred provider organization; HMO = health maintenance organization.
Most of the readmissions were the result of infections (all systems included, 28%) (Table 4). Infections, as a reason for readmission, were followed by hip arthroplasty (11.4%), cardiovascular problems (9.1%), problems with the orthopaedic device or procedure (7.0%), and anemia/blood disorders (6.8%) (Table 5). Among patients discharged to home without home care, the most frequent reason for readmission was malfunction, reaction, and complication of the orthopaedic device or procedure (18.5% of all readmissions), whereas for patients discharged to a SNF, it was anemia and blood disorders (8.3%). For patients discharged to home with home health care or discharged to other facilities, the most frequent reason for readmission was hip arthroplasty (21.6% and 13.6%, respectively).
Table 4.
Types of infections that led to readmissions after hip arthroplasties
| Type of infection | Patients readmitted (number) | Frequency (%) (from total number of readmitted patients, n = 1356) |
|---|---|---|
| Postoperative, posttraumatic, other device infection | 81 | 6.0 |
| Septicemia and disseminated infections | 81 | 6.0 |
| Kidney and urinary tract infections | 58 | 4.3 |
| Other pneumonia | 53 | 3.9 |
| Major respiratory infections and inflammation | 41 | 3.0 |
| Major gastrointestinal and peritoneal infections | 26 | 1.9 |
| Postoperative, posttrauma, other device infections with operating room procedure | 21 | 1.5 |
| Cellulitis and other bacterial skin infection | 12 | 0.9 |
| Other infectious and parasitic diseases | 1 | 0.1 |
| Total | 374 | 27.6 |
Table 5.
Most frequent reasons for readmissions
| Reasons for readmission | Patients readmitted (number) | Percent of total |
|---|---|---|
| Hip arthroplasty | 155 | 11.4 |
| Malfunction, reaction, and complications of orthopaedic device or procedure | 95 | 7.0 |
| Other anemia and disorders of blood and blood-forming organs | 92 | 6.8 |
| Postoperative, posttraumatic, other device infections | 81 | 6.0 |
| Septicemia and disseminated infections | 81 | 6.0 |
| Kidney and urinary tract infections | 58 | 4.3 |
| Peripheral and other vascular disorders | 56 | 4.1 |
| Heart failure | 55 | 4.1 |
| Other pneumonia | 53 | 3.9 |
| Other complications of treatment | 52 | 3.8 |
| Hip and femur procedures for nontrauma except joint arthroplasty | 42 | 3.1 |
| Major respiratory infections and inflammations | 41 | 3.0 |
| Renal failure | 36 | 2.7 |
| Chronic obstructive pulmonary disease | 32 | 2.4 |
| Pulmonary embolism | 32 | 2.4 |
| Major gastrointestinal and peritoneal infections | 26 | 1.9 |
| Syncope and collapse | 23 | 1.7 |
| Other musculoskeletal system and connective tissue diagnoses | 22 | 1.6 |
| Other and unspecified gastrointestinal hemorrhage | 21 | 1.5 |
| Postoperative, posttrauma, other device infections with operating room procedure | 21 | 1.5 |
| Total of patients readmitted | 1356 |
Discussion
High readmission rates are viewed by CMS as a sign of poor quality of care. Currently, hospitals with high rates face a 1% financial penalty over their base Medicare reimbursements, but penalties will increase to 2% in 2013 and 3% in 2014 [23]. The private sector has adopted a similar policy. WellPoint [27] will increase reimbursements only to hospitals that score high enough on various treatment quality indicators including whether the facility prevents rehospitalizations [1]. Currently, policymakers consider readmission rates as a quality measure. Our data, although only descriptive in nature, show readmission rates can be driven by a multitude of factors in addition to baseline health status. Socioeconomic factors such as insurance type and discharge disposition do affect them. We believe not enough consideration has been given to the validity of such rates as a quality measure when we realize that not all factors are well known and much less taken into account and weighted during risk-adjusted rate calculations. The implementation of the readmission policy should be done only after all factors are well understood and considered so that risk-adjustment calculations could be properly done. Readmission rate is by definition a measure of health service use and it is influenced by care quality and patient’s health status but it is also a function of access to health services and socioeconomic resources like income or social support [16]. In addition, racial, ethnic, and socioeconomic patient characteristics have been seen to influence those rates [15]. Factors inversely related to readmission rates such as mortality [6, 7, 9] and length of stay [6, 7] would also need recognition. In summary, the current approach to readmissions in hip arthroplasty does not consider important variables that determine readmissions [2]. In an effort to better recognize and understand what drives readmissions, we studied them in the state of Florida paying particular attention to their relationships with patient, payer, and healthcare provider characteristics. We ascertained (1) 15-day readmission rates and how they related to insurance type, discharge factors, and mental health status; (2) charges of rehospitalizations; and (3) reasons for readmissions. Lastly the time period in which readmission rates are studied is a key factor. Nationally 30 days readmissions rates are currently used.
The results of the current investigation should be interpreted in light of several limitations. First, we used administrative data that tend to underestimate the prevalence of some comorbid conditions [12, 22]. This limitation is shared by the whole readmission policy, which relies on administrative databases. Second, we did not have access to all data collated by the FHA and consequently we could not directly confirm its accuracy; in addition, no data were available to do comparisons adjusting for baseline patient characteristics. However, data were used by the readmission task force at the Florida Orthopedic Society during the investigations conducted regarding readmissions. Third, it is possible that government-insured patients were sicker than the privately insured and this might explain the differences in readmission rates between them. However, the mere acknowledgement of this phenomenon regarding payers warrants attention and further investigation as it relates to future risk-adjustment calculations. Fourth, although the CMS systematically audits the coding of DRGs, discharge disposition data are generally not used for payment and may be unreliable. Finally, the ethnic and socioeconomic characteristics of the population of Florida are particular as a result of the high proportion of Hispanics and retirees. Generalizations to the overall population or other regions cannot be made expeditiously.
The 5% overall readmission rate observed in the current investigation is similar to the ones reported in previous investigations (Table 6) [3, 7, 8, 18, 24, 26, 28, 29]. In Florida, 21% of patients were readmitted to hospitals different from the ones of the original procedure. This is in agreement with the literature as much as it has been reported [13] that 24.4% of patients discharged from hospitals with 1000 or more Medicare discharges end up readmitted to institutions different from the ones of the index surgery. In the current study, readmission rates varied by type of insurance because self-pay/underinsured, Medicaid, and Medicare had approximately twice the readmission rates as individuals with commercial insurance, HMO, or PPOs. Previous research has demonstrated high rates of rehospitalization among patients with government insurance. Jencks et al. [13] studied rehospitalizations among patients in the Medicare program (2003–2004) and found a 19.6% rate within 30 days and a 34% within 90 days. In Florida, we found patients discharged to a SNF had more than twice the rates of readmission when compared with patients discharged to home with or without home healthcare services. This phenomenon has been reported by various investigators. Bueno et al. [6] in a study of 6,955,461 Medicare hospitalizations for HF (from 2003 to 2006) observed that during the study period, discharges to home or under home care service decreased from 74.0% to 66.9%; discharges to SNFs increased from 13.0% to 19.9%; and the 30-day readmission rate increased from 17.2% to 21% (p < 0.001). Cram et al. [7] from 1991 to 2008 reported that the proportion of patients discharged home declined from 68.0% to 48.2%; the proportion discharged to SNFs increased from 17.8% to 34.3%; and the 30-day readmission rate increased from 5.9% to 8.5% (p < 0.001). Bini et al. [3] found that patients undergoing THA discharged to SNFs had higher odds of readmission within 90 days of surgery than patients discharged to home (p = 0.008). We observed that patients with mental health issues were readmitted twice as frequently as patients without them. This is in agreement with the literature because comorbidities have been previously reported to negatively affect the outcomes of patients undergoing THA [4, 18].
Table 6.
Comparison of readmission rates after hip arthroplasty
| Authors | Followup (days) | Total readmission rates (%) | Primary readmission rates (%) | Revision readmission rates (%) |
|---|---|---|---|---|
| Cram et al. [7] (2011) | 30 | N/A | 8.5 | 14.1 |
| Bini et al. [3] (2010) | 90 | N/A | 2.9 | N/A |
| Seagroatt et al. [24] (1991) | 28 | 2.7 | N/A | N/A |
| Mahomed et al. [18] (2003) | 90 | N/A | 4.6 | 10 |
| Vorhies et al. [26] (2011) | 30 | 6.3 | N/A | N/A |
| Zhan et al. [29] (2007) | 30 | N/A | 4.9 | 8.5 |
| Cullen et al. [8] (2006) | 28 | N/A | 8.5 | N/A |
| Wolf et al. [28] (2012) | 90 | 11.8* | 10.9 | 17.6 |
| Current study (2012) | 15 | 5 | N/A | N/A |
* Calculated based on (n) values provided in article (number of hospitalizations/number of all-cause readmissions); N/A = not available.
We found that Medicare charges comprised 81% of the total readmission charges. The cost for Medicare of unplanned rehospitalizations has been estimated to be over USD 17 billion a year [13]. This situation has attracted attention from policymakers who now seek reducing the rates of readmissions as a way of cost containment.
Hip arthroplasties (11.4%) were the second most frequent reason, even surpassing cardiovascular problems (9.1%). Hip arthroplasties represent a procedure different from the original hip arthroplasty. We believe most of these hip arthroplasties were the contralateral hip. This was planned in advance and done to decrease the morbidity associated with simultaneous arthroplasties. This finding puts into question the specificity of an all-cause readmission policy, because administrative data might not fully discriminate between related and unrelated readmissions. Readmission rates as a quality measure have both conceptual problems in their interpretation and technical problems in their implementation. Granularity in the readmission process is required to use these rates in the value purchasing program. An all-cause readmission policy does not discriminate unavoidable causes that lead to readmissions such as an anticoagulant-related hematoma, which requires drainage to prevent infection, in a patient with well-controlled coagulation markers. We did not have access to mortality data in this cohort; nonetheless, we believe it is comparable to the 0.06% rate reported for all 29,210 Florida patients who were hospitalized for hip arthroplasty during 2011 [25]. However, it is important to point out the inverse relationship between mortality and readmissions, well illustrated in the study performed by Gorodeski et al. [9]. They found a higher occurrence of readmissions after index admissions as a result of HF was associated with lower risk-adjusted 30-day mortality. As such, to some extent, the higher readmission rate might have been a consequence of successful care.
Surgeons and hospitals that have destination centers will be particularly hurt with the implementation of the readmission policy. In most of these destination practices, patients return to their original areas after the surgical interventions. In those far away communities, in the event of a complication, the emergency department physicians and covering specialists might not be familiar with the normal appearance and behavior of a postoperative total hip and could admit to the hospital patients who otherwise can be managed with outpatient observation. There are also medicolegal incentives to admit the patients. There is no doubt that readmissions represent a heavy burden to society, but with the implementation of the readmission policy, reduced payments could be unfairly applied to hospitals focused on difficult cases, hospitals treating minorities, or both.
In conclusion, multiple complex factors play a role in short-term readmissions after hip arthroplasty. Infections in general were the most frequent reasons for readmission followed by hip arthroplasty. Patients were more frequently readmitted if their payer was government-funded, they were discharged to a SNF, or if they had a mental health issue. Our data suggest readmission rates alone do not necessarily reflect quality of care.
Acknowledgments
We thank the Agency for Health Care Administration, the Florida Hospital Association, the Florida Orthopedic Society, Andrew Wong, MD, and the readmission task force at the Florida Orthopedics, Kim Streit (FHA), and Christy Sharp for allowing access to the data.
Footnotes
One of the authors (CJL) has or may receive payments or benefits, during the study period, an amount of USD 10,000–USD 100,000 from Mako Surgical Corp (Fort Lauderdale, FL, USA); has or may receive payments or benefits, during the study period, an amount of USD 10,000–USD 100,000 from Johnson & Johnson (New Brunswick, NJ, USA); has or may receive payments or benefits, during the study period, an amount of USD 10,000–USD 100,000 from Zimmer (Warsaw, IN, USA); has or may receive payments or benefits, during the study period, an amount of USD 10,000–USD 100,000 from Wright (Arlington, TN, USA); and has or may receive payments or benefits, during the study period, an amount of USD 10,000–USD 100,000 from Symmetry Medical Inc (Warsaw, IN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Orthopaedic Institute at Mercy Hospital, Miami, FL, USA.
References
- 1.Adamy J. WellPoint Shakes Up Hospital Payment. 2011. Available at: http://online.wsj.com/article/SB10001424052748704281504576325163218629124.html. Accessed May 17, 2011.
- 2.Bhalla R, Kalkut G. Could Medicare readmission policy exacerbate health care system inequity? Ann Intern Med. 2010;152:114–117. doi: 10.7326/0003-4819-152-2-201001190-00185. [DOI] [PubMed] [Google Scholar]
- 3.Bini SA, Fithian DC, Paxton LW, Khatod MX, Inacio MC, Namba RS. Does discharge disposition after primary total joint arthroplasty affect readmission rates? J Arthroplasty. 2010;25:114–117. doi: 10.1016/j.arth.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 4.Bjorgul K, Novicoff WM, Saleh KJ. Evaluating comorbidities in total hip and knee arthroplasty: available instruments. J Orthop Traumatol. 2010;11:203–209. doi: 10.1007/s10195-010-0115-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bozic KJ, Rubash HE, Sculco TP, Berry DJ. An analysis of Medicare payment policy for total joint arthroplasty. J Arthroplasty. 2008;23:133–138. doi: 10.1016/j.arth.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 6.Bueno H, Ross JS, Wang Y, Chen J, Vidan MT, Normand SL, Curtis JP, Drye EE, Lichtman JH, Keenan PS, Kosiborod M, Krumholz HM. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010;303:2141–2147. doi: 10.1001/jama.2010.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cram P, Lu X, Kaboli PJ, Vaughan-Sarrazin MS, Cai X, Wolf BR, Li Y. Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991–2008. JAMA. 2011;305:1560–1567. doi: 10.1001/jama.2011.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cullen C, Johnson DS, Cook G. Re-admission rates within 28 days of total hip replacement. Ann R Coll Surg Engl. 2006;88:475–478. doi: 10.1308/003588406X116909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gorodeski EZ, Starling RC, Blackstone EH. Are all readmissions bad readmissions? N Engl J Med. 2010;363:297–298. doi: 10.1056/NEJMc1001882. [DOI] [PubMed] [Google Scholar]
- 10.Hackbarth G, Reischauer R, Mutti A. Collective accountability for medical care—toward bundled Medicare payments. N Engl J Med. 2008;359:3–5. doi: 10.1056/NEJMp0803749. [DOI] [PubMed] [Google Scholar]
- 11.Healthcare-Informatics. NQF Endorses Readmissions Measures. 2012. Available at: http://www.healthcare-informatics.com/news-item/nqf-endorses-readmissions-measures. Accessed October 9, 2012.
- 12.Humphries KH, Rankin JM, Carere RG, Buller CE, Kiely FM, Spinelli JJ. Co-morbidity data in outcomes research: are clinical data derived from administrative databases a reliable alternative to chart review? J Clin Epidemiol. 2000;53:343–349. doi: 10.1016/S0895-4356(99)00188-2. [DOI] [PubMed] [Google Scholar]
- 13.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 14.Jha AK, Joynt KE, Orav EJ, Epstein AM. The long-term effect of premier pay for performance on patient outcomes. N Engl J Med. 2012;366:1606–1615. doi: 10.1056/NEJMsa1112351. [DOI] [PubMed] [Google Scholar]
- 15.Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305:675–681. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kangovi S, Grande D. Hospital readmissions—not just a measure of quality. JAMA. 2011;306:1796–1797. doi: 10.1001/jama.2011.1562. [DOI] [PubMed] [Google Scholar]
- 17.Lee SJ, Walter LC. Quality indicators for older adults: preventing unintended harms. JAMA. 2011;306:1481–1482. doi: 10.1001/jama.2011.1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mahomed NN, Barrett JA, Katz JN, Phillips CB, Losina E, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Rates and outcomes of primary and revision total hip replacement in the United States Medicare population. J Bone Joint Surg Am. 2003;85:27–32. doi: 10.2106/00004623-200301000-00005. [DOI] [PubMed] [Google Scholar]
- 19.CMS FY 2014–2016 Measures for CMS Payment Determination. Washington, DC, USA: Premier Safety Institute; 2012. [Google Scholar]
- 20.Pronovost PJ, Berenholtz SM, Goeschel CA. Improving the quality of measurement and evaluation in quality improvement efforts. Am J Med Qual. 2008;23:143–146. doi: 10.1177/1062860607313146. [DOI] [PubMed] [Google Scholar]
- 21.Pronovost PJ, Miller M, Wachter RM. The GAAP in quality measurement and reporting. JAMA. 2007;298:1800–1802. doi: 10.1001/jama.298.15.1800. [DOI] [PubMed] [Google Scholar]
- 22.Quan H, Parsons GA, Ghali WA. Validity of information on comorbidity derived from ICD-9-CCM administrative data. Med Care. 2002;40:675–685. doi: 10.1097/00005650-200208000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Rau J. Medicare to Penalize 2,211 Hospitals for Excess Readmissions. 2012. Available at: http://www.kaiserhealthnews.org/Stories/2012/August/13/medicare-hospitals-readmissions-penalties.aspx. Accessed October 5, 2012.
- 24.Seagroatt V, Tan HS, Goldacre M, Bulstrode C, Nugent I, Gill L. Elective total hip replacement: incidence, emergency readmission rate, and postoperative mortality. BMJ. 1991;303:1431–1435. doi: 10.1136/bmj.303.6815.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sternberg S. Shopping for a Hip Replacement in Florida? Go by the Numbers. 2012. US News & World Report. Available at: health.usnews.com/health-news/blogs/second-opinion/2012/12/28/shopping-for-a-hip-replacement-in-florida-go-by-the-numbers_print.html. Accessed December 28, 2012.
- 26.Vorhies JS, Wang Y, Herndon J, Maloney WJ, Huddleston JI. Readmission and length of stay after total hip arthroplasty in a national Medicare sample. J Arthroplasty. 2011;26:119–123. doi: 10.1016/j.arth.2011.04.036. [DOI] [PubMed] [Google Scholar]
- 27.WellPoint. About WellPoint. 2012. Available at: http://www.wellpoint.com/AboutWellPoint/index.htm. Accessed July 3, 2012.
- 28.Wolf BR, Lu X, Li Y, Callaghan JJ, Cram P. Adverse outcomes in hip arthroplasty: long-term trends. J Bone Joint Surg Am. 2012;94:e103. doi: 10.2106/JBJS.J.00764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhan C, Kaczmarek R, Loyo-Berrios N, Sangl J, Bright RA. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg Am. 2007;89:526–533. doi: 10.2106/JBJS.F.00952. [DOI] [PubMed] [Google Scholar]