Abstract
Methicillin-resistant Staphylococcus aureus (MRSA) has emerged as a major public health threat. In this retrospective cohort study, we included patients with laboratory-confirmed MRSA infections treated at Children's National Medical Center in Washington, District of Columbia between July 2003 and December 2010. The secular trends in the incidence rates of skin/soft tissue and invasive MRSA infections were assessed. Molecular analyses were performed on a subset of patients with invasive infections whose MRSA isolates were available for genotyping. The study identified 3750 patients with MRSA infections. The incidence of MRSA infections peaked in 2007 (incidence rate: 5.34 per 1000 patient-visits) and subsequently declined at a rate of 5% per year. By December 2010, the MRSA incidence rate reached 3.77 per 1000 patient-visits. Seventeen (14.7%) patients with invasive MRSA infections died, and the mortality risk significantly increased if the MRSA infections were healthcare-associated (HA) or if an isolate was resistant to clindamycin and/or trimethoprim/sulfamethoxazole. In conclusion, this study described a descending trend in MRSA infections in children since 2007. Although invasive MRSA infections only accounted for a small portion of the total MRSA infections, they were associated with a high mortality risk. The prevention and control of the spread of MRSA remains a crucial and challenging task.
Keywords: children, invasive infections, MRSA, trend
INTRODUCTION
In the late 1990s, dramatic increases in the frequency of community-acquired methicillin-resistant Staphylococcus aureus (MRSA) infections were noted among children without established risk factors for MRSA infections (e.g., recent hospitalization, recent surgery, residence in a long-term care facility or injection-drug use).1 Between 1996 and 1999, MRSA was linked to at least four fatal infections in pediatric population patients.2 These incidents indicated that serious MRSA infections could be acquired in the community and suggested the emergence of a new community strain that was different from the strain isolated in healthcare settings.1,2,3 Since then, MRSA has been recognized as a major threat to public health. In 2005 alone, the Centers for Disease Control and Prevention estimated that 94 360 invasive MRSA infections occurred in the United States, and these infections were associated with 18 650 deaths.4 Due to nationwide MRSA outbreaks5,6,7,8,9,10,11 and the increase of MRSA skin and soft tissue infections in patients seeking emergency care,12,13,14 the prevention of MRSA in both community and healthcare settings has been a priority. Strategies including active screening, the use of contact precautions and decolonization have been enforced through legislative efforts, as well as evidence-based practices. By 2009, a subsequent study conducted in the same patient population revealed that invasive MRSA infections in the United States had decreased, largely due to the reduction in central line-associated bloodstream infections in healthcare settings.15
We recognized that the identification of the epidemiology and infection patterns in local hospital settings remains critical as it directly affects clinical management plans and patient outcomes. Therefore, we conducted this study to describe the epidemiological characteristics of patients with MRSA infections treated at a free-standing children's hospital in the District of Columbia (DC).
MATERIALS AND METHODS
Study setting
This study was conducted at the Children's National Medical Center (CNMC) in Washington, DC. As the only exclusive provider of pediatric care in the metropolitan Washington area and the only freestanding children's hospital between Philadelphia, Pittsburgh, Norfolk and Atlanta, the hospital serves as the regional referral center for pediatric emergency, trauma, cancer, cardiac and critical care, as well as neonatology, orthopedic surgery, neurology and neurosurgery.
The Children's Hospital at CNMC features 303 inpatient beds, an emergency department (ED) that treats an average of 70 000 patients each year and clinics that provide primary and specialty outpatient care for newborns up to adolescents.
Study design and patient population
This was a retrospective cohort study that included patients treated for a MRSA infection at CNMC between July 2003 and December 2010; these infections were confirmed by the microbiology laboratory at CNMC.
Skin and soft tissue infections due to Staphylococcus aureus (S. aureus) were isolated from a specimen of the selected body site, including nail, arm, axilla, back, buttock, catheter insertion site, face, finger, foot, leg, vesicle, neck, nose, penis, perianal area, scrotum, skin, toe, umbilicus or genital site.
An infection was classified as invasive MRSA if it was recovered from a specimen collected at a normally sterile site, such as blood, peritoneal fluid, cerebrospinal fluid, joint/synovial fluid, pleural fluid, bone, pericardial fluid or from an internal body site, such as lymph node, brain, heart, liver, spleen, vitreous fluid, kidney, pancreas or ovary.4
Cases of invasive infection were further classified as healthcare-associated (HA) if the patients had one or more of the following risk factors: history of hospitalization in the past year, the presence of a percutaneous device or indwelling catheter, dialysis within the previous year, history of MRSA infection or colonization, history of surgery within 1 year prior to the culture date or history of residence at a long-term care facility.14 Patients with no documented healthcare risks or cases with positive cultures from normally sterile sites obtained at admission or within 48 h of admission without documented HA risk factors were considered to have community-associated MRSA (CA-MRSA) infections.
Microbiology testing and genetic analysis
MRSA was detected using 5% sheep blood agar, chocolate agar and CNA agar. If there was a specific request for a MRSA rule out, mannitol salt agar was added to the inoculation media for the detection of MRSA.
Genetic analysis using repetitive sequence-based PCR (DiversiLab; bioMerieux Inc., Durham, North Carolina, USA) was performed for a subset of cases with invasive infections if their MRSA isolates remained viable at the time of this study. Samples for genetic analysis were first re-cultured on a standard blood agar medium. Colonies of viable isolates were extracted, amplified and detected via electrophoresis to determine the specific genetic patterns. These patterns were then compared to a DNA database provided by the manufacturer and classified as identical if a 95% or higher similarity was detected.
Data sources
Cases of MRSA infections detected at the CNMC microbiology laboratory were identified from the laboratory information system (Sunquest Information Systems; Sunquest Information Systems, Inc., Tuscan, Arizona, USA). The database provided patient identifiers, date of birth, specimen collection date, location and body site, and MRSA susceptibility to a panel of antimicrobial agents.
Additional information was extracted from the medical charts for cases with invasive infections diagnosed between January 2006 and December 2010. This included risk factors determining the status of HA versus CA infections, duration of intensive care if applicable, duration of hospitalization and death at the time of discharge.
Statistical analysis
We calculated the annual incidence rate of MRSA infections per 1000 patient-encounters over a 12-month fiscal year (FY) period (July through June of the following year). Patient-encounters were defined as the number of patient visits in the ED and/or inpatient admissions. Changes in the annual incidence rate were tested using Poisson regression analysis for statistical significance. In addition, we assessed changes in regards to the proportion of MRSA-invasive infections compared to the total MRSA infections detected every year.
Unadjusted logistic regression analysis was performed to identify factors that independently predicted the risk of death in cases with invasive infections. All analyses were performed using Stata 11.0 (Stata Corp., College Station, Texas, USA).
This study was approved by the Institutional Review Board of Children's Research Institutes.
RESULTS
Secular trend in incidence rate of MRSA infections
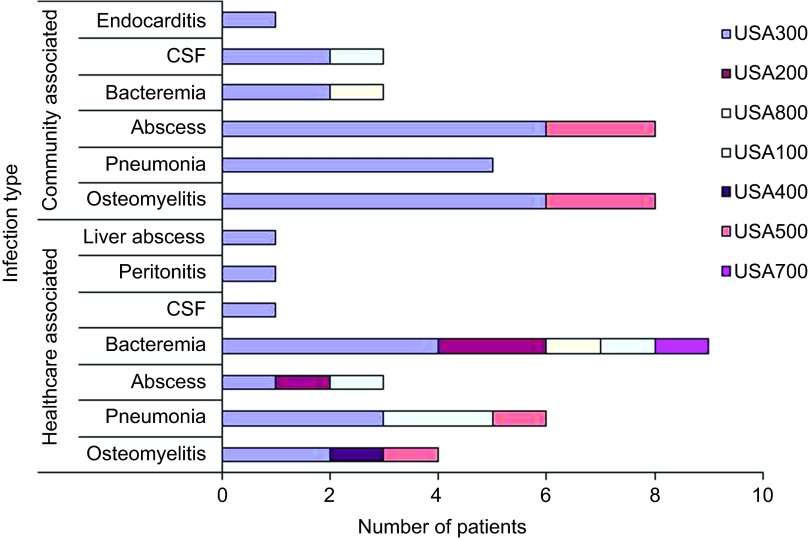
During the study period of July 2003 through December 2010, 3750 patients that were seeking medical care at our facility had a MRSA infection confirmed by the microbiology testing. As shown in Figure 1, MRSA infections increased significantly from 0.93 per 1000 patient-encounters in FY 2004 to a peak of 5.34 per 1000 patient-encounters in FY 2007. Beginning in July 2007, the MRSA incidence rate steadily declined at a rate of 5% every year (incidence rate ratio (IRR): 0.95; 95% confidence interval (CI): 0.94–0.98) and reached 3.77 per 1000 patient-encounters by December 2010.
Figure 1.
Incidence of methicillin-resistant Staphylococcus aureus infections in a children's hospital in the Washington metropolitan area of the United States, 2003–2010.
Over half (54.6%) of these MRSA infections were skin and soft tissue infections treated in the ED. Similar to the overall MRSA incidence rates, the skin and soft tissue infections treated in the ED rose rapidly in FY 2004 from 0.54 to 4.95 per 1000 patient-encounters in FY 2007. Afterwards, the incidence began to decline and reached 2.56 per 1000 patient-encounters by December 2010.
Invasive infections accounted for 5.4% of the MRSA infections in this study cohort. The incidence was the highest in FY 2006 (0.35 per 1000 patient-encounters) and declined at a rate of 19% each year (IRR: 0.81; 95% CI: 0.74–0.90).
The proportion of MRSA in all S. aureus isolated cultures remained relatively stable. MRSA comprised an average of 57.7% of all S. aureus isolates. Of the patients treated in the ED for a skin or soft tissue infection caused by S. aureus, MRSA accounted for 71.8% of the isolates.
Epidemiological and clinical characteristics of patients with invasive infections
Of the 128 patients with invasive MRSA infections during the study period, 116 cases had complete charts for review and were included in the analysis. Of these patients, 58 (50%) were male, and 76 (65.5%) were African American. The majority (n=81, 70%) of the patients were children younger than five years old, including 15 neonates who were 28 days or younger and 42 infants aged between 29 days and one year old.
Bacteremia was the most common invasive infection (31.9%), followed by osteomyelitis (22.4%) and abscess (19.8%). Sixty-four (55.2%) cases met the criteria for HA infections, and the remaining 52 cases were CA. Of these HA cases, two MRSA isolates were resistant to both clindamycin and trimethoprim/sulfamethoxazole and 33 MRSA isolates were resistant to only clindamycin.
Seventeen (14.7%) patients in this cohort died. The mortality risk increased significantly if the MRSA infections were HA (IRR: 1.63; 95% CI: 1.22–2.19) or caused by a MRSA isolate resistant to clindamycin and/or trimethoprim/sulfamethoxazole (IRR: 2.54; 95% CI: 1.69 – 3.76).
Molecular epidemiology of invasive MRSA infections
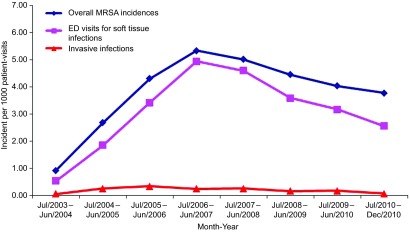
The MRSA isolates for 53 cases were available for molecular genotyping. The USA300 strain was the predominant type for both the HA-MRSA and CA-MRSA infections and accounted for 66.0% of the isolates. This was followed by the USA100 and USA200 strains combined (15.1%) and the USA500 strain (11.3%). Eight of the 12 osteomyelitis cases, eight of the 11 pneumonia cases, and seven of the 11 abscess cases were caused by the USA300 strain (Figure 2). One isolate of the USA300 strain developed resistance to clindamycin but remained susceptible to trimethoprim/sulfamethoxazole. MRSA USA100 and USA200 were mainly found in HA-MRSA pneumonias (n=2; 8%) and bacteremia (n=3, 12.5%). Of the 25 strains causing HA-MRSA infections, nine developed resistance to clindamycin but remained susceptible to trimethoprim/sulfamethoxazole. The distribution of the strain types among the five deaths was two for the USA100 strain, two for the USA 200 strain and one for the USA300 strain.
Figure 2.
Distribution of MRSA strain type by the infection site and source. CSF, cerebrospinal fluid.
DISCUSSION
In this retrospective study, we described the secular trends of MRSA infections identified among pediatric patients receiving medical careinour facility between July 2003 and December 2010. In this seven-year study, MRSA infections reached the highest incidence rate in 2007 and then declined steadily. The same pattern was observed among children in California16 and veterans in Atlanta17 and Maryland.18 These data seemed to suggest that the decline of MRSA infections might have affected adults and children in a growing number of geographic locations in the United States.
As expected,19,20 most of the MRSA cases identified in our study were skin and soft tissue infections encountered in the ED. These findings were similar to those reported by Gerber et al. who described the national trend, as well as characteristics, of S. aureus infections among patients seeking medical care in one of the 40 free-standing children's hospitals supplying administrative discharge data to the Pediatric Health Information System.
Gerber's study included patients discharged from one of the Pediatric Health Information System hospitals between 2002 and 2007. In contrast, our study has extended the study period to 2010 and was able to demonstrate a descending trend of MRSA infections that started in 2007. The decline of MRSA central line bloodstream infections among patients was seen in a subset of intensive care units participating in the National Healthcare Safety Network.21,22 Since the publication of the population-based national studies in 2006,4,13 many interventions, ranging from mandatory active screening in patients admitted to medical facilities to public health education campaigns on the prevention and control of MRSA in residential places, were implemented.23,24 Although we could not attribute the decline in MRSA infections observed in our study to any particular intervention, it was plausible that communities in a metropolitan area, such as the DC, were having increasing success in limiting the spread of MRSA.
The decline in the overall MRSA infection rate had a small impact on the proportion of MRSA in the total number of S. aureus isolates. In our study cohort, 70% of the S. aureus infections were MRSA infections. This proportion remained constant and was nearly double the national MRSA prevalence that was estimated prior to the wide spread of MRSA in communities.25 Therefore, the empirical management of all infections when S. aureus is suspected should include treatment for MRSA.
Despite the decline in overall incidence, MRSA remains a major health threat to individual pediatric patients. In particular, patients with a history of MRSA colonization are predisposed to invasive MRSA infections, which could be life threatening and carry a 15% crude mortality risk.
The USA300 strain was established as the predominant cause of community-acquired infection in the United States. Although the USA300 strain was commonly associated with skin and soft tissue infections, the USA300 strain has caused an increasing number of invasive infections, as previously reported.26,27 In a neonatal intensive care unit, the USA300 strain emerged as the principal clone by 2007.28 In contrast to previous studies, we found that the USA300 strain was not only responsible for a large proportion (up to 66%) of the overall MRSA infections, but it was also responsible for invasive infections, including pneumonia and osteomyelitis, in children and young adolescents.
As a single site epidemiology study, we recognize the inherent limitations, such as the lack of generalizability, in this study. Nonetheless, this study took place in a regional referral center that serves a large metropolitan area on the east coast of the United States. This study was further strengthened by the inclusion of a large cohort of nearly 4000 patients with lab confirmed MRSA infections. Second, limited by the information available for the study, we were unable to determine the factors that contributed to the decline in MRSA incidence. Particularly, because we only examined MRSA skin and soft tissue infections confirmed by a positive microbiology culture, it is plausible that an increased use of empirical management of skin infections without culturing had contributed to the decline in MRSA incidence. Third, limited by resources, we did not collect data on the drug susceptibility of the MRSA strains other than clindamycin and trimethoprim/sulfamethoxazole. Therefore, further studies are warranted to provide a more comprehensive description of the drug susceptibility patterns associated with MRSA strains and infections. Fourth, the information on the patients with invasive infections was extracted from electronic medical records. Although this approach reduced the information bias during documentation, incomplete charting could lead to gaps in knowledge. Finally, this study was limited by a small sample size of patients with invasive infections and a lack of information on the patient's underlying diseases to adequately control for confounders.
Taken together, this retrospective observational study noted that the incidence of MRSA infections peaked in 2007 and has since declined. Although invasive MRSA infections only accounted for a small portion, these infections were associated with a high mortality rate. The prevention and control of the spread of MRSA remains a crucial yet challenging task. Large multicenter- and population-based studies are needed to reassess the burden of MRSA infections one decade after its spread into communities and to determine the effectiveness of the current prevention strategies.
References
- Herold BC, Immergluck LC, Maranan MC, et al. Community-acquired methicillin-resistant Staphylococcus aureus in children with no identified predisposing risk. JAMA. 1998;279:593–598. doi: 10.1001/jama.279.8.593. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Four pediatric deaths from community-acquired methicillin-resistant Staphylococcus aureus—Minnesota and North Dakota, 1997–1999. MMWR Morb Mortal Wkly Rep. 1999;48:707–710. [PubMed] [Google Scholar]
- Groom AV, Wolsey DH, Naimi TS, et al. Community-acquired methicillin-resistant Staphylococcus aureus in a rural American Indian community. JAMA. 2001;286:1201–1205. doi: 10.1001/jama.286.10.1201. [DOI] [PubMed] [Google Scholar]
- Klevens RM, Morrison MA, Nadle J, et al. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA. 2007;298:1763–1771. doi: 10.1001/jama.298.15.1763. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Four pediatric deaths from community-acquired methicillin-resistant Staphylococcus aureus—Minnesota and North Dakota, 1997–1999. JAMA. 1999;282:1123–1125. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Methicillin-resistant Staphylococcus aureus skin or soft tissue infections in a state prison—Mississippi, 2000. JAMA. 2002;287:181–182. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Public health dispatch: outbreaks of community-associated methicillin-resistant Staphylococcus aureus skin infections—Los Angeles County, California, 2002–2003. JAMA. 2003;289:1377. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Outbreaks of community-associated methicillin-resistant Staphylococcus aureus skin infections—Los Angeles County, California, 2002–2003. MMWR Morb Mortal Wkly Rep. 2003;52:88. [PubMed] [Google Scholar]
- Barrett TW, Moran GJ.Update on emerging infections: news from the Centers for Disease Control and Prevention. Methicillin-resistant Staphylococcus aureus infections among competitive sports participants—Colorado, Indiana, Pennsylvania, and Los Angeles County, 2000–2003 Ann Emerg Med 20044343–45.discussion 45–47. [DOI] [PubMed] [Google Scholar]
- Begier EM, Frenette K, Barrett NL, et al. A high-morbidity outbreak of methicillin-resistant Staphylococcus aureus among players on a college football team, facilitated by cosmetic body shaving and turf burns. Clin Infect Dis. 2004;39:1446–1453. doi: 10.1086/425313. [DOI] [PubMed] [Google Scholar]
- Romano R, Lu D, Holtom P. Outbreak of community-acquired methicillin-resistant Staphylococcus aureus skin infections among a collegiate football team. J Athl Train. 2006;41:141–145. [PMC free article] [PubMed] [Google Scholar]
- Chen KT, Huard RC, Della-Latta P, Saiman L. Prevalence of methicillin-sensitive and methicillin-resistant Staphylococcus aureus in pregnant women. Obstet Gynecol. 2006;108:482–487. doi: 10.1097/01.AOG.0000227964.22439.e3. [DOI] [PubMed] [Google Scholar]
- Moran GJ, Amii RN, Abrahamian FM, Talan DA. Methicillin-resistant Staphylococcus aureus in community-acquired skin infections. Emerg Infect Dis. 2005;11:928–930. doi: 10.3201/eid1106.040641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran GJ, Talan DA. Community-associated methicillin-resistant Staphylococcus aureus: is it in your community and should it change practice. Ann Emerg Med. 2005;45:321–322. doi: 10.1016/j.annemergmed.2004.11.007. [DOI] [PubMed] [Google Scholar]
- Kallen AJ, Mu Y, Bulens S, et al. Health care-associated invasive MRSA infections, 2005–2008. JAMA. 2010;304:641–648. doi: 10.1001/jama.2010.1115. [DOI] [PubMed] [Google Scholar]
- Gutierrez K, Halpern MS, Sarnquist C, Soni S, Arroyo AC, Maldonado Y. Staphylococcal infections in children, California, USA, 1985–2009. Emerg Infect Dis. 2013;quiz 185;19:10–20. doi: 10.3201/eid1901.111740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stenehjem E, Stafford C, Rimland D. Reduction of methicillin-resistant Staphylococcus aureus infection among veterans in Atlanta. Infect Control Hosp Epidemiol. 2013;34:62–68. doi: 10.1086/668776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracy LA, Furuno JP, Harris AD, Singer M, Langenberg P, Roghmann MC. Staphylococcus aureus infections in US veterans, Maryland, USA, 1999–2008. Emerg Infect Dis. 2011;17:441–448. doi: 10.3201/eid1703.100502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerber JS, Coffin SE, Smathers SA, Zaoutis TE. Trends in the incidence of methicillin-resistant Staphylococcus aureus infection in children's hospitals in the United States. Clin Infect Dis. 2009;49:65–71. doi: 10.1086/599348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mongkolrattanothai K, Aldag JC, Mankin P, Gray BM. Epidemiology of community-onset Staphylococcus aureus infections in pediatric patients: an experience at a Children's Hospital in central Illinois. BMC Infect Dis. 2009;9:112. doi: 10.1186/1471-2334-9-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton DC, Edwards JR, Horan TC, Jernigan JA, Fridkin SK. Methicillin-resistant Staphylococcus aureus central line-associated bloodstream infections in US intensive care units, 1997–2007. JAMA. 2009;301:727–736. doi: 10.1001/jama.2009.153. [DOI] [PubMed] [Google Scholar]
- Gregory ML, Eichenwald EC, Puopolo KM. Seven-year experience with a surveillance program to reduce methicillin-resistant Staphylococcus aureus colonization in a neonatal intensive care unit. Pediatrics. 2009;123:e790–e796. doi: 10.1542/peds.2008-1526. [DOI] [PubMed] [Google Scholar]
- Tan TQ. The truth about “the superbug,” community-associated methicillin-resistant Staphylococcus aureus: what the practicing clinician needs to know. Arch Pediatr Adolesc Med. 2008;162:183–184. doi: 10.1001/archpediatrics.2007.56. [DOI] [PubMed] [Google Scholar]
- Tisinger CK. Empowering your patients in the fight against methicillin-resistant Staphylococcus aureus. J Am Acad Nurse Pract. 2008;20:204–211. doi: 10.1111/j.1745-7599.2007.00291.x. [DOI] [PubMed] [Google Scholar]
- Fridkin SK, Edwards JR, Tenover FC, Gaynes RP, McGowan JE., Jr Antimicrobial resistance prevalence rates in hospital antibiograms reflect prevalence rates among pathogens associated with hospital-acquired infections. Clin Infect Dis. 2001;33:324–330. doi: 10.1086/321893. [DOI] [PubMed] [Google Scholar]
- van de Griend P, Herwaldt LA, Alvis B, et al. Community-associated methicillin-resistant Staphylococcus aureus, Iowa, USA. Emerg Infect Dis. 2009;15:1582–1589. doi: 10.3201/eid1510.080877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiersma P, Tobin D'Angelo M, Daley WR, et al. Surveillance for severe community-associated methicillin-resistant Staphylococcus aureus infection. Epidemiol Infect. 2009;137:1674–1678. doi: 10.1017/S0950268809002490. [DOI] [PubMed] [Google Scholar]
- Carey AJ, Della-Latta P, Huard R, et al. Changes in the molecular epidemiological characteristics of methicillin-resistant Staphylococcus aureus in a neonatal intensive care unit. Infect Control Hosp Epidemiol. 2010;31:613–619. doi: 10.1086/652526. [DOI] [PMC free article] [PubMed] [Google Scholar]