Abstract
Rationale: The relationship between airway inflammation and obesity in severe asthma is poorly understood.
Objectives: We sought to determine the relationship between sputum mediator profiles and the distribution of eosinophilic inflammation and obesity in people with severe asthma.
Methods: Clinical parameters and eight mediators in sputum were assessed in 131 subjects with severe asthma from a single center categorized into lean, overweight, and obese groups defined by their body mass index. In an independent group of people with severe asthma (n = 45) and healthy control subjects (n = 19) eosinophilic inflammation was enumerated in bronchial submucosa, blood, and sputum and related to their body mass index.
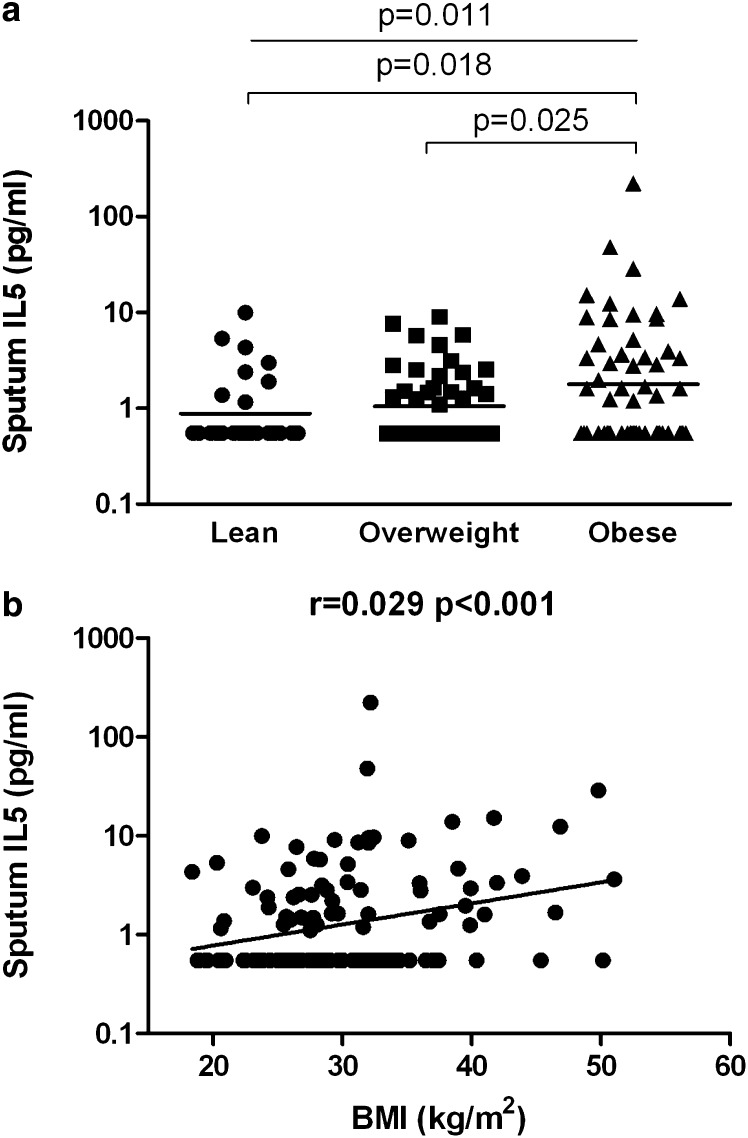
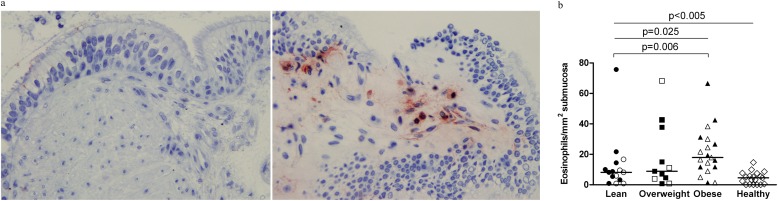
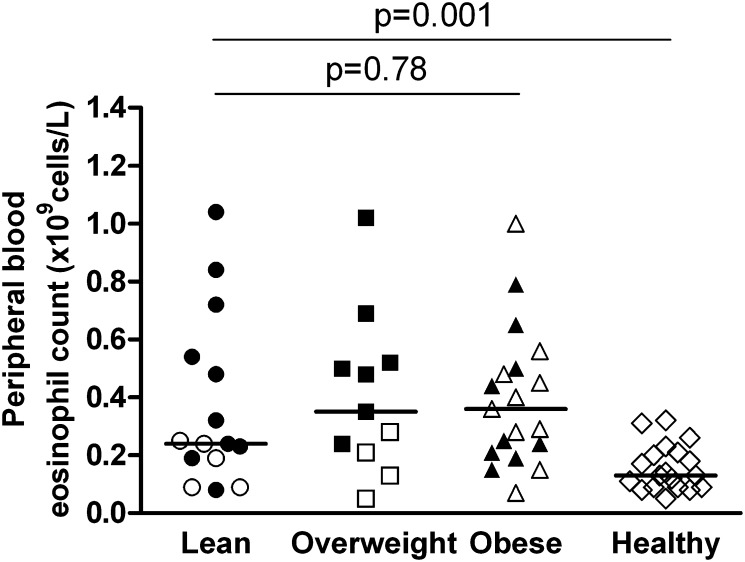
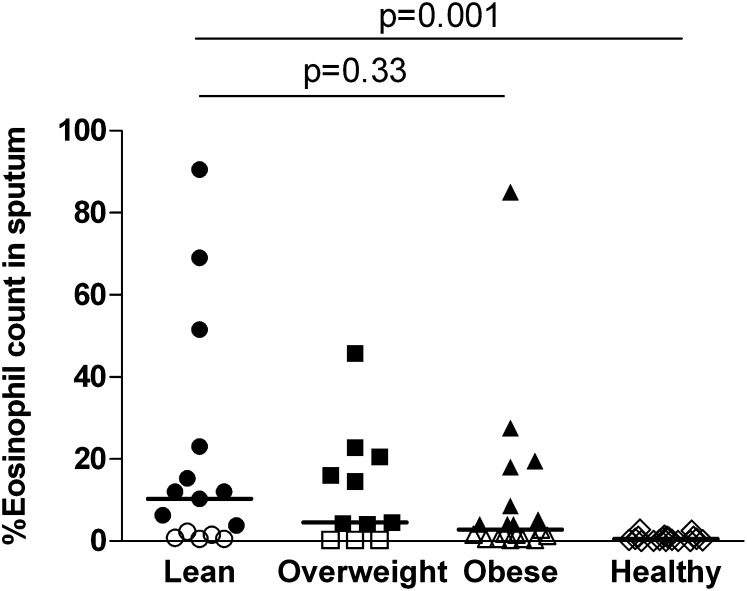
Measurements and Main Results: Sputum IL-5 geometric mean (95% confidence interval) (pg/ml) was elevated in the obese (1.8 [1.2–2.6]) compared with overweight (1.1 [0.8–1.3]; P = 0.025) and lean (0.9 [0.6–1.2]; P = 0.018) subjects with asthma and was correlated with body mass index (r = 0.29; P < 0.001). There was no relationship among body mass index, the sputum cell count, or other sputum mediators. In the bronchoscopy group the submucosal eosinophil number in the subjects with asthma was correlated with body mass index (Spearman rank correlation, rs = 0.38; P = 0.013) and the median (interquartile range) number of submucosal eosinophils was increased in obese (19.4 [11.8–31.2]) (cells per square millimeter) versus lean subjects (8.2 [5.4–14.6]) (P = 0.006). There was no significant association between sputum or peripheral blood eosinophil counts and body mass index.
Conclusions: Sputum IL-5 and submucosal eosinophils, but not sputum eosinophils, are elevated in obese people with severe asthma. Whether specific antieosinophilic therapy is beneficial, or improved diet and lifestyle in obese asthma has antiinflammatory effects beyond weight reduction, requires further study.
Keywords: asthma, obesity, cytokines, phenotypes, eosinophil
At a Glance Commentary
Scientific Knowledge on the Subject
Obesity and severe asthma are commonly associated. The relationship between airway inflammation and obesity in severe asthma is poorly understood.
What This Study Adds to the Field
Sputum IL-5 and submucosal eosinophils, but not sputum eosinophils, are elevated in obese people with severe asthma. Whether specific antieosinophilic therapy is beneficial, or improved diet and lifestyle in obese asthma has antiinflammatory effects, requires further study.
Asthma is a common, complex inflammatory disorder affecting about 5% of adults in the general population, of which approximately 5–10% suffer from severe disease (1, 2). Severe disease is often associated with comorbidities, such as obesity, and is particularly important because these patients suffer from substantial morbidity and consume a disproportionately high amount of the overall healthcare resources spent on asthma management (3–6).
Asthma, and in particular severe asthma, is a heterogeneous disease as highlighted by the different phenotypes identified using cluster analysis of clinical data (7–10) and cytokine profiles of airway samples (11–13). The key benefit of dividing a multidimensional disease, such as asthma, into distinct phenotypes is expected to be more effective treatment targeting. This has been effectively shown with the success of eosinophilic airway inflammation–directed corticosteroid (14–16) and anti–IL-5 treatment (17–19) to prevent asthma exacerbations in eosinophilic subjects with asthma. The association of obesity and asthma has been evident from epidemiologic studies, including case control studies and cross-sectional studies that have shown an increased risk of asthma in obese individuals based on the body mass index (BMI) (20–23). Emerging evidence suggests that obesity might represent a distinct severe asthma phenotype (6) with changes in exhaled nitric oxide metabolism (24) and macrophage function (25, 26). Its association with eosinophilic inflammation is contentious with some reports suggesting no association with sputum (27) or blood cell counts (6) and others suggesting there is a noneosinophilic obese phenotype (7).
We hypothesized that sputum mediator profiles and eosinophilic inflammation are differentially expressed among subjects with severe asthma categorized into normal, overweight, and obese subgroups. To test our hypothesis we measured in two independent groups of subjects with severe asthma stratified by their BMI sputum mediators and eosinophilic inflammation in the peripheral blood, bronchial submucosa, and sputum.
Methods
Subjects
We recruited three independent subject groups. The severe asthma “sputum cytokine profiling” group (n = 131) were recruited from a single center, the Difficult Asthma Clinic, Leicester, United Kingdom. All subjects had a clinician’s diagnosis of asthma requiring treatment step 4 or 5 according to GINA guidelines (2). A second group, the “bronchoscopy” group, included subjects with severe asthma recruited from the Difficult Asthma Clinic (n = 45) and healthy control subjects (n = 19). Sputum cytokine data from a group of patients with chronic obstructive pulmonary disease described previously (n = 34) was used as a disease control group (28). Written informed consent was obtained from all subjects and the study was approved by the Leicestershire, Northamptonshire, and Rutland ethics committee.
Protocol
Demographics and spirometry were recorded for all subjects. Reversibility was assessed after administration of 400 μg albuterol by a spacer device. Atopy was defined as a wheal 3 mm greater than control on skin-prick testing or specific IgE (Pharma CAP; ALK-Abelló, Madrid, Spain) to one or more of Dermatophagoides pteronyssinus, grass, tree, cat, dog, or Aspergillus fumigatus allergens. Sputum samples were collected in those subjects with asthma after spontaneous expectoration.
In the “sputum cytokine profiling” group asthma control was determined by the Asthma Control Questionnaire (29). Severe exacerbations were defined as worsening of symptoms requiring greater than or equal to 3 days of high-dose systemic corticosteroids (30). In the “bronchoscopy” group subjects underwent bronchoscopy in accordance with the British Thoracic Society guidelines within 1 week of their baseline assessment.
Sputum Processing and Cytokine Assessment
Sputum was selected, dispersed using mucolytic dithiothreitol, and processed to generate a sputum differential cell count and cell-free supernatants (31). Sputum mediator measurements were performed using the sensitive Meso Scale Discovery Platform (Meso Scale Discovery, Gaithersburg, MD) for eight mediators that we had previously established to be valid after spiking experiments (28). In half of the bronchoscopy subjects (n = 23) eosinophil proteins in sputum macrophages were assessed by quantifying the red hue of sputum macrophages on Romanovsky-stained cytospins as described previously (32).
Immunohistochemistry
The 2-μm sections from glycomethacrylate-embedded bronchial biopsies were stained using major basic protein monoclonal antibody (clone BMK13, Monosan; Caltag MedSystems, Buckingham, UK) or isotype control (DAKO, Ely, UK) and enumerated as eosinophils per square millimeter submucosa (33).
Statistical Analysis
Statistical analysis was performed using PRISM version 4 (GraphPad Software, San Diego, CA); SAS version 8.02 (SAS Institute, Inc., Cary, NC); and SPSS version 16 (SPSS, Inc., Chicago, IL). Data were independently coded and verified using R. Parametric and nonparametric data are presented as mean (standard error of the mean) and median (interquartile range), respectively. Log-transformed data are presented as geometric mean (95% confidence interval). Sputum cytokine concentrations and eosinophilic inflammation in different compartments were presented in the subjects with asthma stratified by BMI (<25 lean, 25 to <30 overweight, >30 obese). One-way analysis of variance with Tukey correction and Kruskal-Wallis test with Dunn intergroup comparison or unpaired t test and Mann-Whitney test were used to compare across groups for parametric and nonparametric data, respectively, as appropriate. A P value of less than 0.05 was taken as the threshold of statistical significance.
Results
In the severe asthma “sputum cytokine profiling” group the clinical characteristics of the lean, overweight, and obese groups were not significantly different except for a small difference in airflow obstruction, which was less evident in the obese group (Table 1). The sputum cytokine profiles were similar across the groups except for sputum IL-5 (Table 2) without a significant difference in the sputum eosinophil or neutrophil counts (Table 1). Sputum IL-5 geometric mean (95% confidence interval) (pg/ml) was elevated in the obese (1.8 [1.2–2.6]) compared with overweight (1.1 [0.8–1.3]; P = 0.025) and lean (0.9 [0.6–1.2]; P = 0.018) subjects with asthma (analysis of variance across groups, P = 0.011) (Table 2 and Figure 1a). Sputum IL-5 was correlated with BMI (r = 0.29; P < 0.001) (Figure 1b). There was no association between sputum IL-5 and other clinical parameters including age, sex, atopy, or medication. Similarly, in chronic obstructive pulmonary disease the sputum IL-5 concentration was correlated with BMI (r = 0.55; P < 0.001) (see Figure E1a in the online supplement) and significantly increased in those overweight and obese subjects compared with those with lean BMI (see Figure E1B).
TABLE 1.
CHARACTERISTICS OF SUBJECTS WITH ASTHMA CLASSIFIED BY THEIR BODY MASS INDEX
| All Subjects (n = 131) | Lean (n = 28) | Overweight (n = 48) | Obese (n = 55) | P Value | |
|---|---|---|---|---|---|
| Current age |
50 (1) |
51 (3) |
49 (2) |
51 (2) |
0.63 |
| Male, n (%) |
58 (44) |
12 (43) |
26 (54) |
20 (36) |
0.19 |
| Age of onset |
26 (2) |
24 (4) |
23 (3) |
29 (3) |
0.23 |
| BMI, kg/m2 |
30 (0.6) |
22.0 (0.4) |
27.5 (0.2) |
36.2 (0.8) |
<0.001 |
| Smoking history, pack-years |
5.1 (1.3) |
7.4 (2.1) |
2.9 (1.4) |
5.9 (2.7) |
0.42 |
| Severe exacerbations |
3.5 (0.3) |
3.6 (0.5) |
3.3 (0.4) |
3.6 (0.5) |
0.87 |
| ACQ6 score* |
2.4 (0.13) |
2.6 (0.26) |
2.4 (0.21) |
2.3 (0.22) |
0.82 |
| Oral corticosteroid use, n (%) |
70 (53) |
15 (54) |
27 (56) |
28 (51) |
0.75 |
| Daily prednisolone dose, mg |
6.0 (0.7) |
5.7 (1.2) |
6.6 (1.3) |
5.6 (1.0) |
0.78 |
| ICS dose† |
1,600 (1,000–2,000) |
1,600 (1,000–2,000) |
1,600 (1,265–2,000) |
2,000 (1,200–2,000) |
0.37 |
| Atopy present, n (%) |
59 (45) |
11 (39) |
23 (48) |
25 (46) |
0.76 |
| Total IgE, IU/L‡ |
156 (121–201) |
168 (84–339) |
172 (116–256) |
137 (95–200) |
0.77 |
| Pre-BD FEV1 |
2.1 (0.1) |
2.2 (0.2) |
2.0 (0.1) |
2.0 (0.1) |
0.54 |
| Pre-BD FEV1% predicted |
70.0 (1.9) |
76.2 (4.1) |
64.6 (3.3) |
71.6 (2.7) |
0.06 |
| Pre-BD FEV1/FVC ratio |
68.1 (1.2) |
65.6 (3.4) |
64.5 (2.0) |
72.3 (1.3) |
0.007 |
| BD reversibility %FEV1 |
8.8 (1.2) |
7.1 (2.5) |
11 (2.2) |
7.8 (1.8) |
0.39 |
| Post-BD FEV1% predicted |
75.3 (1.9) |
81.1 (4.3) |
70.9 (3.4) |
76.2 (2.7) |
0.14 |
| Eosinophils, %‡ |
3.1 (2.3–4.2) |
2.5 (1.3–4.8) |
3.0 (1.8–5.0) |
3.6 (2.3–5.7) |
0.70 |
| Neutrophils, %‡ |
55.6 (49.2–62.8) |
57.0 (44.0–74.0) |
58.3 (47.2–72.0) |
52.8 (43.4–64.2) |
0.77 |
| Total cell count (106/g sputum)‡ | 1.6 (1.2–2.1) | 1.2 (0.6–2.5) | 1.5 (0.9–2.5) | 1.9 (1.4–2.6) | 0.47 |
Definition of abbreviations: ACQ = Asthma Control Questionnaire; BD = bronchodilator; BMI = body mass index; ICS = inhaled corticosteroids.
Data expressed as mean (SEM) unless otherwise stated.
ACQ score was adjusted to remove effect of FEV1% predicted domain.
Doses of all inhaled corticosteroids were converted to the equivalent dose of beclomethasone dipropionate and expressed here as median dose (interquartile range).
Data expressed as geometric mean (95% confidence interval). P value based on analysis of variance for continuous variables.
TABLE 2.
SPUTUM MEDIATOR LEVELS IN THE GROUPS CLASSIFIED BY BODY MASS INDEX
| Mediators | All Subjects (n = 131) | Lean (n = 28) | Overweight (n = 48) | Obese (n = 55) | P Value* |
|---|---|---|---|---|---|
| Cytokines/receptors |
|
|
|
|
|
| IL-1β |
127 (94–171) |
128 (83–199) |
159 (88–288) |
105 (67–165) |
0.46 |
| IL-5 |
1.3 (1.0–1.5) |
0.9 (0.6–1.2) |
1.1 (0.8–1.3) |
1.8 (1.2–2.6) |
0.011 |
| IL-6 |
63 (48–84) |
68 (39–120) |
65 (39–108) |
60 (38–94) |
0.93 |
| IL-8 |
3,318 (2,280–4,830) |
4,945 (3,066–7,974) |
3,658 (2,028–6,596) |
2,525 (1,260–5,063) |
0.39 |
| TNF-α |
4.0 (2.9–5.3) |
3.5 (2.1–6.0) |
5.4 (2.9–9.8) |
3.2 (2.2–4.8) |
0.31 |
| Chemokines |
|
|
|
|
|
| CCL4 |
210 (150–293) |
215 (109–423) |
272 (156–474) |
167 (97–289) |
0.44 |
| CXCL10 |
481 (342–677) |
610 (302–1,234) |
481 (278–832) |
429 (241–766) |
0.75 |
| Growth factors |
|
|
|
|
|
| VEGF | 1,521 (1,258–1,840) | 1,670 (1,086–2,568) | 1,787 (1,334–2,394) | 1,272 (929–1,740) | 0.26 |
Definition of abbreviations: TNF = tumor necrosis factor; VEGF = vascular endothelial growth factor.
All data represented as geometric mean (95% confidence interval), all values are in pg/ml.
P value based on analysis of variance for continuous variables on log data.
Figure 1.
The relationship of sputum IL-5 and obesity in severe asthma. (a) Subjects are classified by their body mass index (BMI) (kg/m2) into lean (<24.9); overweight (≥25–29.9); and obese (≥30). The bar represents the geometric mean sputum IL-5 concentration (pg/ml). P value across the groups (ANOVA) is given above the solid line. For pairwise comparisons, P values are given above the line with markings at each end (unpaired t tests for exact P values, when Tukey’s post hoc test P < 0.05). (b) Correlation between sputum IL-5 and BMI.
We then considered whether the elevated sputum IL-5 in the overweight and obese subjects with severe asthma, in the absence of an increased sputum eosinophil count, might reflect eosinophilic inflammation in another compartment, such as the bronchial submucosa. We therefore stratified an independent population of subjects with severe asthma that underwent bronchoscopy (n = 45) into three groups based on their BMI and assessed the burden of eosinophilic inflammation in these groups and healthy control subjects (n = 19) in (1) bronchial submucosa, (2) peripheral blood, (3) sputum, and (4) red hue of eosin-stained sputum macrophages as a marker of eosinophil clearance. There were no significant differences in the clinical characteristics among the asthma groups (Table 3). The median (interquartile range) number of submucosal eosinophils was increased in severe asthma compared with healthy control subjects as a whole (Table 3). A representative example of submucosal eosinophil staining in an obese subject with asthma is as shown (Figure 2a). Submucosal eosinophil number were increased in the obese (19.4 [11.8–31.2]) (cells per square millimeter) versus lean subjects with asthma (8.2 [5.4–14.6]; P = 0.006) (Figure 2b). The submucosal eosinophil number in the subjects with asthma was correlated with BMI (Spearman rank correlation, rs = 0.38; P = 0.013) (see Table E1). Likewise, the peripheral blood eosinophil (Figure 3) count and sputum eosinophil count (Figure 4) were increased in severe asthma compared with healthy control subjects as a whole and in all three BMI-defined groups, but were not significantly different among the lean, overweight, and obese severe asthma groups. BMI was correlated with peripheral blood (rs = 0.32; P = 0.040), but not sputum eosinophil count (rs = −0.17; P = 0.30) (see Table E1). A smaller number of patients (n = 23) had eosinophilic protein measurement in their airway macrophages and there was no significant difference among groups, although the red hue was lowest in the obese severe asthma group (see Figure E2). In the healthy control subjects there were no significant correlations between the eosinophil number and BMI in any of the compartments (data not shown).
TABLE 3.
CHARACTERISTICS OF BRONCHIAL BIOPSY FROM SUBJECTS WITH ASTHMA AND HEALTHY CONTROL SUBJECTS
| Healthy Control Subjects (n = 19) | All Asthma Subjects (n = 45) | P Value | Lean (n = 15) | Overweight (n = 11) | Obese (n = 19) | P Value | |
|---|---|---|---|---|---|---|---|
| Current age |
40 (4) |
49 (1) |
0.012 |
49 (1) |
48 (1) |
50 (1) |
0.9 |
| Male, n (%) |
11 (57) |
20 (44) |
0.36 |
4 (26) |
7 (63) |
9 (47) |
0.29 |
| BMI, kg/m2 |
25.5 (0.9) |
29.7 (0.9) |
0.014 |
23.1 (0.4) |
27.1 (0.4) |
35.7 (1.1) |
<0.001 |
| Smoking history, pack-years |
0 |
1.5 (2) |
— |
1 (0.5) |
3 (2) |
0.5 (1.5) |
0.44 |
| Oral corticosteroid use, n (%) |
— |
14 (30) |
— |
2 (15) |
5 (45) |
7 (20) |
0.28 |
| Daily prednisolone dose, mg |
— |
11.5 (2) |
— |
6.5 (1.5) |
13.5 (4.5) |
13 (3) |
0.39 |
| ICS dose* |
— |
1,600 (640–4,000) |
— |
1,440 (1,000–4,000) |
1,600 (1,000–4,000) |
1,600 (640–4,000) |
0.90 |
| Atopy present, n (%) |
4 (21) |
21 (45) |
0.06 |
6 (40) |
5 (45) |
10 (52) |
0.80 |
| Total IgE, IU/L† |
— |
163 (86–310) |
— |
185 (80–427) |
203 (31–1,306) |
128 (53–284) |
0.43 |
| Pre-BD FEV1 |
3.3 (0.2) |
2.37 (0.11) |
<0.005 |
2.4 (0.2) |
2.4 (0.2) |
2.3 (0.2) |
0.83 |
| Pre-BD FEV1% predicted |
99.8 (3.6) |
80.8 (3.1) |
<0.005 |
87 (5.5) |
78 (7.4) |
77 (4.4) |
0.43 |
| Pre-BD FEV1/FVC ratio |
79 (0.01) |
72 (0.3) |
<0.005 |
78 (0.6) |
64 (0.8) |
71 (0.5) |
0.37 |
| Total cell count (106/g sputum) |
1.3 (0.8–2.2) |
2.3 (1.5–3.4) |
0.79 |
2.5 (0.8–5.4) |
1.6 (0.5–4.4) |
2.7 (1.6–4.6) |
0.60 |
| Sputum eosinophils, %‡ |
0.5 (0–1) |
4 (1.35–17) |
0.001 |
10.25 (1.5–23) |
4.2 (0.25–20.5) |
3 (1.25–8.5) |
0.33 |
| Sputum neutrophils, % |
56.6 (40.7–74.3) |
48.1 (37.6–61.5) |
0.43 |
40.5 (27.4–65.1) |
51 (36.3–71.7) |
59.3 (46.3–75.8) |
0.26 |
| Eosinophils/mm2 submucosa‡ |
4.6 (0.5–7.5) |
11.7 (6–25.6) |
<0.005 |
8.2 (5.4–14.6) |
8.8 (3.9–37.7) |
19.4 (11.8–31.2) |
0.025 |
| Peripheral blood eosinophil count (×109cells/L)‡ | 0.13 (0.09–0.23) | 0.29 (0.2–0.51) | 0.001 | 0.24 (0.19–0.54) | 0.35 (0.21–0.52) | 0.36 (0.21–0.5) | 0.78 |
Definition of abbreviations: BD = bronchodilator; BMI = body mass index; ICS = inhaled corticosteroids.
Subjects with asthma stratified by their BMI.
Data expressed as mean (SEM) unless otherwise stated.
Doses of all inhaled corticosteroids were converted to the equivalent dose of beclomethasone dipropionate and expressed here as median dose (range).
Data expressed as geometric mean (95% confidence interval).
Data expressed as median (interquartile range).
Figure 2.
Bronchial submucosal eosinophil count in subjects with severe asthma stratified by body mass index. (a) Photomicrograph of a bronchial biopsy from an obese subject with severe asthma showing isotype control (left) and major basic protein-stained eosinophils (right) (original magnification, ×200). (b) Subjects with asthma are classified by their body mass index (kg/m2) into lean (<24.9), overweight (≥25–29.9), and obese (≥30) and compared with healthy control subjects. The horizontal bar is the median. Open symbols denote subjects with sputum eosinophilia less than 3%; closed symbols denote subjects with sputum eosinophilia greater than or equal to 3%. P values for across and between group comparisons are as shown.
Figure 3.
Peripheral blood eosinophil count in subjects with severe asthma stratified by body mass index. Subjects with asthma are classified by their body mass index (kg/m2) into lean (<24.9), overweight (≥25–29.9), and obese (≥30) and compared with healthy control subjects. The horizontal bar is the median. Open symbols denote subjects with sputum eosinophilia less than 3%; closed symbols denote subjects with sputum eosinophilia greater than or equal to 3%. P values for across and between group comparisons are as shown.
Figure 4.
Sputum eosinophil count in subjects with severe asthma stratified by body mass index. Subjects with asthma are classified by their body mass index (kg/m2) into lean (<24.9), overweight (≥25–29.9), and obese (≥30) and compared with healthy control subjects. The horizontal bar is the median. Open symbols denote subjects with sputum eosinophilia less than 3%; closed symbols denote subjects with sputum eosinophilia greater than or equal to 3%. P values for across and between group comparisons are as shown.
Discussion
Here we have identified for the first time that obesity in severe asthma is associated with an elevated bronchial submucosal eosinophil number, and sputum IL-5 in the absence of an increased sputum eosinophil count. Our findings suggest that eosinophilic inflammation may play an important role in a group of obese subjects with asthma that hitherto have been labeled as noneosinophilic. This underscores the importance of the combination of clinical and biologic phenotyping with the inclusion of inflammatory profiles in different compartments in severe asthma to further understand the complexity of the disease.
In the sputum mediator profiling our most striking observation was the surprising finding that the overweight and obese groups with severe asthma were paradoxically associated with the highest sputum IL-5 concentration without a significant increase in the sputum eosinophil count. We believe this observation is robust and unlikely to be caused by chance because in addition to elevated sputum IL-5 in the obese subjects with severe asthma we found it was also elevated in a disease control group of obese subjects with chronic obstructive pulmonary disease, notwithstanding the heterogeneity in the sputum IL-5 concentration and relatively small numbers in each subgroup. Interestingly, an association between sputum Th2 cytokines and obesity in asthma has been challenged (34). However, in this earlier study sputum IL-5 was increased in obese subjects with asthma and control subjects combined compared with those subjects with a lean BMI and demonstrated a nonsignificant increase in sputum IL-5 in the obese subjects with asthma versus those with a lean BMI (P = 0.052) (34). Similarly, serum eotaxin levels were correlated with obesity and weight loss after bariatric surgery (35). In a recent 10-week intervention study of 38 subjects with asthma that underwent either weight reduction or exercise alone or in combination with weight reduction, subjects in the exercise-only arm had a significant reduction in sputum eosinophils (36). Taken together these small studies do begin to suggest a relationship between changes in body habitus and eosinophilic airway inflammation. Our findings might seem contrary to the current dogma of an association between obesity in asthma and noneosinophilic inflammation. However, studies have reported in asthma a decrease (37, 38) and no difference in the proportion of people with asthma that have a sputum eosinophilia (27, 39) between those with and without obesity. Here we again show that a sputum and peripheral blood eosinophil count is not elevated in obese subjects with severe asthma, but for the first time report an increase in submucosal eosinophils and sputum IL-5 in obese subjects with asthma. This apparent anomaly between an increased Th2 sputum cytokine profile in the absence of a sputum eosinophilia suggests that either eosinophil function is altered in obesity, such that response to CCR3 chemokines and Th2 cytokines is impaired, or that eosinophils are retained in the airway wall and possibly have an altered survival or adhesion within the airway wall.
To test this hypothesis we enumerated the number of eosinophils in the peripheral blood, bronchial submucosa, sputum, and eosinophil uptake by sputum macrophages in an independent group of subjects with severe asthma. Indeed, the number of submucosal eosinophils was increased in the obese subjects with severe asthma. This was associated with a trend to a reduction in the eosinophil clearance by macrophages, although this did not reach statistical significance. This increase in tissue, but not luminal airway eosinophilia, in obesity is entirely consistent with animal models. Murine models of asthma have shown that CC chemokines are up-regulated in obesity (40) with increased eosinophilia in lung tissue, but not bronchoalveolar lavage. Whether these tissue eosinophils are activated in obese people with asthma and contribute to disease needs to be further investigated.
Noneosinophilic asthma defined by sputum cell counts is associated with a poor response to corticosteroids and obesity itself is associated with corticosteroid insensitivity. Therefore, it is recognized that this group responds poorly to inhaled or systemic corticosteroid therapy. This questions the clinical importance of a bronchial submucosal eosinophilia in obese asthma. However, after corticosteroid therapy and specific anti–IL-5 monoclonal therapy submucosal eosinophils are incompletely attenuated (41) suggesting that this important immunopathologic feature of asthma is refractory to current therapy. Given that the presence of airway eosinophilia has convincingly been shown to drive exacerbation frequency, further randomized controlled trials are indicated to assess whether the target population for novel eosinophil-targeted therapies is much greater than first anticipated. Thus, it remains a possibility that the tissue eosinophilia in this group is clinically important and their reduction may translate into meaningful clinical outcomes. Whether alternative strategies to reduce eosinophilic inflammation by targeting the IL-5 receptor (42), CRTh2 (43), or important eosinophil-derived cytokines, such as IL-13 (44, 45), have efficacy in obese people with asthma needs to be tested.
Our findings also underscore the importance of obesity as a driver for the production of numerous proinflammatory cytokines and suggest that obesity may contribute to the inflammatory burden in asthma and cause increased work of breathing, as a consequence of extrathoracic restriction. Therefore, strategies targeted at diet and lifestyle to reduce obesity including bariatric surgery may indeed have an antiinflammatory role beyond simply weight reduction and may contribute to the benefits in lung function observed after successful weight reduction (46, 47).
Our study has a number of potential limitations. We have focused on severe asthma because this group represents the patients with the greatest unmet need. Whether our findings are consistent across disease severity needs to be studied. Adherence to therapy was not systematically assessed (48) and therefore we cannot completely exclude the possibility that some of the differences observed among the groups stratified by BMI are in part caused by differences in adherence to therapy. Our findings would have been strengthened by further increasing the granularity of our assessments to include additional mediators, molecular phenotyping, such as genomic, epigenomic, and transcriptomic analysis (49, 50). We have not assessed fully the environmental exposure to allergens, occupational sensitizers and irritants, pollutants, or pathogens. Our study also only includes measures at stable visits and does not include assessments at exacerbations. The integration of transcriptomic, proteomic, and cellular data, longitudinally and at times of instability, will provide further insight into the phenotypic complexity of severe asthma. The specificity of BMI as a measure of fat-free mass has been questioned, but we have previously reported that BMI and fat-free mass index are very closely related in severe asthma (27). Recent studies have suggested that a fatty diet might promote neutrophilic inflammation (51). The subjects’ diets were not formally assessed in this study and future studies should relate body habitus and diet to airway inflammation.
In conclusion, we have undertaken a comprehensive analysis of the clinical, cellular, and sputum mediator profiles of severe asthma. Our most important observation was that in the absence of a sputum eosinophilia obese subjects with severe asthma have elevated sputum IL-5 and eosinophils in their airway wall. This has important implications in the understanding of the impact of obesity in the immunopathology of asthma. It questions the view on the choice of current and future biologic therapy in this group, and highlights the importance of strategies to improve diet and lifestyle that may provide benefits in terms of weight reduction, reduced risk of comorbidities, and as suggested here eosinophilic airway inflammation.
Acknowledgments
Acknowledgment
The authors express their gratitude to Beverley Hargadon, Maria Shelly, William Monteiro, and Vijay Mistry.
Footnotes
Supported by MedImmune and grants from GlaxoSmithKline; C.E.B. is a Wellcome Trust Senior Clinical Fellow, and the research was performed in laboratories in part funded by the European Regional Development Fund (ERDF 05567). This article presents independent research partly funded by the National Institute for Health Research (NIHR). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health. The Wellcome Trust, NIHR, and the European Regional Development Fund had no involvement in the design of the study, data collection, analysis and interpretation of the data, writing of the manuscript, or decision to submit the manuscript. Coauthors from MedImmune and GlaxoSmithKline research groups were involved in the design of the study, its interpretation, writing of the manuscript, and approval of its submission.
Author Contributions: D.D., M.B., A.S., P.H., S. Siddiqui, and S. Shah were involved in the recruitment of volunteers and in data collection. F.A.S., D.D., and C.E.B. were involved in the immunohistochemistry. J.W. undertook the sputum mediator assessment. N.K. and C.E.B. were involved in the macrophage color assessment. C.N., A.H., D.D., P.H., and C.E.B. were involved in statistical analyses and interpretation. D.D., S.G., M.B., P.H., A.S., P.B., R.G., N.K., I.P., R.D.M., A.J.W., and C.E.B. were involved in the design of the study and interpretation. D.D., A.J.W., and C.E.B. were involved in the study design, volunteer recruitment, data collection, data interpretation, and data analysis, and had full access to the data and are responsible for the integrity of the data and final decision to submit. All authors contributed to the writing of the manuscript and have approved the final version for submission.
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.201208-1470OC on April 3, 2013
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.British Thoracic Society/Scottish Intercollegiate Guidelines NetworkAsthma guidelines [accessed 2012 Dec 27]. Available from: www.brit-thoracic.org.uk/guidelines/asthma-guidelines.aspx
- 2.Global Initiative for Asthma Guidelines [accessed 2012 Dec 27]. Available from: www.ginasthma.org/Guidelines/guidelines-resources.html
- 3.Chanez P, Wenzel SE, Anderson GP, Anto JM, Bel EH, Boulet LP, Brightling CE, Busse WW, Castro M, Dahlen B, et al. Severe asthma in adults: what are the important questions? J Allergy Clin Immunol. 2007;119:1337–1348. doi: 10.1016/j.jaci.2006.11.702. [DOI] [PubMed] [Google Scholar]
- 4.American Thoracic Society. Proceedings of the ATS workshop on refractory asthma: current understanding, recommendations, and unanswered questions. Am J Respir Crit Care Med. 2000;162:2341–2351. doi: 10.1164/ajrccm.162.6.ats9-00. [DOI] [PubMed] [Google Scholar]
- 5.Bousquet J, Mantzouranis E, Cruz AA, Aït-Khaled N, Baena-Cagnani CE, Bleecker ER, Brightling CE, Burney P, Bush A, Busse WW, et al. Uniform definition of asthma severity, control, and exacerbations: document presented for the World Health Organization Consultation on Severe Asthma. J Allergy Clin Immunol. 2010;126:926–938. doi: 10.1016/j.jaci.2010.07.019. [DOI] [PubMed] [Google Scholar]
- 6.Gibeon D, Batuwita R, Osmond M, Heaney JG, Brightling CE, Niven RM, Mansur AH, Chaudri R, Bucknall CE, Rowe A, et al. Obesity associated severe asthma represents a distinct clinical phenotype. Analysis of the British Thoracic Society Difficult Asthma Registry patient cohort according to body mass index. Chest. 2013;143:406. doi: 10.1378/chest.12-0872. [DOI] [PubMed] [Google Scholar]
- 7.Haldar P, Pavord ID, Shaw DE, Berry MA, Thomas M, Brightling CE, Wardlaw AJ, Green RH. Cluster analysis and clinical asthma phenotypes. Am J Respir Crit Care Med. 2008;178:218–224. doi: 10.1164/rccm.200711-1754OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moore WC, Meyers DA, Wenzel SE, Teague WG, Li H, Li X, D’Agostino R, Jr, Castro M, Curran-Everett D, Fitzpatrick AM, et al. National Heart, Lung, and Blood Institute’s Severe Asthma Research Program. Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am J Respir Crit Care Med. 2010;181:315–323. doi: 10.1164/rccm.200906-0896OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta S, Siddiqui S, Haldar P, Entwisle JJ, Mawby D, Wardlaw AJ, Bradding P, Pavord ID, Green RH, Brightling CE. Quantitative analysis of high-resolution computed tomography scans in severe asthma subphenotypes. Thorax. 2010;65:775–781. doi: 10.1136/thx.2010.136374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anderson GP. Endotyping asthma: new insights into key pathogenic mechanisms in a complex, heterogeneous disease. Lancet. 2008;372:1107–1119. doi: 10.1016/S0140-6736(08)61452-X. [DOI] [PubMed] [Google Scholar]
- 11.Brasier AR, Victor S, Boetticher G, Ju H, Lee C, Bleecker ER, Castro M, Busse WW, Calhoun WJ.Molecular phenotyping of severe asthma using pattern recognition of bronchoalveolar lavage-derived cytokines J Allergy Clin Immunol 200812130–37., e6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brasier AR, Victor S, Ju H, Busse WW, Curran-Everett D, Bleecker E, Castro M, Chung KF, Gaston B, Israel E, et al. Predicting intermediate phenotypes in asthma using bronchoalveolar lavage-derived cytokines. Clin Transl Sci. 2010;3:147–157. doi: 10.1111/j.1752-8062.2010.00204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bhavnani SK, Victor S, Calhoun WJ, Busse WW, Bleecker E, Castro M, Ju H, Pillai R, Oezguen N, Bellala G, et al. How cytokines co-occur across asthma patients: from bipartite network analysis to a molecular-based classification. J Biomed Inform. 2011;44:S24–S30. doi: 10.1016/j.jbi.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Green RH, Brightling CE, McKenna S, Hargadon B, Parker D, Bradding P, Wardlaw AJ, Pavord ID. Asthma exacerbations and sputum eosinophil counts: a randomised controlled trial. Lancet. 2002;360:1715–1721. doi: 10.1016/S0140-6736(02)11679-5. [DOI] [PubMed] [Google Scholar]
- 15.Jayaram L, Pizzichini MM, Cook RJ, Boulet LP, Lemière C, Pizzichini E, Cartier A, Hussack P, Goldsmith CH, Laviolette M, et al. Determining asthma treatment by monitoring sputum cell counts: effect on exacerbations. Eur Respir J. 2006;27:483–494. doi: 10.1183/09031936.06.00137704. [DOI] [PubMed] [Google Scholar]
- 16.Chlumský J, Striz I, Terl M, Vondracek J. Strategy aimed at reduction of sputum eosinophils decreases exacerbation rate in patients with asthma. J Int Med Res. 2006;34:129–139. doi: 10.1177/147323000603400202. [DOI] [PubMed] [Google Scholar]
- 17.Haldar P, Brightling CE, Hargadon B, Gupta S, Monteiro W, Sousa A, Marshall RP, Bradding P, Green RH, Wardlaw AJ, et al. Mepolizumab and exacerbations of refractory eosinophilic asthma. N Engl J Med. 2009;360:973–984. doi: 10.1056/NEJMoa0808991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nair P, Pizzichini MM, Kjarsgaard M, Inman MD, Efthimiadis A, Pizzichini E, Hargreave FE, O’Byrne PM. Mepolizumab for prednisone-dependent asthma with sputum eosinophilia. N Engl J Med. 2009;360:985–993. doi: 10.1056/NEJMoa0805435. [DOI] [PubMed] [Google Scholar]
- 19.Pavord ID, Korn S, Howarth P, Bleecker ER, Buhl R, Keene ON, Ortega H, Chanez P. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet. 2012;380:651–659. doi: 10.1016/S0140-6736(12)60988-X. [DOI] [PubMed] [Google Scholar]
- 20.Sin DD, Jones RL, Man SF. Obesity is a risk factor for dyspnea but not for airflow obstruction. Arch Intern Med. 2002;162:1477–1481. doi: 10.1001/archinte.162.13.1477. [DOI] [PubMed] [Google Scholar]
- 21.Young SYN, Gunzenhauser JD, Malone KE, McTiernan A. Body mass index and asthma in the military population of the northwestern United States. Arch Intern Med. 2001;161:1605–1611. doi: 10.1001/archinte.161.13.1605. [DOI] [PubMed] [Google Scholar]
- 22.Ford ES.The epidemiology of obesity and asthma J Allergy Clin Immunol 2005115897–909., quiz 910 [DOI] [PubMed] [Google Scholar]
- 23.Boulet L-P. Influence of obesity on the prevalence and clinical features of asthma. Clin Invest Med. 2008;31:E386–E390. doi: 10.25011/cim.v31i6.4926. [DOI] [PubMed] [Google Scholar]
- 24.Holguin F, Comhair SA, Hazen SL, Powers RJ, Khatri SS, Bleecker ER, Busse WW, Calhoun WJ, Castro M, Fitzpatrick AM, et al. An association between L-arginine/ADMA balance, obesity and the age of asthma onset phenotype. Am J Respir Crit Care Med. 2013;187:153–159. doi: 10.1164/rccm.201207-1270OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fernandez-Boyanapalli R, Goleva E, Kolakowski C, Min E, Day B, Leung DY, Riches DW, Bratton DL, Sutherland ER. Obesity impairs apoptotic cell clearance in asthma. J Allergy Clin Immunol. 2013;131:1041–1047. doi: 10.1016/j.jaci.2012.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lugogo NL, Hollingsworth JW, Howell DL, Que LG, Francisco D, Church TD, Potts-Kant EN, Ingram JL, Wang Y, Jung SH, et al. Alveolar macrophages from overweight/obese subjects with asthma demonstrate a proinflammatory phenotype. Am J Respir Crit Care Med. 2012;186:404–411. doi: 10.1164/rccm.201109-1671OC. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 27.Bafadhel M, Singapuri A, Terry S, Hargadon B, Monteiro W, Green RH, Bradding PH, Wardlaw AJ, Pavord ID, Brightling CE.Body mass and fat mass in refractory asthma: an observational 1 year follow-up study J Allergy (Cairo) 20102010:251758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bafadhel M, Saha S, Siva R, McCormick M, Monteiro W, Rugman P, Dodson P, Pavord ID, Newbold P, Brightling CE. Sputum IL-5 concentration is associated with a sputum eosinophilia and attenuated by corticosteroid therapy in COPD. Respiration. 2009;78:256–262. doi: 10.1159/000221902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Juniper EF, Svensson K, Mörk AC, Ståhl E. Measurement properties and interpretation of three shortened versions of the asthma control questionnaire. Respir Med. 2005;99:553–558. doi: 10.1016/j.rmed.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 30.Reddel HK, Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, Casale TB, Chanez P, Enright PL, Gibson PG, et al. American Thoracic Society/European Respiratory Society Task Force on Asthma Control and Exacerbations. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med. 2009;180:59–99. doi: 10.1164/rccm.200801-060ST. [DOI] [PubMed] [Google Scholar]
- 31.Pavord ID, Pizzichini MM, Pizzichini E, Hargreave FE. The use of induced sputum to investigate airway inflammation. Thorax. 1997;52:498–501. doi: 10.1136/thx.52.6.498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kulkarni NS, Hollins F, Sutcliffe A, Saunders R, Shah S, Siddiqui S, Gupta S, Haldar P, Green R, Pavord I, et al. Eosinophil protein in airway macrophages: a novel biomarker of eosinophilic inflammation in patients with asthma J Allergy Clin Immunol 201012661–69., e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brightling CE, Bradding P, Symon FA, Holgate ST, Wardlaw AJ, Pavord ID. Mast-cell infiltration of airway smooth muscle in asthma. N Engl J Med. 2002;346:1699–1705. doi: 10.1056/NEJMoa012705. [DOI] [PubMed] [Google Scholar]
- 34.Sutherland TJ, Cowan JO, Young S, Goulding A, Grant AM, Williamson A, Brassett K, Herbison GP, Taylor DR. The association between obesity and asthma: interactions between systemic and airway inflammation. Am J Respir Crit Care Med. 2008;178:469–475. doi: 10.1164/rccm.200802-301OC. [DOI] [PubMed] [Google Scholar]
- 35.Vasudevan AR, Wu H, Xydakis AM, Jones PH, Smith EO, Sweeney JF, Corry DB, Ballantyne CM. Eotaxin and obesity. J Clin Endocrinol Metab. 2006;91:256–261. doi: 10.1210/jc.2005-1280. [DOI] [PubMed] [Google Scholar]
- 36.Scott HA, Gibson PG, Garg ML, Pretto JJ, Morgan PJ, Callister R, Wood LG. Dietary restriction and exercise improve airway inflammation and clinical outcomes in overweight and obese asthma: a randomized trial. Clin Exp Allergy. 2013;43:36–49. doi: 10.1111/cea.12004. [DOI] [PubMed] [Google Scholar]
- 37.van Veen IH, Ten Brinke A, Sterk PJ, Rabe KF, Bel EH. Airway inflammation in obese and nonobese patients with difficult-to-treat asthma. Allergy. 2008;63:570–574. doi: 10.1111/j.1398-9995.2007.01597.x. [DOI] [PubMed] [Google Scholar]
- 38.Telenga ED, Tideman SW, Kerstjens HA, Hacken NH, Timens W, Postma DS, van den Berge M. Obesity in asthma: more neutrophilic inflammation as a possible explanation for a reduced treatment response. Allergy. 2012;67:1060–1068. doi: 10.1111/j.1398-9995.2012.02855.x. [DOI] [PubMed] [Google Scholar]
- 39.Todd DC, Armstrong S, D’Silva L, Allen CJ, Hargreave FE, Parameswaran K. Effect of obesity on airway inflammation: a cross-sectional analysis of body mass index and sputum cell counts. Clin Exp Allergy. 2007;37:1049–1054. doi: 10.1111/j.1365-2222.2007.02748.x. [DOI] [PubMed] [Google Scholar]
- 40.Calixto MC, Lintomen L, Schenka A, Saad MJ, Zanesco A, Antunes E. Obesity enhances eosinophilic inflammation in a murine model of allergic asthma. Br J Pharmacol. 2010;159:617–625. doi: 10.1111/j.1476-5381.2009.00560.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Flood-Page PT, Menzies-Gow AN, Kay AB, Robinson DS. Eosinophil’s role remains uncertain as anti-interleukin-5 only partially depletes numbers in asthmatic airway. Am J Respir Crit Care Med. 2003;167:199–204. doi: 10.1164/rccm.200208-789OC. [DOI] [PubMed] [Google Scholar]
- 42.Kolbeck R, Kozhich A, Koike M, Peng L, Andersson CK, Damschroder MM, Reed JL, Woods R, Dall’acqua WW, Stephens GL, et al. MEDI-563, a humanized anti-IL-5 receptor alpha mAb with enhanced antibody-dependent cell-mediated cytotoxicity function J Allergy Clin Immunol 20101251344–1353., e2 [DOI] [PubMed] [Google Scholar]
- 43.Barnes N, Pavord I, Chuchalin A, Bell J, Hunter M, Lewis T, Parker D, Payton M, Collins LP, Pettipher R, et al. A randomized, double-blind, placebo-controlled study of the CRTH2 antagonist OC000459 in moderate persistent asthma. Clin Exp Allergy. 2012;42:38–48. doi: 10.1111/j.1365-2222.2011.03813.x. [DOI] [PubMed] [Google Scholar]
- 44.Corren J, Lemanske RF, Hanania NA, Korenblat PE, Parsey MV, Arron JR, Harris JM, Scheerens H, Wu LC, Su Z, et al. Lebrikizumab treatment in adults with asthma. N Engl J Med. 2011;365:1088–1098. doi: 10.1056/NEJMoa1106469. [DOI] [PubMed] [Google Scholar]
- 45.Piper E, Brightling CE, Niven R, Oh C, Faggioni R, Poon K, She D, Kell C, May RD, Geba GP, et al. A phase II placebo-controlled study of tralokinumab in moderate-to-severe asthma. Eur Respir J. 2013;41:330–338. doi: 10.1183/09031936.00223411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Haselkorn T, Fish JE, Chipps BE, Miller DP, Chen H, Weiss ST. Effect of weight change on asthma-related health outcomes in patients with severe or difficult-to-treat asthma. Respir Med. 2009;103:274–283. doi: 10.1016/j.rmed.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 47.Boulet LP, Turcotte H, Martin J, Poirier P. Effect of bariatric surgery on airway response and lung function in obese subjects with asthma. Respir Med. 2012;106:651–660. doi: 10.1016/j.rmed.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 48.Gamble J, Stevenson M, McClean E, Heaney LG. The prevalence of nonadherence in difficult asthma. Am J Respir Crit Care Med. 2009;180:817–822. doi: 10.1164/rccm.200902-0166OC. [DOI] [PubMed] [Google Scholar]
- 49.Baines KJ, Simpson JL, Wood LG, Scott RJ, Gibson PG.Transcriptional phenotypes of asthma defined by gene expression profiling of induced sputum samples J Allergy Clin Immunol 2011127153–160., 160, e1–e9 [DOI] [PubMed] [Google Scholar]
- 50.Woodruff PG, Modrek B, Choy DF, Jia G, Abbas AR, Ellwanger A, Koth LL, Arron JR, Fahy JV. T-helper type 2-driven inflammation defines major subphenotypes of asthma. Am J Respir Crit Care Med. 2009;180:388–395. doi: 10.1164/rccm.200903-0392OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Scott HA, Gibson PG, Garg ML, Wood LG. Airway inflammation is augmented by obesity and fatty acids in asthma. Eur Respir J. 2011;38:594–602. doi: 10.1183/09031936.00139810. [DOI] [PubMed] [Google Scholar]