Abstract
Background:
Changes in the long-term survival of people admitted to hospital is unknown. This study examined trends in 1-year survival of patients admitted to hospital adjusted for improved survival in the general population.
Methods:
One-year survival after admission to hospital was determined for all adults admitted to hospital in Ontario in 1994, 1999, 2004, or 2009 by linking to vital statistics datasets. Annual survival in the general population was determined from life tables for Ontario.
Results:
Between 1994 and 2009, hospital use decreased (from 8.8% to 6.3% of the general adult population per year), whereas crude 1-year mortality among people with hospital admissions increased (from 9.2% to 11.6%). During this time, patients in hospital became significantly older (median age increased from 51 to 58 yr) and sicker (the proportion with a Charlson comorbidity index score of 0 decreased from 68.2% to 60.0%), and were more acutely ill on admission (elective admissions decreased from 47.4% to 42.0%; proportion brought to hospital by ambulance increased from 16.1% to 24.8%). Compared with 1994, the adjusted odds ratio (OR) for death at 1 year in 2009 was 0.78 (95% confidence interval [CI] 0.77–0.79). However, 1-year risk of death in the general population decreased by 24% during the same time. After adjusting for improved survival in the general population, risk of death at 1 year for people admitted to hospital remained significantly lower in 2009 than in 1994 (adjusted relative excess risk 0.81, 95% CI 0.80–0.82).
Interpretation:
After accounting for both the increased burden of patient sickness and improved survival in the general population, 1-year survival for people admitted to hospital increased significantly from 1994 to 2009. The reasons for this improvement cannot be determined from these data.
Hospitals have a special place in most health care systems. Hospital staff care for the people with the most serious illnesses and the most vulnerable. They are frequently the location of many life-defining moments — including birth, surgery, acute medical illness and death — of many people and their families. Hospitals serve as a focus in the training of most physicians. In addition, they consume a considerable proportion of health care expenditures worldwide. 1
Given the prominence of hospitals in health care systems, measuring outcomes related to hospital care is important. In particular, the measurement of trends for outcomes of hospital care can help us to infer whether the care provided to hospital patients is improving. Previous such studies have focused on survival trends for specific diseases or patients who received treatment in specific departments. 2 – 12 None of these studies have adjusted for survival trends in the general population, the adjustment for which is important to determine whether changes in survival of patients in hospital merely reflect changes in the overall population. In this study, whether or not patient outcomes have changed over time was determined by examining trends in 1-year survival in all patients admitted to hospital, adjusting for improved survival in the general population.
Methods
Study design and data sources
This study used 2 population-based administrative databases to identify patients admitted to hospital in Ontario during the study period: the Discharge Abstract Database, which records demographic and diagnostic information on all nonpsychiatric admissions to hospital, and the Registered Persons Database, which records the date of death for all residents of Ontario.
Study period and population
Population life tables for Ontario were used to measure trends in 1-year survival of adults admitted to hospital relative to the general population. At the time of the study, 2009 was the latest year for which life tables were available. To measure trends in survival of patients admitted to hospital, 5-year decrements from 2009 were selected to the earliest year possible given the data available in the Discharge Abstract Database and Registered Persons Database (i.e., 1991).
The Discharge Abstract Database was used to identify all adults (defined as age > 20 yr) admitted to any Ontario acute care hospital in 1994, 1999, 2004 or 2009. Exclusions included same-day surgeries, admissions to psychiatric facilities (because their data are captured in another data set), and admissions to in-patient rehabilitation or long-term care facilities (because they are distinct from acute care hospitals). In addition, patients ineligible for health care coverage in Ontario were excluded because the capture of their outcomes would be incomplete. Only the first admission for each person in each year was used in the analysis.
Outcome measures
The primary outcome was all-cause mortality within 1 year of admission to hospital. This outcome was chosen instead of in-hospital mortality to account for potential temporal changes in several factors, including patient discharge thresholds (which could decrease over time as lengths of stay decrease, thereby potentially decreasing in-hospital mortality at the expense of an increased risk of death after discharge) and home-based palliative care services after admission to hospital (the increased prevalence of such services over time and increasing prevalence of dying at home for patients with recent stays in hospital 13 could decrease the risk of death in hospital). The Registered Persons Database was used to determine whether patients died within the year following their admission date.
Covariates were identified from each person’s Discharge Abstract Database record and included age, sex, urgency of the admission (elective or urgent), whether the patient arrived by ambulance, admission service (medical, surgical or obstetrics–gynecology) and comorbidity. Comorbidity was measured using the Charlson comorbidity index score, as calculated by diagnoses coded in each person’s index Discharge Abstract Database record, as well as those coded for all admissions to hospital within the previous year. To calculate the final Charlson comorbidity index score, the International Classification of Diseases, 9th revision, clinical modification (ICD-9-CM), and International Classification of Diseases, 10th revision (ICD-10), diagnostic codes were grouped into the Charlson medical conditions using methods from Quan and colleagues 14 and weights from Schneeweiss and colleagues. 15 Finally, admissions were categorized into primary diagnosis groups using the ICD-9-CM code for their most responsible diagnosis; to do this for the 2004 and 2009 cohorts, ICD-10 codes were first converted to ICD-9-CM using “cross-walks” from the Canadian Institute for Health Information.
Statistical analysis
Ontario adult population estimates from Statistics Canada for each study year were used to calculate rates of hospital use. Multivariate binomial logistic regression was used to measure the independent association of admission year with risk of death at 1 year adjusted for patient factors (age, sex and Charlson comorbidity index score) and admission covariates (urgency, service and ambulance status). To further delineate trends in survival, this model was repeated for secondary outcomes, including death in hospital and death after discharge (up to 1 year after admission).
Ontario life tables for each study year were used to determine the annual risk of death in the general population for all age–sex strata. Methods from Dickman and colleagues 16 , 17 were used to measure the unadjusted 1-year risk of death for patients in hospital relative to the Ontario population. This unadjusted relative survival was calculated as the ratio of observed survival (calculated as e − x , where x is the observed number of deaths divided by the total observation time) to expected survival (determined from provincial life tables). To compare relative survival between years, standardized weighted mean relative survival was calculated using weights based on age proportions from all 4 years in the study period.
Multivariate relative survival models were then used to measure trends of 1-year survival in patients in hospital, adjusting for patient-level covariates, as well as the improved survival of the general population. Relative survival models are additive hazards models in which the total hazard (or risk) of death in the patient group is the sum of the known hazard in the general population and the excess hazard in the patient group. 17 The hazard for the general population was determined from Ontario life tables. The parameter estimates for the full relative survival model were determined with a Poisson error structure in SAS 9.3 17 and were exponentiated to calculate the relative excess risk. 18 The relative excess risk quantifies the change in death risk relative to the comparator group, adjusted for model covariates and changes in population survival over time.
Results
During the 4 years studied, a total of 3 616 026 nonpsychiatric admissions to hospital for adults occurred in Ontario. Of these admissions, 1 060 123 were excluded because they were repeat admissions, for a total of 2 555 903 adult residents of Ontario with at least 1 admission during the study period. Population-based rates of admission to hospital decreased significantly between 1994 and 2009 (8.8% v. 6.3%, Mantel–Haenszel χ 2 for trend 41 478, p < 0.001) ( Table 1 ).
Table 1:
Characteristics of hospital admissions, by year
| Characteristic | Study year, no. (%) * | |||
|---|---|---|---|---|
| 1994 | 1999 | 2004 | 2009 | |
| Ontario adult population, no. | 7 866 531 | 8 410 845 | 9 259 115 | 9 967 803 |
| Adults with ≥ 1 admissions to hospital † | 691 414 (8.8) | 615 461 (7.3) | 621 166 (6.7) | 627 862 (6.3) |
| Death within 1 yr of admission date ‡ | 63 839 (9.2) | 66 698 (10.8) | 69 021 (11.1) | 72 763 (11.6) |
| Age, yr, median (IQR) | 51 (32–70) | 55 (35–73) | 56 (36–74) | 58 (36–75) |
| Female sex | 435 799 (63.0) | 387 720 (63.0) | 388 313 (62.5) | 391 232 (62.3) |
| Charlson Comorbidity Index score | ||||
| 0 | 471 306 (68.2) | 384 044 (62.4) | 399 750 (64.4) | 376 922 (60.0) |
| 1–2 | 137 215 (19.8) | 136 196 (22.1) | 126 145 (20.3) | 135 433 (21.6) |
| 3–4 | 46 152 (6.7) | 51 497 (8.4) | 47 765 (7.7) | 59 185 (9.4) |
| ≥ 5 | 36 741 (5.3) | 43 724 (7.1) | 47 506 (7.6) | 56 322 (9.0) |
| Elective admission | 327 629 (47.4) | 261 631 (42.5) | 260 404 (41.9) | 263 435 (42.0) |
| Arrival by ambulance | 111 309 (16.1) | 116 887 (19.0) | 126 044 (20.3) | 156 021 (24.8) |
| Admitting service | ||||
| Medicine | 285 402 (41.3) | 273 770 (44.5) | 278 922 (44.9) | 280 837 (44.7) |
| Surgical | 222 641 (32.2) | 182 414 (29.6) | 183 050 (29.5) | 188 021 (29.9) |
| Obstetrics–Gynecology | 183 371 (26.5) | 159 277 (25.9) | 159 194 (25.6) | 159 004 (25.3) |
| Primary diagnosis group | ||||
| Complications of pregnancy, childbirth and puerperium | 148 327 (21.5) | 128 010 (20.9) | 130 534 (21.1) | 134 177 (21.5) |
| Diseases of the circulatory system | 102 260 (14.8) | 101 418 (16.5) | 95 409 (15.4) | 87 539 (14.0) |
| Diseases of the digestive system | 87 863 (12.7) | 66 718 (10.9) | 67 295 (10.9) | 67 282 (10.8) |
| Diseases of the genitourinary system | 62 609 (9.1) | 53 286 (8.7) | 49 077 (7.9) | 45 720 (7.3) |
| Neoplasms | 48 244 (7.0) | 47 564 (7.7) | 48 102 (7.8) | 48 447 (7.7) |
| Injury and poisoning | 50 056 (7.3) | 45 738 (7.5) | 46 834 (7.6) | 48 320 (7.7) |
| Diseases of the musculoskeletal system and connective tissue | 41 532 (6.0) | 37 560 (6.1) | 40 841 (6.6) | 47 487 (7.6) |
| Diseases of the respiratory system | 42 210 (6.1) | 41 359 (6.7) | 35 202 (5.7) | 36 872 (5.9) |
| Symptoms, signs and ill-defined conditions | 35 745 (5.2) | 35 044 (5.7) | 37 963 (6.1) | 32 513 (5.2) |
| Endocrine, nutritional, metabolic diseases and immunity disorders | 13 131 (1.9) | 12 622 (2.1) | 14 075 (2.3) | 15 431 (2.5) |
| Factors influencing health status and contact with health services | 9 613 (1.4) | 8 603 (1.4) | 16 467 (2.7) | 20 245 (3.2) |
| Diseases of the nervous system and sense organs | 18 414 (2.7) | 11 597 (1.9) | 12 584 (2.0) | 11 190 (1.8) |
| Infectious and parasitic diseases | 7 437 (1.1) | 6 614 (1.1) | 7 399 (1.2) | 11 212 (1.8) |
| Mental disorders | 8 164 (1.2) | 6 727 (1.1) | 6 852 (1.1) | 7 990 (1.3) |
| Diseases of the skin and subcutaneous tissue | 8 248 (1.2) | 5 712 (0.9) | 5 212 (0.8) | 4 799 (0.8) |
| Diseases of the blood and blood-forming organs | 4 108 (0.6) | 3 909 (0.6) | 4 740 (0.8) | 5 129 (0.8) |
| Other | 1 735 (0.3) | 1 299 (0.2) | 895 (0.1) | 1 089 (0.2) |
Unless otherwise stated.
Mantel–Haenszel χ 2 value for trend 41 478 ( p < 0.001).
Mantel–Haenszel χ 2 value for trend 2 247 ( p < 0.001).
From 1994 to 2009, crude mortality 1 year after admission increased progressively from 9.2% to 11.6% (χ 2 for trend 2247, p < 0.001) ( Table 1 ). However, patients admitted to hospital during this time were progressively older and sicker ( Table 1 ): the median age of patients increased from 51 to 58 years, the proportion of patients with scores of 0 on the Charlson comorbidity index decreased from 68.2% to 60.0%, the proportion of patients admitted electively decreased from 47.4% to 42.0%, and the proportion of patients brought to hospital by ambulance increased from 16.1% to 24.8%. Overall, the proportion of patients within each primary diagnosis group was consistent throughout the study.
After adjusting for changes in patient characteristics over the years studied, the 1-year risk of death decreased significantly between 1994 and 2004. Independent of patient age, sex and comorbidity, admission urgency and service, and ambulance status, the 1-year adjusted odds of death were 22% lower in 2009 than in 1994 (adjusted odds ratio [OR] 0.78, 95% CI 0.77–0.79) ( Table 2 , model A). The adjusted relative odds of death increased notably with patient age (adjusted OR 43.8, 95% CI 40.1–47.9 in patients aged ≥ 95 yr v. patients aged < 25 yr) and comorbidity burden (adjusted OR 17.0, 95% CI 16.8–17.3 for patients with Charlson comorbidity index score ≥ 5 v. 0). Compared with patients admitted to medical wards, the adjusted odds of death were 37% lower in patients admitted to surgical wards (adjusted OR 0.63, 95% CI 0.63–0.64) and 78% lower in patients admitted to an obstetrics–gynecology service (adjusted OR 0.22, 95% CI 0.20–0.23). The logistic model had excellent discrimination ( C statistic 0.896) and very good calibration (Appendix 1, available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.130875/-/DC1 ). Significant improvements between 1994 and 2009 were also seen when the model outcome was either death in hospital or death after discharge (Appendix 2, available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.130875/-/DC1 ).
Table 2:
Odds of death within 1 year of admission to hospital
| Factor | Model A: Adjusted OR (95% CI) | Model B: Relative survival, * excess risk (95% CI) |
|---|---|---|
| Study year | ||
| 1994 | 1.00 (ref) | 1.00 (ref) |
| 1999 | 0.92 (0.91–0.94) | 0.93 (0.91–0.94) |
| 2004 | 0.90 (0.89–0.91) | 0.92 (0.91–0.93) |
| 2009 | 0.78 (0.77–0.79) | 0.81 (0.80–0.82) |
| Patient age, yr | ||
| 20–25 | 1.00 (ref) | 1.00 (ref) |
| 25–29 | 1.09 (0.98–1.22) | 1.16 (1.03–1.30) |
| 30–34 | 1.37 (1.24–1.51) | 1.44 (1.30–1.60) |
| 35–39 | 1.95 (1.78–2.13) | 1.96 (1.77–2.16) |
| 40–44 | 2.69 (2.46–2.94) | 2.53 (2.30–2.78) |
| 44–49 | 3.25 (2.98–3.54) | 2.90 (2.65–3.19) |
| 50–55 | 3.94 (3.62–4.29) | 3.33 (3.04–3.65) |
| 55–59 | 4.56 (4.19–4.96) | 3.69 (3.36–4.04) |
| 60–64 | 5.42 (4.98–5.89) | 4.11 (3.76–4.51) |
| 65–69 | 6.37 (5.86–6.92) | 4.50 (4.11–4.93) |
| 70–75 | 7.54 (6.94–8.19) | 4.87 (4.44–5.33) |
| 75–79 | 9.28 (8.54–10.1) | 5.31 (4.85–5.81) |
| 80–84 | 11.9 (11.0–13.0) | 5.85 (5.34–6.40) |
| 85–89 | 16.0 (14.8–17.4) | 6.44 (5.88–7.06) |
| 90–94 | 25.0 (23.0–27.2) | 8.08 (7.37–8.86) |
| ≥ 95 | 43.8 (40.1–47.9) | 10.58 (9.59–11.7) |
| Female sex | 0.8 (0.79–0.81) | 0.89 (0.88–0.91) |
| Charlson comorbidity index score | ||
| 0 | 1.00 (ref) | 1.00 (ref) |
| 1–2 | 2.85 (2.81–2.89) | 4.93 (4.82–5.04) |
| 3–4 | 4.60 (4.53–4.67) | 8.87 (8.66–9.08) |
| ≥ 5 | 17.0 (16.8–17.3) | 26.8 (26.2–27.4) |
| Elective admission | 0.57 (0.56–0.58) | 0.54 (0.54–0.55) |
| Arrival by ambulance | 1.70 (1.68–1.71) | 1.58 (1.56–1.60) |
| Admitting service | ||
| Medicine | 1.00 (ref) | 1.00 (ref) |
| Surgery | 0.63 (0.63–0.64) | 0.62 (0.61–0.63) |
| Obstetrics–Gynecology | 0.22 (0.20–0.23) | 0.20 (0.19–0.22) |
Note: CI = confidence interval, OR = odds ratio.
Relative excess risk quantifies risk of death relative to the comparator group adjusted for model covariables and changes in population survival over time.
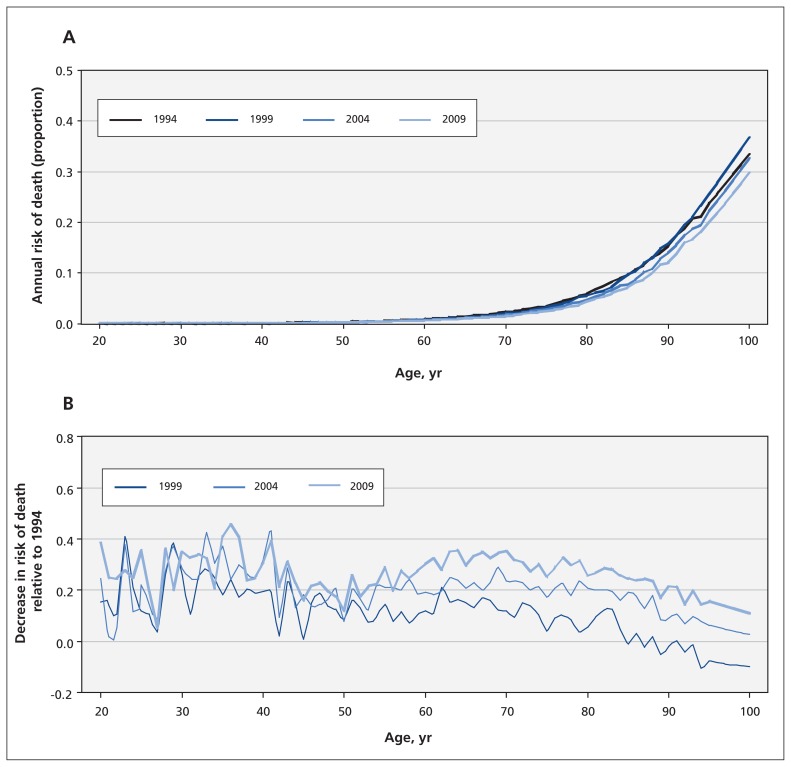
Changes in survival in the general population
The annual risk of death in the general population notably decreased during the study period for most age groups ( Figure 1A ). During all 4 years studied, the annual risk increased significantly with patient age, but decreased throughout the study period (relative to 1994 values) within almost all age strata ( Figure 1B ). For people under 50 years of age, the annual risk of death (relative to 1994) decreased by 18% in 1999, 22% in 2004 and 28% in 2009 (data not shown). More consistent separation in survival between the years was seen in people 50 years of age and older: relative to 1994, the average relative death risk in this age group decreased progressively by 4% in 1999, 14% in 2004 and 22% in 2009 (data not shown).
Figure 1:
Annual risk of death for adults in Ontario, 1994–2009. (A) Annual risk of death in each study cohort year for all adults. (B) Decrease in annual risk of death relative to 1994.
Survival of patients in hospital relative to the general population
Survival of patients discharged from hospital relative to the general population decreased as patients aged. For women, the average relative survival (over all 4 years studied) was 99.8% for women 20 years of age, 94.8% for women 50 years of age and 80.3% in women 80 years of age, respectively (data not shown). Relative survival was significantly lower for men, with corresponding values of 98.8%, 93.4% and 73.6% (data not shown). Unadjusted relative survival in the entire population (accounting for the significantly increased age of the population in hospital in 2009 v. 1994) decreased slightly for both women (92.1% in 1994 v. 91.2% in 2009) and men (89.2% in 1994 v. 88.5% in 2009) (data not shown).
Relative survival of patients in hospital was poorest in strata defined by covariables that increased the risk of death. For example, unadjusted relative survival decreased as Charlson comorbidity index score increased ( Table 3 ). Similar patterns were seen for admission urgency, ambulance status and admission service ( Table 3 ). After standardizing for significant changes in the age structure of patients admitted to hospital, unadjusted relative survival changed minimally within all covariable strata.
Table 3:
Age- and sex-standardized 1-year relative survival of patients with hospital admissions by patient group and study year
| Patient group | Study year, relative survival, % | |||
|---|---|---|---|---|
| 1994 | 1999 | 2004 | 2009 | |
| Charlson comorbidity index score | ||||
| 0 | 93.9 | 93.4 | 93.4 | 93.4 |
| 1–2 | 87.1 | 86.0 | 86.2 | 86.1 |
| 3–4 | 83.7 | 82.2 | 82.3 | 82.2 |
| ≥ 5 | 84.8 | 83.4 | 83.6 | 83.5 |
| Admission urgency | ||||
| Elective | 94.4 | 94.0 | 94.0 | 94.0 |
| Urgent | 88.4 | 87.4 | 87.5 | 87.3 |
| Arrival by ambulance | ||||
| No | 92.6 | 92.0 | 92.1 | 92.1 |
| Yes | 84.5 | 83.0 | 83.1 | 82.9 |
| Admitting service | ||||
| Medicine | 87.0 | 85.9 | 86.0 | 85.9 |
| Surgical | 90.5 | 89.7 | 89.8 | 89.8 |
| Obstetrics–Gynecology | 98.3 | 98.2 | 98.1 | 98.1 |
Significant increases in 1-year survival for patients in hospital were seen in the adjusted relative survival model ( Table 2 , model B). After accounting for notable improvements in survival for the general population ( Figure 1B ) and adjusting for the important covariables that influence patient outcomes ( Table 1 ), 1-year risk of death for patients admitted to hospital decreased significantly throughout the study period ( Table 4 ). Improved adjusted relative survival was consistent in all patient strata but appeared to vary significantly by patient age and Charlson comorbidity index score. Improved relative survival between 1994 and 2009 was particularly prominent in younger patients, as patient comorbidity increased, and in patients with diseases of the circulatory system, nervous system and blood or blood-forming organs, as well as infectious or parasitic diseases.
Table 4:
Changes in adjusted excess risk of death at 1 year relative to 1994 in specific patient groups
| Patient group | Excess risk of death, adjusted * HR (95% CI) | ||
|---|---|---|---|
| 1999 | 2004 | 2009 | |
| Overall | 0.926 (0.914–0.939) | 0.918 (0.906–0.930) | 0.806 (0.796–0.897) |
| Age, yr | |||
| < 50 | 0.846 (0.807–0.888) | 0.868 (0.828–0.911) | 0.780 (0.743–0.819) |
| 50–69 | 0.870 (0.849–0.891) | 0.875 (0.854–0.896) | 0.759 (0.741–0.777) |
| 70–79 | 0.930 (0.909–0.952) | 0.920 (0.899–0.942) | 0.797 (0.778–0.816) |
| ≥ 80 | 1.002 (0.978–1.026) | 0.977 (0.955–1.000) | 0.883 (0.864–0.903) |
| Sex | |||
| Female | 0.931 (0.913–0.949) | 0.941 (0.924–0.959) | 0.825 (0.809–0.840) |
| Male | 0.924 (0.907–0.941) | 0.897 (0.881–0.914) | 0.789 (0.775–0.803) |
| Charlson comorbidity index score | |||
| 0 | 1.088 (1.032–1.148) | 1.203 (1.144–1.264) | 1.201 (1.143–1.262) |
| 1–2 | 0.919 (0.897–0.942) | 0.992 (0.968–1.017) | 0.861 (0.840–0.883) |
| 3–4 | 0.936 (0.911–0.962) | 0.886 (0.862–0.911) | 0.786 (0.765–0.808) |
| ≥ 5 | 0.890 (0.873–0.908) | 0.846 (0.830–0.863) | 0.750 (0.736–0.765) |
| Admission urgency | |||
| Elective | 0.937 (0.924–0.950) | 0.939 (0.926–0.952) | 0.839 (0.828–0.851) |
| Urgent | 0.957 (0.920–0.995) | 0.891 (0.855–0.929) | 0.656 (0.628–0.684) |
| Arrival by ambulance | |||
| No | 0.899 (0.883–0.915) | 0.918 (0.901–0.935) | 0.802 (0.787–0.817) |
| Yes | 0.961 (0.943–0.980) | 0.926 (0.909–0.944) | 0.830 (0.815–0.845) |
| Admitting service | |||
| Medicine | 0.961 (0.943–0.980) | 0.926 (0.909–0.944) | 0.830 (0.815–0.845) |
| Surgery | 0.946 (0.914–0.979) | 0.884 (0.854–0.915) | 0.709 (0.684–0.734) |
| Obstetrics–Gynecology | 0.903 (0.751–1.086) | 1.182 (0.992–1.409) | 0.829 (0.689–0.997) |
| Primary diagnosis group | |||
| Diseases of the circulatory system | 0.903 (0.880–0.926) | 0.865 (0.843–0.888) | 0.713 (0.694–0.733) |
| Diseases of the digestive system | 0.980 (0.930–1.033) | 0.979 (0.930–1.030) | 0.840 (0.799–0.883) |
| Diseases of the genitourinary system | 1.006 (0.923–1.097) | 1.019 (0.940–1.106) | 0.874 (0.808–0.945) |
| Neoplasms | 0.913 (0.892–0.935) | 0.903 (0.882–0.925) | 0.778 (0.759–0.797) |
| Injury and poisoning | 1.123 (1.053–1.198) | 1.085 (1.017–1.158) | 0.987 (0.927–1.051) |
| Diseases of musculoskeletal system | 1.103 (0.954–1.276) | 1.014 (0.875–1.176) | 0.770 (0.664–0.893) |
| Diseases of the respiratory system | 0.984 (0.947–1.022) | 1.099 (1.059–1.141) | 1.006 (0.970–1.044) |
| Symptoms, signs and ill-defined conditions | 1.071 (0.999–1.149) | 1.131 (1.057–1.209) | 1.063 (0.995–1.136) |
| Endocrine, nutritional, metabolic and immune diseases | 0.960 (0.888–1.039) | 0.976 (0.905–1.052) | 0.864 (0.802–0.931) |
| Factors influencing health status and contact with health services | 1.026 (0.955–1.103) | 1.030 (0.964–1.101) | 1.379 (1.296–1.467) |
| Diseases of the nervous system and sense organs | 1.038 (0.928–1.161) | 0.813 (0.728–0.907) | 0.701 (0.628–0.783) |
| Infectious and parasitic diseases | 0.743 (0.681–0.810) | 0.894 (0.825–0.969) | 0.727 (0.675–0.783) |
| Mental disorders | 1.074 (0.956–1.207) | 1.073 (0.957–1.204) | 1.051 (0.944–1.169) |
| Diseases of the skin and subcutaneous tissue | 1.369 (1.145–1.637) | 1.532 (1.288–1.822) | 1.328 (1.118–1.579) |
| Diseases of the blood and blood-forming organs | 1.072 (0.966–1.191) | 0.934 (0.842–1.035) | 0.734 (0.661–0.816) |
Interpretation
Hospital care is common and consumes a large proportion of health care resources. It is therefore important to measure trends in outcomes of patients admitted to hospital to help gauge the performance of this component of the health care system. This retrospective cohort study found that, between 1994 and 2009, hospital use in Ontario decreased, but patient sickness increased. In addition, the crude 1-year risk of death for patients with hospital admissions increased, but decreased when adjusted for important confounders. During the same period, all-cause risk of death in the general population decreased, but this trend did not explain the improved 1-year adjusted survival seen in patients with hospital admissions. This study identifies important improvements in health outcomes in a very common patient population.
A study by Ford and colleagues 19 attributed reduced mortality trends in coronary artery disease to medical treatment and risk factor modification. These mechanisms could also explain improved survival in patients admitted to hospital. Improved survival may reflect advances in medical care since the early 1990s, such as interventions for acute coronary syndromes, 20 aggressive use of statin and antiplatelet therapy in chronic coronary artery disease, 20 the use of angiotensin-converting enzyme (ACE) inhibitors, angiotensin-receptor blockers and β-blockers for congestive heart failure, 20 implantable cardioverter defibrillators for sudden cardiac death, 20 aromatase inhibitors and other hormone treatments for breast cancer, 21 and effective antiretroviral therapy for AIDS. 22 This trend may also reflect increased uptake of evidence-based treatments. For example, studies have shown increased use of evidence-based treatments for cardiovascular diseases including β-blockers, statins, ACE inhibitors and angiotensin-receptor blockers in patients after myocardial infarction 23 and in patients with congestive heart failure. 24
In addition to advances in treatments and increased use of such improvements, the positive effects of preventive health strategies might further explain these results. It is possible that a greater focus on lifestyle modifications over the study period contributed to the improved outcomes of patients admitted to hospital.
Limitations
The earliest date of the study was 1994 owing to data availability. It is possible that improved patient survival would have been more extensive if one had been able to look back further in time. In addition, it is uncertain whether these results are generalizable to other jurisdictions. Because the data required for this study are available in many countries, these analyses could be replicated in other provinces and countries to determine whether similar results are seen elsewhere. It cannot be determined whether — and to what extent — the increased patient Charlson comorbidity score is due to more complete diagnostic coding over time. If this potential bias was pervasive, then the odds of death would be biased down for later years in the adjusted model. This problem is unlikely to explain the study’s findings for 2 reasons: almost all hospital physicians who were clinically active during the study period would state that patients have become sicker over time; and the stratified model suggested that patients with a Charlson comorbidity index score of 0 had a significantly worse outcome over time ( Table 4 ), a result that would not be expected with “up-coding,” because patients in each of the index’s strata would be getting healthier over time.
Finally, it is possible that changes in admission patterns could explain some decrease in risk of death over time. For example, patients with a poor prognosis (such as an undefined metastatic cancer or a palliative case) may have been more likely to be admitted to hospital (for work-up or palliation) in 1994 than in 2009. This would increase the prevalence of patients with a poor prognosis in early years of study observation. However, given that survival improvements were seen in a broad assortment of patient populations ( Table 4 ), it is unlikely that such potential changes would explain the study’s results.
Conclusion
This study noted significant improvement between 1994 and 2009 in survival of patients admitted to hospital in Ontario. Because admissions to hospital are so common, and the drop in the risk of death is so extensive, these changes translate into a meaningful decrease in life-years lost.
Supplementary Material
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Disclaimer: This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
References
- 1. Anderson GF . In search of value: an international comparison of cost, access and outcomes . Health Aff (Millwood) 1997 . ; 16 : 163 – 71 . [DOI] [PubMed] [Google Scholar]
- 2. Joynt KE , Orav EJ , Jha AK . Mortality rates for Medicare beneficiaries admitted to critical access and non-critical access hospitals, 2002–2010 . JAMA 2013 . ; 309 : 1379 – 87 . [DOI] [PubMed] [Google Scholar]
- 3. Kaboli PJ , Go JT , Hockenberry J , et al. . Associations between reduced hospital length of stay and 30-day readmission rate and mortality: 14-year experience in 129 Veterans Affairs hospitals . Ann Intern Med 2012 . ; 157 : 837 – 45 . [DOI] [PubMed] [Google Scholar]
- 4. Lenihan CR , Montez-Rath ME , Mora Mangano CT , et al. . Trends in acute kidney injury, associated use of dialysis, and mortality after cardiac surgery, 1999 to 2008 . Ann Thorac Surg 2013 . ; 95 : 20 – 8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yeung DF , Boom NK , Guo H , et al. . Trends in the incidence and outcomes of heart failure in Ontario, Canada: 1997 to 2007 . CMAJ 2012 . ; 184 : E765 – 73 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Coles AH , Fisher KA , Darling C , et al. . Recent trends in post-discharge mortality among patients with an initial acute myocardial infarction . Am J Cardiol 2012 . ; 110 : 1073 – 7 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Girotra S , Nallamothu BK , Spertus JA , et al. . Trends in survival after in-hospital cardiac arrest . N Engl J Med 2012 . ; 367 : 1912 – 20 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kirksey M , Chiu YL , Ma Y , et al. . Trends in in-hospital major morbidity and mortality after total joint arthroplasty: United States 1998–2008 . Anesth Analg 2012 . ; 115 : 321 – 7 . [DOI] [PubMed] [Google Scholar]
- 9. Lindenauer PK , Lagu T , Shieh MS , et al. . Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003–2009 . JAMA 2012 . ; 307 : 1405 – 13 . [DOI] [PubMed] [Google Scholar]
- 10. Anjum A , von Allmen R , Greenhalgh R , et al. . Explaining the decrease in mortality from abdominal aortic aneurysm rupture . Br J Surg 2012 . ; 99 : 637 – 45 . [DOI] [PubMed] [Google Scholar]
- 11. Chen J , Normand SL , Wang Y , et al. . National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998–2008 . JAMA 2011 . ; 306 : 1669 – 78 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Moxey PW , Hofman D , Hinchliffe RJ , et al. . Trends and outcomes after surgical lower limb revascularization in England . Br J Surg 2011 . ; 98 : 1373 – 82 . [DOI] [PubMed] [Google Scholar]
- 13. Wilson DM , Truman CD , Thomas R , et al. . The rapidly changing location of death in Canada . Soc Sci Med 2009 . ; 68 : 1752 – 8 . [DOI] [PubMed] [Google Scholar]
- 14. Quan H , Sundararajan V , Halfon P , et al. . Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data . Med Care 2005 . ; 43 : 1130 – 9 . [DOI] [PubMed] [Google Scholar]
- 15. Schneeweiss S , Wang PS , Avorn J , et al. . Improved comorbidity adjustment for predicting mortality in Medicare populations . Health Serv Res 2003 . ; 38 : 1103 – 20 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dickman PW . Estimating and modelling relative survival using SAS . 2004 . . Available: http://biostat3.net/download/sas/relative_survival_using_sas.pdf ( accessed 2013 Sep. 9 ).
- 17. Dickman PW , Sloggett A , Hills M , et al. . Regression models for relative survival . Stat Med 2004 . ; 23 : 51 – 64 . [DOI] [PubMed] [Google Scholar]
- 18. Suissa S . Relative excess risk: an alternative measure of comparative risk . Am J Epidemiol 1999 . ; 150 : 279 – 82 . [DOI] [PubMed] [Google Scholar]
- 19. Ford ES , Ajani UA , Croft JB , et al. . Explaining the decrease in US deaths from coronary disease, 1980–2000 . N Engl J Med 2007 . ; 356 : 2388 – 98 . [DOI] [PubMed] [Google Scholar]
- 20. Teo KK . Recent advances. Cardiology . BMJ 1998 . ; 316 : 911 – 5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Howell A , Dowsett M . Recent advances in endocrine therapy of breast cancer . BMJ 1997 . ; 315 : 863 – 6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cohn JA . Recent advances. HIV infection — I . BMJ 1997 . ; 314 : 487 – 91 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Austin PC , Tu JV , Ko DT , et al. . Use of evidence-based therapies after discharge among elderly patients with acute myocardial infarction . CMAJ 2008 . ; 179 : 895 – 900 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lee DS , Mamdani MM , Austin PC , et al. . Trends in heart failure outcomes and pharmacotherapy: 1992 to 2000 . Am J Med 2004 . ; 116 : 581 – 9 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.