Abstract
The past 20 years have been witness to a growing knowledge base of research highlighting the critical importance of cognition in understanding functional status and outcome in schizophrenia. This work has led to an increased emphasis on identifying and evaluating treatments that enhance cognition in schizophrenia, with the hope that this would translate into a better quality of life and improved outcome for patients. At the same time, this research has raised new questions about the specificity of cognitive impairments to schizophrenia and the degree to which similar cognitive impairments may be present in other disorders that can involve psychotic symptoms (eg, schizoaffective disorder, bipolar disorder, and psychotic major depression). This article provides a brief overview of work comparing cognitive function across the nonaffective and affective psychoses and highlights areas of similarity and dissimilarity in the role cognition plays in these disorders.
Introduction
Researchers have long recognized that individuals with schizophrenia experience challenges in a wide range of cognitive domains. Thus, research on cognitive impairment in schizophrenia is not a recent phenomenon. However, the past 10 to 20 years have seen an increasing recognition of the central importance of cognition to understanding function and outcome in this illness [1], an awareness that has shifted the emphasis of at least some work on schizophrenia. More specifically, there has been a rapidly growing body of work on methods of enhancing cognition in schizophrenia as a means to potentially facilitate improved outcome and quality of life for individuals with this debilitating illness. This work has included major initiatives within the field designed to improve the measurement of cognition in schizophrenia during the conduct of clinical trials, such as the Measurement and Treatment Research to Improve Cognition in Schizophrenia program [2] and the Cognitive Neuroscience Treatment Research to Improve Cognition in Schizophrenia program [3]. Work on cognitive function in other disorders that can involve psychosis (eg, schizoaffective disorder, bipolar disorder, and psychotic major depression) has been in progress for many years, spurred in part by the early work on cognitive impairment in schizophrenia.
However, the enhanced emphasis on cognition as a constraint on functional capacity in schizophrenia has led to a growing number of studies inquiring about similarities and differences in the role that cognition may play across the nonaffective and affective psychoses. If cognitive impairment constrains functional capacity and outcome in schizophrenia, and if similar cognitive impairments are present in affective psychoses, then cognition may also be a critical determinant of functional status in these other illnesses. If so, then the work on the methods and mechanisms of cognitive enhancement in schizophrenia may have applicability to similar attempts to enhance cognition and functional capacity in affective psychoses. Thus, the goal of this article is to briefly overview the work on cognitive function in affective psychoses so as to understand where cognition may play a similar role in affective psychoses and where it may play a different role.
Are the Profile and Severity of Cognitive Impairment Similar in Schizophrenia and Affective Psychoses?
A first critical question to ask is whether the nature and/or severity of cognitive impairment found in affective psychoses is similar or different to that found in schizophrenia. If it is qualitatively different, this would argue for a fundamentally different role for cognition in affective psychoses. However, if the pattern or profile of cognitive impairment is similar across affective and nonaffective psychosis—even if the severity is different—then such a result would be consistent with the hypothesis that there are common dimensions of psychopathology across the affective and nonaffective psychoses [4••]. A growing number of studies and metaanalyses have been designed to answer this question, with somewhat mixed results. However, the apparent discrepancy across studies often may reflect more of an interpretation difference (glass half empty vs glass half full) rather than a true difference in the results of such comparative studies. Empiric and meta-analytic studies have shown fairly consistently that the degree of cognitive impairment in schizophrenia is worse than the degree of cognitive impairment in disorders such as bipolar I and psychotic major depression, with an effect size typically in the range of 0.3 to 0.5 [5-8]. The studies in this area have varied in the degree to which they have included actively ill versus euthymic patients and the degree to which samples have been well matched on demographic and clinical characteristics that can influence cognitive function. However, the effect sizes for the differences from schizophrenia are not dramatically larger if one focuses only on studies in remitted patients [8], although even remitted patients with bipolar disorder show clear cognitive impairments [9]. The literature on the comparison of schizoaffective disorders with schizophrenia also provides mixed evidence, with some studies finding little difference in the severity of cognitive impairments between these two disorders [10,11] but others finding evidence of worse impairment in schizophrenia [12].
Despite the evidence of a larger magnitude of cognitive impairment in schizophrenia compared with affective psychoses, the literature is much more consistent in suggesting that the profile of cognitive impairment is relatively similar across schizophrenia and affective psychoses. In other words, the relative severity of impairments across different cognitive domains tends to be very similar in bipolar disorder, psychotic major depression, and schizoaffective disorders compared with schizophrenia [5-7,11]. Perhaps one of the clearest examples of such a result was recently provided by Reichenberg and colleagues [13••]. These researchers used the Suffolk County Mental Health project cohort of consecutive first admissions with psychotic disorders to compare individuals with consensus research diagnoses of schizophrenia, schizoaffective disorder, major depressive disorder with affective features, and bipolar disorder with psychotic features. Overall, individuals with schizophrenia and schizoaffective disorder were more impaired than individuals with psychotic mood disorders, and the prevalence of cognitive impairment was higher in schizophrenia and schizoaffective disorder using all the definitions that they examined. However, as shown in Figure 1, the individuals within all four groups showed the same relative pattern of impairment across cognitive domains, with the greatest impairment in verbal memory and the least impairment in visual processing and general verbal ability. Depp et al. [5] provided another compelling example in their study comparing individuals with schizophrenia, bipolar disorder, and healthy controls. Unlike Reichenberg et al. [13••], Depp et al. [5] found that bipolar patients were as impaired as schizophrenia patients on many of the tests. Furthermore, the profile of impairment was very similar across groups, with the most impairment in information processing speed for both groups and the least impairment in crystallized IQ. In addition, evidence indicates that the factor structure of cognition is very similar across schizophrenia and bipolar disorder [14].
Figure 1.
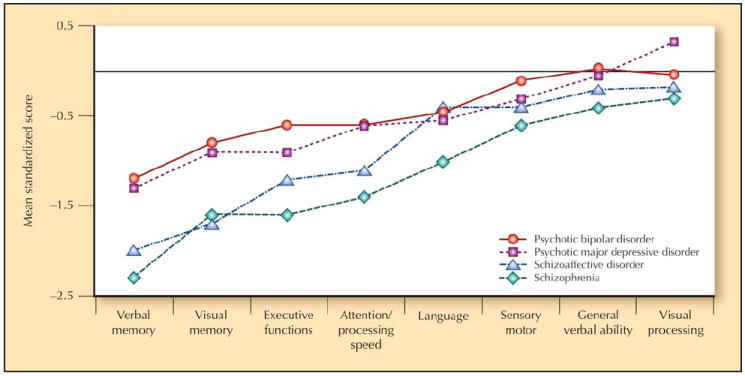
Neuropsychological performance profile of psychotic bipolar disorder, psychotic major depressive disorder, schizoaffective disorder, and schizophrenia patients (straight solid line indicates average normal performance). Raw data are available from the corresponding author.
In summary, the literature on the nature of cognitive dysfunction in schizophrenia and the affective psychoses suggests that although all the affective psychoses are associated with some level of cognitive impairment, it may be less severe for individuals with psychotic bipolar disorder and psychotic major depression. However, in at least some studies, the cognitive impairment in schizoaffective disorders is as severe as that seen in schizophrenia. The degree of cognitive impairment in affective psychoses may be influenced by whether an individual is currently in a psychotic episode. However, even individuals in a remitted state show significant cognitive impairments. Furthermore, and importantly from the perspective of understanding etiology, the profile or pattern of cognitive impairment across affective psychoses is very similar to that seen in schizophrenia. This finding is consistent with the idea that common mechanisms lead to cognitive dysfunction across the nonaffective and affective psychoses.
Are Cognitive Impairments More Stable in Schizophrenia Than in Affective Psychoses?
The field of schizophrenia research has grown to conceptualize cognitive deficits in schizophrenia as potentially reflecting endophenotypic markers of risk. According to Gottesman and Hanson [15], an endophenotype should be present whether or not the trait or disease is present if it is a vulnerability marker for the disorder. From the perspective of individuals with the disease, this criterion implies that cognitive dysfunction should be present before the onset of the illness, should be relatively stable (although it may be influenced by clinical exacerbation), and should not disappear when clinical symptoms remit. Consistent with this conceptualization of cognitive deficits, one of the key findings in research on cognition in schizophrenia is that cognitive impairment is clearly present even at the onset of illness (eg, in the first episode) and appears to be relatively stable over time [16-18]. Some studies have shown evidence for improvement in cognitive function over time or over the course of a clinical trial in the placebo condition. However, these improvements tend to be of a small effect size and may be accounted for by practice effects on the assessment instruments [19].
Individuals with affective psychoses can also display cognitive deficits during the first episode of their illness, often to the same level as that seen in individuals with first-episode schizophrenia [7,20-22]. Furthermore, very clear evidence indicates that cognitive deficits remain even during remission in individuals with affective psychoses [9,13••,23]. There is even some evidence for the stability of cognitive deficits in remitted individuals with bipolar disorder [24]. However, despite evidence of clear persistence of cognitive impairment during remission in affective psychoses, it is less clear whether cognitive function is more disrupted by the occurrence of an acute psychotic episode in affective psychoses than in individuals with schizophrenia. In cross-sectional work, the level of cognitive impairment has been determined to be similar in individuals with active mania and those in remission compared with controls [25]. However, there are also indications in the literature that cognition can vary as a function of episode status in affective psychoses. For example, first-episode patients with schizophrenia showed little evidence of improvement at 4-week followup despite a large degree of clinical improvement [21]. In contrast, individuals with psychotic major depression and psychotic bipolar disorder show more evidence of improvement in cognitive function with improvements in clinical symptoms [21]. However, the sample sizes in such longitudinal studies directly comparing affective and nonaffective psychoses have been small, and the range of cognitive functions assessed relatively narrow, leaving open the possibility that other domains of cognitive impairment are more stable.
Are Cognitive Deficits in Affective Psychoses Related to the Same Symptom Dimensions as Found in Schizophrenia?
Cognitive deficits in schizophrenia are clearly present at the onset of the illness and are relatively stable during acute episodes and relative remission. However, evidence also indicates that the severity of cognitive impairment in schizophrenia co-varies with the severity of certain dimensions of psychopathology. Specifically, there is strong evidence that the relative severity of positive symptoms in schizophrenia is not associated with cognitive impairment, but that the severity of negative and disorganization symptoms is consistently associated with the severity of impairment across a range of cognitive domains [26-28]. Furthermore, there is evidence that cognitive deficits are correlated with these same domains of psychopathology in schizoaffective disorder, but evidence is mixed in psychotic bipolar disorder [5]. However, studies of psychotic bipolar disorder and major depression do not always assess the same dimensions of psychopathology as studies of schizophrenia and schizoaffective disorders, making it difficult to compare psychopathological correlates of cognitive function across different disorders and studies.
Are Cognitive Deficits Present in the Unaffected Relatives of Individuals With Affective Psychoses as They Are in the Relatives of Individuals With Schizophrenia?
As described previously, the conceptualization of cognitive deficits as endophenotypic markers of vulnerability to schizophrenia suggests that they should be present in individuals at risk for the development of schizophrenia (eg, first-degree relatives) who do not yet have manifest illness. Many studies have demonstrated this to be true for the relatives of individuals with schizophrenia, with evidence for the existence of moderate to large effect size deficits in relatives across a range of cognitive domains [27,29,30]. Such deficits are present in the siblings of adolescents and adults with schizophrenia and in the children of individuals with schizophrenia [31,32].
Relatively few studies have been conducted on the relatives of individuals with schizoaffective disorder (separately from mixed groups of schizophrenia and schizoaffective disorder), although there is suggestive evidence of cognitive impairments in their first-degree relatives [33]. For bipolar disorder, the evidence is much more mixed. Several review articles have examined the nature and severity of cognitive impairment in the relatives of individuals with bipolar disorder [34,35]. Although several studies have found evidence for at least moderate impairments in cognitive function in the relatives of individuals with bipolar disorder, the results have been relatively variable compared with the literature on schizophrenia, and there were a number of null results [36]. However, one of the difficulties in interpreting this literature is that such relative studies have not necessarily distinguished between individuals with bipolar disorder who did and did not have psychotic symptoms. It is possible that studies focusing only on the relatives of individuals with psychotic bipolar disorder would find clearer evidence of cognitive impairment in relatives. For example, Bora et al. [37] found that the relatives of individuals with a history of psychotic bipolar disorder performed worse on measures of executive function than the relatives of individuals with nonpsychotic bipolar disorder. In contrast, Jabben and colleagues [36] found that a history of positive psychotic symptoms in bipolar patients was associated with better cognitive function in several domains in their relatives [36]. Thus, more work distinguishing between the relatives of individuals with bipolar disorder with and without psychotic features is needed to answer this question clearly.
Interestingly, all the studies that examined the offspring of individuals with bipolar disorder found evidence of cognitive impairment, although the domains examined varied across studies [35]. The current evidence suggests that bipolar disorder is highly heritable, potentially with an even stronger genetic influence than schizophrenia [38,39]. However, Cardno et al. [40] provide counterevidence. Thus, it is possible that studies of adult relatives with bipolar disorder at times may represent a relatively “unenriched” sample if the absence of a mood or psychotic disorder in the relative is a criterion for study entry. This issue may be less apparent in studies of children, as they have not yet passed through the period of risk. Thus, such studies may include high-risk individuals who will still go on to develop the disorder.
Do Cognitive Impairments Predict Functional Status and Outcome in Affective and Nonaffective Psychoses?
As described previously, one of the reasons for a resurgence of interest in cognitive function in schizophrenia is the growing evidence that cognitive impairment places an important constraint on functional status and functional outcome in this illness [1,41,42]. The relationship between cognitive function and functional status is present in cross-sectional studies, but there is also evidence that baseline cognitive function can predict functional outcome over longer periods of time in domains such as work and social behavior [42]. Many of these studies included patients with both schizophrenia and schizoaffective disorder, providing at least indirect evidence of a similar relationship between cognition and function in these disorders [43]. Importantly, growing evidence suggests that cognition predicts function in a similar way in affective psychoses [25]. For example, recent work by Tabares-Seisdedos et al. [44••] showed that baseline cognitive performance predicts functional outcome 1 year later in individuals with schizophrenia and those with bipolar disorder, with better baseline cognitive performance associated with better outcome. Furthermore, neurocognitive function in bipolar disorder can predict clinical recovery, with better cognitive function again associated with better function at follow-up [45] and some evidence for an association between better baseline cognitive function and faster recovery [20].
Another way in which to look at cognition predicting functional outcome in schizophrenia is the degree to which cognitive deficits in at-risk individuals predict the likelihood of those individuals developing manifest illness. For example, Niendam et al. [46] found that children who later developed schizophrenia and their unaffected siblings both showed performance deficits on selected subtests of the Wechsler Intelligence Scale for Children administered at age 7 years, but the future schizophrenia probands performed worse than siblings who never developed the illness. Similarly, genetic high-risk research has demonstrated that a severe deficit on an attentional task (Continuous Performance Test, Identical Pairs version) in childhood among the offspring of individuals with schizophrenia predicted the development of schizophrenia spectrum disorders in adulthood [47]. Thus, some evidence suggests that the severity of the cognitive deficits in childhood and adolescence in relatives of schizophrenia probands may be an indicator of psychotic outcome among these individuals. Few studies have addressed similar questions in individuals at risk for the development of affective psychoses. However, the existing evidence does not suggest that there are early indicators of cognitive impairment in children or adolescents who go on to develop affective psychoses [48]. Thus, although cognitive impairment may predict functional outcome similarly in adults with schizophrenia and affective psychoses, the developmentally predictive role of cognition may differ across affective and nonaffective psychoses.
Conclusions
At a broad level, the literature on cognitive function in ill individuals with affective and nonaffective psychoses suggests a picture of more similarity than dissimilarity overall, which has important implications for work on the pathophysiology and treatment of psychotic disorders. Although evidence clearly indicates that cognitive impairment can be greater in schizophrenia/schizoaffective disorder compared with psychotic bipolar or major depressive disorders, the similarity in the profiles of impairment suggests important common factors (as least final common pathway mechanisms) across psychotic disorders. Furthermore, there is growing evidence that cognitive impairment predicts functional outcome in affective and nonaffective psychoses and preliminary evidence for similarities in the relationships between symptom dimensions and cognitive function in at least schizophrenia and schizoaffective disorder.
On one level, such results are consistent with the hypothesis that common etiologic mechanisms contribute to psychosis and cognitive dysfunction across diagnostic boundaries. However, it is also possible that these similarities reflect commonalities in the proximal mechanisms that govern the common final pathways to cognitive impairment but that deficits in these proximal mechanisms may result from etiologically distinct distal mechanisms. This mechanistic question can be addressed in part by determining the degree to which the same neurobiologic deficits, at a functional or structural level, contribute to cognitive impairments across diagnostic boundaries. As of yet, the literature in this regard is limited, and there is evidence for similarities [49] and dissimilarities [50] in the neurobiology of nonaffective and affective psychoses.
Consistent with the idea that there may be different pathways to apparently similar patterns of cognitive impairment, the domains in which the nonaffective and affective psychosis may be more dissimilar relate to the role that cognitive dysfunction may play in vulnerability or risk for illness. Very consistent evidence indicates that cognitive deficits are present before the onset of illness in schizophrenia, even in unaffected relatives, and some evidence suggests that the severity of cognitive dysfunction in childhood may predict eventual development of schizophrenia (at least when compared with siblings who do not develop schizophrenia). In contrast, there is less robust evidence for impairments in unaffected relatives of individuals with psychotic bipolar disorder and major depression and little evidence as to whether cognitive deficits predict the development of psychotic mood disorders among those who may be at heightened risk for such disorders.
What is also clear from this selective review is that there are critical gaps in the literature that future research needs to fill. In particular, there is a relative dearth of studies that have examined multiple psychotic disorders using the exact same methods and approaches. Although there are some excellent examples of studies that have included multiple categories of psychotic disorders, in many cases, consumers of the literature must compare across studies using widely different assessment methods and experimental designs. The results of such studies including multiple diagnostic categories would greatly facilitate the evaluation of similarities and dissimilarities across disorders. This need is particularly strong in studies of at-risk populations, in which much more information is needed about the similarities and differences in the predictive utility of cognitive function as a risk factor for the development of affective psychotic disorders. In addition, the need for such comparative studies is also strong in work on the neurobiology of cognitive impairment across affective and nonaffective psychoses, as examining multiple levels of analysis may reveal differences in the underlying etiologic mechanisms that are not apparent from behavior alone. The need for such additional research does not lessen the importance of attending to the growing evidence for the importance of cognition in understanding functional status across diagnostic boundaries. It does provide a clear research agenda that will help to guide more empirically driven diagnostic boundaries.
Footnotes
Disclosure
No potential conflict of interest relevant to this article was reported.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as:
-
•
Of importance
-
••
Of major importance
- 1.Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull. 2000;26:119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- 2.Marder SR, Fenton W. Measurement and Treatment Research to Improve Cognition in Schizophrenia: NIMH MATRICS initiative to support the development of agents for improving cognition in schizophrenia. Schizophr Res. 2004;72:5–9. doi: 10.1016/j.schres.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 3.Carter CS, Barch DM. Cognitive neuroscience-based approaches to measuring and improving treatment effects on cognition in schizophrenia: the CNTRICS initiative. Schizophr Bull. 2007;33:1131–1137. doi: 10.1093/schbul/sbm081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4••.Craddock N, O’Donovan MC, Owen MJ. Psychosis genetics: modeling the relationship between schizophrenia, bipolar disorder, and mixed (or “schizoaffective”) psychoses. Schizophr Bull. 2009;35:482–490. doi: 10.1093/schbul/sbp020. This article reviews recent research focused on identifying specific genetic contributions to risk for schizophrenia and other psychotic disorders. Importantly, it also reviews the evidence of common genetic influences on risk across the boundaries of psychotic disorders. The authors argue that such research challenges our traditional diagnostic categories and call for a reconceptualization of how to create a psychiatric nosology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Depp CA, Moore DJ, Sitzer D, et al. Neurocognitive impairment in middle-aged and older adults with bipolar disorder: comparison to schizophrenia and normal comparison subjects. J Affect Disord. 2007;101:201–209. doi: 10.1016/j.jad.2006.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schretlen DJ, Cascella NG, Meyer SM, et al. Neuropsychological functioning in bipolar disorder and schizophrenia. Biol Psychiatry. 2007;62:179–186. doi: 10.1016/j.biopsych.2006.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hill SK, Keshavan MS, Thase ME, Sweeney JA. Neuropsychological dysfunction in antipsychotic-naive first-episode unipolar psychotic depression. Am J Psychiatry. 2004;161:996–1003. doi: 10.1176/appi.ajp.161.6.996. [DOI] [PubMed] [Google Scholar]
- 8.Krabbendam L, Arts B, van Os J, Aleman A. Cognitive functioning in patients with schizophrenia and bipolar disorder: a quantitative review. Schizophr Res. 2005;80:137–149. doi: 10.1016/j.schres.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 9.Bora E, Yucel M, Pantelis C. Cognitive endophenotypes of bipolar disorder: a meta-analysis of neuropsychological deficits in euthymic patients and their first-degree relatives. J Affect Disord. 2009;113:1–20. doi: 10.1016/j.jad.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 10.Gooding DC, Tallent KA. Spatial working memory performance in patients with schizoaffective psychosis versus schizophrenia: a tale of two disorders? Schizophr Res. 2002;53:209–218. doi: 10.1016/s0920-9964(01)00258-4. [DOI] [PubMed] [Google Scholar]
- 11.Smith MJ, Barch DM, Csernansky JG. Bridging the gap between schizophrenia and psychotic mood disorders: relating neurocognitive deficits to psychopathology. Schizophr Res. 2009;107:69–75. doi: 10.1016/j.schres.2008.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heinrichs RW, Ammari N, McDermid Vaz S, Miles AA. Are schizophrenia and schizoaffective disorder neuropsychologically distinguishable? Schizophr Res. 2008;99:149–154. doi: 10.1016/j.schres.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 13••.Reichenberg A, Harvey PD, Bowie CR, et al. Neuropsychological function and dysfunction in schizophrenia and psychotic affective disorders. Schizophr Bull. 2008 May 20; doi: 10.1093/schbul/sbn044. (Epub ahead of print). This study compared neuropsychological function across four diagnostic categories among individuals in the Suffolk County Mental Health first-episode psychosis study. The groups were individuals with a 2-year follow-up diagnosis of schizophrenia, schizoaffective disorder, psychotic bipolar disorder, and psychotic major depression. Those with schizophrenia and schizoaffective disorder showed similar levels of cognitive impairment that was more severe than the cognitive impairment found in psychotic bipolar and major depression, although the profile of cognitive impairment was very similar across the four disorders. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Czobor P, Jaeger J, Berns SM, et al. Neuropsychological symptom dimensions in bipolar disorder and schizophrenia. Bipolar Disord. 2007;9:71–92. doi: 10.1111/j.1399-5618.2007.00428.x. [DOI] [PubMed] [Google Scholar]
- 15.Gottesman II, Hanson DR. Human development: biological and genetic processes. Ann Rev Psychol. 2005;56:263–286. doi: 10.1146/annurev.psych.56.091103.070208. [DOI] [PubMed] [Google Scholar]
- 16.Rund BR. A review of longitudinal studies of cognitive functions in schizophrenia patients. Schizophr Bull. 1998;24:425–435. doi: 10.1093/oxfordjournals.schbul.a033337. [DOI] [PubMed] [Google Scholar]
- 17.Rodriguez-Sanchez JM, Perez-Iglesias R, Gonzalez-Blanch C, et al. 1-year follow-up study of cognitive function in first-episode non-affective psychosis. Schizophr Res. 2008;104:165–174. doi: 10.1016/j.schres.2008.05.020. [DOI] [PubMed] [Google Scholar]
- 18.Hill SK, Schuepbach D, Herbener ES, et al. Pretreatment and longitudinal studies of neuropsychological deficits in antipsychotic-naive patients with schizophrenia. Schizophr Res. 2004;68:49–63. doi: 10.1016/S0920-9964(03)00213-5. [DOI] [PubMed] [Google Scholar]
- 19.Szoke A, Trandafir A, Dupont ME, et al. Longitudinal studies of cognition in schizophrenia: meta-analysis. Br J Psychiatry. 2008;192:248–257. doi: 10.1192/bjp.bp.106.029009. [DOI] [PubMed] [Google Scholar]
- 20.Gruber SA, Rosso IM, Yurgelun-Todd D. Neuropsychological performance predicts clinical recovery in bipolar patients. J Affect Disord. 2008;105:253–260. doi: 10.1016/j.jad.2007.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barch DM, Carter CS, Cohen JD. Context processing deficit in schizophrenia: diagnostic specificity, 4-week course, and relationships to clinical symptoms. J Abnorm Psychol. 2003;112:132–143. [PubMed] [Google Scholar]
- 22.Albus M, Hubmann W, Wahlheim C, et al. Contrasts in neuropsychological test profile between patients with first episode schizophrenia and first-episode affective disorders. Acta Psychiatr Scand. 1996;94:87–93. doi: 10.1111/j.1600-0447.1996.tb09830.x. [DOI] [PubMed] [Google Scholar]
- 23.Robinson LJ, Thompson JM, Gallagher P, et al. A metaanalysis of cognitive deficits in euthymic patients with bipolar disorder. J Affect Disord. 2006;93:105–115. doi: 10.1016/j.jad.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 24.Mur M, Portella MJ, Martinez-Aran A, et al. Long-term stability of cognitive impairment in bipolar disorder: a 2-year follow-up study of lithium-treated euthymic bipolar patients. J Clin Psychiatry. 2008;69:712–719. [PubMed] [Google Scholar]
- 25.Martinez-Aran A, Vieta E, Reinares M, et al. Cognitive function across manic or hypomanic, depressed, and euthymic states in bipolar disorder. Am J Psychiatry. 2004;161:262–270. doi: 10.1176/appi.ajp.161.2.262. [DOI] [PubMed] [Google Scholar]
- 26.Pelletier M, Achim AM, Montoya A, et al. Cognitive and clinical moderators of recognition memory in schizophrenia: a meta-analysis. Schizophr Res. 2005;74:233–252. doi: 10.1016/j.schres.2004.08.017. [DOI] [PubMed] [Google Scholar]
- 27.Delawalla Z, Barch DM, Fisher Eastep JL, et al. Factors mediating cognitive deficits and psychopathology among siblings of individuals with schizophrenia. Schizophr Bull. 2006;32:525–537. doi: 10.1093/schbul/sbj082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nieuwenstein MR, Aleman A, de Haan EH. Relationship between symptom dimensions and neurocognitive functioning in schizophrenia: a meta-analysis of WCST and CPT studies. Wisconsin Card Sorting Test. Continuous Performance Test. J Psychiatr Res. 2001;35:119–125. doi: 10.1016/s0022-3956(01)00014-0. [DOI] [PubMed] [Google Scholar]
- 29.Snitz BE, Macdonald AW, 3rd, Carter CS. Cognitive deficits in unaffected first-degree relatives of schizophrenia patients: a meta-analytic review of putative endophenotypes. Schizophr Bull. 2006;32:179–194. doi: 10.1093/schbul/sbi048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fusar-Poli P, Perez J, Broome M, et al. Neurofunctional correlates of vulnerability to psychosis: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2007;31:465–484. doi: 10.1016/j.neubiorev.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 31.Hans SL, Marcus J, Nuechterlein KH, et al. Neurobehavioral deficits at adolescence in children at risk for schizophrenia: the Jerusalem Infant Development Study. Arch Gen Psychiatry. 1999;56:741–748. doi: 10.1001/archpsyc.56.8.741. [DOI] [PubMed] [Google Scholar]
- 32.Maziade M, Rouleau N, Gingras N, et al. Shared neurocognitive dysfunctions in young offspring at extreme risk for schizophrenia or bipolar disorder in eastern Quebec multigenerational families. Schizophr Bull. 2008 Jun 11; doi: 10.1093/schbul/sbn058. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bertisch H, Mesen-Fainardi A, Martin MV, et al. Neuropsychological performance as endophenotypes in extended schizophrenia families from the Central Valley of Costa Rica. Psychiatr Genet. 2009;19:45–52. doi: 10.1097/YPG.0b013e3283202816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Balanza-Martinez V, Rubio C, Selva-Vera G, et al. Neurocognitive endophenotypes (endophenocognitypes) from studies of relatives of bipolar disorder subjects: a systematic review. Neurosci Biobehav Rev. 2008;32:1426–1438. doi: 10.1016/j.neubiorev.2008.05.019. [DOI] [PubMed] [Google Scholar]
- 35.Robinson LJ, Ferrier IN. Evolution of cognitive impairment in bipolar disorder: a systematic review of cross-sectional evidence. Bipolar Disord. 2006;8:103–116. doi: 10.1111/j.1399-5618.2006.00277.x. [DOI] [PubMed] [Google Scholar]
- 36.Jabben N, Arts B, Krabbendam L, van Os J. Investigating the association between neurocognition and psychosis in bipolar disorder: further evidence for the overlap with schizophrenia. Bipolar Disord. 2009;11:166–177. doi: 10.1111/j.1399-5618.2009.00663.x. [DOI] [PubMed] [Google Scholar]
- 37.Bora E, Vahip S, Akdeniz F, et al. Executive and verbal working memory dysfunction in first-degree relatives of patients with bipolar disorder. Psychiatry Res. 2008;161:318–324. doi: 10.1016/j.psychres.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 38.Gottesman II. Schizophrenia Genesis: The Origins of Madness. New York: Freeman; 1991. [Google Scholar]
- 39.Bertelsen A. A Danish twin study of manic-depressive disorders. Prog Clin Biol Res. 1978;24A:119–124. [PubMed] [Google Scholar]
- 40.Cardno AG, Marshall EJ, Coid B, et al. Heritability estimates for psychotic disorders: the Maudsley twin psychosis series. Arch Gen Psychiatry. 1999;56:162–168. doi: 10.1001/archpsyc.56.2.162. [DOI] [PubMed] [Google Scholar]
- 41.Bowie CR, Leung WW, Reichenberg A, et al. Predicting schizophrenia patients’ real-world behavior with specific neuropsychological and functional capacity measures. Biol Psychiatry. 2008;63:505–511. doi: 10.1016/j.biopsych.2007.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Green MF, Kern RS, Heaton RK. Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr Res. 2004;72:41–51. doi: 10.1016/j.schres.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 43.Kurtz MM, Wexler BE, Fujimoto M, et al. Symptoms versus neurocognition as predictors of change in life skills in schizophrenia after outpatient rehabilitation. Schizophr Res. 2008;102:303–311. doi: 10.1016/j.schres.2008.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44••.Tabares-Seisdedos R, Balanza-Martinez V, Sanchez-Moreno J, et al. Neurocognitive and clinical predictors of functional outcome in patients with schizophrenia and bipolar I disorder at one-year follow-up. J Affect Disord. 2008;109:286–299. doi: 10.1016/j.jad.2007.12.234. These researchers examined cognitive function and functional status at baseline and at 1-year follow-up in individuals with schizophrenia and bipolar disorder. Importantly, the results suggested that baseline cognitive function in both schizophrenia and bipolar disorder predicted functional outcome 1 year later, although the exact cognitive predictors varied somewhat across the two disorders. [DOI] [PubMed] [Google Scholar]
- 45.Jaeger J, Berns S, Loftus S, et al. Neurocognitive test performance predicts functional recovery from acute exacerbation leading to hospitalization in bipolar disorder. Bipolar Disord. 2007;9:93–102. doi: 10.1111/j.1399-5618.2007.00427.x. [DOI] [PubMed] [Google Scholar]
- 46.Niendam TA, Bearden CE, Rosso IM, et al. A prospective study of childhood neurocognitive functioning in schizophrenic patients and their siblings. Am J Psychiatry. 2003;160:2060–2062. doi: 10.1176/appi.ajp.160.11.2060. [DOI] [PubMed] [Google Scholar]
- 47.Cornblatt B, Obuchowski M, Roberts S, et al. Cognitive and behavioral precursors of schizophrenia. Dev Psychopathol. 1999;11:487–508. doi: 10.1017/s0954579499002175. [DOI] [PubMed] [Google Scholar]
- 48.Cannon M, Moffitt TE, Caspi A, et al. Neuropsychological performance at the age of 13 years and adult schizophreniform disorder: prospective birth cohort study. Br J Psychiatry. 2006;189:463–464. doi: 10.1192/bjp.bp.105.020552. [DOI] [PubMed] [Google Scholar]
- 49.Morgan KD, Dazzan P, Orr KG, et al. Grey matter abnormalities in first-episode schizophrenia and affective psychosis. Br J Psychiatry Suppl. 2007;51:s111–s116. doi: 10.1192/bjp.191.51.s111. [DOI] [PubMed] [Google Scholar]
- 50.MacDonald A, Carter CS, Kerns JG, et al. Specificity of prefrontal dysfunction and context processing deficits to schizophrenia in a never medicated first-episode psychotic sample. Am J Psychiatry. 2005;162:475–484. doi: 10.1176/appi.ajp.162.3.475. [DOI] [PubMed] [Google Scholar]


