Fig. 1.
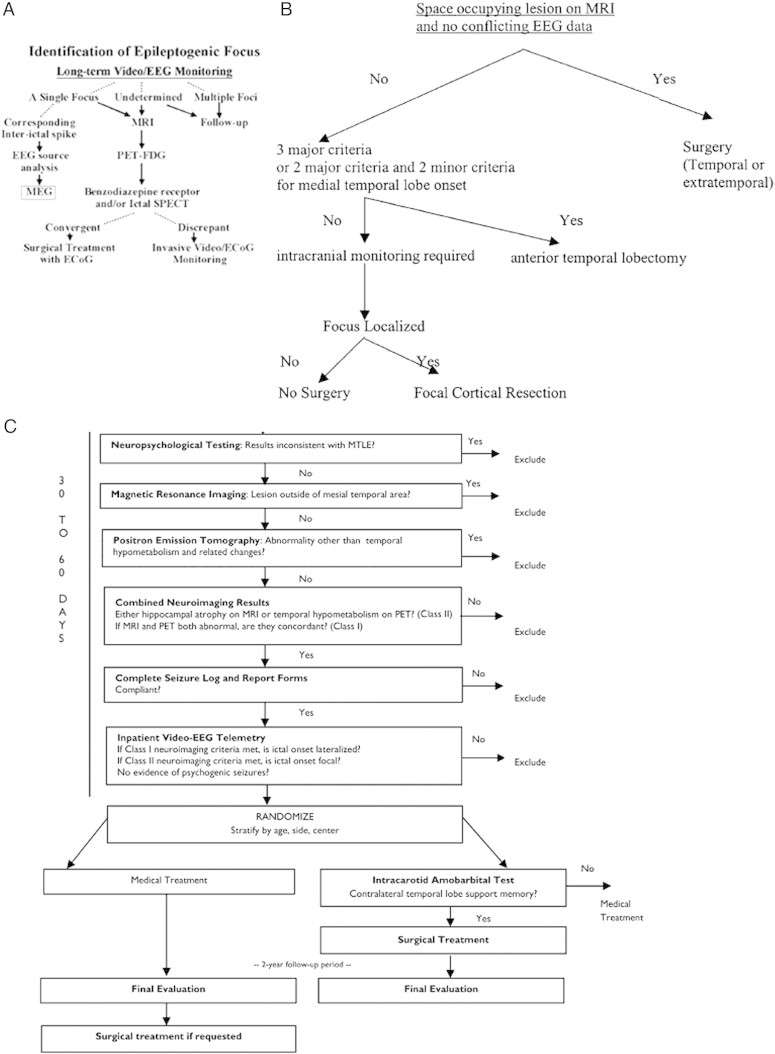
Flow charts indicating the decision making process in epilepsy presurgical evaluation.
A. Decision tree for source localization in Kyoto University Hospital (Shibasaki et al., 2007; courtesy of Dr. Shibasaki; reprinted with permission from Shibasaki et al., 2007). The branch after MEG analysis was in parallel with the main stream of evaluation (i.e., if the findings of EEG/ESI and MEG/MSI in focus localization are convergent, then perform surgery with ECoG; otherwise, perform invasive monitoring).
B. Decision tree for invasive monitoring across 7 epilepsy centers (Haut et al., 2002; courtesy of Dr. Haut; reprinted with permission from Haut et al., 2002).
Major and minor criteria supporting medial temporal lobe onset:
1. Major criteria:
(1) Interictal EEG: At least 70% of interictal discharges with a single anterior temporal field, in a sample of ≥ 50 discharges.
(2) Ictal EEG: Seizure with rhythmic theta or alpha discharge confined to one temporal lobe at least one third of seizures, with no conflicting data.
(3) MRI: Mesial temporal sclerosis.
2. Minor criteria:
(1) Interictal focal temporal EEG slowing present ≥ 50% of the time during wakefulness.
(2) PET: medial temporal hypometabolism (required if major criteria are 1 and 2).
(3) SPECT: temporal hypoperfusion.
(4) Wada test lateralized (percentage of items recalled after each injection differed by > 20%).
(5)Neuropsychological testing: medial temporal deficits present.
C. Multicenter ERSET protocol flow chart (Engel et al., 2010; courtesy of Dr. Engel; reprinted with permission from Engel et al., 2010).
