Abstract
Background
In Germany, the number of people with dementia living in nursing homes is rapidly increasing. Providing adequate care for their special needs is a challenge for institutions and their staff members. Because of the growing number of people with dementia, changes to the conceptual orientation of nursing homes have occurred. These changes include specialized living arrangements and psychosocial interventions recommended for people with dementia. Until now, the provision of dementia care and its association to the residents’ behavior and quality of life is not well investigated in Germany. The purpose of this study is to describe the provision of dementia care and to identify resident- as well as facility-related factors associated with residents behavior and quality of life.
Methods/Design
The DemenzMonitor study is designed as a longitudinal study that is repeated annually. Data will be derived from a convenience sample consisting of nursing homes across Germany. For the data collection, three questionnaires have been developed that measure information on the level of the nursing home, the living units, and the residents. Data collection will be performed by staff members from the nursing homes. The data collection procedure will be supervised by a study coordinator who is trained by the research team. Data analysis will be performed on each data level using appropriate techniques for descriptions and comparisons as well as longitudinal regression analysis.
Discussion
The DemenzMonitor is the first study in Germany that assesses how dementia care is provided in nursing homes with respect to living arrangements and recommended interventions. This study links the acquired data with residents’ outcome measurements, making it possible to evaluate different aspects and concepts of care.
Background
In Germany, up to 70% of care-dependent people with dementia live in nursing homes [1]. Over the last decade, care for people with dementia in nursing homes has changed [2-4]. Modern nursing homes provide a more home-like environment and more privacy for residents [5]. The former traditional medical model is being replaced by a more holistic and person-centered approach which aims at meeting residents' individual needs and enhancing their quality of life [4]. Two core aspects of dementia care concepts in nursing homes are living arrangements and dementia specific interventions.
For Germany, research-based guidelines for the care of people with dementia and challenging behavior in nursing homes are available since 2007 [6]. Several researchers developed the guideline based on a literature review and expert consensus. They recommend the creation of a dementia-friendly environment and architecture, possibilities for further education for nurses, and various forms of living arrangements for residents with dementia. For nursing care, recommendations include psychosocial interventions (validation, multisensory stimulation, reminiscence therapy, physical activities) as well as diagnostics and behavioral assessments. Although the guidelines are not compulsory, they can be considered as a document of high priority for nursing homes. In addition to addressing the residents’ behavior, the overall aim of the guideline is to improve residents' quality of life and well-being.
Today, German nursing homes differ with respect to living arrangements. Two forms exist: integrative and segregative. The principle of integration allows residents with and without dementia to live together; segregation includes several forms of specialized living arrangements exclusively for residents with dementia (e.g., Dementia Special Care Units [DSCU], small living units with home-like environment). Regarding dementia specific interventions, a great effort has been invested in developing, testing and implementing such interventions in Germany [7].
In the last decade, national as well as international studies evaluated the implementation and the effect of dementia specific living arrangements and interventions on resident’s behavior and quality of life.
Evaluation of living arrangements
The effect of DSCU residence on residents quality of life was investigated in a large survey study from the United States involving 390 nursing homes and 13,983 residents [8]. The results of this study indicated a positive relationship between quality of life and residence in a DSCU. Moreover, this study showed that facility characteristics play an important role in resident perception of quality of life [8]. A study from Spain [9] showed contradictory results: the staff rated residents’ quality of life on DSCU’s lower than of residents living in a regular unit. For Germany, no study exists that applied a quality of life measurement. The only study that evaluates DSCU’s in Germany investigated indicators for quality of life such as social contacts and activities [10]. They found benefits to living in a DSCU compared to traditional units. Concerning challenging behavior, the study did not show a beneficial effect of DSCU placement, a result that is confirmed by the latest Cochrane Review [11].
Regarding small-scale living arrangements a German study did not show a clear effect on residents quality of life or on behavioral problems [12]. Studies from the Netherlands and Belgium reported the same findings [13,14].
Conclusions drawn from these studies suggest that the implementation of best practices may be more important than providing a specialized environment [11] and that future research should focus more on the quality and content of care than on the scale or specialization for the evaluation of quality of life [14].
Evaluation of quality of care
Concerning the implementation of guidelines for psychosocial interventions in dementia care, a comparison of seven European guidelines, including the German version, showed weaknesses in their applicability [15]. The latest review on nonpharmacological interventions concluded that the feasibility of the investigated interventions is limited because of resource requirements [16]. Recently, a set of 12 quality indicators for psychosocial care in dementia in nursing homes was developed as part of the European Collaboration on Dementia project (EuroCoDe), which was initiated by Alzheimer Europe [17]. The results from the first application draw a different picture than what may was suspected. They indicate that the majority of residents receive psychosocial interventions tailored to the person’s needs and abilities (this was found for 50% of residents with dementia in Dutch nursing homes and 97% in Spanish nursing homes), that the residents documented care plan included different forms of activity (100% of the Dutch sample and 21% of the Spanish sample) and that – at least in the Netherlands – 75% of the residents with dementia and behavioral problems are treated with a psychosocial intervention first [17]. But these results have to be interpreted cautiously taking the limitations into account: the discriminatory capacity is not yet assessed and the assessment of the indicators relies on documentation only [17].
There are few studies reporting on the quality of care in specialized units compared to traditional units. Studies have investigated differences in care processes in dementia special care units compared to traditional units [10,18,19], but these studies mainly focused on clinical process measures (e.g., feeding tube use, physical restraint use, psychotropic medication use, and incontinence care) whereas the use of dementia specific interventions remains unclear. Only Weyerer et al. [10] report more participation in physical activities, activities in and outside the nursing home, memory training and biography-oriented groups/individual sessions for DSCU’s compared to traditional units.
In summary, a large amount of research has been conducted to evaluate current approaches to dementia care in nursing homes. But still a knowledge gap exists regarding details of how dementia care is provided in practice, which type of interventions are in use, how these interventions are related to existing institutional resources and resident characteristics and how facility characteristics, such as size, ownership type, staffing levels and the provision of dementia specific interventions influence resident’s behavior and quality of life [20-25].
Explorative knowledge about the provision of institutional care for people with dementia and the factors that are associated with quality of life and behavior is necessary for future intervention research and the further development of quality indicators to base policy decisions on sound scientific evidence.
Aims and research questions of the study
We have designed a longitudinal study called the “DemenzMonitor”. The overarching aim of the study is to identify resident- and facility-related factors and covariates that are associated with
a) the residents behavior and
b) the residents quality of life.
To reach this aim, the following research questions will be answered:
1. How is dementia care provided in German nursing homes? Which living arrangements are in use? Which recommended interventions are in use? Who gets which interventions?
We assume that there will be differences with respect to the care provided between segregative and integrative living units, as well as small- and large-scale units. Therefore, we will investigate these as fixed groups. Based on certain other key variables (ownership, costs, special reimbursements, staff) we aim to build further possible groups with similar characteristics.
2. Are there any differences between the groups regarding the resident’s demographic data, cognition, care dependency? Are there any differences between the groups regarding the interventions provided?
For the whole population as well as for the groups we seek to answer this question:
3. Which of the investigated variables are associated with the resident’s outcomes behavior and quality of life when controlling for resident-related covariates such as age, sex, length of stay? Are there differences between the results of the whole population and the groups?
Since the study provides longitudinal data, we will also be able to answer the questions:
4. Are the resident’s outcomes behavior and quality of life stable over time or are they changing? If they change, are there differences in associated factors and covariates between the two points of time so that time needs to be considered as an influencing factor? Which factors are associated with the change of the resident’s outcomes?
Based on these results, hypothesis on influencing factors of resident’s behavior and quality of life will be generated.
Methods
Design
The DemenzMonitor is intended to be an ongoing observational descriptive longitudinal study to be repeated every year.
Study population and recruitment
Nursing homes across Germany are invited to participate in the study. In 2011, more than 12,000 nursing homes existed in Germany [26]. Because it is not feasible to contact every institution, the study will be published in high-circulation professional journals, newsletters, and the websites of nursing and geriatric information services. It will also be presented at national nursing conferences. It is assumed that the motivation of nursing homes to participate will be strongly driven by the benefits they will receive from the study. Therefore, the participating institutions will receive an individual report with living-unit- and resident-related results. The template for this report was developed together with institutions from the pilot study to ensure practicability (see “Dissemination of study results to the participating institutions”).
Accurate data collection requires a considerable amount of time and motivation by participating institutions and their employees; therefore, participation is voluntary. If an institution chooses to participate, it is that institution’s responsibility to determine how many living units will be involved. If informed consent is given, we propose a whole-population survey of the participating living units. The goal is to involve the institutions for as long as possible to gather longitudinal data. However, because participation is voluntary, the institutions will decide how long they will participate and how many data collections will be performed. It is assumed that a number of institutions will decline to participate repeatedly. Therefore, new institutions will be recruited and involved each year.
After each data collection cycle, recruitment rates for the proportion of participating institutions in every federal state will be calculated to get an idea of representativeness.
Conceptual framework
The study is based on a self-developed conceptual framework that guided its design, development, and the selection of the range of potential determinants of residents’ outcomes. The framework is based on the concept of multi-level social epidemiology frameworks [27]. These frameworks arose from a critical discussion about the limitations of epidemiology’s dominant causal models and views. In this paradigm, causality is assumed to be linear with proximate, individual risk factors, whereas social epidemiology frameworks account for the joint and dynamic influence of social, environmental, and biological factors that affect health [28]. “Eco-epidemiology”, a framework proposed by Mervyn Susser in 1996 [29], encompasses multiple interactive systems at different levels. Eco-epidemiology is grounded in the principle of ecologism, which seeks to understand phenomena in relation to the boundaries of context rather than seeking universal explanations that may be context-free [30].
The framework developed for the study refers to the work of Lawton and Nahemow [31,32], which focuses on behavior and quality of life. The central thesis of this work is that competencies of the individual, the environment, and the interaction of the individual with the environment influence human behavior and quality of life. According to ecological frameworks, the DemenzMonitor framework relies on two dimensions to clarify the complexity of social realities: environment- and person-focused dimensions. The environment-focused dimension comprises physical and social environments. The person-focused dimension includes demographics, function, and dementia-specific characteristics such as cognition, behavior, and quality of life. Figure 1 shows the conceptual framework.
Figure 1.
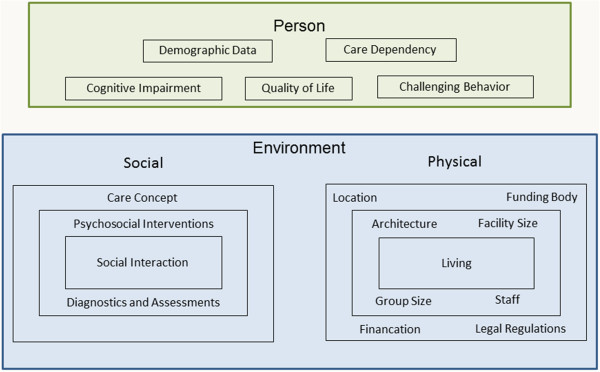
Conceptual framework of the study.
Instrument development
To assess the different dimensions, it was necessary to develop a new instrument that covers three levels: the level of the institution, the living units, and the residents.
Based on the conceptual framework, we conducted a literature search to identify existing instruments or measurements that are suitable to assess the different aspects of the dimensions. This search identified instruments for person-related aspects (care dependency, cognitive impairment, challenging behavior, quality of life). As we did not find any suitable instruments relating to the aspects of the social and physical environment dimension, new items had to be developed. The development of these items was conceptually based on the German guidelines for the care of people with dementia and challenging behavior in nursing homes [6]. Additionally, we conducted a systematic literature review on the development, implementation and use of this interventions in the practice [7]. Focus groups and quantitative expert ratings were also conducted to achieve content and face validity [33,34]. A multi-method pretest with intended users revealed problems with comprehensibility and practicability [35,36].
Each step of the instrument development and testing followed a revision of the instrument. The developed instrument was applied in a pilot study in May 2012.
Questionnaires
The new instrument contains three questionnaires divided into several sections. An overview of the sections for every questionnaire provides Table 1.
Table 1.
Overview of the questionnaires
| |
Items on each level |
||
|---|---|---|---|
| Section | Institution | Living unit | Resident |
| General characteristics |
37 |
4 |
17 |
| Staff characteristics |
27 |
42 |
/ |
| Characteristics of living environment |
6 |
19 |
3 |
| Living and care concept |
31 |
14 |
/ |
| Provision of dementia care |
/ |
38 |
80 |
| Care dependency (PSMS) |
/ |
/ |
6 |
| Challenging behaviour (NPI-Q) |
/ |
/ |
24 |
| Dementia (Diagnosis) |
/ |
/ |
1 |
| Dementia (FAST) |
/ |
/ |
16 |
| Dementia (DSS) |
/ |
/ |
7 |
| Quality of Life (Qualidem) |
/ |
/ |
40 |
| Total | 101 | 117 | 194 |
At both the nursing home and living unit levels, the questionnaires focus on environmental aspects (e.g., general and staff characteristics, characteristics of the living environment, living and care concepts). The provision of care is operationalized at the level of the living unit and the residents. Additionally, several assessment instruments are included in the residents’ questionnaire, as explained below.
Tables 2, 3 and 4 provide an overview of the questionnaires. The questionnaires can be obtained on request.
Table 2.
Measurements on nursing home level
| Nursing Homes [NH] - assessed by nursing home mangers | |||
|---|---|---|---|
|
Conceptual domain |
Operational definition |
Number of items |
Empirical measure |
| General characteristics |
Funding body |
1 |
3-response option |
| Locality measured in inhabitants |
1 |
4-response option |
|
| Location (federal state) |
1 |
16-response option |
|
| Number of beds in long term care / respite care / day care / night care / residential care |
5 |
Free-text |
|
| Number of residents per care level |
5 |
Free-text |
|
| Number of residents per care level with substantial additional care needs according to Long Term Care Insurance |
5 |
Free-text |
|
| Costs for care per care level / accommodation & expenditure (single/double room) |
9 |
Free-text |
|
| Existence of a segregative living unit (SLU) with additional costs |
1 |
Yes/No |
|
| Costs for the SLU for care per care level / accommodation & expenditure (single/double room) |
9 |
Free-text |
|
| Staff characteristics |
Staff divided in subgroups (administrative staff / registered nurses / nursing assistants / nursing students / additional care staff / facilitating services) |
13 |
Fulltime equivalent (planned) |
| Number of volunteers |
1 |
Free-text |
|
| Number of engaged clinical nurse specialists for Psychogeriatrics / Psychiatry / Palliative care / Dementia Care Mapping (Basic User) / multisensory stimulation / validation therapy / other dementia-related trainings |
7 |
Free-text |
|
| Training of at least half of all nurses employed in case conferences / behavioral cognition assessments / validation therapy / reminiscence therapy / multisensory stimulation / physical activity |
6 |
Yes/No |
|
| Characteristics of living environment |
Year of nursing home (NH) foundation |
1 |
Free-text |
| Time span since last modernization |
1 |
6-response option |
|
| Number of living units |
1 |
Free-text |
|
| Number of single / double / multi-shared rooms |
3 |
Free-text |
|
| Living and care concept | Solely specialized for dementia |
1 |
Yes/No |
| Type of living arrangement (integrative/segregative) |
1 |
2-response option |
|
| Number of segregative living units (SLU) |
1 |
Free-text |
|
| SLU for residents with very severe dementia |
1 |
Yes/No |
|
| Care is based on a written dementia-specific concept |
1 |
Yes/No |
|
| * Concept basis (Person centered care [Tom Kitwood] / Psycho-Biography [Erwin Böhm] / Validation concept [Naomi Feil, Nicole Richard, Cora van der Kooij] / Milieu therapy / Normalization principles / None of these approaches) |
7 |
Yes/ No |
|
| * Characteristics of institutional dementia-specific concept (nurses/assistants are always working on the same LU / engagement of additional staff for daily activities / small scale living [max. 15 residents] / standard for admission procedures / structuring of daily activities / flexible mealtimes / night times / personal hygiene / active involvement of relatives) |
12 |
Choose a maximum of 3 |
|
| * Nursing interventions as part of the dementia-specific concept (case conferences / behavioral and cognition assessments / validation therapy / reminiscence therapy / multisensory stimulation / physical activity / others) | 7 | Yes/No | |
* conditional answer depending on previous answer.
Table 3.
Measurements on living unit level
| Unit level (Living Units [LU] – assessed by head nurses) | |||
|---|---|---|---|
|
Conceptual domain |
Operational definition |
Number of items |
Empirical measure |
| General characteristics |
Number of beds in long term care / respite care |
2 |
Free-text |
| Number of residents at day of data collection in long term care / respite care |
2 |
Free-text |
|
| Staff characteristics |
Staff divided in subgroups working on the ward at certain times (4) (registered nurses (RN) / nursing assistants (NA) / nursing students / additional care staff / facilitating services) |
36 |
Free-text |
| RN and NA are constantly allocated to the unit |
1 |
Yes/No |
|
| Service workers are constantly allocated to the unit |
1 |
Yes/No |
|
| Continuous presence of a RN during day shift |
1 |
Yes/No |
|
| Qualification of the head nurse of the unit (Psychogeriatrics / Psychiatry / Palliative care) |
3 |
3-response option |
|
| Characteristics of living environment |
Number of single / double / multi-shared rooms |
3 |
Free-text |
| Dementia specific architecture |
1 |
Yes/No |
|
| Time span since last modernization |
1 |
6-response option |
|
| Permission of residents to bring own furniture |
1 |
Yes/No |
|
| Furnishing of public rooms (more functional / functional and individual / more individual) |
1 |
3-response option |
|
| Permission to bring a pet |
1 |
Yes/No |
|
| Possibility to have contact with animals |
1 |
Yes/No |
|
| Accessible (safe-guarded) outdoor area |
1 |
Yes/No |
|
| Preparation of meals in the living-unit |
1 |
Yes/No |
|
| * Preparation of breakfast / lunch / coffee & tea / dinner / snacks |
5 |
Yes/No |
|
| Meal serving system (tablet / served by staff / buffet / home-like) |
3 |
Yes/No |
|
| Living and Care Concept |
Living arrangement (integrative/segregative) |
1 |
2-response option |
| Structural segregation |
1 |
Yes/No |
|
| Exit control |
1 |
Yes/No |
|
| Special refinancation of segregative living unit (SLU) |
1 |
Yes/No |
|
| * Scope of refinanciation (staff / concept / structure / others) |
4 |
Yes/No |
|
| * Criteria for admission to SLU (diagnosis of dementia / care level / dementia severity / challenging behaviour / mobility / others) |
6 |
Yes/No |
|
| Provision of dementiacare | Performance of case conferences (CC) |
1 |
Yes/No |
| * Characteristics of CC: CC are following a structured procedure / CC are conducted multidisciplinary / an external moderator is involved if needed / invitation of residents / relatives / results are recorded / results are evaluated / during CC’s staff has no other duties |
7 |
Yes/No |
|
| * Occupational groups invited to CC (residents / relatives / legal guardian / head nurse / nurses / additional care staff / physicians / therapists / others) |
9 |
Yes/No |
|
| * Time schedule of CC |
1 |
3-response option |
|
| * Location of case conference (conference room / nurses office / staff recreation room) |
1 |
3-response option |
|
| * Frequency of disruptions of CC due to work demands on the living unit |
1 |
4-response option |
|
| Snoezelen equipment on the living unit |
1 |
Yes/No |
|
| Performance of physical activities (PA): duration |
8 |
Free-text |
|
| Performance of PA: frequency |
8 |
3-response option |
|
| PA for residents with mobility restrictions | 1 | Yes/No | |
* Conditional answer depending on previous answer.
Table 4.
Measurements on the resident level
| Resident level (assessed by nurses) | |||
|---|---|---|---|
|
Conceptual domain |
Operational definition |
Number of items |
Empirical measure |
| General Characteristics |
Gender |
1 |
Female/Male |
| Date of birth |
1 |
Date |
|
| Place of residence before NH admission |
1 |
5-response option |
|
| Date of entry into nursing home and write NH |
1 |
Date |
|
| Legal guardian |
1 |
4-response option |
|
| Court order for admission |
1 |
Yes/No |
|
| Court order for physical restraints |
1 |
Yes/No |
|
| Care level according to Long Term Care Insurance (LTCI) |
1 |
5-response option |
|
| Substantial additional care needs according to LTCI § 87b |
1 |
3-response option |
|
| Visitors |
1 |
Yes/No |
|
| * Frequency of visits (spouse / other relatives / friends-neighbors / legal guardian / volunteers / other residents / others) |
7 |
4 point-Likert-Scale |
|
| Characteristics of Living Environment |
Residents room (single / double / multi-shared rooms) |
1 |
3-response option |
| Individual furniture in residents room |
1 |
Yes/No |
|
| Resident brought a pet to the NH |
1 |
Yes/No |
|
| Provision of Dementia Care |
Case conference (CC) after admission |
1 |
Yes/No |
| * Date of last CC |
1 |
Date |
|
| * Participants of last CC (resident / relatives / legal guardian / head nurse / ward nurses / other care staff / physicians / therapeutic staff / facilitating service / external moderators / others) |
11 |
Yes/No |
|
| * Reason for conducting last CC (due to an acute occasion / due to the routines) |
1 |
2-response option |
|
| * Content of last CC (nutrition / continence problems / risk of falls-actual falls / chronic wound / physical restraints / acute health problems / pain / cognition based problems / challenging behavior / psychosocial situation / quality of life - well-being / needs of the resident and relatives / admission to NH / hospital stay / others) |
15 |
Yes/No |
|
| Assessment of pain |
1 |
Yes/No |
|
| * Instrument used for pain assessment |
1 |
11-response option |
|
| * Date of pain assessment |
1 |
Date |
|
| Assessment of behavior |
1 |
Yes/No |
|
| * Instrument used for behavioral assessment |
1 |
6-response option |
|
| * Date of behavioral assessment |
1 |
Date |
|
| Assessment of dementia severity |
1 |
Yes/No |
|
| * Instrument used for dementia severity assessment |
1 |
10-response option |
|
| MMSE-Score (if available) |
1 |
Free-text |
|
| * Date of MMSE |
1 |
Date |
|
| Assessment of quality of life |
1 |
Yes/No |
|
| * Instrument used for quality of life assessment |
1 |
6-response option |
|
| * Date of quality of life assessment |
1 |
Date |
|
| Assessment of depression |
1 |
Yes/No |
|
| * Instrument used for depression assessment |
1 |
3-response option |
|
| * Date of depression assessment |
1 |
Date |
|
| Participation in Dementia Care Mapping |
1 |
Yes/No/Unknown |
|
| *Date of last Dementia Care Mapping |
1 |
Date |
|
| Assessment of biography |
1 |
Yes/No |
|
| * Amendment of biography assessment after initial assessment |
1 |
Yes/No/Unknown |
|
| Provision of multisensory stimulation (aroma therapy / music therapy / massage / listening to music / Basale Stimulation© / Snoezelen / cuddling pets / using touch materials / others / none) |
10 |
Yes/No |
|
| Provision of validation therapy |
1 |
Yes/No |
|
| * Kind of validation therapy (use in daily conversation / in personal communications / in group therapy / as a crisis intervention) |
4 |
Yes/No |
|
| Frequency of being in the open air during the last week |
1 |
5 point-Likert-Scale |
|
| Participation on physical activities (PA) (gymnastics / dance / games / walk outside / physiotherapy / others / none) |
1 |
Yes/No |
|
| * Kind of PA (gymnastics / dance / games / walk outside / physiotherapy / others) |
10 |
Yes/No |
|
| Incidence of acute psychiatric crisis in the last 6 months |
1 |
Yes/No/Unknown |
|
| * Frequency of acute psychiatric crisis in the last 6 months |
1 |
4 point-Likert-Scale |
|
| Continuous attendance by a General Practitioner |
1 |
Yes/No |
|
| Continuous attendance by a neurologist/psychiatrist |
1 |
Yes/No |
|
| Care Dependency |
Physical Self Maintenance Scale (PSMS) [55] |
6 |
5 point-Likert- Scale |
| Behavior |
Neuropsychiatric Inventory (NPI-Q) [48] |
12 |
3 point-Likert-Scale |
| Dementia |
Medical diagnosis of dementia |
1 |
Yes/No/Unknown |
| Functional Assessment Staging (FAST) [51] |
16 |
7 stages |
|
| Dementia Screening Scale (DSS) [53] |
7 |
3 point-Likert-Scale |
|
| Quality of Life | Qualidem [41] | 40 | 4 point-Likert-Scale |
* Conditional answer depending on previous answer.
Assessments
The residents’ questionnaire includes five assessments described in detail below. All assessments used are proxy-rating instruments and administered by the professional caregiver who is most familiar with the respective residents.
Quality of life
Quality of life is a complex and multidimensional concept that is influenced by both individual and environmental factors [37,38]. Moreover, the definition of quality of life involves a subjective component. For this reason, self-reports are considered the gold standard [39,40]. However, communication, memory, and cognitive impairments hamper the evaluation of self-reported quality of life in people with dementia, and the reliability and validity of self-reported quality of life is questioned in the literature [41]. Therefore, specific proxy-rating instruments for people with dementia have been developed. For this study, the quality of life assessment will be conducted using the Qualidem questionnaire, which has been specifically designed and validated [42] for institutionalized residents with dementia over the age of 65 years who suffer from mild to severe dementia. It is available in German and shows satisfactory psychometric properties in the German translation [43,44]. Qualidem assesses nine domains of quality of life, including 37 indicative and contraindicative items with four possible responses (i.e., never, rarely, sometimes, and frequently). Responses to these items determine the subscales: care relationship, positive affect, negative affect, restless or tense behavior, positive self-image, social relations, social isolation, feeling at home, and something to do. In the case of severe dementia (Global Deterioration Scale 7), six subscales can be applied using 18 of the 37 items [45]. To ensure reliability, Qualidem should be administered by two professional caregivers [42]. For this study, the institutions were informed of and requested to follow this recommendation.
Challenging behavior
Challenging behavior is also a complex and multidimensional construct [46]. In general, behaviors ranging from aggressive to apathetic are distinguished [6]. Several instruments exist to assess challenging behavior in residents with dementia. The Neuropsychiatric Inventory (NPI-NH) is a widely used instrument to measure neuropsychiatric behavior in dementia research [47]. It comprises 12 domains: delusion, hallucination, depression, anxiety, euphoria, aggression, apathy, disinhibition, irritability, aberrant motor behavior, sleep problems, and eating disorders. For this study, the simplified clinical form of the NPI, the NPI-Q [48], is used. It reports two scores for each domain: the presence of behavior and the severity of behavior on a 0–3 scale (0 = none, 1 = mild, 2 = moderate, 3 = severe). The calculations use either the severity score for each domain or the total score, which ranges from 0 to 36. The clinical form of the NPI was chosen for feasibility reasons.
Dementia diagnosis
Data on diagnosis of dementia are obtained from nursing home records.
Cognitive impairment
There are several ways to assess cognitive impairment in study participants [49]. A common tool for assessing cognitive function is the Mini Mental Status Examination (MMSE) [50]. For practical reasons, a MMSE cannot be performed for this study. However, in several nursing homes, a MMSE is performed regularly as a standard procedure. Therefore, we assess whether a MMSE value is available for a resident and, if so, when the MMSE was conducted. To gather more information about the cognitive status of residents, two other assessment instruments are part of the DemenzMonitor questionnaire. As a staging scale, the Functional Assessment Staging (FAST) [51] will be applied. Additionally, a new dementia screening instrument is included, the Dementia Screening Scale (DSS) [52,53].
The FAST allows the evaluation of changes in functional performance throughout the entire course of Alzheimer’s disease. It assesses functional capabilities including activities of daily living (ADL) as well as instrumental activities of daily living (IADL). The FAST scale includes seven major functional levels (1–7) operationalized by 16 items that are concordant with the corresponding global level of cognition and functional capacity of the Global Deterioration Scale [54]. The results of psychometric testing indicate that the FAST is a valid and reliable instrument for evaluating functional deterioration in people with Alzheimer’s disease.
The DSS was developed in German, shows satisfactory psychometric properties, and can differentiate among residents with severe dementia [53]. It was chosen because it is a simple and economic screening instrument that can be applied by nurses and is feasible for screening a large number of residents. Furthermore, it allows comparisons with results from national studies. The instrument comprises a series of seven items and includes two domains of cognitive functioning: memory and orientation. Items are rated on a 0–2 scale (0 = always, 1 = sometimes, 2 = never). The total score ranges from 0 to 14; a higher score indicates stronger impairment.
Functional status
To indicate the functional status of the residents, the Physical Self-Maintenance Scale (PSMS) [55] was chosen. The PSMS assesses self-maintaining and instrumental activities of daily living, such as (in)continence, requiring assistance with feeding, getting dressed, personal hygiene, mobility, and bathing. The items are rated on a 1–5 scale, with more points indicating greater dependency. The PSMS is a valid and reliable measure [55] and is recommended on the basis of an expert consensus [56].
Ethical considerations
The health care staff will collect data from residents. Therefore, written informed consent must be secured. The residents or their registered legal representatives must be informed of the purpose of the study and the conditions of participation. In terms of data security the residents’ identity will be kept confidential by using a pseudonym (code) for the questionnaires. The code list with the names of the residents will be stored in the nursing homes. The researchers are not going to have access to the list.
The ethics committee of the German society of Nursing Science approved the study.
Procedure for data collection
Every participating institution must designate a study coordinator to be the contact person for the researchers. The study coordinator is responsible for the entire data collection process, which includes informing and educating all persons involved in the study (nurses and residents), selecting the persons who will collect the data, briefing and supporting these persons, codifying the living units and residents, and disseminating the results within the institution. The research team will prepare the study coordinators for this task. The coordinators will be trained during a one-day lecture on the data collection procedures that focuses particularly on the questionnaires. Furthermore, the research team will provide the coordinators with all necessary material, including brochures and letters.
If a study coordinator leaves the institution but the institution continues to participate, a new study coordinator will be designated and trained.
The data collection will be conducted within a fixed time period of one month. Individual institutions will decide when to collect the data during this period.
Data entry, coding, cleaning, and storage
There are two ways of entering the data: online or paper-pencil. Secured online data collection will be conducted using the web tool LimeSurvey and the research center’s own server. Both data sets will be merged into a self-developed database and processed offline.
The study coordinators will code the residents’ questionnaires. To generate an individual code they will use constant items related to the resident (i.e., number of the nursing home and living unit, sex, date of birth, and first and last letter of the family name). Correct coding is important when collecting longitudinal data; therefore, we developed a technique that enables us to correct the code if necessary. With the help of stable items (e.g., date of entry), a matching method will indicate highly similar cases. This process is able to detect typing errors or mistakes in the coding such that manual error handling is possible. A detailed description of this technique is described elsewhere [57].
Data will be checked for missing items, plausibility, and the observance of determined time periods required to correctly complete the assessment instruments. Missing items will be imputed where appropriate. Inconsistent items will be removed.
For longitudinal analysis data sets will be checked for drop outs. Missing data due to drop-outs of the nursing home or death of the resident will not further be considered in the longitudinal analysis.
Data will be saved in a demilitarized zone of the research center for ten years. The paper-and-pencil questionnaires will be scanned and saved in the same manner.
Data analysis
Since the nature of the study is explorative, predominantly data mining techniques such as visualization of data, classifications of data, association and regression analysis will be applied. To answer the first research question, frequency analysis will be computed for the data from the whole study population. An appropriate classification technique (e.g. cluster analysis) will be conducted to identify possible groups. To answer the second research question descriptive statistics will be applied. Performing association and regression analysis will answer the third and fourth research question. To account for the nested structure of data due to different levels of data and time points, mixed effects generalized linear models will be used.
Dissemination of study results to the participating institutions
The research team will fed back the residents results for practical use. Therefore, a self-developed Access© database will automatically generate a report for every participating institution. This report will contain the results of the assessments for each resident as well as aggregated resident results for every living unit. For each resident, the report will display results of the DSS, NPI-Q, PSMS and Qualidem graphically. Table 5 displays the reported indicators on the living unit level. The report will also contain the average results for the whole sample as a benchmark for every indicator. The indicators will be for practical use only and will not be validated for scientific use at the time of their dissemination.
Table 5.
Indicators included in feedback reports
| Numerator | Denominatora |
|---|---|
|
Assessment |
|
| 1. Number of residents who are assessed for pain during the last 4 weeks / 3 months / > 3 months |
Total number of residents |
| 2. Number of residents who are assessed for behavior during the last 4 weeks / 3 months / > 3 months |
Total number of residents |
| 3. Number of residents who are assessed for dementia severity |
Number of residents with a medical diagnosis of dementia |
| 4. Number of residents who are assessed for depression during the last 4 weeks / 3 months / > 3 months |
Total number of residents |
| 5. Number of residents who are assessed for quality of life during the last 4 weeks / 3 months / > 3 months |
Total number of residents |
|
Recommended interventions |
|
| 6. Number of residents for whom a case conference was conducted since he/she moved in |
Total number of residents |
| 7. Number of residents who received multisensory stimulation interventions | |
| 8. Number of residents who received validation therapy | |
| 9. Number of residents who were daily in the open air during the last week | |
| 10. Number of residents who were not at all in the open air during the last week | |
| 11. Number of residents who participated in a physical activity | |
| 12. Number of residents who received an intervention for managing an acute psychiatric crisis during the last six months | |
|
Behavioral problems |
|
| 13. Number of residents with delusions |
Total number of residents |
| 14. Number of residents with hallucinations | |
| 15. Number of residents with depression | |
| 16. Number of residents with anxiety | |
| 17. Number of residents with euphoria | |
| 18. Number of residents with aggression/agitation | |
| 19. Number of residents with apathy | |
| 20. Number of residents with disinhibition | |
| 21. Number of residents with irritability | |
| 22. Number of residents with aberrant motor behavior | |
| 23. Number of residents with problematic nightly behavior | |
| 24. Number of residents with problematic eating behavior | |
|
Dementia | |
| 25. Number of residents with a medical diagnosis of dementia |
Total number of residents |
| 26. Number of residents with dementia according to DSS | |
| 27. Number of residents with dementia according to FAST | |
a The total number refers to the number of residents with complete data for this item.
Discussion
The DemenzMonitor is the first study in Germany to assess how dementia care is provided in nursing homes with respect to structural conditions and psychosocial interventions and to link these data with residents’ outcome measurements.
The study is intended to be repeated every year to facilitate long term observations. Yearly repetition will allow structural changes in the nursing home care sector to be monitored, and longitudinal data will allow the investigation of relations without experimental manipulation.
The newly developed questionnaires allow the characterization of participating institutions in multiple ways. Given the broad variety of facilities, it will be possible to evaluate different aspects of care and the influence of resident and facility characteristics. Because the questionnaires are partly based on the German guideline and only parts are used internationally, conclusions drawn from the study will apply primarily to the German long term care system. However, the results of the study will contribute to the exploration of complex residents’ outcomes, such as quality of life and challenging behavior by adding to the body of literature on this topic [58-63]. The longitudinal approach of the study will allow for the observation of changes and factors associated with changes in residents’ outcome measures and the exploration of variations in resident outcomes. Understanding the nature of change is important for the development of interventions and the identification of residents who most likely will benefit from them [64].
The knowledge derived from this study is also important for the further development of quality tools, including national guidelines and instruments to enhance the quality of care, such as quality indicators. Moreover, this study will allow for a deeper understanding of which interventions should be recommended for whom and when. Regarding the methodological development of quality indicators, this study will contribute information on what type of self-reported data should be considered as a data source for quality indicators. Further testing of the developed questionnaire would be required to determine the validity and reliability.
Limitations
This study design has certain limitations that restrict the generalizability of the results. Because data are derived from a convenience sample, the results are limited in their representativeness. Once the study is established and experience is gained concerning the data collection procedures, changes in the sampling strategy will be considered. Given this recruitment approach, the results from the study must be interpreted cautiously. Best performing institutions may be more willing to participate, which could cause a potential selection bias. Moreover, data concerning the provision of care are collected using staff self-reports, resulting in a potential bias due to social desirability. Concerning the residents’ assessments, proxy-ratings also have methodological constraints. For quality of life, proxy-ratings systematically score lower than self-ratings [65,66] and correlate with caregiver burden [67] and staff attitudes [59,68].
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
RP drafted the manuscript. KK, CS, SB, and BH helped draft this manuscript. All authors contributed to designing the study. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Rebecca Palm, Email: Rebecca.Palm@dzne.de.
Kerstin Köhler, Email: Kerstin.Koehler@dzne.de.
Christian GG Schwab, Email: Christian.Schwab@dzne.de.
Sabine Bartholomeyczik, Email: Sabine.Bartholomeyczik@uni-wh.de.
Bernhard Holle, Email: Bernhard.Holle@dzne.de.
Acknowledgements
The German Centre for Neurodegenerative Diseases funded the study.
References
- Rothgang H, Iwansky S, Müller R, Sauer S, Unger R. BARMER GEK Pflegereport 2010 [BARMER GEK Care Report 2010] St. Augustin: Asgard-Verlag; 2010. Volume 5. [Google Scholar]
- Schneekloth U, Törne I. In: Pflegebedarf und Versorgungssituation bei älteren Menschen in Heimen. Schneekloth U, Wahl HW, editor. Stuttgart: Kohlhammer Verlag; 2009. Entwicklungstrends in der stationären Versorgung - Ergebnisse der Infratest-Repräsentativerhebung [Development trends in long term care-results of a representative infratest survey] pp. 43–157. [Google Scholar]
- Rahman AN, Schnelle JF. The nursing home culture-change movement: recent past, present, and future directions for research. Gerontologist. 2008;48(2):142–148. doi: 10.1093/geront/48.2.142. [DOI] [PubMed] [Google Scholar]
- Ragsdale V, McDougall GJ Jr. The changing face of long-term care: looking at the past decade. Issues Ment Health Nurs. 2008;29(9):992–1001. doi: 10.1080/01612840802274818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michell-Auli P, Kremer-Preiss U, Sowinksi C. Akteure im Quartier - füreinander, miteinander. [Stakeholders in the quarter - with each other, for each other] Pro Alter. 2010. pp. 30–35. November/Dezember.
- Bartholomeyczik S, Halek M, Sowinski C, Besselmann K, Dürrmann P, Haupt M, Kuhn C, Müller-Hergl C, Perrar KM, Riesner C, In: Rahmenempfehlungen zum Umgang mit herausforderndem Verhalten bei Menschen mit Demenz in der stationären Altenhilfe [Guidelines for handling challenging behavior in people with dementia living in nursing homes] Gesundheit B f, editor. Berlin; 2007. [Google Scholar]
- Palm R, Köhler K, Dichter MN, Bartholomeyczik S, Holle B. Entwicklung, Umsetzung und Evaluation pflegerischer Interventionen für Menschen mit Demenz in der stationären Altenhilfe in Deutschland - eine Literaturstudie. [Development, application and evaluation of nursing interventions for people with dementia in nursing homes in Germany - a literature review] Pflege. 2013;26(5):337–355. doi: 10.1024/1012-5302/a000317. [DOI] [PubMed] [Google Scholar]
- Abrahamson K, Lewis T, Perkins A, Clark D, Nazir A, Arling G. The influence of cognitive impairment, special care unit placement, and nursing facility characteristics on resident quality of life. J Aging Health. 2013;25(4):574–588. doi: 10.1177/0898264313480240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crespo M, Hornillos C, Gomez MM. Dementia special care units: a comparison with standard units regarding residents' profile and care features. Int Psychogeriatr. 2013. pp. 1–9. DOI 10.1017/S1041610213001439. [DOI] [PubMed]
- Weyerer S, Schäufele M, Hendlmeier I. Evaluation of special and traditional dementia care in nursing homes: results from a cross-sectional study in Germany. Int J Geriatr Psychiatry. 2010;25(11):1159–1167. doi: 10.1002/gps.2455. [DOI] [PubMed] [Google Scholar]
- Lai CK, Yeung JH, Mok V, Chi I. Special care units for dementia individuals with behavioural problems. Cochrane Database Syst Rev. 2009;4 doi: 10.1002/14651858.CD006470.pub2. CD006470. [DOI] [PubMed] [Google Scholar]
- Wolf-Ostermann K, Worch A, Fischer T, Wulff I, Gräske J. Health outcomes and quality of life of residents of shared-housing arrangements compared to residents of special care units - results of the Berlin DeWeGE-study. J Clin Nurs. 2012;21(21–22):3047–3060. doi: 10.1111/j.1365-2702.2012.04305.x. [DOI] [PubMed] [Google Scholar]
- Verbeek H, Zwakhalen SM, van Rossum E, Ambergen T, Kempen GI, Hamers JP. Dementia care redesigned: Effects of small-scale living facilities on residents, their family caregivers, and staff. J Am Med Dir Assoc. 2010;11(9):662–670. doi: 10.1016/j.jamda.2010.08.001. [DOI] [PubMed] [Google Scholar]
- de Rooij AH, Luijkx KG, Schaafsma J, Declercq AG, Emmerink PM, Schols JM. Quality of life of residents with dementia in traditional versus small-scale long-term care settings: a quasi-experimental study. Int J Nurs Stud. 2012;49(8):931–940. doi: 10.1016/j.ijnurstu.2012.02.007. [DOI] [PubMed] [Google Scholar]
- Vasse E, Vernooij-Dassen M, Cantegreil I, Franco M, Dorenlot P, Woods B, Moniz-Cook E. Guidelines for psychosocial interventions in dementia care: a European survey and comparison. Int J Geriatr Psychiatry. 2012;27(1):40–48. doi: 10.1002/gps.2687. [DOI] [PubMed] [Google Scholar]
- Seitz D, Purandare N, Conn D. Prevalence of psychiatric disorders among older adults in long-term care homes: a systematic review. Int Psychogeriatr. 2010;22(7):1025–1039. doi: 10.1017/S1041610210000608. [DOI] [PubMed] [Google Scholar]
- Vasse E, Moniz-Cook E, Rikkert MO, Cantegreil I, Charras K, Dorenlot P, Fumero G, Franco M, Woods B, Vernooij-Dassen M. The development of quality indicators to improve psychosocial care in dementia. Int Psychogeriatr. 2012;24(6):921–930. doi: 10.1017/S1041610211002523. [DOI] [PubMed] [Google Scholar]
- Cadigan RO, Grabowski DC, Givens JL, Mitchell SL. The quality of advanced dementia care in the nursing home: the role of special care units. Med Care. 2012;50(10):856–862. doi: 10.1097/MLR.0b013e31825dd713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruneir A, Lapane KL, Miller SC, Mor V. Is dementia special care really special? A new look at an old question. J Am Geriatr Soc. 2008;56(2):199–205. doi: 10.1111/j.1532-5415.2007.01559.x. [DOI] [PubMed] [Google Scholar]
- Forbes D, Forbes S, Morgan DG, Markle-Reid M, Wood J, Culum I. Physical activity programs for persons with dementia. Cochrane Database Syst Rev. 2008;3 doi: 10.1002/14651858.CD006489.pub2. CD006489. [DOI] [PubMed] [Google Scholar]
- Woods B, Spector A, Jones C, Orrell M, Davies S. Reminiscence therapy for dementia. Cochrane Database Syst Rev. 2005;2 doi: 10.1002/14651858.CD001120.pub2. CD001120. [DOI] [PubMed] [Google Scholar]
- Neal M, Briggs M. Validation therapy for dementia. Cochrane Database Syst Rev. 2003;3 doi: 10.1002/14651858.CD001394. CD001394. [DOI] [PubMed] [Google Scholar]
- Viggo Hansen N, Jorgensen T, Ortenblad L. Massage and touch for dementia. Cochrane Database Syst Rev. 2006;4 doi: 10.1002/14651858.CD004989.pub2. CD004989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vink AC, Birks JS, Bruinsma MS, Scholten RJ. Music therapy for people with dementia. Cochrane Database Syst Rev. 2004;3 doi: 10.1002/14651858.CD003477.pub2. CD003477. [DOI] [PubMed] [Google Scholar]
- Chung JC, Lai CK, Chung PM, French HP. Snoezelen for dementia. Cochrane Database Syst Rev. 2002;4 doi: 10.1002/14651858.CD003152. CD003152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistisches Bundesamt. Pflegestatistik 2011. Pflege im Rahmen der Pflegeversicherung. [Care Statistics 2011. Care according to the Long Term Care Insurance.] Wiesbaden: Statistisches Bundesamt; 2013. [Google Scholar]
- Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol. 2001;30(4):668–677. doi: 10.1093/ije/30.4.668. [DOI] [PubMed] [Google Scholar]
- Richard L, Gauvin L, Raine K. Ecological models revisited: their uses and evolution in health promotion over two decades. Annu Rev Public Health. 2011;32:307–326. doi: 10.1146/annurev-publhealth-031210-101141. [DOI] [PubMed] [Google Scholar]
- Susser M, Susser E. Choosing a future for epidemiology: II From black box to Chinese boxes and eco-epidemiology. Am J Public Health. 1996;86(5):674–677. doi: 10.2105/AJPH.86.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaren L, Hawe P. Ecological perspectives in health research. J Epidemiol Community Health. 2005;59(1):6–14. doi: 10.1136/jech.2003.018044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton MP, Nahemow L. In: The psychology of adult development and aging. Eisdorfer C, Lawton MP, editor. Washington, D.C: American Psychological Association; 1973. Ecology and the ageing process; pp. 619–674. [Google Scholar]
- Nahemow L, Lawton MP. Toward an ecological theory of adaptation and aging. Environmental Design Research. 1973;1:24–32. [Google Scholar]
- Grant JS, Davis LL. Selection and use of content experts for instrument development. Res Nurs Health. 1997;20(3):269–274. doi: 10.1002/(SICI)1098-240X(199706)20:3<269::AID-NUR9>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Lynn MR. Determination and quantification of content validity. Nurs Res. 1986;35(6):382–385. [PubMed] [Google Scholar]
- Presser S, Couper MP, Lessler JT, Martin E, Martin J, Rothgeb JM, Singer E. Methods For Testing And Evaluating Survey Questions. Public Opin Q. 2004;68(1):109–130. doi: 10.1093/poq/nfh008. [DOI] [Google Scholar]
- Napoles-Springer AM, Santoyo-Olsson J, O'Brien H, Stewart AL. Using cognitive interviews to develop surveys in diverse populations. Med Care. 2006;44(11 Suppl 3):21–30. doi: 10.1097/01.mlr.0000245425.65905.1d. [DOI] [PubMed] [Google Scholar]
- Lawton MP. Quality of life in Alzheimer disease. Alzheimer disease and associated disorders. 1994;8(Suppl 3):138–150. [PubMed] [Google Scholar]
- Lawton MP. In: The Concept and Measurement of Quality of Life in the Frail Elderly. Birren JE, Lubben JE, Rowe JC, Deutchman DE, editor. San Diego: Academic Press, Inc; 1991. A Multidimensional View of Quality of Life in Frail Elders; pp. 3–27. [Google Scholar]
- Kane RA. Definition, measurement, and correlates of quality of life in nursing homes: toward a reasonable practice, research, and policy agenda. Gerontologist. 2003;43(Spec No 2):28–36. doi: 10.1093/geront/43.suppl_2.28. [DOI] [PubMed] [Google Scholar]
- Brod M, Stewart AL, Sands L, Walton P. Conceptualization and measurement of quality of life in dementia: the dementia quality of life instrument (DQoL) Gerontologist. 1999;39(1):25–35. doi: 10.1093/geront/39.1.25. [DOI] [PubMed] [Google Scholar]
- Ettema TP, Droes RM, de Lange J, Mellenbergh GJ, Ribbe MW. A review of quality of life instruments used in dementia. Qual Life Res. 2005;14(3):675–686. doi: 10.1007/s11136-004-1258-0. [DOI] [PubMed] [Google Scholar]
- Ettema TP, Droes RM, de Lange J, Mellenbergh GJ, Ribbe MW. QUALIDEM: development and evaluation of a dementia specific quality of life instrument-validation. Int J Geriatr Psychiatry. 2007;22(5):424–430. doi: 10.1002/gps.1692. [DOI] [PubMed] [Google Scholar]
- Dichter M, Bartholomeyczik S, Nordheim J, Achterberg W, Halek M. Validity, reliability, and feasibility of a quality of life questionnaire for people with dementia. Z Gerontol Geriatr. 2011;44(6):405–410. doi: 10.1007/s00391-011-0235-9. [DOI] [PubMed] [Google Scholar]
- Dichter MN, Dortmann O, Halek M, Meyer G, Holle D, Nordheim J, Bartholomeyczik S. Scalability and internal consistency of the German version of the dementia-specific quality of life instrument QUALIDEM in nursing homes - a secondary data analysis. Health and quality of life outcomes. 2013;11:91. doi: 10.1186/1477-7525-11-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouman AI, Ettema TP, Wetzels RB, van Beek AP, de Lange J, Droes RM. Evaluation of Qualidem: a dementia-specific quality of life instrument for persons with dementia in residential settings; scalability and reliability of subscales in four Dutch field surveys. Int J Geriatr Psychiatry. 2011;26(7):711–722. doi: 10.1002/gps.2585. [DOI] [PubMed] [Google Scholar]
- Zuidema S, Koopmans R, Verhey F. Prevalence and predictors of neuropsychiatric symptoms in cognitively impaired nursing home patients. J Geriatr Psychiatry Neurol. 2007;20(1):41–49. doi: 10.1177/0891988706292762. [DOI] [PubMed] [Google Scholar]
- Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology. 1994;44(12):2308–2314. doi: 10.1212/WNL.44.12.2308. [DOI] [PubMed] [Google Scholar]
- Kaufer DI, Cummings JL, Ketchel P, Smith V, MacMillan A, Shelley T, Lopez OL, DeKosky ST. Validation of the NPI-Q, a brief clinical form of the Neuropsychiatric Inventory. J Neuropsychiatry Clin Neurosci. 2000;12(2):233–239. doi: 10.1176/appi.neuropsych.12.2.233. [DOI] [PubMed] [Google Scholar]
- Olde Rikkert MG, Tona KD, Janssen L, Burns A, Lobo A, Robert P, Sartorius N, Stoppe G, Waldemar G. Validity, reliability, and feasibility of clinical staging scales in dementia: a systematic review. Am J Alzheimers Dis Other Demen. 2011;26(5):357–365. doi: 10.1177/1533317511418954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-Mental State (a practical method for grading the state of patients for the clinician) J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Reisberg B. Functional assessment staging (FAST) Psychopharmacol Bull. 1988;24(4):653–659. [PubMed] [Google Scholar]
- Schäufele M, Köhler L, Lode S, Weyerer S. In: Pflegebedarf und Versorgungssituation bei älteren Menschen in Heimen Demenz, Angehörige und Freiweillige, Beispiele für "Good Practice". Schneekloth U, Wahl HW, editor. Stuttgart: Kohlhammer Verlag; 2009. Menschen mit Demenz in stationären Altenpflegeeinrichtungen: aktuelle Versorgungssituation [People with dementia in nursing homes: current life and care situation] pp. 159–219. [Google Scholar]
- Köhler L, Weyerer S, Schäufele M. Proxy screening tools improve the recognition of dementia in old-age homes: results of a validation study. Age Ageing. 2007;36(5):549–554. doi: 10.1093/ageing/afm108. [DOI] [PubMed] [Google Scholar]
- Sclan SG, Reisberg B. Functional assessment staging (FAST) in Alzheimer's disease: reliability, validity, and ordinality. International psychogeriatrics/IPA 1992. 1992;4(Suppl 1):55–69. doi: 10.1017/s1041610292001157. [DOI] [PubMed] [Google Scholar]
- Lawton PM, Brody EM. Assessement of Older People: Self-Maintaining and Instrumental Activities of Daily Living. Gerontologist. 1969;9(3):179–186. [PubMed] [Google Scholar]
- Moniz-Cook E, Vernooij-Dassen M, Woods R, Verhey F, Chattat R, De Vugt M, Mountain G, O'Connell M, Harrison J, Vasse E. et al. A European consensus on outcome measures for psychosocial intervention research in dementia care. Aging Ment Health. 2008;12(1):14–29. doi: 10.1080/13607860801919850. [DOI] [PubMed] [Google Scholar]
- Schwab CGG, Palm R, Holle B. 57. Jahrestagung der Deutschen Gesellschaft für Medizinische Informatik, Biometrie und Epidemiologie e.V. (GMDS), 42. Jahrestagung der Gesellschaft für Informatik e.V. (GI): 16.-21.09.2012. Braunschweig; 2012. Automatisiertes Reporting von Forschungsdaten für Einrichtungen der stationären Altenhilfe. [Automated Reporting of Research Data for Nursing Homes] [Google Scholar]
- Abrahamson K, Clark D, Perkins A, Arling G. Does cognitive impairment influence quality of life among nursing home residents? Gerontologist. 2012;52(5):632–640. doi: 10.1093/geront/gnr137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winzelberg GS, Williams CS, Preisser JS, Zimmerman S, Sloane PD. Factors associated with nursing assistant quality-of-life ratings for residents with dementia in long-term care facilities. Gerontologist. 2005;45(1):106–114. doi: 10.1093/geront/45.suppl_1.106. [DOI] [PubMed] [Google Scholar]
- Samus QM, Rosenblatt A, Steele C, Baker A, Harper M, Brandt J, Mayer L, Rabins PV, Lyketsos CG. The association of neuropsychiatric symptoms and environment with quality of life in assisted living residents with dementia. Gerontologist. 2005;45(1):19–26. doi: 10.1093/geront/45.suppl_1.19. [DOI] [PubMed] [Google Scholar]
- Li XJ, Suishu C, Hattori S, Liang HD, Gao H, Feng CQ, Lou FL. The comparison of dementia patient's quality of life and influencing factors in two cities. J Clin Nurs. 2013;22(15–16):2132–2140. doi: 10.1111/jocn.12032. [DOI] [PubMed] [Google Scholar]
- Wetzels RB, Zuidema SU, de Jonghe JF, Verhey FR, Koopmans RT. Determinants of quality of life in nursing home residents with dementia. Dement Geriatr Cogn Disord. 2010;29(3):189–197. doi: 10.1159/000280437. [DOI] [PubMed] [Google Scholar]
- Koopmans RT, van der Molen M, Raats M, Ettema TP. Neuropsychiatric symptoms and quality of life in patients in the final phase of dementia. Int J Geriatr Psychiatry. 2009;24(1):25–32. doi: 10.1002/gps.2040. [DOI] [PubMed] [Google Scholar]
- Hoe J, Hancock G, Livingston G, Woods B, Challis D, Orrell M. Changes in the quality of life of people with dementia living in care homes. Alzheimer Dis Assoc Disord. 2009;23(3):285–290. doi: 10.1097/WAD.0b013e318194fc1e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettema TP, Droes RM, de Lange J, Ooms ME, Mellenbergh GJ, Ribbe MW. The concept of quality of life in dementia in the different stages of the disease. Int Psychogeriatr. 2005;17(3):353–370. doi: 10.1017/S1041610205002073. [DOI] [PubMed] [Google Scholar]
- Gräske J, Fischer T, Kuhlmey A, Wolf-Ostermann K. Quality of life in dementia care-differences in quality of life measurements performed by residents with dementia and by nursing staff. Aging Ment Health. 2012;16(7):819–827. doi: 10.1080/13607863.2012.667782. [DOI] [PubMed] [Google Scholar]
- Novella JL, Jochum C, Jolly D, Morrone I, Ankri J, Bureau F, Blanchard F. Agreement between patients' and proxies' reports of quality of life in Alzheimer's disease. Qual Life Res. 2001;10(5):443–452. doi: 10.1023/A:1012522013817. [DOI] [PubMed] [Google Scholar]
- Sands LP, Ferreira P, Stewart AL, Brod M, Yaffe K. What explains differences between dementia patients' and their caregivers' ratings of patients' quality of life? Am J Geriatr Psychiatry. 2004;12(3):272–280. [PubMed] [Google Scholar]


