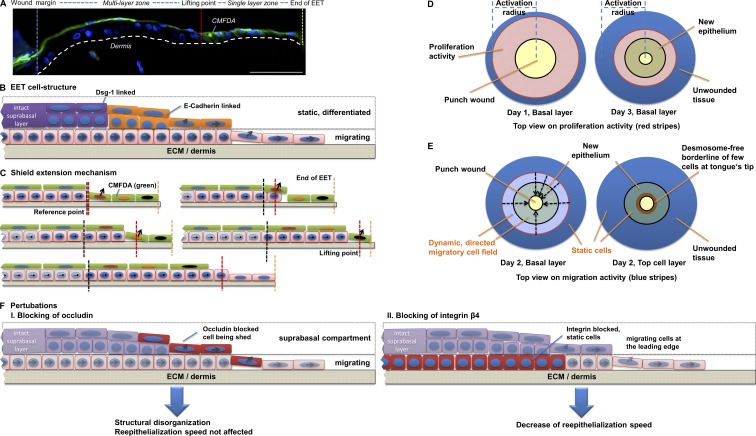
Figure 10.
The ESM is based on collectively migrating basal cells. (A) Results from the double fluorescent staining experiment show that stained cells always become distributed on top of the EET, which can be principally structured in a single layer and a multilayer zone. The broken line denotes dermal–epidermal junction. (B) Cells within the suprabasal compartments of the multilayer zone form mechanically stable tight junctions and desmosomes serving as a shield for the underlying wound bed. Because of its cell junction composition, this suprabasal layer is more static, whereas the underlying basal compartment exclusively expresses E- and P-cadherin, which can rapidly be remodeled, showing a dynamic migration behavior. (C) Because of the mechanically stable structure of the shield, extension can only be achieved by adding cells at the point at which the single layer zone connects to the multilayer zone (lifting point). At the lifting point, cells are transported upwards by following basal cells, whereas not yet lifted single-layer tip cells continue migration until they are lifted by the following cells. (D) Cells of the basal layer that supply the extending shield are in the beginning (day 1) produced in the intact unwounded tissue by a proliferative burst. With progressing wound closure (day 3), proliferation activity follows the EET to the center of the wound. (E) Viewed from top, dynamically moving cell fields can be identified characterized by directed cell migration. Although basal cells from the unwounded tissue show collective cell migration to actively supply the shield extension, static suprabasal cells shield the in-migrating basal cells by continuously building a mechanically stable barrier. (F) Depending on the contact point of perturbation, it results in a structural disorganization and shedding of occludin-blocked cells or in a decrease of reepithelialization speed if integrin β4 is blocked. Bar, 100 µm.