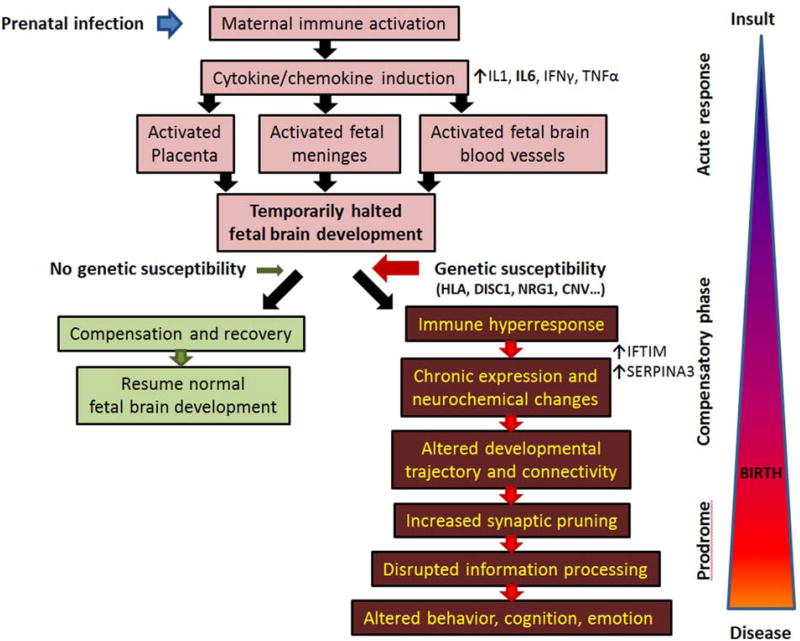
Figure 3. Schematic representation of maternal immune activation and its proposed role in schizophrenia pathophysiology.
Prenatal infection leads to strong maternal immune system activation, which induces a systemic release of cytokines, including, but not limited to IL1, IL6, TNFα and IFγ. These cytokines, and especially IL6, have multiple effects on the developing fetus involving activation of placenta, fetal blood vessel and fetal meninges. The developing brain, even in the absence of the virus, is flooded by cytokines and immune-response proteins. This leads to temporarily slowed/halted development, which in the absence of genetic susceptibility resumes normally in a relatively short period of time. Yet, in the presence of schizophrenia-predisposing genetic elements the fetal meninges and blood vessels are hyper responsive, the inflammatory response becomes chronic, and never quite disappears. This low-level, persistent blood vessel and meningeal immune activation results in continuous secretion of various chemokines and cytokines, changing postnatal developmental trajectory by interfering with proper neuronal connectivity and potentially altering normal synapse pruning. As a result, once the brain's intrinsic compensatory mechanisms are exhausted, information processing is disrupted, and the symptoms of the disease manifest themselves.