Abstract
School-based interventions are thought to be the most universally applicable and effective way to counteract low physical activity (PA) and fitness although there is controversy about the optimal strategy to intervene. The objective of this review was therefore to summarize recent reviews with the aim of increasing PA or fitness in youth and carry out a systematic review of new intervention studies. Relevant systematic reviews and original controlled and randomized controlled school-based trials with a PA or fitness outcome measure, a duration of ≥12 weeks, a sufficient quality and involvement of a healthy (non-clinical) population aged 6-18 years that were published from 2007-2010 were included. In these reviews, 47-65% of trials were found to be effective. The effect was mostly seen in school-related PA while effects outside school were often not observed or assessed. The school-based application of multicomponent intervention strategies was the most consistent promising intervention strategy, while controversy existed regarding the effectiveness of family involvement, focus on healthy populations at increased risk, or duration and intensity of the intervention. All 20 trials fulfilling the inclusion criteria in the review update showed a positive effect on in-school, out-of-school or overall PA, and 6 of 11 studies showed an increase in fitness. Taking into consideration both assessment quality and Public Health relevance, multicomponent approaches in children including family components showed the highest level of evidence for increasing overall PA. This review confirms the Public Health potential of high quality school-based PA interventions for increasing PA and possibly fitness in healthy children and adolescents.
Keywords: Physical activity, fitness, motor skills, children, adolescents, school, intervention
INTRODUCTION
Physical inactivity and low fitness in children and adolescents are raising health burdens worldwide. Physical inactivity in adults has been established as one of the leading established risk factors for mortality1 and burden of disease.2 Moreover, a high fitness has been shown to prolong life and even seems to be able to counterbalance adiposity-related mortality.1 The fact that these factors also track into adulthood,3 emphasizes the necessity to evaluate and find effective strategies for increasing physical activity (PA) and fitness in youth. School is the place where almost all of the children and adolescents spend most of their days and family-based interventions have been shown to be of limited effectiveness. 4-5 Therefore, a focus on the globally available school system seems justified.
As well-performed and relatively recent systematic reviews were available, we decided to summarize existing knowledge from these reviews and focus on the new literature of school-based interventions not included in the earlier reviews. We have used compatible search strategies and have not included articles published during the periods studied in the earlier reviews, but some studies may have been included in several reviews.
The objective of this review was therefore 1. to summarize recent reviews of studies with the aim of increasing PA or fitness in children and adolescents, 2. to define, based on these reviews, potentially relevant factors for a positive outcome, and 3. to carry out a systematic review of new intervention studies and prospectively verify the predefined factors.
Methods
The base of this review was the collection of recent systematic reviews published after 2006 that summarized the evidence on PA promotion in children and adolescents and update these reviews by searching original controlled and randomized controlled school-based trials published afterwards. The reviews were analyzed in detail by one researcher (SK) and discussed with the co-authors.
Literature search and quality control
For our own systematic review, we used a combination of the search strategy used by others 6,5 and applied it to Pubmed, Medline, Embase, Psycinfo, Sportdiscus and Embase using a time frame from January 2007 to December 2010 (Supplementary Table 1). Inclusion criteria were 1. controlled (CT) or randomized, controlled trials (RCT) of interventions aimed at increasing PA or fitness, 2. target populations including school-aged children from 6 to 18 years of age (corresponding to mandatory school age), 3. PA or fitness measured as an outcome at baseline and at least one follow-up, 4. a duration of the intervention of at least 3 months, 5. intervention delivered at school, 6. control group not receiving a PA intervention, and 7. statistical analyses of the PA/fitness outcome reported. Studies in children with a specific disease or studies applying structured exercise programs for obese children were excluded. Likewise we did not include trials with the main goal of decreasing inactivity.
Two reviewers (SK, UM) each checked half of the titles and abstracts obtained from the searches. After exclusion of non-relevant studies, each remaining paper was read in full text by two researchers (UM, SK or EM) who independently scored them. The methodological quality of the studies was then assessed using a predefined previously used quality assessment tool focussing mainly on internal validity (Supplementary Table 3).5 Any disagreement was solved by discussion and studies of weak methodology, i.e. with a score below 5 of 10, were excluded.
Data extraction and evaluation
An overview of the studies included was established. Thereafter, a checklist with the relevant trial characteristics was constructed to allow a systematic data extraction. These factors included the age group (children vs. adolescents), duration of the trials (interventions of 1 year or less vs. longer trials), focus of the trials (solely on the school setting vs. including also family or community components), implementation by classroom teachers or physical education specialists, mandatory or voluntary nature of the intervention, method of outcome assessment (accelerometers, pedometers or observation vs. questionnaires; VO2max test vs. field tests). Children were defined as the age group up to 12 years, while adolescents were 13 years old or older. A program was defined mandatory if the intervention was an integral part of the school curriculum in which neither teachers nor children had the free choice of participation or withdrawal, and if there was a report of compliance or the intervention was monitored. This rating was carried out by two independent researchers prior to the systematic reporting of study results. In case of disagreement consensus was reached by discussion.
RESULTS
Summary and synthesis of recent reviews with focus on the school setting
Table 1 provides an overview of the four most recent and comprehensive systematic reviews covering PA promotion in schools.4-8 The reviews included controlled or (cluster)-randomized controlled trials with the goal of PA promotion in youth reporting a baseline and at least one follow-up measure of PA and/or fitness. Between 754 and 100%9 of studies included focused on the school system. While the upper range of age included was generally 18 to19 years of age, the lower range of age varied from no limit,5 to 4 years,4 6 years9 or 10 years.7 A description of the reviews and their conclusions is provided below.
Table 1.
Overview of systematic reviews of school-based physical activity or lifestyle interventions to increase physical activity or fitness in children and adolescents
| Dobbins | De Meester/ Crutzen |
Salmon | van Sluijs | current review | |
|---|---|---|---|---|---|
| Time searched | to June 07 | from Jan 95 to May 08 | from Jan 85 to June 06 | to Dec 06 | from Jan 07 to Dec 10 |
| Databases searched | Medline, Biosis, Cinahl, Embase, Sportdiscus, Psycinfo, Sociological abstracts, Central |
Pubmed, Medline, Web of Science, Sport Discus, Cochrane library |
Medline, Biosis, Cinahl, Embase, Sportdiscus, Psycinfo, PsycARTICLES, Cochrane, Central, ScienceDirect, Web of Knowledge, Social SciSearch, Ovid Databases |
Medline, Embase, Sportdiscus, Psycinfo, Pubmed, Scopus |
Medline, Embase, Sportdiscus, Psycinfo, Pubmed, Scopus |
| Inclusion criteria |
primarily school-based int that promote PA and/or fitness |
all interventions that promote PA among European teenagers |
all interventions that promote PA |
all interventions that promote PA |
primarily school-based interventions to promote PA and/or fitness |
| CT or RCT with PA/fitness measured at baseline and post-intervention | |||||
| Setting | school, school and/or family and/or community |
school, family, community, primary care, internet |
school, family, community, internet- based, primary care |
school, family, community | school, school and family or community |
| Quality control | Cochrane recommendations, i.e. external validity, study design, confounders, blinding, reliability/validity of measurement tool, dropouts |
no quality control | based on predominantly internal validity, including baseline comparability, randomisation, unit of analyses, validated outcome measure, dropout, timing of measurement, follow up measure, intention-to-treat analysis, blinding, confounding |
||
| Exlusion critera | low quality | if only fitness or PA during PE reported |
sample size (n<16), if only fitness measured |
none | low quality, duration <3 months |
|
Selected studies
in children/in adolescents/in both in school setting |
n=26 22/4/0 all (=100%) |
n=20 0/20/0 15/20 (=75%) |
n=76 42/25/9 57/76 (=75%) |
n=57 33/24/0 47/57 (=82%) |
n=20 15/4/1 all (=100%) |
| Age | 6 to 18 years | 10 to 19 years | 4 to 19 years | ≤18 years | 6 to 18 years |
|
Countries
(US+Canada/Europe/other) |
16/8/2 | 0/20/0 | 59/14/3 | 37/17/3 | 6/12/3 |
|
Overall results (with
special focus on studies including the school system) |
|
|
|
|
|
|
Intervention success
factors |
|
|
|
|
|
| Significant effect on PA | 8/14 (57%) | 13/20 (65%) | PA: 38/76 (50%) | 27/57 (47%) | 16/16(100%) |
|
Significant effect on
fitness |
3/5 (60%) | na | na | na | 6/11 (55%) |
|
Significant effect on
motor skills |
na | na | na | na | 4/6 (67%) |
Abbreviations: PA=physical activity, LTPA=leisure time PA (=PA outside school), PE=physical education, CT=controlled trial, RCT=randomized controlled trial, SES=socio-economic status, na=not applicable.
Dobbins et al.4 reviewed the available evidence of school-based PA promotion including trials up to June 2007. After a rigorous quality control of the potentially eligible trials based on Cochrane recommendations, they reported results of 26 studies. They reported positive impact on duration of PA (mostly for PA during school time) and on aerobic fitness measured by VO2max, but there was no evidence that school-based trials also affected out-of-school PA positively. Although the authors were positive about the beneficial effects in general, this evidence was mostly based on self-reports. The authors discussed several limitations of included studies such as the low number of trials reporting out-of-school PA (n=7) despite the fact that the primary goal of most trials was to promote overall PA, the lack of long-term follow-up, and the measurement of PA mostly by self-report which may have attenuated the results due to the inability of accurately reporting PA by children.10 They further remarked that the most notable difference regarding effects on out-of-school PA was the use of physical education specialists to deliver the intervention. For PA in school, successful trials tended to intervene for a longer period and applied multicomponent approaches. All these studies were conducted in children.
De Meester et al.7 included trials in European teenagers that were published from 1995 to May 2008 and identified 20 relevant studies. They found that school-based interventions lead to short-term improvements in PA levels, but effects were limited to school-related PA with no conclusive transfer to out-of-school PA. In a second article integrating the analyses of effect sizes8 they concluded, in contrast to the original review, that a multi-component approach including environmental components and a focus on PA only rather than aiming to change several health behaviours was most effective. PA improvements were reported to be of short duration, as in all 3 studies including longer term follow-up increases were not maintained. The authors also discussed the absence of school-based PA increases to out-of-school PA increases. Their original suggestion of an additional involvement of families was supported by 3 favourable trials combining the school and family setting. However, based on the effect size calculations it was later considered premature.8
Salmon et al.4 reviewed the literature from 1985 to June 2006 and summarized the findings of 76 studies, with 57 of them (=75%) carried out in the school setting. Half of the studies were effective at increasing PA (not further specified). The authors observed that 16 of 25 (=64%) studies using objective PA measures reported positive effects on PA compared to 25 of 66 (=38%) studies using questionnaires. They felt that multicomponent interventions focusing on physical education, that implemented activity breaks or that included family strategies were most successful among children, but the situation was inconclusive in adolescents. In many trials, overall PA was not measured leaving the debate open whether successful increases in PA during school would be sustained during out-of-school or rather compensated by a respective decrease as suggested11-12 by others. Many of the studies included in this review were not considered in the review by Dobbins et al.9 because of weaknesses in their methodology - although this was recognized.
Van Sluijs et al.5 summarized all interventions with a PA promotion in youth up to December 2006. Fifty-seven studies were identified, with 47 involving the school system and about half of them of high quality. As in the other reviews presented above, a meta-analysis was not performed, because of the methodological heterogeneity of the studies. Although all studies were included that fulfilled the inclusion criteria, level of evidence was drawn on the basis of consistency of results of studies with the highest available level of quality. Strong evidence was found for the effectiveness of multicomponent interventions and for trials including both school and family or community components in adolescents, while there was no conclusive finding for the best strategy in children. Interventions seemed to be more effective in adolescents than in children. Based on their findings, the authors questioned the usefulness of interventions targeting ethnic minority populations or girls only, or approaches using isolated educational approaches. They also mentioned important limitations of many studies caused by the absent description of attendance, of implementation or of quality assurance in the interventions. The total lack of cross-cultural evaluation of the studies also made it impossible to generalise findings from different parts of the world.
In summary, the existing reviews of trials promoting PA in schools agreed upon their positive impact but have not supplied a clear picture of effective strategies to increase PA and/or fitness in youth. Their conclusions concerning the effects of specific intervention types in different age groups varied. Methodological limitations in existing studies were cited including the lack of valid PA measures, of data on overall PA, on compliance and the lack of studies with long-term follow-up or clear implementation strategies. All requested more trials of adequate quality to be performed.
New literature since January 2007
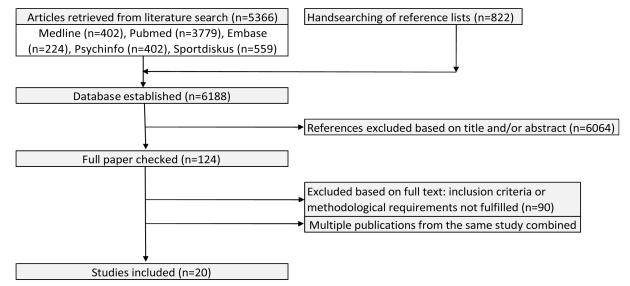
Figure 1 presents a flowchart of the literature search. We identified 20 relevant trials (11 randomized controlled and 9 controlled trials) (Supplementary Table 2)13-34 of sufficient quality (see Supplementary Table 3 for the rating system and results of the methodological quality assessment) published between January 2007 and December 2010. Sixteen of 20 trials reported effects on a PA outcome, 11 of 20 reported on a fitness-related outcome and 6 of 20 assessed also motor skills. A list of excluded studies, based on full text reviews is provided in Supplementary Table 4.
Figure 1.
Flowchart of study selection in updated review
Three trials were performed in the US, two in Canada, 12 in Europe, and one each in Australia, Brazil and Iran. The study size at baseline ranged from 132 to 2848 and the duration of the intervention from 6 months to 4 years, including seven trials with a duration of more than a year.13,15,19,24,30,33,35 Only three trials reported follow-ups of 6 to 12 months after the end of the intervention.16,25-26 Fourteen trials included children until 12 years of age, 4 studies were done in adolescents, and 2 trials included both age ranges. Most studies focused on a general population of school children, 2 studies only included girls,28,31 and 3 focused on children from low socio-economic backgrounds.22,25-26 About half of the programs were mandatory rather than voluntary, also half of them were multicomponent and 60% included family or community components. The intervention was applied by physical education experts in 5 studies, while in 9 studies classroom teachers were responsible for the implementation, and in 3 studies a combination was used. Among the 16 studies with a PA outcome, 6 trials solely used questionnaires to assess PA14,17,22,27,31,35 and 10 used accelerometers or pedometers in the whole sample16,18,21,23,25-26 or a subsample,13,18,20,33 including 6 that used a combination of PA assessments. Common methodological limitations of the included studies were missing information on the use of intention-to-treat analyses, on blinding procedures or on randomisation procedures and compliance.
Content-wise, each single study was different and none of the program used the same content of intervention. Overall, 4 programs focused solely on education, 4 applied only curricular changes, 1 only changed the environment while the remaining trials used any combination of approaches with educational, curricular or environmental adaptations. About half of the programs complemented physical education lessons and/or added PA breaks, supported active play during recess, lunchtime or after school. This included for example adding additional physical education lessons, provision of equipment, more time for breaks, PA homework or special events during weekends. In addition, most programs added some sort of education as extra lessons during school or as integrated part of the usual curriculum. Two third of all trials integrated family components ranging from simple written advice to audiovisual education or active participation in workshops with or without the children or adolescents.
Effect on physical activity
The overall picture shows that every single study with a PA outcome (n=16) reported a significant intervention effect on at least one domain of PA, either in-school, out-of-school or overall. We defined a hierarchy of PA findings including assessment quality (i.e. objective versus subjective means of PA measurement, RCT versus CT) and Public Health relevance (i.e. overall versus in-school versus out-of-school PA) by using one key PA measure per study that provided the strongest evidence of an intervention effect. Five studies were effective at increasing total PA assessed by accelerometers or pedometers,16,18,21,23,26 but 2 of them showed significant effects only in a subgroup.16,23 By the use of questionnaires, total PA was increased in 4 studies15,17,28,31 (one in a subgroup15) while 1 did not show effects.20 In-school PA was increased in 2 studies,25,32 both using objective means of assessing PA. Out-of-school PA was only assessed by subjective means, but all these 4 studies13-14,22,35 showed significant positive effects on PA in favour of the intervention. Among the 3 studies documenting a longer follow-up (6 to 12 months), all reported maintained effects in at least one measure of PA.16,26,36 Two RCTs with an intervention duration of one school year attained the highest hierarchy level of evidence with significant increases of objectively measured overall PA in the whole study population of children. One applied daily PE lessons with additional PA breaks and PA homework,21 the other focused on providing weekly sessions of either behavioural modification (regarding PA and sedentary behavior), improvement of fundamental motor skills or a combination of both.26 Both RCTs were integrated as part of the school curriculum, used PE specialists and included family support.
Effect on aerobic fitness and motor skills
Aerobic fitness was assessed in 11 studies, of which 3 used spiroergometry (VO2max)28,34,37 and the remaining used field tests such as the shuttle run or a 6-minute run. Six studies21,23-24,28,30,34 showed significant intervention effects, including all studies with VO2max measurements. They all used PE specialists to implement the weekly program which generally consisted of five sessions of at least 45 min. Six studies also assessed motor skills in addition to fitness or PA.15,18,26,30,32,34 Measurements differed considerably, ranging from observational ratings of the form and function of fundamental movement skills like forehead strike, lift and carry or leap15 to different validated tests batteries such as the body coordination test (KTK)19,34 or the Eurofit test.30,33 Four of the trials11,14,23,27 showed significant positive intervention effects. Concomitant effects on fitness or PA were inconsistent and heterogeneous. No follow-up assessments for fitness or motor skills were reported.
DISCUSSION
The school setting has long been defined as the ideal setting for PA promotion interventions. As young people spend the majority of their waking hours in the school setting, it is possible to globally reach the population of interest without having to stigmatize or discriminate and without being primarily dependent on families. Recent reviews generally showed that school-based PA promotion was effective at increasing PA during school, while the critical transfer to a parallel increase in out-of-school or overall PA was less clear. The reviews agreed that multicomponent interventions combining educational, curricular and environmental elements seem to be more effective than isolated education5 or curricular changes4, but opinions differed on whether this was the case for children and adolescents. In some reviews, the focus on change of multiple health behaviours instead of focusing only on PA was considered as a stumbling block for success.7,9 The involvement of families within school-based interventions was well supported by most,4-5,9 but not all reviews.7-8 While Van Sluijs et al.5 stated that studies in adolescents tended to be more successful than in children possibly because of more potential for change and/or a higher quality of studies, the other reviews were unable to draw the same conclusion, possibly limited by small numbers of trials in the adolescent age range. In general, it was highlighted that many studies were of questionable methodology, i.e. assessing only school-related PA and using only questionnaires or permitting only conclusions on short-term follow-up. There was questionable generalizability because of the lack of trans-cultural studies.
The updated literature review identified 20 studies that fulfilled the inclusion and quality criteria and revealed a highly consistent picture with all included studies documenting significant effects on at least one measure of PA and 6 out of 11 trials reporting a significant positive effect on fitness. These findings document stronger evidence than ever that school-based PA interventions are able to increase PA and possibly fitness in healthy children and adolescents. The intervention effects were consistently positive for PA in school, out-of-school PA and even more importantly in 9 out of 10 studies for overall PA. In contrast to most previous reviews, only trials with adequate methodology, a pre-post assessment of PA or fitness and a minimal duration of 3 months were included. The minimal duration was chosen to ascertain training effects38 and at least some sustainability of behavioural change as suggested,9 thereby increasing the strength of evidence of these findings. Of note, the inclusion of 4 studies excluded only based on short duration39-42 would not have changed the conclusions drawn here.
Publication bias in the sense of under-reporting of studies with negative effects might have influenced the overall picture, particularly given the high number of effective studies. However, given the considerable effort that goes into carrying out a proper outcome assessment, it can be assumed that researchers willing to make this effort will also strive to publish their findings even if they are negative. Therefore one might consider not generalising the conclusions of this review to low intensity and low effort physical activity promotion interventions in schools.
the fact that 20 trials were eligible over a 4 year period (compared to 26 trials over 50 years in the Cochrane review9) shows important progress in quality of the published studies. Seventy-five percent of all trials assessing a PA outcome reported on overall PA, in 60% of all studies the PA outcome was measured by objective means. The predominance of positive intervention effects on PA was no longer limited to school-based PA, but extended to out-of-school and overall PA. From a Public Health perspective, this is a very important finding.
In the current compared to the previous reviews, the proportion of European studies was considerably higher. The methodological quality of the included studies has improved considerably, with more overall and objective assessments of PA and with more adequate statistical analyses (i.e. power analyses, cluster adjustment). When looking at the trials with the highest combined hierarchy level of quality and Public Health relevance (i.e.RCTs that assessed overall PA objectively and found significant effects in the whole study population), they both included children, intervened over one school year by multicomponent approaches including physical education, behavioural modification lessons or a combination. The programs were integrated into the regular school curriculum and taught by PE experts, both tried to involve families by written information. Although one has to be cautious to draw conclusions based on two trials, a multicomponent mandatory program with involvement of specialists and supported by the families seems to be effective in increasing overall PA in children. Interestingly, similar conclusions have been drawn for lifestyle interventions in children to reduce obesity.43
These findings confirm previous recommendations to use multicomponent approaches in children to broaden the reach of the population of interest,4-5 and to include families as important mediators for PA outside school4 and for positive attitudes towards PA in general.44 Whether the involvement of family components in school-based interventions for adolescents proves beneficial remains open for debate. While van Sluijs et al.5 described strong evidence based on positive findings in 2 out of 3 high quality RCTs, findings in the review by deMeester et al.7 were inconclusive and effect sizes in the 3 effective studies were at most moderate.45 It is possible that the influence of the family on health behaviour becomes less important in debonding adolescents who are trying to become autonomous.
There was no difference in the effect of interventions on PA whether the study used objective or self-report measures of PA, contrasting findings of previous reviews.4-5 However, several studies used objective means of PA assessment only in a subpopulation,18,20,32,46 which may have induced a selection bias, and some even reported discordant findings when objective and subjective means were both applied.20 Nevertheless, there is no doubt that objective means of assessing PA in the whole study population should be the goal in the future.47 Methodological limitations such as the absence of proper description of the randomisation procedures to judge representativeness of the population, of documentation of compliance of those applying or receiving the intervention, and finally of long-term follow-ups were still present.
Trials assessing aerobic fitness by VO2max were consistently effective at increasing it, while only half of the trials using field tests showed positive effects. Additional factors differentiating effective from ineffective trials were a duration of the intervention of less than 1 year, a mandatory compared to a voluntary nature of the intervention, and an intervention in school only rather than extending it to the family or community. Importantly, they all used PE specialists to implement the program consisting of daily sessions of at least 45 minutes. Studies without an effect on fitness were less intensive, less extensive and mostly voluntary in nature. This underlines the importance of an intervention of sufficient quantity and quality. The method of measuring aerobic fitness may also be an important consideration, since field tests may have methodological limitations in precision, motivation and standardisation. The fact that shorter programs were more effective highlights the risk of losing the interest of teachers and pupils over time. The success of mandatory programs could be indirect evidence that compliance is one of most critical factors in school-based interventions to raise aerobic fitness as one of the most important health factor in youth.38
In general, effects of the intervention on PA were stronger than the effects on fitness. This might be because changes in PA were not sufficient to cause changes in fitness, because the measurements were not of sufficient accuracy or because there was simply over-reporting.
Motor skills were not defined as a main outcome in this review, but they were reported as additional finding in some trials. Four of 6 studies showed significant intervention effects on motor skills, but concomitant effects on fitness or PA were heterogeneous. Based on this review we cannot draw any conclusion on the relevance of focusing on motor skills to increase PA or fitness, although it may be plausible that children and adolescents with improved motor skills would have the precondition to increase their fitness or PA by their improved competence.48
There is now good evidence that school-based interventions can increase PA and fitness in youth. Although this is a first step towards improving health and well-being in youth we are still faced with the much bigger challenge of establishing sustainability of these interventions and their effects as well as transferring these programs into real world settings. The proof of sustainability of effects in these efficacy trials will probably never be done due to the “dispersion nature” of schoolchildren. Some research groups have tried to perform long-term follow-ups but evidence remains brittle because of the tiny percentage of original study populations that could be reached.49-51 Yet, effectiveness trials in larger populations and different settings may shed light on the capacity of large-scale and long-term health effects of PA promotion in youth as nicely shown in malaria prevention programs.52 One program that may be an example in this direction is the Action Schools BC initiative 53-54 which was started in 2004 including 275 schools and 25′740 children and reaching 550′000 children 6 years later. This implementation was supported by the provincial government mandating 30 minutes of daily PA in schools. In order to find the best effectiveness for PA interventions in youth, research efforts should include studying mediation of the intervention effect55-56 and implementation issues,46,57 that should enable us to successfully reach large populations. Further research also needs to consider the generalisability of the results as most of the studies included in the updated review originated from Europe. Now that we can be more confident that school-based PA interventions have the potential to change young people’s PA behaviour, at least in the short term, we need to focus on programmes that obtained the highest effect sizes,8 but also study the cost-effectiveness in real-world trials ideally with long-term follow-ups. Only then can we be more confident that PA changes in youth can be sustained and translate into better health in later life, as previously suggested.38,51,58-60
CONCLUSION
This review shows strong evidence for the positive effect of school-based interventions on PA in children and adolescents. These conclusions are based on four systematic reviews published after 2006 of studies focussing on PA promotion in school and other settings and on a new systematic review of trials published between January 2007 and December 2010. Our review of the more recent publications is the first to show that PA promotion in the school setting not only leads to an increase in school-based PA, but is also associated with an increase in out-of-school, and even more importantly, in overall PA. There is some evidence that school-based interventions can have positive effects on aerobic fitness, although this evidence is weaker. Since efficacy of school-based PA promotion is globally evident, the time is ripe to look at long-term effects and to figure out effective implementation strategies.
Supplementary Material
Table 2.
Overview of the studies included in the updated review, classified by effectiveness on physical activity, fitness and motor skills
| STUDY | OUTCOME MEASURE | RESULTS | |||
|---|---|---|---|---|---|
|
| |||||
| Study (first author and year of publication) |
Outcome: instrument | Total PA | PA in school or LTPA | Fitness | Motor skills |
|
| |||||
| Angelopoulos 09 | PA: quest | + (LTPA) | |||
|
| |||||
| Boyles-Holmes 10 | PA: quest, FIT: field, MS: qual | + (4th grade) | 0 | + | |
|
| |||||
| Gentile 09 | PA: ped, quest | 0 (all), + (girls) | |||
|
| |||||
| Gomes 09 | PA: quest | + | |||
|
| |||||
| Gorely 09 | PA: ped, accss, FIT: field | +, (+ Accss) | 0 | ||
|
| |||||
| Graf 08 | FIT: field, MS: quant | 0 | + (1 of 4 tests) | ||
|
| |||||
| Haerens 07 | PA: quest , accss | 0, (+ Accss) | + (PA at school), 0 (LTPA) | ||
|
| |||||
| Kriemler 10 | PA: acc, FIT: field | + | + (MVPA and TPA in school) | + | |
|
| |||||
| de Meij 10 | PA: quest, accss, FIT: field | (0 Accss) | + (sport participation) | 0 | |
|
| |||||
| Mc Neil 08 | PA: quest | + (LTPA) | |||
|
| |||||
| Naylor 08 | PA: ped, questss, FIT: fieldss | + (boys) | +ss | ||
|
| |||||
| Reseland 09 | FIT: VO2max | + | |||
|
| |||||
| Ridgers 07 | PA: acc, hr | + (recess, lunch) | |||
|
| |||||
| Salmon 08 | PA: acc, MS: qual | + | 0 (all), + (girls) | ||
|
| |||||
| Schneider 08 | PA: quest, FIT: VO2max | + | + (LTPA) | + | |
|
| |||||
| Simon 08 | PA: quest | + (LTPA) | |||
|
| |||||
| Sollerhed 08 | FIT: field, MS: quant | + | + | ||
|
| |||||
| Taymoori 08 | PA: quest | + | |||
|
| |||||
| Verstraete 07 | PA: quest, obsss, accss, FIT: field, MS: quant | (+ Accss) | +(LTPA), + (obsss), 0 (Accss) | 0 | 0 |
|
| |||||
| Walther 09 | FIT: VO2max, MS: quant | + | 0 | ||
|
| |||||
| Summary | PA only (n=8) FIT only (n=4) combined (n=8) |
+ (n=6) | + (n=8) | + (n=5) | + (n=3) |
| +ss (n=3) | +ss (n=1) | ||||
| +sg (n=3) | +sg(n=1) | ||||
| 0 (n=2) | 0 (n=1) | 0 (n=5) | 0 (n=2) | ||
| 0ss (n=1) | |||||
| na (n=8) | na (n=11) | na (n=9) | na (n=14) | ||
Abbreviations: PA=physical activity, FIT=fitness, MS=motor skills, quest=questionnaire based PA assessment, acc=PA measured by accelerometers, ped=PA measured by pedometers, obs=PA assessed by observation, hr=PA assessed by heart rate, TPA=total physical activity, LTPA=leisure time physical activity, VO2max=fitness assessed by measurement of maximal oxygen uptake, field=fitness assessed by field test, quant=quantitative assessment of motor skills, qual=qualitative assessment of motor skills. sssubsample=random subset of individuals from within the whole population, sgsubgroup=group within the study population with a defined characteristic (i.e. gender, grade). +=significant positive effect of the intervention, +ss=significant effect in a subsample, 0=no effect of the intervention, 0ss=no effect in a subsample, na=not applicable/not assessed
REFERENCES
- 1.Lee CD, Blair SN, Jackson AS. Cardiorespiratory fitness, body composition, and all-cause and cardiovascular disease mortality in men. Am J Clin Nutr. 1999;69:373–80. doi: 10.1093/ajcn/69.3.373. [DOI] [PubMed] [Google Scholar]
- 2.WHO . WHO. Global health risks. Mortality and burden of disease attributable to selected major risks. World Health Organisation; Geneva: 2009. pp. 10–12. [Google Scholar]
- 3.Twisk JW, Kemper HC, van Mechelen W. Tracking of activity and fitness and the relationship with cardiovascular disease risk factors. Med Sci Sports Exerc. 2000;32:1455–61. doi: 10.1097/00005768-200008000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Salmon J, Booth ML, Phongsavan P, et al. Promoting physical activity participation among children and adolescents. Epidemiol Rev. 2007;29:144–59. doi: 10.1093/epirev/mxm010. [DOI] [PubMed] [Google Scholar]
- 5.van Sluijs EMF, McMinn AM, Griffin S. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ. 2007;335:703–07. doi: 10.1136/bmj.39320.843947.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dobbins M, De Corby K, Robeson P, et al. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6-18. Cochrane Database Syst Rev. 2009 doi: 10.1002/14651858.CD007651. [DOI] [PubMed] [Google Scholar]
- 7.De Meester F, van Lenthe FJ, Spittaels H, et al. Interventions for promoting physical activity among European teenagers: a systematic review. Int J of Behav Nutr Phys Act. 2009;6 doi: 10.1186/1479-5868-6-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crutzen R. Adding effect sizes to a systematic review on interventions for promoting physical activity among European teenagers. Int J Behav Nutr Phys Act. 2010;7 doi: 10.1186/1479-5868-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dobbins M, De Corby K, Robeson P, et al. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6-18. Cochrane Database Syst Rev. 2009;21:CD007651. doi: 10.1002/14651858.CD007651. [DOI] [PubMed] [Google Scholar]
- 10.Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71:S1–14. [PubMed] [Google Scholar]
- 11.Donnelly JE, Jacobsen DJ, Whatley JE, et al. Nutrition and physical activity program to attenuate obesity and promote physical and metabolic fitness in elementary school children. Obes Res. 1996;4:229–43. doi: 10.1002/j.1550-8528.1996.tb00541.x. [DOI] [PubMed] [Google Scholar]
- 12.Mallam KM, Metcalf BS, Kirkby J, et al. Contribution of timetabled physical education to total physical activity in primary school children: cross sectional study. BMJ. 2003;327:592–3. doi: 10.1136/bmj.327.7415.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de Meij JS, Chinapaw MJ, van Stralen MM, et al. Effectiveness of JUMP-in, a Dutch primary school-based community intervention aimed at the promotion of physical activity. Br J Sports Med. 2010 doi: 10.1136/bjsm.2010.075531. [DOI] [PubMed] [Google Scholar]
- 14.Angelopoulos PD, Milionis HJ, Grammatikaki E, et al. Changes in BMI and blood pressure after a school based intervention: The CHILDREN study. Eur J Public Health. 2009;19:319–25. doi: 10.1093/eurpub/ckp004. [DOI] [PubMed] [Google Scholar]
- 15.Boyle-Holmes T, Grost L, Russell L, et al. Promoting elementary physical education: Results of a school-based evaluation study. Health Edu Behav. 2010;37:377–89. doi: 10.1177/1090198109343895. [DOI] [PubMed] [Google Scholar]
- 16.Gentile DA, Welk G, Eisenmann JC, et al. Evaluation of a multiple ecological level child obesity prevention program: Switch what you Do, View, and Chew. BMC Med. 2009;7:49. doi: 10.1186/1741-7015-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gomes de Barros MV, Nahas MV, Hallal PC, et al. Effectiveness of a school-based intervention on physical activity for high school students in Brazil: The Saude na Boa project. J Phys Act Health. 2009;6:163–69. doi: 10.1123/jpah.6.2.163. [DOI] [PubMed] [Google Scholar]
- 18.Gorely T, Nevill ME, Morris JG, et al. Effect of a school-based intervention to promote healthy lifestyles in 7-11 year old children. Int J Behav Nutr Phys Act. 2009;6 doi: 10.1186/1479-5868-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Graf C, Koch B, Falkowski G, et al. School-based prevention: Effects on obesity and physical performance after 4 years. J Sports Sci. 2008;26:987–94. doi: 10.1080/02640410801930176. [DOI] [PubMed] [Google Scholar]
- 20.Haerens L, De Bourdeaudhuij I, Maes L, et al. School-based randomized controlled trial of a physical activity intervention among adolescents. J Adolesc Health. 2007;40:258–65. doi: 10.1016/j.jadohealth.2006.09.028. [DOI] [PubMed] [Google Scholar]
- 21.Kriemler S, Zahner L, Schindler C, et al. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary schoolchildren: cluster randomised controlled trial. BMJ. 2010;340:c785. doi: 10.1136/bmj.c785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McNeil DA, Wilson BN, Siever JE, et al. Connecting Children to Recreational Activities: Results of a Cluster Randomized Trial. Am J of Health Prom. 2009;23:376–87. doi: 10.4278/ajhp.071010107. [DOI] [PubMed] [Google Scholar]
- 23.Naylor PJ, Macdonald HM, Warburton DE, et al. An active school model to promote physical activity in elementary schools: action schools BC. Br J Sports Med. 2008;42:338–43. doi: 10.1136/bjsm.2007.042036. [DOI] [PubMed] [Google Scholar]
- 24.Resaland GK, Andersen LB, Mamen A, et al. Effects of a 2-year school-based daily physical activity intervention on cardiorespiratory fitness: the Sogndal school-intervention study. Scand J Med Sci Sports. 2009 doi: 10.1111/j.1600-0838.2009.01028.x. [DOI] [PubMed] [Google Scholar]
- 25.Ridgers ND, Stratton G, Fairclough SJ, et al. Long-term effects of a playground markings and physical structures on children’s recess physical activity levels. Prev Med. 2007 doi: 10.1016/j.ypmed.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 26.Salmon J, Ball K, Hume C, et al. Outcomes of a group-randomized trial to prevent excess weight gain, reduce screen behaviours and promote physical activity in 10-year-old children: switch-play. Int J Obes (Lond) 2008;32:601–12. doi: 10.1038/sj.ijo.0803805. [DOI] [PubMed] [Google Scholar]
- 27.Schneider M, Dunton GF, Cooper DM. Physical activity and physical self-concept among sedentary adolescent females: An intervention study. Psychol Sport Exerc. 2008;9:1–14. doi: 10.1016/j.psychsport.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schneider M, Dunton GF, Bassin S, et al. Impact of a school-based physical activity intervention on fitness and bone in adolescent females. J of Phys Act Health. 2007;4:17–29. doi: 10.1123/jpah.4.1.17. [DOI] [PubMed] [Google Scholar]
- 29.Simon C, Schweitzer B, Oujaa M, et al. Successful overweight prevention in adolescents by increasing physical activity: a 4-year rvandomized controlled intervention. Int J of Obesity. 2008;32:1489–98. doi: 10.1038/ijo.2008.99. [DOI] [PubMed] [Google Scholar]
- 30.Sollerhed AC, Ejlertsson G. Physical benefits of expanded physical education in primary school: findings from a 3-year intervention study in Sweden. Scand J of Med Sci Sports. 2008;18:102–07. doi: 10.1111/j.1600-0838.2007.00636.x. [DOI] [PubMed] [Google Scholar]
- 31.Taymoori P, Niknami S, Berry T, et al. A school-based randomized controlled trial to improve physical activity among Iranian high school girls. Int J Behav Nutr Phys Act. 2008;5 doi: 10.1186/1479-5868-5-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Verstraete SJM, Cardon GM, De Clercq DLR, et al. A comprehensive physical activity promotion programme at elementary school: The effects on physical activity, physical fitness and psychosocial correlates of physical activity. Public H Nutr. 2007;10:477–84. doi: 10.1017/S1368980007223900. [DOI] [PubMed] [Google Scholar]
- 33.Verstraete SJM, Cardon GM, De Clercq DLR, et al. Effectiveness of a Two-Year Health-Related Physical Education Intervention in Elementary Schools. J Teach Phys Edu. 2007;26:20–34. [Google Scholar]
- 34.Walther C, Gaede L, Adams V, et al. Effect of Increased Exercise in School Children on Physical Fitness and Endothelial Progenitor Cells A Prospective Randomized Trial. Circulation. 2009;120:2251–59. doi: 10.1161/CIRCULATIONAHA.109.865808. [DOI] [PubMed] [Google Scholar]
- 35.Simon C, Schweitzer B, Oujaa M, et al. Successful overweight prevention in adolescents by increasing physical activity: a 4-year randomized controlled intervention. Int J of Obesity. 2008;32:1489–98. doi: 10.1038/ijo.2008.99. [DOI] [PubMed] [Google Scholar]
- 36.Ridgers ND, Fairclough SJ, Stratton G. Twelve-Month Effects of a Playground Intervention on Children’s Morning and Lunchtime Recess Physical Activity Levels. J of Phys Act Health. 2010;7:167–75. doi: 10.1123/jpah.7.2.167. [DOI] [PubMed] [Google Scholar]
- 37.Resaland GK, Mamen A, Anderssen SA, et al. Cardiorespiratory fitness and body mass index values in 9-year-old rural Norwegian children. Acta Paediatr. 2009;98:687–92. doi: 10.1111/j.1651-2227.2008.01181.x. [DOI] [PubMed] [Google Scholar]
- 38.Strong WB, Malina RM, Blimkie CJ, et al. Evidence based physical activity for school-age youth. J Pediatr. 2005;146:732–7. doi: 10.1016/j.jpeds.2005.01.055. [DOI] [PubMed] [Google Scholar]
- 39.Francis M, Nichols SS, Dalrymple N. The effects of a school-based intervention programme on dietary intakes and physical activity among primary-school children in Trinidad and Tobago. Public Health Nutr. 2010;13:738–47. doi: 10.1017/S1368980010000182. [DOI] [PubMed] [Google Scholar]
- 40.Hill C, Abraham C, Wright DB. Can theory-based messages in combination with cognitive prompts promote exercise in classroom settings? Soc Sci Med. 2007;65:1049–58. doi: 10.1016/j.socscimed.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 41.Horne PJ, Hardman CA, Lowe CF, et al. Increasing children’s physical activity: a peer modelling, rewards and pedometer-based intervention. Eur J Clin Nutr. 2009;63:191–8. doi: 10.1038/sj.ejcn.1602915. [DOI] [PubMed] [Google Scholar]
- 42.McManus AM, Masters RS, Laukkanen RM, et al. Using heart-rate feedback to increase physical activity in children. Prev Med. 2008;47:402–8. doi: 10.1016/j.ypmed.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 43.Connelly JB, Duaso MJ, Butler G. A systematic review of controlled trials of interventions to prevent childhood obesity and overweight: a realistic synthesis of the evidence. Public Health. 2007;121:510–7. doi: 10.1016/j.puhe.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 44.Heitzler CD, Martin SL, Duke J, et al. Correlates of physical activity in a national sample of children aged 9-13 years. Prev Med. 2006;42:254–60. doi: 10.1016/j.ypmed.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 45.Crutzen R. Adding effect sizes to a systematic review on interventions for promoting physical activity among European teenagers. Int J Behav Nutr Phys Act. 2010;7 doi: 10.1186/1479-5868-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Meij JSBD. Promoting physical activity in children: the stepwise development of the primary school-based JUMP-in intervention applying the RE-AIM evaluation framework. Br J of Sports Med. 2010;44:879–87. doi: 10.1136/bjsm.2008.053827. [DOI] [PubMed] [Google Scholar]
- 47.Corder K, Ekelund U, Steele RM, et al. Assessment of physical activity in youth. J Appl Physiol. 2008;105:977–87. doi: 10.1152/japplphysiol.00094.2008. [DOI] [PubMed] [Google Scholar]
- 48.Lubans DR, Morgan PJ, Cliff DP, et al. Fundamental movement skills in children and adolescents: review of associated health benefits. Sports Med. 2010;40:1019–35. doi: 10.2165/11536850-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 49.Kafatos I, Manios Y, Moschandreas J, et al. Health and nutrition education program in primary schools of Crete: changes in blood pressure over 10 years. Eur J of Clin Nutr. 2007;61:837–45. doi: 10.1038/sj.ejcn.1602584. [DOI] [PubMed] [Google Scholar]
- 50.Klepp KI, Tell GS, Vellar OD. Ten-year follow-up of the Oslo Youth Study Smoking Prevention Program. 1993;22:453–62. doi: 10.1006/pmed.1993.1037. [DOI] [PubMed] [Google Scholar]
- 51.Trudeau F, Laurencelle L, Tremblay J, et al. Daily primary school physical education: effects on physical activity during adult life. Med Sci Sports and Exerc. 1999;31:111–17. doi: 10.1097/00005768-199901000-00018. [DOI] [PubMed] [Google Scholar]
- 52.Magesa SM, Lengeler C, deSavigny D, et al. Creating an “enabling environment” for taking insecticide treated nets to national scale: the Tanzanian experience. Malar J. 2005;4:34. doi: 10.1186/1475-2875-4-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Naylor PJ, McKay HA. Prevention in the first place: schools a setting for action on physical inactivity. Br J Sports Med. 2009;43:10–13. doi: 10.1136/bjsm.2008.053447. [DOI] [PubMed] [Google Scholar]
- 54.Reed KE, Warburton DE, Macdonald HM, et al. Action Schools BC: a school-based physical activity intervention designed to decrease cardiovascular disease risk factors in children. Prev Med. 2008;46:525–31. doi: 10.1016/j.ypmed.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 55.Haerens L, Cerin E, Maes L, et al. Explaining the effect of a 1-year intervention promoting physical activity in middle schools: a mediation analysis. Public Health Nutr. 2008;11:501–12. doi: 10.1017/S136898000700078X. [DOI] [PubMed] [Google Scholar]
- 56.Lubans DR, Morgan PJ, Callister R, et al. Exploring the mechanisms of physical activity and dietary behavior change in the program x intervention for adolescents. J Adolesc Health. 2010;47:83–91. doi: 10.1016/j.jadohealth.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 57.Naylor PJ, Scott J, Drummond J, et al. Implementing a whole school physical activity and healthy eating model in rural and remote first nations schools: a process evaluation of action schools BC. Rural and remote health. 2010;10:1296. [PubMed] [Google Scholar]
- 58.Andersen LB, Harro M, Sardinha LB, et al. Physical activity and clustered cardiovascular risk in children: a cross-sectional study (The European Youth Heart Study) Lancet. 2006;368:299–304. doi: 10.1016/S0140-6736(06)69075-2. [DOI] [PubMed] [Google Scholar]
- 59.Perez CE. Children who become active. Health Rep. 2003;14(Suppl):17–28. [PubMed] [Google Scholar]
- 60.Li S, Zhao JH, Luan J, et al. Physical activity attenuates the genetic predisposition to obesity in 20,000 men and women from EPIC-Norfolk prospective population study. PLoS Med. 2010;7 doi: 10.1371/journal.pmed.1000332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.